Abstract
AIM: To evaluate the safety and effectiveness of endoscopic papillary large balloon dilation (EPLBD) for bile duct stone extraction in patients with periampullary diverticula.
METHODS: The records of 223 patients with large common bile duct stones (≥ 10 mm) who underwent EPLBD (12-20 mm balloon diameter) with or without limited endoscopic sphincterotomy (ES) from July 2006 to April 2011 were retrospectively reviewed. Of these patients, 93 (41.7%) had periampullary diverticula (PAD), which was categorized into three types. The clinical variables of EPLBD with limited ES (EPLBD + ES) and EPLBD alone were analyzed according to the presence of PAD.
RESULTS: Patients with PAD were significantly older than those without (75.2 ± 8.8 years vs 69.7 ± 10.9 years, P = 0.000). The rates of overall stone removal and complete stone removal in the first session were not significantly different between the PAD and non-PAD groups, however, there was significantly less need for mechanical lithotripsy in the PAD group (3.2% vs 11.5%, P = 0.026). Overall stone removal rates, complete stone removal rates in the first session and the use of mechanical lithotripsy were not significantly different between EPLBD + ES and EPLBD alone in patients with PAD (96.6% vs 97.1%; 72.9% vs 88.2%; and 5.1% vs 0%, respectively). No significant differences with respect to the rates of pancreatitis, perforation, and bleeding were observed between EPLBD + ES and EPLBD alone in the PAD group (3.4% vs 14.7%, P = 0.095; 0% vs 0%; and 3.4% vs 8.8%, P = 0.351, respectively).
CONCLUSION: EPLBD with limited ES and EPLBD alone are safe and effective modalities for common bile duct stone removal in patients with PAD, regardless of PAD subtypes.
Keywords: Endoscopic papillary large balloon dilation, Endoscopic sphincterotomy, Periampullary diverticula
Core tip: Endoscopic papillary large balloon dilation (EPLBD) is a highly effective technique for treating difficult bile duct stones. However, the safety of EPLBD is of concern, especially in patients with periampullary diverticula (PAD). In the present study, the clinical outcomes and complications of EPLBD with limited endoscopic sphincterotomy (ES) (EPLBD + ES) and EPLBD alone according to the presence of PAD were not significantly different. We suggest that EPLBD + ES and EPLBD alone are safe and feasible modalities for large bile duct stone removal in patients with PAD. Furthermore, the presence of PAD was not found to affect therapeutic outcomes.
INTRODUCTION
Although endoscopic sphincterotomy (ES) is the standard therapy for choledocholithiasis, it has been reported to produce several serious complications, such as bleeding and perforation[1-3]. Endoscopic papillary balloon dilation (EPBD), which was introduced by Staritz et al[4], has been used as an alternative procedure for the removal of common bile duct (CBD) stones. However, several cases of post-procedural pancreatitis and two deaths associated with EPBD have been documented[5]. Furthermore, it has been reported that mechanical lithotripsy is more frequently required during EPBD than during ES[6,7].
Some bile duct stones are difficult to remove due to a large size, a rectangular shape, or anatomical difficulties, and these remain challenges for endoscopists despite advancements in expertise and the developments of various accessories. Several recent series have demonstrated that endoscopic papillary large balloon dilation (EPLBD) combined with limited endoscopic sphincterotomy (EPLBD + ES) has a similar therapeutic effect, but a lower complication rate than standard ES for the removal of difficult bile duct stones[8-12]. In particular, anatomical variations, such as periampullary diverticula (PAD), which can influence endoscopic outcomes because of the high risk of procedure-associated complications. Duodenal diverticula are outpouchings of mucosa, submucosa, and partially speckled muscle along the intestinal wall. Reported locations and incidences of PAD in the general population vary[13-18]. PAD is known to be associated with an increased frequency of pancreatobiliary diseases, and it is widely accepted that the presence of diverticula can be a technical obstacle to cannulation and requires skillful endoscopy manipulation[13,14]. However, recent two studies have shown that rates of successful cannulation are not dependent on the presence of diverticula[17,19].
Nevertheless, when EPLBD is performed in patients with PAD, the potential risks of perforation and bleeding are of concern, because the ampullary area in PAD is composed of thin mucosa without sphincter muscle. Recent studies have indicated that EPLBD without ES is as effective and safe as ES for the removal of large bile duct stones, regardless of the presence of PAD[20-22]. Accordingly, the aim of this study was to evaluate the technical feasibility and safety of EPLBD with or without ES for the removal of CBD stones in patients with PAD.
MATERIALS AND METHODS
The records of 223 patients with CBD stones ≥ 10 mm in diameter who underwent EPLBD combined with antecedent ES (EPLBD + ES) or EPLBD alone (EPLBD - ES) for the removal of bile duct stones from July 2006 to April 2011 were retrospectively reviewed. Patients with a history of endoscopic sphincterotomy or Roux-en-Y gastrojejunostomy were excluded. All procedures were performed using side-viewing endoscopes (TJF-240; Olympus Optical Corporation, Tokyo, Japan). Endoscopic retrograde cholangiopancreatography (ERCP) was performed by experienced endoscopists at a single center. Cannulation was attempted using an ERCP catheter or a pull-type sphincterotome. When conventional cannulation failed, a pre-cut technique using a needle knife was applied. EPLBD was performed using a dilating balloon catheter (CRE balloon, Boston Scientific Cork, Ireland) positioned at the center of the balloon across the ampullary orifice (Figure 1). Dilating balloon catheters with a diameter of 12-20 mm were used. Ballooning size was determined based on stone sizes and CBD diameter, but should not exceed 2 mm of the diameter of the distal CBD. Balloons were inflated with caution until balloon notches disappeared. Mechanical lithotripsy was attempted when stones were too difficult to remove intact. When incomplete stone removal was suspected, a nasobiliary tube or a plastic stent was placed to prevent cholangitis. Complete stone removal was confirmed either by cholangiogram at the end of each procedure or by follow-up cholangiogram through a nasobiliary tube. The presence and types of diverticula were documented. Duodenal diverticula were categorized into three subtypes based on the locations of the major papilla with respect to diverticula: (1) type 1, when papilla was located inside the diverticulum; (2) type 2, when papilla was located in the margin of the diverticulum; and (3) type 3, when papilla was located outside the diverticulum (Figure 2). Patients were thoroughly observed for possible complications including bleeding, pancreatitis, and perforation during and after ERCP. Post-ERCP pancreatitis was defined as a serum amylase level exceeding three times the upper normal limit and the development of abdominal pain after ERCP. Hyperamylasemia was defined as a serum amylase level exceeding three times the normal upper limit without any abdominal pain. Post-ERCP bleeding was classified as major or minor based on amounts of hemorrhage. Major bleeding was defined as moderate to severe hemorrhage necessitating transfusion or intervention, and minor bleeding was defined as mild hemorrhage not requiring transfusion. Clinical and endoscopic factors were retrospectively evaluated. The study was approved by the institutional review board of our hospital.
Figure 1.
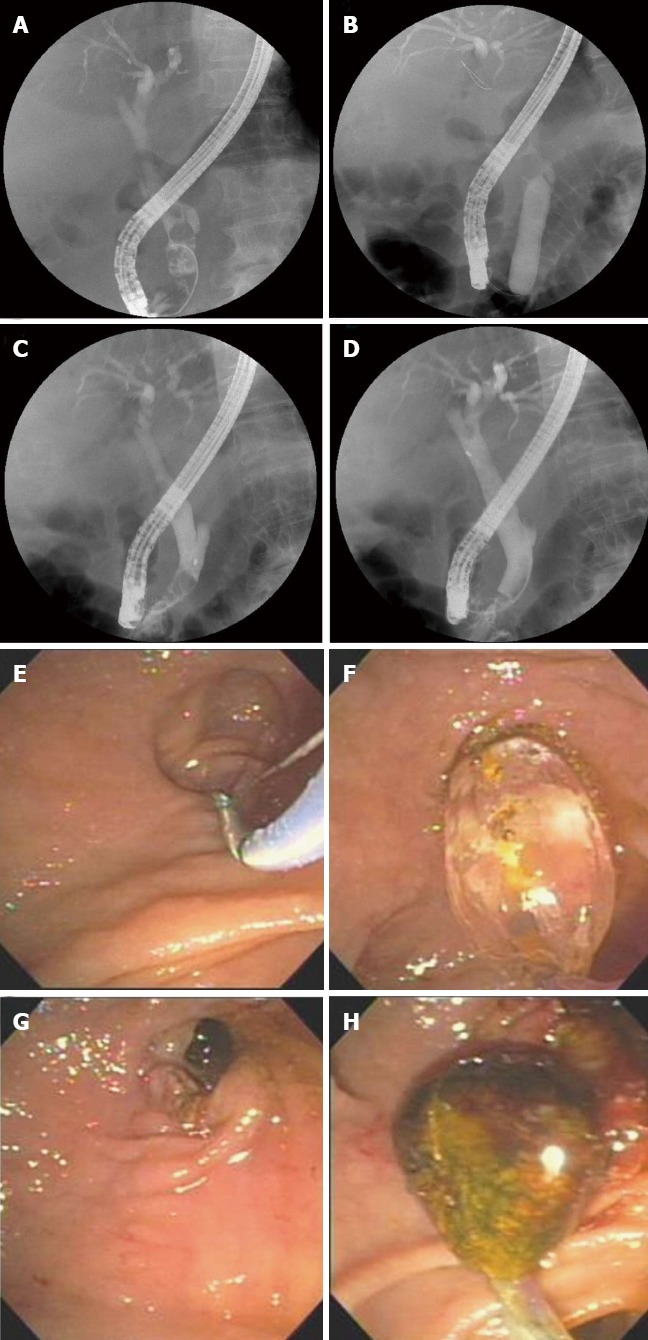
Endoscopic papillary large balloon dilation in a patient with periampullary diverticulum. A: Cholangiogram showing multiple movable filling defects in the common bile duct; B: Fluoroscopic view showing the disappearance of balloon waist after gradual inflation with contrast media; C: Cholangiogram showing a large stone captured in a basket; D: Cholangiogram showing no residual filling defects in the common bile duct; E: Endoscopic sphincterotomy was carefully performed due to the presence of a huge diverticulum; F: Endoscopic view showing a dilating balloon inflated to 15 mm; G: Endoscopic view showing an enlarged ampullary opening; H: Endoscopic view showing a large brown pigment stone being extracted with a basket.
Figure 2.
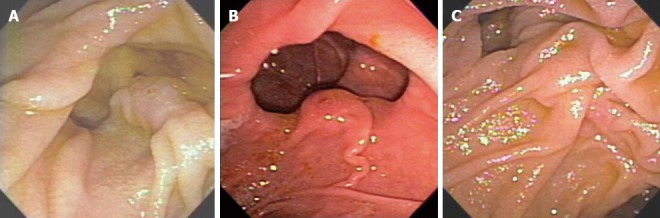
Endoscopic classification of periampullary diverticula. A: Type 1 with major papilla located inside the diverticulum; B: Type 2 with major papilla located in the margin of the diverticulum; C: Type 3 with major papilla located outside the diverticulum.
Statistical analysis
Statistical analysis was carried out using the Student’s t test, the χ2 test, and one-way ANOVA in SPSS version 17.0 (SPSS, Inc., Chicago, IL, United States). A P value < 0.05 was considered statistically significant.
RESULTS
Demographic characteristics of the 223 patients (122 men, 101 women; mean age 72.0 ± 10.4 years) are presented in Table 1. The incidence of PAD was 41.7% (93/223). The mean age was significantly higher in the PAD group (75.2 ± 8.8 years vs 69.7 ± 10.9 years, P = 0.000), and no difference was found between genders. Of the 93 cases of diverticula, 18 cases (19.3%) were of type 1, 41 cases (44.0%) were of type 2, and 34 cases (36.7%) were of type 3. Billroth II gastrectomy state was documented in 7 patients (7.5%) in the PAD group and in 19 patients (14.6%) in the non-PAD group (P = 0.138). The frequencies of EPLBD + ES and EPLBD - ES were not significantly different between the PAD and non-PAD groups (EPLBD + ES, 63.4% vs 56.2%; and EPLBD - ES, 36.6% vs 43.8%, P = 0.334, respectively). The mean stone size in the 223 patients was 15.9 ± 5.8 mm (range, 10-40 mm), the mean bile duct diameter was 19.9 ± 5.3 mm (range, 10-37 mm), and the mean dilated balloon size was 15.6 ± 2.4 mm (range, 12-20 mm). The mean stone(s) and CBD diameters were not significantly different between the PAD and non-PAD groups (16.4 ± 6.0 mm vs 15.5 ± 5.7 mm, P = 0.252; and 20.0 ± 5.0 mm vs 19.8 ± 5.4 mm, P = 0.743, respectively). Mean balloon diameter for EPLBD was 15.5 ± 2.4 mm in the PAD group and 15.8 ± 2.4 mm in the non-PAD group (P = 0.374).
Table 1.
Baseline characteristics of patients n (%)
| Variable | Total (n = 223) | PAD group (n = 93) | Non-PAD group (n = 130) | P value |
| Mean age (yr) | 72.0 ± 10.4 (39-92) | 75.2 ± 8.8 (51-92) | 69.7 ± 10.9 (39-90) | 0.000 |
| Sex (male/female) | 122:101 (54.7:45.3) | 46:47 (49.5:50.5) | 76:54 (58.5:41.5) | 0.220 |
| BMI (kg/m2) | 22.6 ± 3.1 | 22.5 ± 2.8 | 22.6 ± 3.3 | 0.947 |
| Billroth II gastrectomy | 26 (11.7) | 7 (7.5) | 19 (14.6) | 0.138 |
| Large balloon dilation | ||||
| With ES | 132 (59.2) | 59 (63.4) | 73 (56.2) | 0.334 |
| Without ES | 91 (40.8) | 34 (36.6) | 57 (43.8) | |
| Precutting with needle knife | 25 (11.2) | 9 (9.7) | 16 (12.3) | 0.668 |
| CBD stones | ||||
| Mean diameter of stone (mm) | 15.9 ± 5.8 (10-40) | 16.4 ± 6.0 (10-37) | 15.5 ± 5.7 (10-40) | 0.252 |
| Number of stones | ||||
| 1/2/≥ 3 | 119/35/68 | 49/15/29 | 70/20/39 | 0.835 |
| Types of stones | ||||
| Brown/black/cholesterol | 182/33/2 (83.9/15.2/0.9) | 82/9/0 (90.1/9.9/0) | 100/24/2 (79.4/19.0/1.6) | 0.144 |
| Mean diameter of CBD (mm) | 19.9 ± 5.3 (10-37) | 20.0 ± 5.0 (10-35) | 19.8 ± 5.4 (10-37) | 0.743 |
| Distal CBD angulation (degree) | 140.6 ± 21.9 | 142.1 ± 21.8 | 139.4 ± 22.0 | 0.444 |
| Balloon dilation | ||||
| Dilating balloon size (mm) | 15.6 ± 2.4 (12-20) | 15.5 ± 2.4 (12-20) | 15.8 ± 2.4 (12-20) | 0.374 |
| Duration of ballooning (s) | 38.3 ± 16.1(10–60) | 36.1 ± 15.0 (10–60) | 39.9 ± 16.8 (10–60) | 0.081 |
Values are presented as mean ± SD (range). PAD: Periampullary diverticula; BMI: Body mass index; ES: Endoscopic sphincterotomy; CBD: Common bile duct.
Of the 223 patients, stone removal was completed in 96.9% (216/223). The rates of overall stone removal and stone removal in the first session were not significantly different between the PAD and non-PAD groups [90/93 (96.8%) vs 126/130 (96.9%), P = 1.000; and 73/93 (78.5%) vs 93/130 (71.5%), P = 0.277, respectively], but the frequency of mechanical lithotripsy was significantly lower in the PAD group [3/93 (3.2%) vs 15/130 (11.5%), P = 0.026]. When the PAD and non-PAD groups were further divided by EPLBD + ES or EPLBD - ES, no significant differences with respect to overall stone removal rates, stone removal rates in the first session or needs for mechanical lithotripsy were observed [57/59 (96.6%) vs 33/34 (97.1%), P = 1.000; 43/59 (72.9%) vs 30/34 (88.2%), P = 0.016; and 3/59 (5.1%) vs 0 (0%), P = 0.297, respectively, Table 2]. Sub-analysis by PAD type revealed no significant difference with regard to age, stone size, CBD diameter, distal CBD angle, dilated balloon size, or duration of ballooning (Table 3). When comparing types of PAD, overall stone removal rates, complete stone removal rates in the first session, and the use of mechanical lithotripsy were not significantly different (Table 3). Procedure-related complications are listed in Table 4. The rates of post-ERCP pancreatitis, perforation, and bleeding were not significantly different between the PAD and non-PAD groups [7/93 (7.5%) vs 12/130 (9.2%), P = 0.809; 0% vs 1/130 (0.8%), P = 1.000; and 5/93 (5.4%) vs 11/130 (8.5%), P = 0.548, respectively]. When complications of EPLBD with or without ES were compared in the PAD group, the rates of pancreatitis, perforation, and bleeding did not differ significantly [2/59 (3.4%) vs 5/34 (14.7%), P = 0.095; 0% vs 0%; and 2/59 (3.4%) vs 3/34 (8.8%), P = 0.351, respectively]. Moreover, complication rates were not significantly different for PAD subtypes (Table 5). All cases of pancreatitis were mild and they were treated conservatively. There were 16 (7.1%) bleeding cases, including one case (0.4%) of major bleeding and 15 cases (6.7%) of minor bleeding. The one major hemorrhage, which required more than 5 pints of blood, occurred in the non-PAD group. This patient was referred for emergency surgery for bleeding control and was managed effectively, with no further consequence. In addition, there were two in-hospital deaths in the non-PAD group. One in the EPLBD - ES group was caused by retroperitoneal perforation directly attributed to ERCP, and the other occurred in cirrhotic patients with fulminant hepatic failure and multi-organ failure due to sepsis in the EPLBD + ES group.
Table 2.
Comparison of outcomes between the two groups n (%)
|
PAD group (n = 93) |
Non-PAD group (n = 130) |
P value1 | |||||
| EPLBD + ES (n = 59) | EPLBD - ES (n = 34) | P value | EPLBD + ES (n = 73) | EPLBD - ES (n = 57) | P value | ||
| Overall stone removal | 57 (96.6) | 33 (97.1) | 1.000 | 72 (98.6) | 54 (94.7) | 0.319 | 1.000 |
| Complete stone removal in 1st session | 43 (72.9) | 30 (88.2) | 0.116 | 51 (69.9) | 42 (73.7) | 0.632 | 0.277 |
| Mechanical lithotripsy | 3 (5.1) | 0 (0.0) | 0.297 | 9 (12.3) | 6 (10.5) | 0.750 | 0.026 |
Comparison between the periampullary diverticula (PAD) and non-PAD groups. EPLBD: Endoscopic papillary large balloon dilation; ES: Endoscopic sphincterotomy; EPLBD+ES: Endoscopic papillary large balloon dilation with limited endoscopic sphincterotomy; EPLBD-ES: Endoscopic papillary large balloon dilation without endoscopic sphincterotomy.
Table 3.
Baseline characteristics and outcomes of patients by periampullary diverticula type n (%)
| Type 1 (n = 18) | Type 2 (n = 41) | Type 3 (n = 34) | P value | |
| Mean age (yr) | 75.9 ± 6.7 | 76.5 ± 8.7 | 73.2 ± 9.9 | 0.268 |
| Large balloon dilation | ||||
| With ES | 9 (50.0) | 27 (65.9) | 23 (67.6) | 0.257 |
| Without ES | 9 (50.0) | 14 (34.1) | 11 (32.4) | |
| Mean diameter of stone (mm) | 17.8 ± 6.7 | 15.9 ± 5.5 | 16.1 ± 6.2 | 0.514 |
| Mean diameter of CBD (mm) | 20.8 ± 4.9 | 20.5 ± 5.6 | 19.0 ± 4.3 | 0.324 |
| Distal CBD angulation (degree) | 141.8 ± 9.6 | 143.6 ± 29.0 | 140.5 ± 16.6 | 0.869 |
| Balloon dilation | ||||
| Dilating balloon size (mm) | 14.7 ± 2.5 | 15.8 ± 2.4 | 15.5 ± 2.4 | 0.261 |
| Duration of ballooning (s) | 30.6 ± 12.6 | 36.3 ± 12.8 | 38.8 ± 17.9 | 0.165 |
| Overall stone removal | 17 (94.4) | 41 (100) | 32 (94.1) | 0.698 |
| Complete stone removal in 1st session | 14 (77.8) | 33 (80.5) | 26 (76.5) | 0.912 |
| Mechanical lithotripsy | 1 (5.6) | 1 (2.4) | 1 (2.9) | 0.679 |
Values are presented as mean ± SD. Type 1: When major papilla is located inside the diverticulum, Type 2: In the margin of the diverticulum; and Type 3: Outside the diverticulum. PAD: Periampullary diverticula; ES: Endoscopic sphincterotomy; CBD: Common bile duct.
Table 4.
Comparison of complications between the two groups n (%)
|
PAD (n = 93) |
Non-PAD (n = 130) |
P value1 | |||||
| EPLBD + ES (n = 59) | EPLBD - ES (n = 34) | P value | EPLBD + ES (n = 73) | EPLBD - ES (n = 57) | P value | ||
| Pancreatitis | 2 (3.4) | 5 (14.7) | 0.095 | 7 (9.6) | 5 (8.8) | 0.873 | 0.809 |
| Perforation | 0 (0.0) | 0 (0.0) | NA | 0 (0.0) | 1 (1.8) | 0.438 | 1.000 |
| Bleeding | 2 (3.4) | 3 (8.8) | 0.351 | 7 (9.6) | 4 (7.0) | 0.601 | 0.548 |
| Major | 0 (0.0) | 0 (0.0) | 1 (1.4) | 0 (0.0) | |||
| Minor | 2 (13.4) | 3 (8.8) | 6 (8.2) | 4 (7.0) | |||
| Hyperamylasemia | 4 (6.8) | 5 (14.7) | 0.279 | 15 (20.5) | 6 (10.5) | 0.123 | 0.232 |
| Mortality | 0 (0.0) | 0 (0.0) | NA | 1 (1.4) | 1 (1.8) | 1.000 | 0.230 |
Comparison of the periampullary diverticula (PAD) and non-PAD groups. EPLBD: Endoscopic papillary large balloon dilation; ES: Endoscopic sphincterotomy; EPLBD + ES: Endoscopic papillary large balloon dilation with limited ES; EPLBD - ES: Endoscopic papillary large balloon dilation without ES; NA: Not applicable.
Table 5.
Complications of endoscopic papillary large balloon dilation by periampullary diverticula subtype n (%)
|
PAD subtype (n = 93) |
||||
| Type 1 | Type 2 | Type 3 | P value | |
| (n = 18) | (n = 41) | (n = 34) | ||
| Pancreatitis | 1 (5.6) | 4 (9.8) | 2 (5.9) | 0.913 |
| Perforation | 0 (0.0) | 0 (0.0) | 0 (0.0) | NA |
| Bleeding | ||||
| Major | 0 | 0 | 0 (0.0) | NA |
| Minor | 1 (5.6) | 2 (4.9) | 2 (5.9) | 0.930 |
| Hyperamylasemia | 0 (0.0) | 5 (12.2) | 4 (11.8) | 0.240 |
| Mortality | 0 (0.0) | 0 (0.0) | 0 (0.0) | NA |
Type 1: When major papilla is located inside the diverticulum; Type 2: In the margin of the diverticulum; and Type 3: Outside the diverticulum. EPLBD: Endoscopic papillary large balloon dilation; PAD: Periampullary diverticula; NA: Not applicable.
DISCUSSION
Currently, EPLBD combined with limited ES (EPLBD + ES) is regarded as an effective modality for treating difficult common bile duct stones. Complications, such as, hemorrhage and perforation, have been reported to be less frequent in EPLBD + ES than in standard ES[9-12]. Furthermore, mechanical lithotripsy is less required during EPLBD + ES, because it provides spacious ampullary opening, and thus, facilitates complete bile duct stone removal. More recently, it has been suggested that EPLBD without ES is as safe and effective as ES for the removal of large bile duct stones[20-22]. Nevertheless, the safety of EPLBD with or without antecedent ES is still a matter of concern. In particular, risks of complications might be greater in cases of PAD.
Most periampullary diverticula are asymptomatic and are found incidentally during ERCP[15]. Although duodenal diverticula are known to be acquired lesions, the etiology of PAD has not been established[18]. Several studies have mentioned that PAD is rarely found in patients younger than 40 years old, and that the incidence of PAD shows an increasing tendency with age[15,17,18,23]. In the present study, the mean age of patients in the PAD group was significantly higher than in the non-PAD group (75.2 ± 8.8 years vs 69.7 ± 10.9 years, P = 0.000), which concurs with previous reports and supports a substantive relationship between age and the formation of PAD[15,17,18,23]. However, previous studies have reported a prevalence of PAD at ERCP ranging from 5% to 32%, whereas the prevalence of PAD in the present study was higher at 41.7%, which might be explained by the relatively high proportion of older individuals in the present study[13-18].
It is known that PAD represents a technical barrier during ERCP, and that the rate of cannulation failure is higher in PAD patients than in non-PAD patients. Several studies have addressed the influence of PAD on the technical difficulties of ERCP and on complications, and it appears that endoscopist skill, diverticula size, the location of ampulla with respect to the diverticulum, CBD angulation, bowel motility, and patient cooperation contribute to the technical success of cannulation[16,17]. In order to facilitate cannulation of the bile duct in patients with PAD, a number of clever techniques, such as precutting with a needle knife and delicate handling of the scope, have been tried. Several series have reported successful cannulation rates ranging from 94.2% to 97.0%, complete stone removal in the first session ranging from 69.9% to 76.2%, and overall stone removal in up to 95.2% of patients with PAD[15,17,24,25]. In the present study, the rates of overall CBD stone removal and complete stone removal in the first session did not differ significantly between the PAD and non-PAD groups, which concurs with previous studies[17,25]. Moreover, overall stone removal and complete stone removal rates in the first session were not significantly different between PAD subtypes in the present study, which suggests that PAD types do not influence the clinical outcomes of EPLBD.
Mechanical lithotripsy is a rather labor-intensive but necessary technique for removing difficult stones, although EPLBD + ES reportedly reduces the need for mechanical lithotripsy[25,26]. Lowering the frequency of mechanical lithotripsy is important to prevent recurrent duct stones because remnant stone fragments following lithotripsy can act as nidi for stone recurrence. Theoretically, if EPLBD with a large-diameter balloon (12-20 mm) is applied, mechanical lithotripsy might be less required than after EPBD with a small-sized balloon (≤ 10 mm). In the present study, mechanical lithotripsy was used significantly less in the PAD group than in the non-PAD group (3.2% vs 11.5%, P = 0.026). Furthermore, when EPLBD alone was performed, bile duct stones were successfully removed without mechanical lithotripsy in the PAD group. However, when EPLBD + ES was applied, mechanical lithotripsy was required for three patients (5.1%) in the PAD group, although this did not represent a significant difference. One possible explanation of these results is that ampullary enlargement can easily be achieved by EPLBD alone because of the lack of sphincter muscle in patients with PAD, which may explain the reduced need for mechanical lithotripsy after EPLBD without ES. Furthermore, ease of ampullary widening by EPLBD could explain the tendency toward a shorter ballooning time in the PAD group. These findings suggest that EPLBD - ES could be an appropriate technique for CBD stone retrieval in the presence of PAD, as long as safety is guaranteed.
Post ERCP pancreatitis, perforation and bleeding are the most important complications related to EPLBD. According to the present study and previous reports, ERCP-related complication rates are similar in patients with or without PAD and for different PAD types[16,24,25]. Pancreatitis is the most concerning complication, and EPBD is not widely recommended for stone removal due to the possibility of severe pancreatitis[5,7]. This increased risk of pancreatitis is associated with an impairment of pancreatic duct flow or direct pancreatic damage caused by physical compression during balloon dilation[3,26]. Although the pathogenesis of pancreatitis following EPLBD is not clear, it is suggested that ES prior to EPLBD could prevent potential injury of the main pancreatic duct, because ES can steer the direction of balloon dilation toward the CBD and minimize the pressure overload on the pancreatic orifice[8,20-22]. However, the recent studies have proposed that EPLBD alone can be an alternative for the removal of large stones20-22. Repeated cannulation attempts and excessive contrast injection due to anatomical difficulties could be major culprits of post-ERCP pancreatitis in patients with PAD. However, in the present study, no significant difference was observed in rates of post-ERCP pancreatitis between the PAD and non-PAD groups (7.5 % vs 9.2%, P = 0.809) or among types of PAD (5.6% vs 9.8% vs 5.9% for types 1, 2, and 3, respectively, P = 0.913). Furthermore, the rate of post-ERCP pancreatitis in the PAD group (7.5%) was lower in the present study than in previous studies (9.6%-14.5%), which could have been due to cautious and gentle cannulation[24,25]. The relatively high percentage of older patients in this study might be associated with the observed lower incidence of pancreatitis[21]. In particular, it has been suggested that longstanding CBD stones can cause gradual bile duct dilation, and subsequently, a patulous ampullary orifice[22]. In a recent study, a very low incidence of pancreatitis (1.4%) was observed following EPLBD in patients with recurrent CBD stones after ES, which is similar to the pathophysiology of the process of patulous ampulla[27].
Perforation is one of the most serious complications associated with EPLBD. Hypothetically, the risk of perforation should be higher in patients with PAD due to lack of sphincter muscle components around the ampulla. Balloon diameter and duration of ballooning are the important parameters for perforation after EPLBD. In most previous studies, balloon dilators sized from 12 to 20 mm were applied for 10 to 60 seconds, and in the present study, balloon dilators not exceeding CBD diameters were used and balloons were dilated gradually to minimize the risk of perforation[25-27]. As a result, the overall incidence of perforation was 0.4% and the risk of perforation was found to be not higher in the presence of PAD. In fact, only one case of perforation occurred in the non-PAD group. The size of sphincterotomy is another issue to consider before EPLBD. In the present study, after deep cannulation, the length of cutting was adjusted according to the locations of the ampulla and the bile duct axis. Ampullary distension without mucosal rupture around the ampulla can be obtained by gradual inflation and ballooning to an appropriate size. Because the weakest point is vulnerable to rupture by the radial forces produced by ballooning, overdilation of the ampulla exceeding CBD diameter should be avoided to prevent perforation, especially in cases of biliary stricture[27].
Bleeding is another complication and is possibly related to excessive ampullary dilation. Theoretically, bleeding risk can be increased if ES is performed. Previous studies have reported incidences of bleeding after EPLBD + ES ranging from 0% to 9%[5,8-12,25]. However, recent studies involving EPLBD without ES have reported lower rates of post-ERCP bleeding (0%-2.4%), which suggests that EPLBD without ES is suitable in patients with coagulopathies[20,21]. In the present study, we experienced one episode of major bleeding after sphincterotomy in the non-PAD group. It is presumed that most cases of post-ERCP bleeding are associated with small caliber vessels surrounding ampulla that are liable to be injured by radial pressure caused by balloon dilation, whereas large vessels are so elastic that they tend to be repelled by gradual balloon dilation[27]. The rates of adverse events in patients with PAD were acceptable in the present study.
In conclusion, EPLBD combined with limited ES and EPLBD alone appear to be safe and effective modalities for CBD stone removal in patients with PAD. PAD is commonly found in patients undergoing ERCP, and this study shows that the presence of PAD does not affect therapeutic outcome. Furthermore, an incidental finding of PAD presents no additional technical challenge to the achievement of successful EPLBD. This result complements those of previous studies on the management of CBD stones in patients with PAD. Nevertheless, because the present study is limited by its retrospective nature and a relatively small cohort, a large prospective study is needed to analyze the clinical feasibility of EPLBD with or without limited ES in patients with PAD.
COMMENTS
Background
Periampullary diverticula (PAD) may influence endoscopic outcomes because of the high risk of complications associated with anatomical variations. Endoscopic papillary large balloon dilation (EPLBD) is a useful method to remove difficult common bile duct (CBD) stones. However, the effectiveness and safety of this procedure in patients with PAD is not fully established. Accordingly, authors conducted this study to investigate the feasibility and safety of EPLBD with or without ES for the removal of CBD stones in patients with PAD.
Research frontiers
It has been reported that 10%-15% of bile duct stones are difficult to retrieve by conventional techniques. Challenging cases of stone removal are as follows: a rectangular shape, a large size (> 15 mm), Billroth-II gastrectomy, Roux-en-Y gastrojejunostomy, and PAD. PAD can infrequently present a technical barrier during endoscopic retrograde cholangiopancreatography (ERCP). In particular, diverticula size and the location of ampulla may pose technical difficulties associated with ERCP and complications. Much conflicting data regarding the technical success and complications of ERCP have been published, and recently, EPLBD has been introduced for CBD stone removal in patients with PAD.
Innovations and breakthroughs
Endoscopic papillary large balloon dilation following limited ES (EPLBD+ES) by Ersoz et al has been advocated as an alternative to ES for removal of large CBD stones. According to a few recent reports, EPLBD + ES showed a similar therapeutic effect but a lower complication rate than ES. EPLBD + ES requires mechanical lithotripsy less often due to enlargement of the ampullary opening. However, when EPLBD is performed in patients with PAD, the potential risks of perforation and hemorrhage are of particular concern. Nevertheless, several recent studies have suggested that EPLBD without ES is easy to perform for the removal of large bile duct stones, with similar therapeutic outcomes.
Applications
EPLBD combined with limited ES and without ES were found to be safe and effective for treating difficult CBD stones in patients with PAD. An incidental finding of PAD presents no additional technical challenge to the achievement of successful EPLBD.
Terminology
EPLBD + ES is defined as endoscopic papillary balloon dilation (usually ≥ 12 mm in diameter) after limited sphincterotomy, using a dilating balloon catheter (CRE Balloon, Boston Scientific Cork, Ireland). The balloon is positioned across the orifice of ampulla, gradually inflated up to an appropriate size. Duodenal diverticula (PAD) are categorized into three subtypes based on the locations of the major papilla: (1) type 1, when papilla was located inside the diverticulum; (2) type 2, in the margin of the diverticulum; and (3) type 3, located outside the diverticulum
Peer review
This retrospective study was conducted to investigate the technical feasibility and safety of EPLBD for the removal of difficult CBD stones in patients with PAD. The authors conclude that EPLBD + ES and EPLBD alone appear to be safe and effective procedures for CBD stone removal in patients with PAD. This result is encouraging and provides valuable information for other researchers.
Footnotes
Supported by A Yeungnam University Research Grant in 2012
P- Reviewers: Braden B, Osawa S, Triantafyllou K S- Editor: Gou SX L- Editor: Ma JY E- Editor: Ma S
References
- 1.Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y. Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc. 1974;20:148–151. doi: 10.1016/s0016-5107(74)73914-1. [DOI] [PubMed] [Google Scholar]
- 2.Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–393. doi: 10.1016/s0016-5107(91)70740-2. [DOI] [PubMed] [Google Scholar]
- 3.Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909–918. doi: 10.1056/NEJM199609263351301. [DOI] [PubMed] [Google Scholar]
- 4.Staritz M, Ewe K, Meyer zum Büschenfelde KH. Endoscopic papillary dilation (EPD) for the treatment of common bile duct stones and papillary stenosis. Endoscopy. 1983;15 Suppl 1:197–198. doi: 10.1055/s-2007-1021507. [DOI] [PubMed] [Google Scholar]
- 5.Baron TH, Harewood GC. Endoscopic balloon dilation of the biliary sphincter compared to endoscopic biliary sphincterotomy for removal of common bile duct stones during ERCP: a metaanalysis of randomized, controlled trials. Am J Gastroenterol. 2004;99:1455–1460. doi: 10.1111/j.1572-0241.2004.30151.x. [DOI] [PubMed] [Google Scholar]
- 6.Mathuna PM, White P, Clarke E, Merriman R, Lennon JR, Crowe J. Endoscopic balloon sphincteroplasty (papillary dilation) for bile duct stones: efficacy, safety, and follow-up in 100 patients. Gastrointest Endosc. 1995;42:468–474. doi: 10.1016/s0016-5107(95)70052-8. [DOI] [PubMed] [Google Scholar]
- 7.Mac Mathuna P, White P, Clarke E, Lennon J, Crowe J. Endoscopic sphincteroplasty: a novel and safe alternative to papillotomy in the management of bile duct stones. Gut. 1994;35:127–129. doi: 10.1136/gut.35.1.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57:156–159. doi: 10.1067/mge.2003.52. [DOI] [PubMed] [Google Scholar]
- 9.Kim HG, Cheon YK, Cho YD, Moon JH, Park do H, Lee TH, Choi HJ, Park SH, Lee JS, Lee MS. Small sphincterotomy combined with endoscopic papillary large balloon dilation versus sphincterotomy. World J Gastroenterol. 2009;15:4298–4304. doi: 10.3748/wjg.15.4298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Minami A, Hirose S, Nomoto T, Hayakawa S. Small sphincterotomy combined with papillary dilation with large balloon permits retrieval of large stones without mechanical lithotripsy. World J Gastroenterol. 2007;13:2179–2182. doi: 10.3748/wjg.v13.i15.2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kochhar R, Dutta U, Shukla R, Nagi B, Singh K, Wig JD. Sequential endoscopic papillary balloon dilatation following limited sphincterotomy for common bile duct stones. Dig Dis Sci. 2009;54:1578–1581. doi: 10.1007/s10620-008-0534-1. [DOI] [PubMed] [Google Scholar]
- 12.Heo JH, Kang DH, Jung HJ, Kwon DS, An JK, Kim BS, Suh KD, Lee SY, Lee JH, Kim GH, et al. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest Endosc. 2007;66:720–726; quiz 768, 771. doi: 10.1016/j.gie.2007.02.033. [DOI] [PubMed] [Google Scholar]
- 13.Lobo DN, Balfour TW, Iftikhar SY, Rowlands BJ. Periampullary diverticula and pancreaticobiliary disease. Br J Surg. 1999;86:588–597. doi: 10.1046/j.1365-2168.1999.01121.x. [DOI] [PubMed] [Google Scholar]
- 14.Novacek G, Walgram M, Bauer P, Schöfl R, Gangl A, Pötzi R. The relationship between juxtapapillary duodenal diverticula and biliary stone disease. Eur J Gastroenterol Hepatol. 1997;9:375–379. doi: 10.1097/00042737-199704000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Tyagi P, Sharma P, Sharma BC, Puri AS. Periampullary diverticula and technical success of endoscopic retrograde cholangiopancreatography. Surg Endosc. 2009;23:1342–1345. doi: 10.1007/s00464-008-0167-7. [DOI] [PubMed] [Google Scholar]
- 16.Boix J, Lorenzo-Zúñiga V, Añaños F, Domènech E, Morillas RM, Gassull MA. Impact of periampullary duodenal diverticula at endoscopic retrograde cholangiopancreatography: a proposed classification of periampullary duodenal diverticula. Surg Laparosc Endosc Percutan Tech. 2006;16:208–211. doi: 10.1097/00129689-200608000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Vaira D, Dowsett JF, Hatfield AR, Cairns SR, Polydorou AA, Cotton PB, Salmon PR, Russell RC. Is duodenal diverticulum a risk factor for sphincterotomy? Gut. 1989;30:939–942. doi: 10.1136/gut.30.7.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Løtveit T, Osnes M. Duodenal diverticula. Scand J Gastroenterol. 1984;19:579–581. [PubMed] [Google Scholar]
- 19.Chang-Chien CS. Do juxtapapillary diverticula of the duodenum interfere with cannulation at endoscopic retrograde cholangiopancreatography? A prospective study. Gastrointest Endosc. 1987;33:298–300. doi: 10.1016/s0016-5107(87)71602-2. [DOI] [PubMed] [Google Scholar]
- 20.Jeong S, Ki SH, Lee DH, Lee JI, Lee JW, Kwon KS, Kim HG, Shin YW, Kim YS. Endoscopic large-balloon sphincteroplasty without preceding sphincterotomy for the removal of large bile duct stones: a preliminary study. Gastrointest Endosc. 2009;70:915–922. doi: 10.1016/j.gie.2009.04.042. [DOI] [PubMed] [Google Scholar]
- 21.Chan HH, Lai KH, Lin CK, Tsai WL, Wang EM, Hsu PI, Chen WC, Yu HC, Wang HM, Tsay FW, et al. Endoscopic papillary large balloon dilation alone without sphincterotomy for the treatment of large common bile duct stones. BMC Gastroenterol. 2011;11:69. doi: 10.1186/1471-230X-11-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oh MJ, Kim TN. Prospective comparative study of endoscopic papillary large balloon dilation and endoscopic sphincterotomy for removal of large bile duct stones in patients above 45 years of age. Scand J Gastroenterol. 2012;47:1071–1077. doi: 10.3109/00365521.2012.690046. [DOI] [PubMed] [Google Scholar]
- 23.Leivonen MK, Halttunen JA, Kivilaakso EO. Duodenal diverticulum at endoscopic retrograde cholangiopancreatography, analysis of 123 patients. Hepatogastroenterology. 1996;43:961–966. [PubMed] [Google Scholar]
- 24.Panteris V, Vezakis A, Filippou G, Filippou D, Karamanolis D, Rizos S. Influence of juxtapapillary diverticula on the success or difficulty of cannulation and complication rate. Gastrointest Endosc. 2008;68:903–910. doi: 10.1016/j.gie.2008.03.1092. [DOI] [PubMed] [Google Scholar]
- 25.Kim HW, Kang DH, Choi CW, Park JH, Lee JH, Kim MD, Kim ID, Yoon KT, Cho M, Jeon UB, et al. Limited endoscopic sphincterotomy plus large balloon dilation for choledocholithiasis with periampullary diverticula. World J Gastroenterol. 2010;16:4335–4340. doi: 10.3748/wjg.v16.i34.4335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Draganov PV, Evans W, Fazel A, Forsmark CE. Large size balloon dilation of the ampulla after biliary sphincterotomy can facilitate endoscopic extraction of difficult bile duct stones. J Clin Gastroenterol. 2009;43:782–786. doi: 10.1097/MCG.0b013e31818f50a2. [DOI] [PubMed] [Google Scholar]
- 27.Kim KO, Kim TN, Lee SH. Endoscopic papillary large balloon dilation for the treatment of recurrent bile duct stones in patients with prior sphincterotomy. J Gastroenterol. 2010;45:1283–1288. doi: 10.1007/s00535-010-0284-7. [DOI] [PubMed] [Google Scholar]


