Abstract
Objective
The patterns of relationships between diabetes and depression in countries of central and eastern Europe (CEE) might differ from those in countries of western Europe and USA. Among the reasons are specifics of transitioning health care systems (including mental health) and the general social, cultural and economic background of these countries. The aim of this paper is to fill in the existing information gap and analyse the prevalence of depression symptoms in patients with diabetes in Slovakia and to identify its predictors.
Method
1043 diabetes patients from two diabetes outpatient-care offices were recruited for the study. The Patient Health Questionare 9 (PHQ-9) was applied to screen for depression symptoms. Patients were categorized into three categories based on depression symptom severity. Demographic and disease-related factors were analyzed as predictors of depression symptoms.
Results
In the univariate analysis a number of factors were associated with increasing severity of depression symptoms. In the multiavriate analysis lower education (OR 0.43;CI95% 0.28-0.65), and high degree of self-perceived severity of illness (OR 6.94;CI95% 3.39-14.97) were confirmed as independent predictors of depression symptoms in our patients.
Conclusions
Demographic and psychological factors have an important role in developing depression symptoms in patients with diabetes in our population. Further studies into the topic are needed to gain further clues on this topic throughout the Central European region. The findings of this study should be considered by mental health service providers and public health authorities to raise awareness about this important issue.
Keywords: Diabetes Mellitus, Depression, Primary Health Care, Epidemiology
Introduction
Diabetes mellitus is amongst the top 10 causes of death worldwide, and depression is amongst the 20 leading causes of burden of disease. Furthermore, unipolar depressive disorders are the leading cause of burden of disease in middle and high income countries. Both conditions therefore are of global interest and tackling them is a key medical and public health challenge [1]. The relationship between diabetes and depression is well studied and documented [2,3]. Patients with diabetes have double the odds of having depression as compared to general population [2]. A systematic review of studies including patients with type II diabetes revealed that the prevalence of depression among this group is 17.6% vs. 9.8% in the general population [4]. Another review of studies of type I patients with diabetes showed the prevalence of depression of 12.0% for people with diabetes compared with 3.2% in the control groups [5]. Co-morbidity depression results in deleterious effects on glycemic control, worsened diabetes complications, functional disability, and premature mortality [6]. Depression in patients with diabetes might also accelerate other diabetic complications and increase the disease burden for the individual [3]. Furthermore depression is a condition which tends to persist in patients with diabetes which additionally increases the importance of this topic [7].
Out of the large number of scientific studies devoted to prevalence of depression amongst patients with diabetes [4,2,5,8,9] most of the investigations were conducted on patients from the USA, western European countries or other countries outside of Europe. Data from the region of central and eastern Europe (CEE) are limited. It is important to fill in this information gap for a number of reasons. Firstly, the overal burden of disease differs in countries with different levels of economy [1]. Thus, the patterns of diabetes and depression in poorer countries of CEE might differ from countries of western Europe and the USA with higher economy levels, where most of the available data originates. Secondly, the mental health care system and the perception of mental illness (such as depression) in CEE countries is in a specific position – both because of the former communist background of these countries and because of the significantly lower expenditures, on mental health, as a share of GDP when compared to countries of western Europe [10]. Thirdly, the prevalence and patterns of demographic, social, economic or behavioral risk factors known to be associated with depression such as age, education, BMI, prevalence of other comorbidities, marital status or sexual behaviours [11,12] may be related to the social and economic environment of the country [13], and thus can differ by ecomomy level as well. We find it of high importance to examine the specific relationship of diabetes and depression with these facts in mind.
The aim of this paper is to analyse the prevalence and severity of depression symptoms and to identify the demographic, social, economic and disease related factors significantly associated with depression symptoms in patients with diabetes in Slovakia.
Materials and Methods
Participants
A cross-sectional epidemiological study was conducted in the Trnava region of Slovakia. The studied population included patients diagnosed with type I or type II diabetes, whilst having a residence in the Trnava region. Two diabetes outpatient-care offices were identified in Trnava that covered the majority of patients in the region. The patients were recruited for the study during periodical health checks-ups at these offices. A consecutive recruitment strategy with no randomization was used. A total of 1043 patients with clinically confirmed diabetes mellitus of different severity and stage were recruited from August 2008 to February 2009. Patients under 18 years of age and patients undergoing psychiatric treatment were excluded.
Informed consent and IRB Approval
After complete description of the study to the participants, written informed consent was obtained. This study has been approved by the IRB of the Trnava university hospital in Trnava, Slovakia and by the IRB of University of California, Berkeley, USA.
Procedures
Symptoms of depression were measured using the self-administered Patient Health Questionnaire 9 (PHQ9) [14]. The PHQ9 is a screening tool which contains nine straight-forward questions referring to the occurrence of mood swings during the previous two weeks with four options for an answer – ranging from never to nearly every day. An additional questionnaire specifically designed for the study was used in order to obtain demographic, behavioral, social and economic status information as well as information on the severity of diabetes and the occurrence of co-morbidities and complications. All Data collected using this questionnaire were self-reported. Both questionnaires were administered by trained junior researchers and graduate public health students.
Analysis
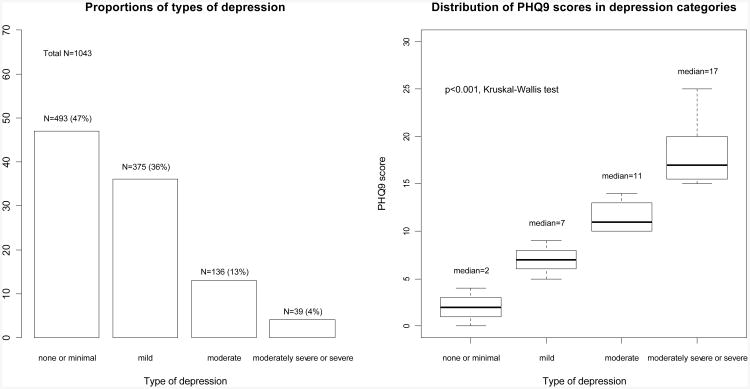
Patients were classified according to the obtained PHQ9 score into four groups: ‘none or minimal depression (NM)’ (PHQ9 scores of 0-4), ‘mild depression (Mi)’ (PHQ9 scores of 5-9, moderate depression (Mo)’ (PHQ9 scores of 10-14) and ‘moderately severe or severe depression (MSS)’ (PHQ9 scores of 15-27). In the univariate analyses a set of demographic, social and economic indicators and disease related indicators were created and differences were tested between the three depression groups. Chi-square test or Fisher's exact test (where counts were lower than 5) were used for comparisons of proportions. The Kruskal-Wallis test was used to test for differences in medians.
Subsequently a multivariate analysis was conducted. Ordinal logistic regression with a response variable of four categories was used. The response variable was coded in an ordinal form as follows: none or minimal depression was coded as ‘1’, mild depression was coded ‘2’, moderate depression was coded as ‘3’ and moderately severe and severe depression was coded as ‘4’. In order to show the relation to the response variable of demographic, social and economic predictors on one hand and disease related predictors on other hand two models were constructed. The first model included all demographic, social and economic predictors alone and subsequently adjusted for disease related predictors. The second model included disease related predictors, again first alone and then adjusted for demographic, social and economic predictors. Odds ratios with 95% confidence intervals are presented. Only variables showing statistically significant differences across the three compared groups in the univariate analysis were included in the models.
All statistical analyses were performed using the open source statistical package R [15]. A P value < 0.05 was considered statistically significant.
Results
The largest proportion of patients were in the NM (median PHQ9 scores 2 points (IQR 1-3), the smallest group were patients in the MSS group (median PHQ9 score of 17 points (IQR 15.5-20).
The available demographic, social and economic characteristics of patients with diabetes in our sample in the four depression symptoms severity groups are presented in table 1. Most of the patients were female, with the largest proportion of males in the NM group. The median age in the whole group was 65 years (IQR 57-72), the highest 69 years, (IQR 60-74) being in the MSS group. In the MSS group most patients were widowed, the majority of patients in the Mi, Mo and NM groups were married at the time of interview. The highest proportion of patients in the Mi, Mo and MSS groups had only elementary education. The proportion of university education was less than 10% in all three groups.
Table 1. Demographic, social and economic characteristics of patients by depression symptom severity.
| Depression severity | None or minimal (NM) | Mild (Mi) | Moderate (Mo) | Moderately severe or severe (MSS) | Total | P-value |
|---|---|---|---|---|---|---|
| N (% of total) | 493 (47%) | 375 (36%) | 136 (13%) | 39 (4%) | 1043 | |
| Age median (IQR) | 64 (56-71) | 66 (58-73) | 66 (59-73) | 69 (60-74) | 65 (57-72) | <0.01 |
| Gender N (% Male) | 223 (46%) | 140 (38%) | 34 (25%) | 12 (32%) | 409 (40%) | <0.01 |
| Marital Status N(%) | ||||||
| Divorced/separated | 25 (5%) | 19 (5%) | 10 (7%) | 2 (5%) | 56 (5%) | <0.05 |
| Married | 320 (65%) | 227 (61%) | 74 (54%) | 17 (44%) | 638 (61%) | |
| Never married | 33 (7%) | 17 (5%) | 7 (5%) | 2 (5%) | 59 (6%) | |
| Widowed | 113 (23%) | 110 (30%) | 45 (33%) | 18 (46%) | 286 (27%) | |
| Education N(%) | ||||||
| Elementary | 126 (26%) | 145 (39%) | 52 (39%) | 22 (56%) | 345 (33%) | <0.001 |
| Middle-graduation | 146 (30%) | 76 (20%) | 28 (21%) | 3 (8%) | 253 (24%) | |
| Middle-no graduation | 176 (36%) | 135 (36%) | 49 (36%) | 10 (26%) | 370 (36%) | |
| University | 41 (8%) | 19 (5%) | 6 (4%) | 4 (10%) | 70 (7%) | |
| Employment status N(%) | ||||||
| Employed | 126 (26%) | 71 (19%) | 16 (12%) | 2 (5%) | 215 (21%) | <0.01 |
| Retired | 356 (72%) | 298 (80%) | 119 (88%) | 36 (92%) | 809 (78%) | |
| Unemployed | 11 (2%) | 6 (2%) | 1 (1%) | 1 (3%) | 19 (1%) | |
| Monthly income N(%) | ||||||
| <500 | 58 (17%) | 65 (24%) | 26 (27%) | 8 (25%) | 157 (21%) | <0.001 |
| 500-800 | 200 (58%) | 162 (60%) | 61 (62%) | 22 (69%) | 445 (60%) | |
| >800 | 90 (26%) | 41 (15%) | 11 (11%) | 2 (6%) | 144 (19%) | |
| Number of persons in household N(%) | ||||||
| One | 96 (20%) | 76 (20%) | 40 (30%) | 13 (33%) | 225 (22%) | n.s. |
| Two | 181 (37%) | 148 (40%) | 50 (37%) | 13 (33%) | 392 (38%) | |
| Three | 95 (19%) | 64 (17%) | 18 (13%) | 7 (18%) | 184 (18%) | |
| Four | 61 (12%) | 44 (12%) | 12 (9%) | 3 (8%) | 120 (12%) | |
| Five or more | 58 (12%) | 41 (11%) | 15 (11%) | 3 (8%) | 117 (11%) | |
n.s.=not significant
Over 70% of patients in all groups were retired. The highest proportion of employed patients was in the NM group. Most of the patients had a monthly income of 500-800 EUR (over 58% in all groups). Patients with the highest recorded income were in the NM group. The proportion of patients with EUR income less than 500 was 27% or below in all groups. Most patients shared the household with one person (33% or more in all groups). The proportion of patients living alone was the highest in the MSS group (33%) and lowest in the NM group (20%).
Table 2 presents the comparison of diabetes severity indicators between the four depression symptoms severity groups. In the NM group, most patients (50%) were diagnosed for diabetes 0-5 years prior to the interview. The highest proportion of patients diagnosed 16 or more years prior to the interview was in the MSS group, the lowest in the NM group. Considerably more patients perceived their illness as very serious in the MSS group compared to other groups. Over 60% of patients overall perceived their illness as serious or very serious. Patients in the MSS groups had the highest proportion of insulin-dependence, highest number of comorbidities and specific complications (diabetic feet were present in 15% of patients and retinopathy in 21%) compared to the rest of our patients.
Table 2. Comparison of diabetes severity indicators by depression symptom severity.
| Depression severity | None or minimal (NM) | Mild (Mi) | Moderate (Mo) | Moderately severe or severe (MSS) | Total | P-value |
|---|---|---|---|---|---|---|
| N (% of total) | 493 (47%) | 375 (36%) | 136 (13%) | 39 (4%) | 1043 | |
| Years from diagnosis N(%) | ||||||
| 0-5 years | 248 (50%) | 141 (38%) | 48 (36%) | 8 (21%) | 445 (43%) | <0.001 |
| 6-10 years | 98 (20%) | 95 (26%) | 40 (30%) | 9 (23%) | 242 (23%) | |
| 11-15 years | 65 (13%) | 67 (18%) | 20 (15%) | 9 (23%) | 161 (16%) | |
| 16 + years | 81 (17%) | 70 (19%) | 26 (20%) | 13 (33%) | 190 (18%) | |
| Self-perceived severity of illness N(%) | ||||||
| Not at all serious | 54 (11%) | 11 (3%) | 6 (5%) | 0 (0%) | 71 (7%) | <0.001 |
| Somewhat serious | 162 (34%) | 131 (35%) | 32 (24%) | 6 (16%) | 331 (32%) | |
| Serious | 212 (44%) | 173 (47%) | 70 (52%) | 15 (41%) | 470 (46%) | |
| Very serious | 54 (11%) | 56 (15%) | 26 (19%) | 16 (43%) | 152 (15%) | |
| Number of comorbidities N(%) | ||||||
| None | 109 (22%) | 75 (20%) | 25 (18%) | 2 (5%) | 211 (20%) | <0.001 |
| One | 181 (37%) | 105 (28%) | 39 (29%) | 4 (10%) | 329 (32%) | |
| Two | 126 (26%) | 105 (28%) | 24 (18%) | 15 (39%) | 270 (26%) | |
| Three + | 77 (16%) | 90 (24%) | 48 (35%) | 18 (46%) | 233 (22%) | |
| Diabetic foot N (%) | 7 (1%) | 10 (3%) | 5 (4%) | 6 (15%) | 28 (3%) | <0.001 |
| Retinopathy N (%) | 35 (7%) | 33 (9%) | 14 (10%) | 8 (21%) | 90 (9%) | <0.05 |
| Insulin dependence N (%) | 99 (20%) | 88 (24%) | 42 (31%) | 15 (39%) | 244 (23%) | <0.01 |
| Dependence on help N (%) | 6 (1 %) | 11 (3%) | 11 (8%) | 3 (8%) | 31 (3%) | <0.01 |
The two multivariate models are showed in tables 3 and 4. In the first model demographic, social and economic predictors (table 3) are presented. Education and self-perceived health status were significantly associated with worsening severity of depression symptoms. Their effect has been shown to be significant even after entering disease-related predictors into the model for adjustment. Table 4 presents the model with disease related predictors. In this model years from diagnosis and a high number of comorbidities had a significant effect on the severity of depression symptoms. However, after adjusting for the effect of demographic, social and economic predictors, this effect was lost.
Table 3. Results of the multivariate analysis of influence of demographic, social and economic factors on the severity of depression symptoms in patients with diabetes.
| Dependent variable (predictor) | Un-adjusted model with demographical, social and economic predictors | Adjusted model with demographical, social and economic predictors* | ||
|---|---|---|---|---|
| OR (CI 95%) | p-value | OR (CI 95%) | p-value | |
| Education | ||||
| Elementary | 1 (reference) | - | 1 (reference) | - |
| Middle – no graduation | 0.78 (0.54-1.11) | 0.178 | 0.76 (0.52-1.09) | 0.141 |
| Middle - graduation | 0.51 (0.32-0.78) | <0.05 | 0.52 (0.33-0.81) | <0.05 |
| University | 0.76 (0.36-1.58) | 0.473 | 0.83 (0.39-1.75) | 0.632 |
| Income | ||||
| <500 | 1 (reference) 0.2358 | - | 1 (reference) | - |
| 500-800 | 0.79 (0.53-1.14) | 0.205 | 0.81 (0.56-1.17) | 0.252 |
| >800 | 0.6 (0.33-1.11) | 0.102 | 0.65 (0.34-1.21) | 0.176 |
| Perceived health status | ||||
| No at all serious | 1 (reference) | - | 1 (reference) | - |
| Somewhat serious | 3.43 (1.72-7.26) | <0.01 | 3.31 (1.66-7.04) | <0.01 |
| Serious | 3.87 (1.97-8.08) | <0.01 | 3.36 (1.69-7.12) | <0.01 |
| Very serious | 6.62 (3.18-14.61) | <0.001 | 5.33 (2.47-12.12) | <0.001 |
| Marital status | ||||
| Married | 1 (reference) | - | 1 (reference) | - |
| Never married | 0.94 (0.47-1.86) | 0.881 | 0.79 (0.38-1.6) | 0.529 |
| Divorced | 1.21 (0.62-2.31) | 0.571 | 1.05 (0.53-2.06) | 0.878 |
| Widowed | 1.2 (0.83-1.74) | 0.327 | 1.13 (0.77-1.64) | 0.529 |
| Employment | ||||
| Employed | 1 (reference) | - | 1 (reference) | - |
| Unemployed | 4.52 (0.54-37.4) | 0.144 | 5.11 (0.64-46.2) | 0.127 |
| Retired | 1.58 (0.92-2.72) | 0.093 | 1.61 (0.92-2.81) | 0.095 |
| Age | 0.99 (0.98-1.01) | 0.531 | 0.99 (0.97-1.01) | 0.429 |
| Gender Female (vs. Male) | 1.16 (0.84-1.63) | 0.365 | 1.22 (0.87-1.71) | 0.251 |
Odds ratios (OR) adjusted for: number of years from diagnosis, number of comorbidities, presence of diabetes foot, presence of retinopathy, presence of insulin dependence
Table 4. Results of the multivariate analysis of influence of disease related factors on the severity of depression symptoms in patients with diabetes.
| Dependent variable (predictor) | Un-adjusted model with diabetes related predictors | Adjusted model with diabetes related predictors* | ||
|---|---|---|---|---|
| OR (CI 95%) | p-value | OR (CI 95%) | p-value | |
| Years from diagnosis | ||||
| 0-5 | 1 (reference) | - | 1 (reference) | - |
| 6-10 | 1.67 (1.23-2.27) | <0.01 | 1.35 (0.91-1.99) | 0.139 |
| 11-15 | 1.55 (1.08-2.21) | <0.05 | 1.25 (0.81-1.95) | 0.319 |
| 16+ | 1.42 (1.01-2.03) | <0.05 | 1.4 (0.89-2.19) | 0.148 |
| Number of comorbidities | ||||
| None | 1 (reference) 0.2358 | - | 1 (reference) | - |
| One | 0.86 (0.61-1.2) | 0.366 | 0.77 (0.49-1.24) | 0.291 |
| Two | 1.06 (0.74-1.51) | 0.736 | 0.91 (0.55-1.49) | 0.722 |
| Three or more | 1.96 (1.35-2.87) | <0.01 | 1.45 (0.86-2.5) | 0.162 |
| Diabetes foot present (vs. not present) | 1.91 (0.91-4.06) | 0.094 | 1.15 (0.51-2.61) | 0.729 |
| Retinopathy foot present (vs. not present) | 1.04 (0.67-1.06) | 0.848 | 0.86 (0.51-1.42) | 0.549 |
| Insulin dependence (vs. non-dependence) | 0.87 (0.64-1.17) | 0.361 | 1.09 (0.74-1.63) | 0.641 |
Odds ratios (OR) adjusted for: education, income, self-perceived health status, marital status, employment, age and gender
Discussion
Our study focused on analyzing the prevalence and predictors of depression amongst patients with diabetes. We have successfully recruited 1043 patients with clinically confirmed diagnosis. The criterion of exclusion of patients undergoing psychiatric treatment was included in the study protocol to eliminate the modification of the depression screening results by such treatment. However, in reality less than 5 patients were excluded based on this criterion and the impact on our findings is not relevant. The Patient Health Questionnaire 9 (PHQ9) was used to screen depression. A systematic review found that out of the over 25 tools they identified the Beck Depression Inventory and the Centre for Epidemiologic Studies Depression Scale were the most frequently used [16]. The PHQ9 has been used in 20 published primary, secondary or tertiary care or community studies of depression among diabetes patients since it was first introduced [14] and it has been proven a valid tool for rapid screening of depression symptoms with adequate sensitivity and specificity on different cut-off points used [17].
We have divided our sample based on the PHQ9 score into four depression severity groups. We have preferred this approach over dividing our patients in a binary manner into a ‘depression group’ and ‘non-depression group’. Although a binary approach has been used in a number of similar studies [2] our approach offers a more sensitive way of a variety of factors to prevalence of depression symptoms of different severity.
We have found that 4% of our patients had severe or moderately severe depression symptoms, 36% moderate moderate, 13% mild and 47% of our subjects had none or minimal depression symptoms. An extensive systematic review found an aggregated estimate of 11% of major depression and 31% of elevated depression symptoms amongst all patients with diabetes studied [2]. Three studies found prevalence of depression similar to our findings, specifically 3,8% [18], 6,1% [19] and 5,4% [20], respectively. Our study did not include a control group (patients without diagnosed diabetes). A study of the general population of Slovakia found depressive symptoms in 23% of their subjects. Out of this number, a very severe degree of intensity of depression was present in 2.8% of cases, a severe degree of intensity in 5.3%, and a moderate degree in 14.6% of subjects [21].
The relatively small proportion of patients with moderately severe or severe depression symptoms as compared to similar studies and the prevalence in the general population of Slovakia might be due to the design of our study. We assume that our subject recruitment procedure might have caused a failure to recruit a part of severely depressed patients with diabetes from our population. There are two reasons for this assumption. Firstly, the most severe patients due to immobility or severe illness might have not been able to visit the outpatient offices where the recruitment for the study was conducted. Such patients might be treated by a specialist at home or brought into the outpatient office at specific appointments. Secondly, a part of patients with more severe diabetes from our study population might be treated in a higher end center in the nearby capital of Slovakia and could not be included in our study. The higher prevalence of depression in the general population might be also due to different study designs and methods used in both studies.
Demographic, social and economic factors and depression symptoms
The median age of our patients was 65 years, with a proportion of male patients being 40%. A significant increase of age medians and of a proportion of female patients is apparent along with the increasing severity of depression symptoms. Although reviews and meta-analyses of studies on depression amongst patients with diabetes found mean ages in the majority of studies over 55 years, also studies with mean ages as low as 20 years were identified [4,2]. The correlation of increasing age and female gender with the likelihood of severe depression symptoms in patients with diabetes as was found in our study is well documented and confirmed by a number of studies [8,12,22,23]. Decreasing proportion of married patients and increasing proportions of widowed patients are significantly associated with increasing severity of depression symptoms. These findings correspond with findings of other studies [12,23]. However, we did not find a significant effect of the number of persons living in the household with the patients in our group. Increasing severity of depression symptoms in our study was also significantly related to education level – severity increased with an increasing proportion of patients with elementary education which is in compliance with other studies [11,12,23]. Our study also confirms previous findings that the level of income significantly relates to severity of depression symptoms amongst patients with diabetes [24,25]. In our multivariate analysis, education and self-perceived severity of illness were the only two independent predictors which showed a significant effect on the severity of depression symptoms, even after adjusting for the effect of disease-related factors.
Disease related factors and depression symptoms
We have used a number of disease related indicators to determine the clinical severity of diabetes amongst the patients in our study (table 2). All of them demonstrated a significant relationship with the severity of depression symptoms identified by the PHQ9. A strong effect of the number of years from diagnosis was found. One third of patients in the MSS group were diagnosed 16 or more years prior to the interview in contrast with 17% in the NM group. In our study, the time-span of illness had a strong effect on the occurrence of depression symptoms amongst patients with diabetes. This contradicts the findings of a number of studies which found no such effect [26,22,23]. However, another study found an increasing likelihood of meeting the criteria for mild depression with the increasing duration of diabetes [12].
Self-perceived seriousness of illness was also strongly associated with increasing severity of depression symptoms. Over 80% of patients in the MSS group perceived their status as serious or very serious in contrast with 55% in the NM group. To some extent the self-perception of severity of illness might be biased toward more serious by the presence of more severe depression symptoms per se. This might be true especially in case of perceiving the illness as very serious in the MSS group where the proportion of such patients was substantially higher (43%) than in the rest of the patients (11 to 19% in NM, Mi and Mo groups). Although, based on our data we are not able to investigate to what extent can the self-perception of illness as very serious be attributable to the presence of depression per se, caution should be used when interpreting the relationship of these two factors and the direction of this relationship especially.
Diabetes comorbidities have been associated with depression amongst patients with diabetes in a number of studies [3,27], and our study confirms these findings. In our study, diabetic feet and retinopathy were significantly more prevalent in the MSS group as compared to NM, Mi and Mo groups and an increasing trend of prevalence of these comorbidities is apparent along with the increasing severity of depression symptoms. The proportion of patients with insulin-dependent diabetes also increased with the increasing severity of depression symptoms – a fact supported by another study in this field [12]. None of the disease related factors had an independent relationship to the severity of depression symptoms after adjusting for demographic, social and economic factors in the multivariate analysis.
Limitations to the study
Our study included both type I and type II patients with diabetes. Although depression is reportedly present in a similar proportion in both types of diabetes [2] the two types of the disease have different etiology, age of onset, different likelihood of comorbidities and in some cases depression might precede type II diabetes [5]. The unknown ratio of both types of diabetes in our sample made it impossible to control for these factors and this should be taken into account when looking at our results.
The aforementioned discussion of possibly missing a part of severe patients with diabetes in our sample may skew our patients towards more mild diabetes, and thus supposedly milder depression symptoms. Furthermore, no control group has been recruited and therefore we had no reference of the prevalence of depression in the general population. As a surrogate, findings of a study from the general population [21] are used as reference values.
The assessment of depression symptoms was done using a screening questionnaire and was not conducted by a mental health professional. The results of the screening do not mean that the patients actually did or did not suffer from clinical depression.
No randomization was used in the sampling process and the median of the age in the sample was 65 years (which means that the sample could be considered as consisting of mostly geriatric patients). These two facts decrease the external validity of our findings.
Conclusions
Out of all analyzed factors, only lower level of education, and the self-perceived seriousness of the diabetes by the patient are factors independently associated with increasing severity of depression symptoms amongst patients with diabetes in our study. Thus, our results suggest that socio-economic and psychological factors may have a more important role than disease related factors in developing depression symptoms in patients with diabetes in our population. Further studies into the topic are needed to overcome the limitations of the presented results and to gain further clues on this relatively under-studied topic in Slovakia and throughout the Central European region. The findings of this study should be considered by mental health service providers and public health authorities to raise awareness about this important issue. Screening or treatment plans for such patients as part of an overall diabetes care management system [28] may help to tackle the problem.
Figure 1. Proportions of patients in three depression symptom severity groups and distribution of PHQ9 scores within the three groups in the study sample.
Acknowledgments
The data for this study has been collected under the project “The Impact of Depression on Diabetes Patients: Prevalence and Costs” conducted by the Center for Health Policy and Public Health, Institute for Social Research, Faculty of Political Administrative and Communication Sciences, Babes-Bolyai University, Cluj-Napoca, Romania and the Trnava University, Faculty of Health Care and Social Work, Department of Public Health, Trnava, Slovakia. Funding for this project was provided by Fogarty International Center (grant# NIH 014605-010). We are grateful to PhD and graduate students at the Faculty of Health Care and Social Work of the Trnava University who helped with data collection and patient recruitment.
Footnotes
Conflicts of interest: none declared.
References
- 1.WHO. The Global Burden of Disease, 2004 update 2008 [Google Scholar]
- 2.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24(6):1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 3.de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. 2001;63(4):619–630. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Ali S, Stone MA, Peters JL, Davies MJ, Khunti K. The prevalence of co-morbid depression in adults with Type 2 diabetes: a systematic review and meta-analysis. Diabet Med. 2006;23(11):1165–1173. doi: 10.1111/j.1464-5491.2006.01943.x. DME1943 [pii]10.1111/j.1464-5491.2006.01943.x. [DOI] [PubMed] [Google Scholar]
- 5.Barnard KD, Skinner TC, Peveler R. The prevalence of co-morbid depression in adults with Type 1 diabetes: systematic literature review. Diabet Med. 2006;23(4):445–448. doi: 10.1111/j.1464-5491.2006.01814.x. DME1814 [pii]10.1111/j.1464-5491.2006.01814.x. [DOI] [PubMed] [Google Scholar]
- 6.Mary de Groot MK, Doyle Todd, Merrill Jennifer, McGlynn Mark, Shubrook Jay, Schwartz Frank. Depression Among Adults With Diabetes: Prevalence, Impact, and Treatment Options. Diabetes Spectrum. 2010;23 doi: 10.2337/diaspect.23.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pibernik-Okanovic M, Begic D, Peros K, Szabo S, Metelko Z. Psychosocial factors contributing to persistent depressive symptoms in type 2 diabetic patients: a Croatian survey from the European Depression in Diabetes Research Consortium. J Diabetes Complications. 2008;22(4):246–253. doi: 10.1016/j.jdiacomp.2007.03.002. S1056-8727(07)00030-X [pii]10.1016/j.jdiacomp.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 8.Eaton WW. Epidemiologic evidence on the comorbidity of depression and diabetes. J Psychosom Res. 2002;53(4):903–906. doi: 10.1016/s0022-3999(02)00302-1. S0022399902003021 [pii] [DOI] [PubMed] [Google Scholar]
- 9.Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care. 2008;31(12):2383–2390. doi: 10.2337/dc08-0985. 31/12/2383 [pii]10.2337/dc08-0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scheffler RM, Potucek M, editors. Mental Health Care Reform in the Czech and Slovak Republics, 1989 to Present. Karolinum Press; Prague: 2008. [Google Scholar]
- 11.Engum A, Mykletun A, Midthjell K, Holen A, Dahl AA. Depression and diabetes: a large population-based study of sociodemographic, lifestyle, and clinical factors associated with depression in type 1 and type 2 diabetes. Diabetes Care. 2005;28(8):1904–1909. doi: 10.2337/diacare.28.8.1904. 28/8/1904 [pii] [DOI] [PubMed] [Google Scholar]
- 12.Katon W, von Korff M, Ciechanowski P, Russo J, Lin E, Simon G, Ludman E, Walker E, Bush T, Young B. Behavioral and clinical factors associated with depression among individuals with diabetes. Diabetes Care. 2004;27(4):914–920. doi: 10.2337/diacare.27.4.914. [DOI] [PubMed] [Google Scholar]
- 13.Marmot M, Wilkinson RG, editors. Social Determinants of Health. Oxforf University Press; London: 1999. [Google Scholar]
- 14.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders Patient Health Questionnaire JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. joc90770 [pii] [DOI] [PubMed] [Google Scholar]
- 15.R-Development-Core-Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2010. [Google Scholar]
- 16.Roy T, Lloyd CE, Pouwer F, Holt RI, Sartorius N. Screening tools used for measuring depression among people with Type 1 and Type 2 diabetes: a systematic review. Diabet Med. 2012;29(2):164–175. doi: 10.1111/j.1464-5491.2011.03401.x. [DOI] [PubMed] [Google Scholar]
- 17.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. jgi01114 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang JMK, Lee DJ. Health status of diabetic Mexican Americans: results from the Hispanic HANES. Ethn Dis. 1991;3(1):273–279. [PubMed] [Google Scholar]
- 19.Eaton WW, Armenian H, Gallo J, Pratt L, Ford DE. Depression and risk for onset of type II diabetes. A prospective population-based study. Diabetes Care. 1996;19(10):1097–1102. doi: 10.2337/diacare.19.10.1097. [DOI] [PubMed] [Google Scholar]
- 20.Lee PWH LK, Lieh-Mak F, Chung KF, So T. Emotional maladjustment, physical malaise and diabetic control in young Chinese patients with diabetes. Psychol Health Med. 1996;(1):119–127. [Google Scholar]
- 21.Heretik As, Heretik A, jr, Novotny V, Pecenak J, Ritomsky A. EPID Epidemiologia depresii na Slovensku. Psychoprof; Nove Zamky: 2003. [Google Scholar]
- 22.Manarte LF, Dias S, Gois C, Boavida JM. Independent factors associated with depression in type 1 diabetes mellitus. Acta Diabetol. 2010;47(3):201–207. doi: 10.1007/s00592-009-0110-y. [DOI] [PubMed] [Google Scholar]
- 23.Tellez-Zenteno JF, Cardiel MH. Risk factors associated with depression in patients with type 2 diabetes mellitus. Arch Med Res. 2002;33(1):53–60. doi: 10.1016/s0188-4409(01)00349-6. S0188-4409(01)00349-6 [pii] [DOI] [PubMed] [Google Scholar]
- 24.Dismuke CE, Egede LE. Association between major depression, depressive symptoms and personal income in US adults with diabetes. Gen Hosp Psychiatry. 2010;32(5):484–491. doi: 10.1016/j.genhosppsych.2010.06.004. S0163-8343(10)00133-7 [pii]10.1016/j.genhosppsych.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 25.Waitzfelder B, Gerzoff RB, Karter AJ, Crystal S, Bair MJ, Ettner SL, Brown AF, Subramanian U, Lu SE, Marrero D, Herman WH, Selby JV, Dudley RA. Correlates of depression among people with diabetes: The Translating Research Into Action for Diabetes (TRIAD) study. Prim Care Diabetes. 2010;4(4):215–222. doi: 10.1016/j.pcd.2010.07.002. S1751-9918(10)00092-6 [pii]10.1016/j.pcd.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Katon W, Russo J, Lin EH, Heckbert SR, Ciechanowski P, Ludman EJ, Von Korff M. Depression and diabetes: factors associated with major depression at five-year follow-up. Psychosomatics. 2009;50(6):570–579. doi: 10.1176/appi.psy.50.6.570. 50/6/570 [pii]10.1176/appi.psy.50.6.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin EH, Rutter CM, Katon W, Heckbert SR, Ciechanowski P, Oliver MM, Ludman EJ, Young BA, Williams LH, McCulloch DK, Von Korff M. Depression and advanced complications of diabetes: a prospective cohort study. Diabetes Care. 2010;33(2):264–269. doi: 10.2337/dc09-1068. dc09-1068 [pii]10.2337/dc09-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Mullane M, McHugh S, Bradley C. Informing the Development of a National Diabetes Register in Ireland: A Literature Review of the Impact of Patient Registration on Diabetes Care. Informatics in Primary Care. 2010;18 doi: 10.14236/jhi.v18i3.768. [DOI] [PubMed] [Google Scholar]