Abstract
Primary objective
To examine the hospitalization costs and discharge outcomes of U.S. children with TBI and to evaluate a severity measure, the predictive mortality likelihood level.
Research design
Data from the 2006 Healthcare Cost and Utilization Project Kids’ Inpatient Database (KID) were used to report the national estimates and characteristics of TBI-associated hospitalizations among U.S. children ≤ 20 years of age. Percentage of children with TBI caused by motor vehicle crashes (MVC) and falls was calculated according to the predictive mortality likelihood levels (PMLL), death in hospital, and discharge into long-term rehabilitation facilities. Associations with the PMLL, discharge outcomes, and average hospital charges were examined.
Results
In 2006, there were an estimated 58,900 TBI-associated hospitalizations among U.S. children, accounting for $2.56 billion in hospital charges. MVCs caused 38.9% and falls caused 21.2% of TBI hospitalizations. The PMLL was strongly associated with TBI type, length of hospital stay, hospital charges, and discharge disposition. About 4% of children with fall or MVC related TBIs died in hospital and 9% were discharged into long-term facilities.
Conclusion
The PMLL may provide a useful tool to assess characteristics and treatment outcomes of hospitalized TBI children but more research is still needed.
Keywords: children, costs, outcome, traumatic brain injury, predictive mortality likelihood level
Introduction
Traumatic brain injury (TBI) is the leading cause of disability and death among children in the United States [1]. Each year, there are an estimated 475,000 TBIs occurring among children aged 0–14 [2]. This estimate includes 2,685 deaths, and an estimated 37,000 hospitalizations, and 435,000 emergency department visits. It is estimated that at the beginning of 2005, there were 145,000 American children, under 20 years of age, living with long-term disability as a result of TBI [3].
TBI can have a more devastating impact on a child’s brain compared with the same injury on an adult’s brain [4]. Many studies have shown that the full impact of a traumatic injury on a child’s brain only becomes apparent over time as the brain fails to mature in step with the child’s physical growth and development [5–7]. While the vast majority of children hospitalized with TBI are discharged directly back to their homes, a significant proportion of these children will face long-term, sometimes lifelong, adverse consequences in terms of medical, physical, cognitive, psychosocial, or neurobehavioral functions [8–11]. Such delayed or latent effects can create a lifetime of challenges for both the children suffering from TBI and their families, as well as schools and communities [12,13].
Previous studies have examined the leading causes, characteristics, and health care utilization and insurance coverage of TBI among U.S. children [1,14–18]. Although previous research studied TBI treatment patterns and outcomes among adults according to severity and mechanism of injury,[19] little has been done to explore associations between measures of TBI severity and medical costs among U.S. children. In addition, most studies did not examine hospitalized children who were discharged into rehabilitation facilities despite their importance.
In this study, we used the most recent Kid’s Inpatient Database (KID) to examine external cause, age patterns, severity measures, discharge outcomes, and hospital-based charges among U.S. children who were hospitalized for TBI. Of special interest were hospital charges by TBI severity and the characteristics of children with TBI who were discharged into long-term rehabilitation facilities. Because motor vehicle crashes and falls are top two leading causes of TBI in the U.S., our analyses focused on hospitalized TBI that were caused by these two causes.
METHODS
Data Source
In this study, we conducted a retrospective analysis of hospitalizations in the U.S. from January 1, 2006, to December 31, 2006, using data from the Kids’ Inpatient Database (KID) [20]. KID is part of the Healthcare Cost and Utilization Project (HCUP), sponsored by the Agency for Healthcare Research and Quality (AHRQ).
KID is a dataset of hospital use, outcomes, and financial information. It is designed to study the use of hospital services by U.S. children. KID data are selected from a sample of discharges from community, non-rehabilitation hospitals (hospitals with an average stay of less than 30 days) in states participating in HCUP. Pediatric discharges are defined as all discharges of patients who are 20 years of age or younger at the time of admission. Inpatient stay records in the KID database include clinical and resource use information typically available from discharge abstracts. Weights and sampling variables are provided for calculating national estimates.
The KID is available every three years and was first collected in 1997. The sampling frame in 2006 includes pediatric discharges from 3,739 non-rehabilitation community hospitals in 38 participating HCUP states. The 2006 KID database includes a sample of 3,131,324 pediatric discharges from all hospitals in the sampling frame.
Identification of TBI Cases
In this study, we used CDC TBI surveillance case definitions and methods to define TBI [21]. TBI-associated hospitalizations were identified from the diagnosis code using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes in the KID dataset. TBI-associated hospitalizations were included if one or more of the 15 diagnosis fields contained a TBI ICD-9-CM diagnosis code that was recommended by the CDC [21]. We used the Barell Injury Diagnosis Matrix to define the type of TBI [22]. Injuries were labeled as Type 1 TBI if there was recorded evidence of an intracranial injury, a moderate or prolonged loss of consciousness (LOC), Shaken Infant Syndrome (SIS), or injury to the optic nerve pathway. Type 2 TBIs included injuries with no recorded evidence of intracranial injury, LOC for less than one hour, LOC for an unknown duration, or an unspecified level of consciousness. Type 3 TBIs included injuries with no evidence of intracranial injury and no LOC.
Classification of TBI severity
For acute severity of injuries, hospitalized TBI children also were evaluated based on a predictive mortality likelihood level (PMLL). The PMLL is one of four disease staging measures that was developed by the Medstat Company [23]. The other three include a disease stage measure and two other predictive scales, one for length of hospital stay and one for total charges. These four disease staging measures were selected by the Agency for Healthcare Research and Quality as measures of disease severity, starting with 2003 KID, as a means to group patients according to expected level of resources need during hospitalization and/or expected outcome of hospitalization. The PMLL had five mortality levels: 0- extremely low (mortality probability less than 0.0001 so excluded from percentile calculation), 1- very low (< 5% of patients), 2- low (2–25% of patients), 3- medium (25–75% of patients), 4- high (75–95% of patients), and 5- very high (> 95% of patients). To avoid small sample size, we combined 0 and 1 mortality levels together when the PMLL was analyzed across gender, age groups, TBI types, length of stay, discharge dispositions, and average hospital charges for treating TBI children.
Outcomes of Hospitalization
In our study, we studied the discharge outcomes and hospital-based charges. We analyzed length of stay and discharge status according to PMLL. We were particularly interested in those children who died in the hospital and those who were discharged into a long-term rehabilitation facility.
E-codes
The principal ICD-9-CM E-code (first E-code) in the KID dataset was used to determine the leading external cause, as recommended by the CDC [24]. E-codes were categorized according to the recommended frameworks for presenting injury data [25].
Statistical Analysis
Statistical analysis was performed using SAS software (version 9.1; SAS Institute, Cary, NC) [26]. The KID database provides discharge weights, stratum, and cluster information to account for the complex sampling. To calculate national estimates, we used SAS survey procedures. National weighted frequencies were estimated using the SURVEYFREQ procedure and national hospital charges for the treatment of TBI were calculated using the SURVEYMEANS procedure. These two procedures use the Taylor expansion method to estimate sampling errors of estimators based on complex sample designs.
We first ranked external causes of TBI among U.S. children by the total number of estimated TBIs with 95% confidence intervals (CIs), in which we found that more than 60% of TBIs were caused by motor vehicle crashes and falls. National estimates of hospital charges for treating TBI and the associated 95% CIs were also calculated according to external causes of TBI. Then we conducted in-depth statistical analysis of TBI caused by motor vehicle crashes and falls. Rates of TBI-associated hospitalizations per 100,000 children that were caused by motor vehicle crashes and falls were generated according to age, gender, and external causes (motor vehicle crashes vs. falls) with publicly available 2006 U.S. census denominator data [27]. Detailed external causes (ICD-9-CM E-codes) were analyzed separately for TBIs caused by falls among infants <1 year of age and motor vehicle crashes among adolescents 16–20 years of age. We did this analysis, because we found that infants < 1 year of age had the highest rate of TBI-associated hospitalization caused by falls, while individuals 16 years of age and older had the highest rates of TBI-associated hospitalization caused by motor vehicle crashes.
TBI type, discharge status, length of hospital stay (days), and the PMLL were analyzed separately for TBI caused by motor vehicle crashes and falls. Furthermore, we calculated percentage (%) of TBI hospitalizations according to PMLL, death in hospital, and discharge into long-term rehabilitation facilities. The 95% CIs for the percentage were calculated to determine whether the differences between groups of children with TBI were statistically significant. If 95% CIs for the two comparison groups did not overlap, the difference was considered statistically significant. Finally, we calculated the average hospital charges for treating TBI children and evaluated the association between the PMLL and average hospital charges.
RESULTS
Based on KID data, there were an estimated 58,900 (95% CI: 53,819 – 63,982) TBI-associated hospital discharges of U.S. children 20 years of age or younger in 2006. The top five external causes were motor vehicle crashes, falls, assaults, other transport (not motor vehicle), and struck by/against objects (table I). Motor vehicle crashes caused 38.9% and falls caused 21.2% of the total TBI-associated hospitalizations. The estimated total hospital charges for the treatment of all TBI were about 2.56 billion U.S. dollars, and TBI caused by motor vehicle crashes accounted for more than half of the total hospital charges (53.0%).
Table I.
Actual sample and national estimates of traumatic brain injury-associated hospitalizations among U.S. children ≤ 20 years of age according to external cause of injury, 2006
| External Cause of Injury | Actual Sample n | National Estimate n (95% CI) | Rank | National Estimated Hospital Charges $ (95% CI) |
|---|---|---|---|---|
| Total Hospitalizations | 36,757 | 58,901 (53,819–63,982) | $2,563,075,142 ($2,254,219,870–$2,871,930,413) | |
| Unintentional | ||||
| Motor vehicle crashes (MVC) | 14,391 | 22,913 (20,534–25,292) | 1 | $1,358,437,711 ($1,169,514,567–$1,547,360,854) |
| Falls | 7,620 | 12,505 (11,291–13,718) | 2 | $245,900,481 ($213,109,161–$278,691,800) |
| Non-MVC transport incidents | 2,247 | 3,616 (3,199–4,033) | 4 | $133,231,284 ($110,700,546–$155,762,021) |
| Struck by/against objects | 2,145 | 3,513 (3,184–3,841) | 5 | $66,646,045 ($57792558–$75,499,531) |
| Non-MVC pedal cyclist incidents | 1,105 | 1,791 (1,569–2,012) | 6 | $35,966,002 ($29,780,908–$42,151,095) |
| Intentional | ||||
| Assault | 3,336 | 5,341 (4,818–5,863) | 3 | $231,297,752 ($197,292,163–$265,303,340) |
| Self-inflicted | 181 | 280 (229–331) | 7 | $17,253,387 ($12,019,551–$22,487,222) |
| Other (including unspecified) | 5,732 | 8,943 (7,618–10,269) | # | $474,342,481 ($395,791,384–$552,893,577) |
Data source: 2006 KID.
Excluded from ranking because of missing E-codes.
The top two external causes of pediatric TBI (motor vehicle crashes and falls) showed dramatic distributional differences by age group (figure I). The average rates of TBI hospitalizations caused by falls were 18.3 per 100,000 children for males and 9.6 per 100,000 children for females. Among infants < 1 year of age, this rate was significantly higher (84.4 per 100,000 for males and 61.1 per 100,000 for females). In comparison, overall rates of hospitalized TBIs caused by motor vehicle crashes were 32.9 per 100,000 children for males and 19.5 per 100,000 children for females. Rates of TBI hospitalizations caused by motor vehicle crashes increased significantly after 15 years of age regardless of gender, peaking at 19 years of age (111.2 per 100,000 children for males and 56.2 per 100,000 for females).
Figure I.
Rate per 100,000 population of traumatic brain injury-associated hospitalizations caused by motor vehicle crashes (MVC) and falls by age and gender among U.S. children, KID 2006
Detailed analysis of external cause of injury for TBIs caused by motor vehicle crashes among adolescents 16–20 years of age and falls among children <1 year of age is shown in table II. Almost half of TBIs caused by motor vehicle crashes among children 16–20 years of age occurred when the child was the passenger (48.3%). Just over 30% of TBI hospitalizations occurred when the occupant was the driver. The remaining 20% involved motorcycles, bikes, pedestrian, and other/unspecified MVC. Of TBIs caused by falls among infants, falls from a bed (22.8%), falls on stairs (8.9%), falls from other furniture (8.7%), and falls from a chair (5.7%) were the leading causes.
Table II.
Detailed E-codes (external causes) of traumatic brain injury-associated hospitalizations caused by motor vehicle crashes (among 16–20 years old ) and falls (among < 1 year-olds) among U.S. children, 2006
| Actual Sample n | National Estimate n | Weighted % (95%CI) Ψ | |
|---|---|---|---|
| Motor Vehicle Crashes (16–20 Years Old) | 9,108 | 14,361 | 100.0 |
| E810–E819(.0–.1) Occupant | 7,230 | 11,398 | 79.4 (78.2–80.5) |
| E810–E819(.0) Driver | 2,828 | 4,459 | 31.1 (30.0–32.1) |
| E810–E819(.1) Passenger | 4,402 | 6,939 | 48.3 (47.1–49.5) |
| E810–E819(.2–.3) Motorcyclist | 642 | 1,001 | 7.0 (6.3–7.6) |
| E810–E819(.6) Pedal cyclist | 192 | 303 | 2.1 (1.8–2.4) |
| E810–E819(.7) Pedestrian | 638 | 1,014 | 7.1 (6.4–7.7) |
| E810–819(.9) Other and unspecified | 406 | 645 | 4.5 (4.0–5.0) |
| Falls (Among < 1 Year-Olds) | 1,815 | 3,030 | 100.0 |
| E880 Fall on or from stairs or steps | 159 | 270 | 8.9 (7.3–10.5) |
| E882 Fall from or out of building or other structure | ≤10 | ≤10 | |
| E884 Other fall from one level to another | 1,383 | 2,308 | 76.2 (73.9–78.4) |
| E884(.0) Fall from playground equipment | ≤10 | ≤10 | |
| E884(.2) Fall from chair | 104 | 173 | 5.7 (4.5–6.9) |
| E884(.4) Fall from bed | 413 | 692 | 22.8 (20.4–25.3) |
| E884(.5) Fall from other furniture | 155 | 263 | 8.7 (7.5–9.9) |
| E884(.9) Other fall from one level to another | 706 | 1,171 | 38.6 (35.6–41.7) |
| E885 Fall on same level from slipping, tripping, or stumbling | 49 | 81 | 2.7 (1.9–3.5) |
| E886 Fall on same level from collision, pushing, or shoving | ≤10 | ≤10 | |
| E888 Other and unspecified fall | 218 | 361 | 11.9 (10.2–13.7) |
Data source: 2006 KID.
According to the National Center for Health Statistics, estimates based on a sample of ≤ 30 cases have low reliability.
TBI hospitalizations as a result of MVC as compared with falls resulted in more severe TBI injuries by all measures shown in table III: TBI type, discharge status, LOS, and the PMLL. While Type 1 TBIs were similar proportions of the TBI hospitalizations for both MVC (48.3%) and falls (49.3%), Type 2 TBIs were a larger proportion of the hospitalizations from MVC (47.9%) when compared with falls related TBIs (32.9%). The least severe Type 3 TBIs were seen more often in falls. Less than 16% of falls-related TBI hospitalizations had LOS longer than 3 days. Just over 43% of MVC TBI hospitalizations had LOS longer than 3 days. The very high PMLL category accounted for 9.7% of the MVC TBI hospitalizations. This very high level accounted for 1.9% of the falls-related TBI hospitalizations. For both MVC and falls, the majority, roughly ¾ of the TBIs were classified as medium or high in terms of the PMLL. Discharge status was routine for 94% of falls TBI hospitalizations, but this was true of only 75.8% of MVC TBI hospitalizations. Instead, discharge to long-term rehabilitation facilities and discharge with a need for home health care were larger proportions of the MVC TBI related hospitalizations. Fatalities were also a larger proportion of the MVC hospitalizations (5.4%), while only 0.8% of falls-related TBI hospitalizations resulted in death.
Table III.
Characteristics of traumatic brain injury-associated hospitalizations caused by motor vehicle crashes (MVC) and falls in U.S. children
| Characteristics | MVC
|
Falls
|
||||
|---|---|---|---|---|---|---|
| Actual Sample n | National Estimate nΨ | Weighted % (95% CI) Ψ | Actual Sample n | National Estimate nΨ | Weighted % (95% CI) Ψ | |
| TBI Type | ||||||
| Type 1 TBI | 6,965 | 11,077 | 48.3 (45.9–50.8)* | 3,765 | 6,171 | 49.3 (47.0–51.7) |
| Type 2 TBI | 6,902 | 10,983 | 47.9 (45.4–50.5)* | 2,528 | 4,119 | 32.9 (30.7–35.2) |
| Type 3 TBI | 524 | 853 | 3.7 (3.3–4.1)* | 1,327 | 2,215 | 17.7 (16.5–18.9) |
| Length of Stay (days) | ||||||
| 0–1 | 4,098 | 6,514 | 28.4 (26.8–30.1)* | 4,144 | 6,818 | 54.5 (52.7–56.3) |
| 2–3 | 4,070 | 6,493 | 28.3 (27.5–29.2) | 2,292 | 3,752 | 30.0 (28.7–31.3) |
| 4–7 | 3,080 | 4,877 | 21.3 (20.5–22.1)* | 839 | 1,366 | 10.9 (10.1–11.7) |
| 8–14 | 1,552 | 2,474 | 10.8 (10.2–11.4)* | 216 | 358 | 2.9 (2.4–3.3) |
| ≥15 | 1,591 | 2,554 | 11.1 (10.3–12.0)* | 129 | 210 | 1.7 (1.4–2.0) |
| Predictive Mortality Likelihood Level # | ||||||
| Extremely low | 616 | 991 | 4.3 (3.9–4.8)* | 786 | 1,293 | 10.3 (9.4–11.3) |
| Very low (%5 of patients) | 902 | 1,448 | 6.3 (5.7–7.0) | 514 | 838 | 6.7 (6.0–7.5) |
| Low (5–25% of patients) | 779 | 1,246 | 5.4(5.0–5.9)* | 280 | 451 | 3.6 (3.2–4.1) |
| Medium (25–75% of patients) | 5,565 | 8,844 | 38.6 (37.5–39.7)* | 3,860 | 6,380 | 51.0 (49.4–52.6) |
| High (75–95% of patients) | 5,131 | 8,168 | 35.7 (34.2–37.1)* | 2,035 | 3,308 | 26.5 (25.1–27.8) |
| Very high (> 95% of patients) | 1,397 | 2,214 | 9.7 (8.9–10.4)* | 144 | 232 | 1.9 (1.5–2.2) |
| Discharge Status | ||||||
| Routine | 10,903 | 17,368 | 75.8 (74.5–77.1)* | 7,170 | 11,790 | 94.3 (93.6–94.9) |
| Transfer to short term hospital | 396 | 611 | 2.7 (2.2–3.2)* | 108 | 166 | 1.3 (1.0–1.6) |
| Discharged to rehabilitation facility | 1,685 | 2,702 | 11.8 (10.8–12.8)* | 175 | 275 | 2.2 (1.8–2.6) |
| Home health care | 537 | 866 | 3.8 (3.3–4.3)* | 84 | 146 | 1.2 (0.9–1.4) |
| Against medical advice | 66 | 101 | 0.4 (0.3–0.6) | 18 | 29 | 0.2 (0.1–0.3) |
| Died in hospital | 784 | 1,234 | 5.4 (4.9–5.9)* | 62 | 96 | 0.8 (0.6–1.0) |
| Discharged alive, destination unknown | 17 | 26 | 0.1 (0.0–0.2) | ≤10 | ≤10 | |
Data source: 2006 KID.
Confidence intervals for MVC and falls do not overlap, indicating that % difference is statistically significant at p< 0.05 level.
One of the severity measurements provided in the 2006 KID data that was developed by MedStat (see text and reference for more details).
According to the National Center for Health Statistics, estimates based on a sample of ≤ 30 cases have low reliability.
Table IV shows the PMLL across demographics, TBI type, LOS, and discharge status. Similarly, hospitalizations resulting in death in the hospital and discharge into long-term rehabilitation facilities are also stratified across these same variables. A statistically significant higher percentage of males (36.2%) had a high PMLL as compared with females (25.8%). The PMLL showed a strong upward trend with increasing age. Children with Type 1 TBI hospitalizations were significantly more likely to have high (52.1%) and very high PMLLs (13.0%). About two third of Type 2 TBI hospitalizations had medium PMLL (76.4%). There was a strong relationship between the PMLL and length of hospital stay. Generally, the longer the hospital stays, the higher the PMLL. Only 3.0% of those hospitalizations that resulted in routine discharge had very high PMLL. In contrast, of the TBI hospitalizations which resulted in discharge to long-term rehabilitation facilities, 20.0% had a very high PMLL. Of those who died in hospital, 57.3% were considered to have a very high PMLL and 36.7% had a high PMLL. The percentage of children with TBI who were discharged against medical advice (23.5%) with very low and low PMLL was comparable with children with routine discharge (20.4%). However, of those who were discharged against medical advice, 36.1% were considered to have high morality and 8.3% to have very high mortality.
Table IV.
Associations with the predictive mortality likelihood level (PMLL) and selected discharge dispositions among children hospitalized after motor vehicle crash or fall
| Characteristics | Predicted Mortality Likelihood Level (Weighted % 95% CI) #
|
Died in Hospital Weighted % (95 CI)
|
Discharged to Rehabilitation Facility Weighted % (95% CI)
|
||||
|---|---|---|---|---|---|---|---|
| 0–1 (Very Low) | 2 (Low) | 3 (Medium) | 4 (High) | 5 (Very High) | |||
| Gender | |||||||
| Male | 11.6 (10.7–12.5) | 4.8 (4.3–5.3) | 40.1 (39.0–41.3) | 36.2 (34.9–37.5) | 7.3 (6.7–7.9) | 3.9 (3.5–4.3) | 8.9 (8.1–9.6) |
| Female | 14.6 (13.5–15.8) | 4.8 (4.3–5.4) | 48.3 (46.8–49.7) | 25.8 (24.5–27.1) | 6.5 (5.8–7.1) | 3.6 (3.1–4.1) | 7.9 (7.0–8.8) |
| Age Group (Yrs) | |||||||
| < 1 | 4.5 (3.5–5.4) | 1.6 (1.1–2.1) | 83.0 (81.1–84.9) | 9.2 (7.8–10.6) | 1.7 (1.1–2.4) | 1.8 (1.2–2.4) | 0.6 (0.2–0.9) |
| 1–4 | 17.5 (15.4–19.5) | 3.5 (2.8–4.1) | 58.3 (56.1–60.6) | 17.0 (15.3–18.8) | 3.6 (2.9–4.4) | 2.2 (1.6–2.8) | 3.2 (2.4–4.0) |
| 5–9 | 19.3 (17.1–21.6) | 4.8 (3.9–5.7) | 40.6 (38.4–42.7) | 29.9 (27.8–32.1) | 5.4 (4.3–6.5) | 2.2 (1.6–2.8) | 4.8 (3.9–5.7) |
| 10–14 | 15.6 (14.0–17.2) | 5.8 (4.9–6.6) | 32.6 (30.8–34.4) | 38.8 (36.6–41.0) | 7.2 (6.2–8.1) | 3.7 (3.0–4.5) | 6.5 (5.5–7.5) |
| 15–20 | 11.1 (10.2–12.0) | 5.5 (5.0–6.0) | 35.4 (33.9–36.7) | 39.1 (37.5–40.8) | 8.9 (8.1–9.6) | 4.8 (4.3–5.3) | 12.4 (11.3–13.4) |
| TBI Type | |||||||
| Type 1 TBI | 1.8 (1.4–2.2) | 1.0 (0.7–1.2) | 32.2 (30.4–33.9) | 52.1 (50.5–53.7) | 13.0 (12.1–13.9) | 7.6 (6.9–8.2) | 14.3 (13.1–15.6) |
| Type 2 TBI | 28.0 (26.7–29.3) | 9.8 (9.1–10.5) | 48.5 (47.4–49.7) | 12.5 (11.5–13.4) | 1.2 (0.9–1.4) | 0.2 (0.1–0.3) | 3.2 (2.7–3.6) |
| Type 3 TBI | 1.3 (0.8–1.8) | 1.6 (1.0–2.2) | 76.4 (74.2–78.7) | 19.6 (17.6–21.7) | 1.0 (0.6–1.4) | 0.1 (0.0–0.2) | 0.8 (0.3–1.4) |
| Length of Hospital Days | |||||||
| 0–1 | 22.8 (21.3–24.2) | 5.8 (5.2–6.5) | 49.5 (47.9–51.0) | 18.6 917.3–19.8) | 3.3 (2.8–3.9) | 5.4 (4.7–6.1) | 0.6 (0.4–0.7) |
| 2–3 | 11.0 (10.0–12.0) | 5.4 (4.8–6.0) | 47.7 (46.4–49.1) | 33.0 (31.5–34.5) | 3.0 (2.5–3.4) | 2.6 (2.1–3.0) | 1.1 (0.8–1.4) |
| 4–7 | 5.5 (4.7–6.3) | 4.6 (3.9–5.3) | 39.5 (37.8–41.2) | 42.1 (40.3–43.9) | 8.3 (7.4–9.2) | 3.5 (2.9–4.1) | 8.0 (6.7–9.2) |
| 8–14 | 2.1 (1.4–2.7) | 2.1 (1.4–2.8) | 31.1 (28.7–33.5) | 45.6 (42.9–48.2) | 19.1 (17.2–21.0) | 3.4 (2.5–4.3) | 28.3 (25.4–31.1) |
| ≥15 | 0.4 (0.1–0.8) | 0.9 (0.5–1.4) | 14.4 (12.2–16.6) | 61.3 (58.6–63.9) | 22.9 (20.8–25.1) | 1.2 (0.6–1.8) | 53.9 (49.8–57.9) |
| Discharge Status | |||||||
| Routine discharge | 15.0 (14.1–16.2) | 5.4 (5.0–5.9) | 47.5 (46.4–48.5) | 29.1 (27.9–30.3) | 3.0 (2.6–3.3) | ||
| Transfer to short term hospital | 6.1 (3.9–8.3) | 2.7 (1.4–3.9) | 37.0 (32.2–41.8) | 41.0 (36.6–45.5) | 13.2 (9.9–16.5) | ||
| Discharged to rehabilitation facility | 1.6 (1.0–2.2) | 1.1 (0.2–1.6) | 17.6 (15.8–19.5) | 59.7 (57.5–61.9) | 20.0 (18.1–21.8) | ||
| Home health care | 6.5 (4.6–8.4) | 5.1 (3.4–6.7) | 44.4 (40.8–48.1) | 33.7 (29.9–37.6) | 10.2 (7.7–12.8) | ||
| Against medical advice | 16.6 (7.5–25.7) | 6.9 (1.2–12.6) | 32.0 (20.9–43.2) | 36.1 (25.8–46.5) | 8.3 (2.5–14.1) | ||
| Died in hospital | 0.1 (0.0–0.4) | 0.4 (0.0–0.9) | 5.4 (3.7–7.1) | 36.7 (33.6–39.8) | 57.3 (54.0–60.6) | ||
| Discharged alive, destination unknown | 0.0 | 0.0 | 40.3 (22.4–58.2) | 45.3 (24.3–66.3) | 14.4 (4.8–24.1) | ||
Data source: 2006 KID.
One of the severity measures provided in the 2006 KID data that was developed by MedStat (see text and reference for more details).
Overall, 3.8% of TBI hospitalizations resulted in a hospital death, and 8.5% were discharged into long-term rehabilitation facilities. Children hospitalized with Type 1 TBIs were significantly more likely to die in hospital (7.6%) or be discharged into long-term rehabilitation facilities (14.3%) as compared to children with Type 2 (0.2% and 3.2%) or Type 3 TBIs (0.1% and 0.8%). Slightly less than one third (28.3%) of children with TBIs had 8–14 day lengths of stay and more than half (53.9%) of children with 15 day or longer hospital stays were discharged into long-term rehabilitation facilities.
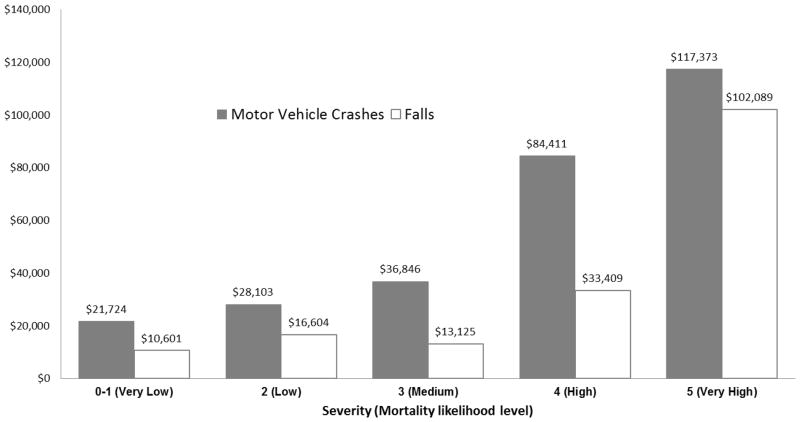
The hospital charges for treating TBI children increased substantially with increased PMLL (figure II). Average charges to MVC TBI hospitalizations with a very high or high predictive mortality levels were approximately two- to six-fold higher than those of the other groups ($117,373 for very high mortality level, $84,411 for high mortality level vs. $36,846, $28,103, $21,725 for medium, low, and very low mortality levels, respectively). Falls-related TBI hospitalizations with very high mortality likelihood had a significantly higher average hospital charges than other groups ($102,089 for very high mortality level, vs. $33,409, $13,125, $16,604, $10,601 for high, medium, low, and very low mortality levels, respectively).
Figure II.
Mean TBI hospitalization charges for motor vehicle crashes and falls by severity (mortality likelihood level) 2006 KID
DISCUSSION
Main Findings
We have examined age and external cause patterns, hospital-based charges, and discharge outcomes of a large sample of U.S. children who were hospitalized in 2006. Based on the KID national data, there were an estimated 58,900 TBI related hospitalizations in the U.S. in 2006 resulting in $2.56 billion in total hospital charges. This estimation is consistent with the CDC estimation that annually almost 60,000 children and adolescents in the U.S. are hospitalized because of TBI [28].
Like other studies, [29] our results suggest that motor vehicle crashes (MVC) and unintentional falls are the two leading causes of TBI-associated hospitalizations. The rate of TBIs caused by MVC increased significantly after 15 years of age regardless of gender, and infants < 1 year of age had the highest rate of TBIs caused by falls. Detailed examination of external causes indicated that almost half of TBIs caused by MVC among children 16–20 years of age occurred when the child was the passenger of the vehicle and almost half of the TBIs among infants < 1 year of age were caused by falls from beds, stairs, chairs, and other furniture.
Our findings indicated that the predictive mortality likelihood level was strongly associated with TBI type, length of hospital stay, hospital charges, and discharge disposition. Classifying TBI both concerning initial severity as well as long-term rehabilitation is considered important for a variety of reasons [30–32]. Previous studies or reviews evaluated an array of TBI classification systems, but no consensus seems to have been reached about acute clinical measurements of severity as well as long-term outcomes [30–32]. To the best of knowledge, our study is the first to assess characteristics and discharge outcomes of TBI children using this disease staging classification developed by the Medstat [23]. The Medstat group also developed predictive scales for hospital charges (resource demand) and length of stay. All three predictive scales (hospital charge, LOS, and mortality) are available in the 2003 and 2006 KID datasets. We only used the predictive mortality level but produced preliminary evidence suggesting that this disease staging classification may serve as a basis for clustering of clinically homogeneous TBI children to assess quality of care, analyze clinical outcomes, and review utilization of resources. Our preliminary findings about a clear correlation between the PMLL and discharge outcomes were encouraging. More research is needed regarding the use other two predictive scales to study hospitalizations and outcomes of U.S. children with TBI.
About 4% of children with a TBI as a result of a fall or MVC died in hospital and 9% were discharged into long-term facilities, and those who stayed in hospital longer than 7 days were significantly more likely to be discharged into long-term facilities. Our study provided evidence that LOS and TBI type were strong predictors for discharge into long-term rehabilitation facilities. In our study, more than half of TBI children who stayed in hospital longer than two weeks and about a third of TBI children who spent 8–14 days in hospital were discharged into long-term rehabilitation facilities. Children with Type 1 TBI were significantly more likely to be discharged into long-term rehabilitation facilities. National statistics on how many and the clinical characteristics of children with TBI who need long-term rehabilitation services is of great importance to people with TBI, their caregivers, and to the society at large [29]. A recent study found that a large proportion of TBI individuals had unmet service need one year after hospital discharge [33]. The greatest barriers reported were lack of awareness, advocacy, and case management. A special report from the Ohio Post-critical Trauma Care Commission concluded that there is little or no statistical data on post-critical traumatic care needs and services [34]. Such need and data gap were also recognized at the national level in 1998 by the NIH Consensus Development Panel on Rehabilitation of Persons With Traumatic Brain Injury [29]. A comprehensive review of accomplishments and unmet goals by the Chairman of the NIH Consensus Conference Panel in 2006 has shown that many TBI rehabilitation issues have not been adequately investigated and rigorous scientific methods are still needed [28].
Strengths and Limitations
The KID database’s uniform coding and access to a large number of hospital discharge records are major strengths of our study. However, several limitations exist. First, the total charges in this study represent billed charges and do not reflect actual payments, professional fees or payments, and/or non-covered charges. Furthermore, as suggested by other authors, hospitalization costs represent only about 5% of the total direct and indirect financial burden of TBI [35]. Second, 2006 KID data were at the discharge level; therefore, individuals who were hospitalized multiple times have multiple records in the KID. Third, almost 15% of TBI-associated records in the 2006 KID had missing ICD-9 E-codes. Finally, we limited our analyses to fall and MVC related TBIs when examining the associations with PMLL, discharge status, and hospitalization costs.
Prevention
TBI prevention measures in the U.S. should focus on MVC, falls, and assaults [1,2,14,36]. Our study pointed to the significant, but different, roles of both MVCs and falls in resulting TBI among different age groups of U.S. children. Therefore, TBI prevention measures should be designed in the context of childhood developmental stages. Unfortunately, caregivers often show insufficient knowledge of the injury risks associated with child development milestones [37].
Poverty, along with age and sex, have been identified as risk factors for unintentional fall injury [38]. Researchers have also recommended that special attention be given to the home environment when considering the prevention of falls in [39]. A recent meta analysis found only a few well designed studies that document the effectiveness of home-safety education and equipment in improving safety practices and reducing injuries due to falls [40]. Understanding differing social groups responses to interventions is an important future research topic.
According to the National Highway Transportation Safety Administration, [35] the fatality and injury rate of MVC among U.S. drivers 16–20 years of age dropped tremendously from 1988 to 2006. Many safety interventions contributed to this reduction in the number of motor vehicle crashes in the U.S., including safety equipment, alcohol drinking laws, graduated driver licensing laws, and educational programs targeting teenagers [41]. Excessive speed, alcohol use, and low rates of seatbelt use contribute heavily to MVC among teenage drivers [35]. Recent research has found evidence in support of educational methods which focus on increasing parent limit setting, including the adoption of parent-teen driving agreements or contracts [42].
Summary
In summary, ongoing standardized surveillance of the occurrence, external causes, and risk factors for TBI is crucial for the design, implementation, and evaluation of effective TBI prevention programs [17]. Evaluation of acute treatment, treatment outcomes, and long-term rehabilitation are equally important. [29] Negative outcomes of childhood TBI often persist well beyond the acute stages of medical treatment and are likely to impact functioning throughout the lifespan [43–45]. Our study suggests that the predictive mortality likelihood level may provide a useful tool to assess characteristics and discharge outcomes of hospitalized TBI children, but more research on disease staging measures is still needed.
Acknowledgments
Dr. J. Shi was a trainee of the USA-China Agricultural Injury Research Training project, funded by a grant from the National Institutes of Health Fogarty International Center (PIs: L. Stallones and H. Xiang, Grant #: 1D43TW007257-01A2).
This study was supported by grants from the National Institutes of Health Fogarty International Center (PIs: L. Stallones and H. Xiang, Grant #: 1D43TW007257-01A2) and the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (PI: H. Xiang, Grant #: R49/CE001172-01).
Contributor Information
Junxin Shi, Email: xiangh@ccri.net.
Huiyun Xiang, Email: huiyun.xiang@nationwidechildrens.org.
Gary A. Smith, Email: gary.smith@nationwidechildrens.org.
Jonathan Groner, Email: jonathan.groner@nationwidechildrens.org.
Zengzhen Wang, Email: wzzh@mails.tjmu.edu.cn.
Krista Wheeler, Email: krista.wheeler@nationwidechildrens.org.
References
- 1.Coronado VG, Thomas KE, Kegler SR. Rates of hospitalization related to traumatic brain injury--nine states, 2003. MMWR. 2007;56(8):167–170. [PubMed] [Google Scholar]
- 2.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375–8. doi: 10.1097/00001199-200609000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Zaloshnja E, Miller T, Langlois JA, Selassie AW. Prevalence of long-term disability from traumatic brain injury in the civilian population of the United States, 2005. J Head Trauma Rehabil. 2008;23(6):394–400. doi: 10.1097/01.HTR.0000341435.52004.ac. [DOI] [PubMed] [Google Scholar]
- 4.Depompei R, Bedell G. Making a difference for children and adolescents with traumatic brain injury. J Head Trauma Rehabil. 2008;23(4):191–6. doi: 10.1097/01.HTR.0000327251.16010.3b. [DOI] [PubMed] [Google Scholar]
- 5.Mandalis A, Kinsella G, Ong B, Anderson V. Working memory and new learning following pediatric traumatic brain injury. Dev Neuropsychol. 2007;32(2):683–701. doi: 10.1080/87565640701376045. [DOI] [PubMed] [Google Scholar]
- 6.Verger K, Junque C, Jurado MA, Tresserras P, Bartumeus F, Nogues P, Poch JM. Age effects on long-term neuropsychological outcome in paediatric traumatic brain injury. Brain Inj. 2000;14(6):495–503. doi: 10.1080/026990500120411. [DOI] [PubMed] [Google Scholar]
- 7.Pullela R, Raber J, Pfankuch T, Ferriero DM, Claus CP, Koh SE, Yamauchi T, Rola R, Fike JR, Noble-Haeusslein LJ. Traumatic injury to the immature brain results in progressive neuronal loss, hyperactivity and delayed cognitive impairments. Dev Neurosci. 2006;28(4–5):396–409. doi: 10.1159/000094166. [DOI] [PubMed] [Google Scholar]
- 8.Max JE, Lansing AE, Koele SL, Castillo CS, Bokura H, Schachar R, Collings N, Williams KE. Attention deficit hyperactivity disorder in children and adolescents following traumatic brain injury. Dev Neuropsychol. 2004;25(1–2):159–77. doi: 10.1080/87565641.2004.9651926. [DOI] [PubMed] [Google Scholar]
- 9.Anderson V, Catroppa C, Morse S, Haritou F, Rosenfeld J. Attentional and processing skills following traumatic brain injury in early childhood. Brain Inj. 2005;19(9):699–710. doi: 10.1080/02699050400025281. [DOI] [PubMed] [Google Scholar]
- 10.Hawley CA. Behaviour and school performance after brain injury. Brain Inj. 2004;18(7):645–59. doi: 10.1080/02699050310001646189. [DOI] [PubMed] [Google Scholar]
- 11.Catale C, Marique P, Closset A, Meulemans T. Attentional and executive functioning following mild traumatic brain injury in children using the Test for Attentional Performance (TAP) battery. J Clin Exp Neuropsychol. 2008:1–8. doi: 10.1080/13803390802134616. [DOI] [PubMed] [Google Scholar]
- 12.Ganesalingam K, Yeates KO, Ginn MS, Taylor HG, Dietrich A, Nuss K, Wright M. Family burden and parental distress following mild traumatic brain injury in children and its relationship to post-concussive symptoms. J Pediatr Psychol. 2008;33(6):621–9. doi: 10.1093/jpepsy/jsm133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stancin T, Wade SL, Walz NC, Yeates KO, Taylor HG. Traumatic brain injuries in early childhood: initial impact on the family. J Dev Behav Pediatr. 2008;29(4):253–61. doi: 10.1097/DBP.0b013e31816b6b0f. [DOI] [PubMed] [Google Scholar]
- 14.Langlois JA, Rutland-Brown W, Thomas KE. The incidence of traumatic brain injury among children in the United States: differences by race. J Head Trauma Rehabil. 2005;20(3):229–38. doi: 10.1097/00001199-200505000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Hawley CA, Ward AB, Long J, Owen DW, Magnay AR. Prevalence of traumatic brain injury amongst children admitted to hospital in one health district: a population-based study. Injury. 2003;34(4):256–60. doi: 10.1016/s0020-1383(02)00193-6. [DOI] [PubMed] [Google Scholar]
- 16.Javouhey E, Guerin AC, Chiron M. Incidence and risk factors of severe traumatic brain injury resulting from road accidents: a population-based study. Accid Anal Prev. 2006;38(2):225–33. doi: 10.1016/j.aap.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Schneier AJ, Shields BJ, Hostetler SG, Xiang H, Smith GA. Incidence of pediatric traumatic brain injury and associated hospital resource utilization in the United States. Pediatrics. 2006;118(2):483–492. doi: 10.1542/peds.2005-2588. [DOI] [PubMed] [Google Scholar]
- 18.Guice KS, Cassidy LD, Oldham KT. Traumatic injury and children: a national assessment. J Trauma. 2007;63(6 Suppl):S68–80. doi: 10.1097/TA.0b013e31815acbb6. discussion S81–6. [DOI] [PubMed] [Google Scholar]
- 19.McGarry LJ, Thompson D, Millham FH, Cowell L, Snyder PJ, Lenderking WR, Weinstein MC. Outcomes and costs of acute treatment of traumatic brain injury. J Trauma. 2002;53(6):1152–9. doi: 10.1097/00005373-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 20.Agency for Healthcare Research and Quality. HCUP Kids’ Inpatient Database (KID) 2008. [DOI] [PubMed] [Google Scholar]
- 21.Marr ALCV, editor. Central nervous system injury surveillance data submission standards---2002. Atlanta,GA: US Department of Health and Human Services, CDC; 2004. [Google Scholar]
- 22.Barell V, Aharonson-Daniel L, Fingerhut LA, Mackenzie EJ, Ziv A, Boyko V, Abargel A, Avitzour M, Heruti R. An introduction to the Barell body region by nature of injury diagnosis matrix. Inj Prev. 2002;8(2):91–6. doi: 10.1136/ip.8.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Medstat Group Inc. Disease Staging Software User Guide. Ann Arbor, MI: Medstat Group, Inc; 2001. [Google Scholar]
- 24.Centers for Disease Control and Prevention, editor. Traumatic brain injury in the United States: assessing outcomes in children. Atlanta, GA: National Center for Injury Prevention and Control; 2001. [Google Scholar]
- 25.Centers for Disease Control and Prevention. Recommended framework of E- code groupings for presenting injury mortality and morbidity data. National Center for Injury Prevention and Control; Sep 15, [Accessed 2008 September 15.]. http://www.cdc.gov/ncipc/osp/matrix2.htm. [Google Scholar]
- 26.SAS Institute Inc. SAS 9.1.3 Help and Documentation,2000–2004. Cary, NC: SAS Institute Inc; [Google Scholar]
- 27.U.S. Census Bureau. Monthly Postcensal Civilian Non-Institutional Population, by single year of age, sex, race, and Hispanic origin, in January 1, 2006. Washington, DC: U.S. Census Bureau; 2008. [Google Scholar]
- 28.Ragnarsson KT. Traumatic brain injury research since the 1998 NIH Consensus Conference: accomplishments and unmet goals. J Head Trauma Rehabil. 2006;21(5):379–387. doi: 10.1097/00001199-200609000-00002. [DOI] [PubMed] [Google Scholar]
- 29.NIH Consensus Development Panel on Rehabilitation of Persons With Traumatic Brain Injury. Consensus conference. Rehabilitation of persons with traumatic brain injury. JAMA. 1999;282(10):974–983. [PubMed] [Google Scholar]
- 30.Saatman KE, Duhaime AC, Bullock R, Maas AI, Valadka A, Manley GT. Classification of traumatic brain injury for targeted therapies. J Neurotrauma. 2008;25(7):719–738. doi: 10.1089/neu.2008.0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sherer M, Struchen MA, Yablon SA, Wang Y, Nick TG. Comparison of indices of traumatic brain injury severity: Glasgow Coma Scale, length of coma and post-traumatic amnesia. J Neurol Neurosurg Psychiatry. 2008;79(6):678–685. doi: 10.1136/jnnp.2006.111187. [DOI] [PubMed] [Google Scholar]
- 32.Van Baalen B, Odding E, Maas AI, Ribbers GM, Bergen MP, Stam HJ. Traumatic brain injury: classification of initial severity and determination of functional outcome. Disabil Rehabil. 2003;25(1):9–18. doi: 10.1080/dre.25.1.9.18. [DOI] [PubMed] [Google Scholar]
- 33.Pickelsimer EE, Selassie AW, Sample PL, Heinemann AW, Gu JK, Veldheer LC. Unmet service needs of persons with traumatic brain injury. J Head Trauma Rehabil. 2007;22(1):1–13. doi: 10.1097/00001199-200701000-00001. [DOI] [PubMed] [Google Scholar]
- 34.Post-critical Trauma Care Commission. Report of Post-critical Trauma Care Commission. Columbus, Ohio: 2003. [Google Scholar]
- 35.Ginsburg KR, Winston FK, Senserrick TM, Garcia-Espana F, Kinsman S, Quistberg DA, Ross JG, Elliott MR. National young-driver survey: teen perspective and experience with factors that affect driving safety. Pediatrics. 2008;121(5):e1391–e1403. doi: 10.1542/peds.2007-2595. [DOI] [PubMed] [Google Scholar]
- 36.Rutland-Brown W, Langlois JA, Thomas KE, Xi YL. Incidence of traumatic brain injury in the United States, 2003. J Head Trauma Rehabil. 2006;21(6):544–548. doi: 10.1097/00001199-200611000-00009. [DOI] [PubMed] [Google Scholar]
- 37.Dedoukou X, Spyridopoulos T, Kedikoglou S, Alexe DM, Dessypris N, Petridou E. Incidence and risk factors of fall injuries among infants: a study in Greece. Arch Pediatr Adolesc Med. 2004;158(10):1002–1006. doi: 10.1001/archpedi.158.10.1002. [DOI] [PubMed] [Google Scholar]
- 38.Khambalia A, Joshi P, Brussoni M, Raina P, Morrongiello B, Macarthur C. Risk factors for unintentional injuries due to falls in children aged 0–6 years: a systematic review. Inj Prev. 2006;12(6):378–81. doi: 10.1136/ip.2006.012161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Runyan CW, Marshall SW, Coyne-Beasley T, Casteel C. Recommendations for home safety research and intervention. Am J Prev Med. 2005;28(1):116–118. doi: 10.1016/j.amepre.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 40.Kendrick D, Watson MC, Mulvaney CA, Smith SJ, Sutton AJ, Coupland CA, Mason-Jones AJ. Preventing childhood falls at home meta-analysis and meta-regression. Am J Prev Med. 2008;35(4):370–379. doi: 10.1016/j.amepre.2008.06.038. [DOI] [PubMed] [Google Scholar]
- 41.National Highway Transportation Safety Administration. Traffic Safety Facts 2005 Data: Younger Drivers. Washington, D.C: US Department of Transportation; 2006. [Google Scholar]
- 42.Simons-Morton B. Parent involvement in novice teen driving: rationale, evidence of effects, and potential for enhancing graduated driver licensing effectiveness. J Safety Res. 2007;38(2):193–202. doi: 10.1016/j.jsr.2007.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Taylor HG, Swartwout MD, Yeates KO, Walz NC, Stancin T, Wade SL. Traumatic brain injury in young children: postacute effects on cognitive and school readiness skills. J Int Neuropsychol Soc. 2008;14(5):734–745. doi: 10.1017/S1355617708081150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: behavior and achievement. Neuropsychology. 2002;16(1):15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- 45.Yeates KO, Swift E, Taylor HG, Wade SL, Drotar D, Stancin T, Minich N. Short- and long-term social outcomes following pediatric traumatic brain injury. J Int Neuropsychol Soc. 2004;10(3):412–426. doi: 10.1017/S1355617704103093. [DOI] [PubMed] [Google Scholar]