Abstract
Severe sepsis results in high morbidity and mortality. Immunomodulation strategies could be an adjunctive therapy to treat sepsis. Endotoxin is a component of gram-negative bacteria and plays an important role in the pathogenesis of septic shock when it is recognized by immune cells. Removal of endotoxin could be an effective adjunctive approach to the management of sepsis. Devices to adsorb endotoxin or inflammatory cytokines have been designed as a strategy to treat severe sepsis, especially sepsis caused by gram-negative bacteria. Polymyxin B-immobilized cartridge has been successfully used to treat patients with sepsis of abdominal origin. Although this cartridge was conceived to adsorb endotoxin, several other immunological mechanisms have been elucidated, and this device has also yielded promising results in patients with nonseptic respiratory failure. In this paper, we summarize the immune modulation actions of Polymyxin B-immobilized cartridge to explore its potential usefulness beyond endotoxin elimination.
1. Introduction
Sepsis is a major healthcare problem. Despite advances in supportive care of critically ill patients, sepsis remains an important cause of death worldwide in adults and children [1–3]. The Surviving Sepsis Campaign (SSC), which standardized the approach to sepsis, was recently updated [4]. Several efforts have been made to improve adherence to SSC guidelines [5, 6]. Nevertheless, mortality and costs are still high [2, 7, 8]. Sepsis is characterized by a complex systemic inflammatory response to a microbial pathogen. First, the presence of microorganisms in the bloodstream causes an innate immune response characterized by the stimulation of monocytes and release of proinflammatory cytokines and the activation of a medley of different immune pathways. Toll-like receptors (TLRs) play a key role in this initial immune activation, acting as innate immune system sensors through the recognition of highly conserved components of a variety of microorganisms [9]. The activation of TLRs induces an inflammatory response to control the infection, which results in local vasodilatation, release of various cytotoxic chemicals, and, hopefully, destruction of the invading pathogen. Many of these same components of inflammation that are beneficial in host defenses against infection can, under some circumstances, be deleterious, causing cell and tissue damage and hence multiple organ failure. Endotoxin, also known as lipopolysaccharide, is a component of gram-negative bacteria and a strong activator of TLR4. The recognition of endotoxin by immune cells is important in the pathogenesis of septic shock [10, 11].
Conventional therapy such as antibiotics and surgical procedures to remove the source of infection is crucial for treating sepsis, but these approaches cannot reverse the effects of the bacterial toxins already released into blood or of the endogenous mediators produced by the host in response to bacteria. Over recent years, numerous attempts have aimed to intervene in the inflammatory cascade. Attempts to stop the inflammatory cascade using antiendotoxin strategies such as monoclonal antibodies or vaccines have failed [12, 13]. Phospholipid emulsion to neutralize endotoxin does not improve outcome in septic patients [14]. A recent phase 2 trial found a nonsignificant trend toward better survival in patients with severe sepsis treated with eritoran tetrasodium, a TLR-4 antagonist [15].
Blood purification techniques including hemoperfusion, plasma exchange, and hemofiltration with hemoperfusion are associated with lower mortality in patients with sepsis as it has been demonstrated in a recent meta-analysis [16]. Removing endotoxin would be an effective adjunctive approach in the management of severe sepsis. Devices to remove endotoxin or inflammatory cytokines have been designed as a strategy to reduce the morbidity and mortality associated with sepsis, especially with sepsis due to gram-negative bacteria. These devices have also been successfully used in patients with sepsis due to gram-positive microorganisms and in patients with acute respiratory distress syndrome (ARDS), suggesting that they could have an immunomodulating action in addition to endotoxin elimination [17–21]. Indeed, many studies report additional beneficial immunological mechanisms for endotoxin removal devices. This review aims to summarize the immune modulation actions of Polymyxin B-immobilized cartridge to understand the potential usefulness of this device beyond endotoxin elimination.
2. Devices to Remove Endotoxin and Inflammatory Molecules
Over recent years, devices to eliminate endotoxin, inflammatory molecules such as cytokines and immune cells, have been designed to mitigate the deleterious effects of the inflammatory cascade. These extracorporeal devices act through convection or adsorption. A double lumen catheter for extracorporeal use is needed. Most of these devices are designed to combine the effect of molecules removal with renal replacement therapies (hemofiltration, dialysis, or hemodiafiltration). The biocompatibility of these devices is the main limitation for its use, thrombocytopenia and bleeding risk are the potential side effects [22]. Table 1 summarizes the mechanism of action and molecules removed by each membrane.
Table 1.
Devices designed to remove endotoxin and cytokines in patients with septic shock.
| Device | Company | Composition | Mechanism | Substance eliminated |
|---|---|---|---|---|
| Toraymyxin 20R | Toray Industries, Japan | Polymyxin B covalently bound to polypropylene-polystyrene fibers fabric | Adsorption | Endotoxin |
|
| ||||
| LPS adsorber | Alteco Medical, Sweden | Synthetic polypeptide bound to porous polyethylene discs | Adsorption | Endotoxin |
|
| ||||
| oXiris | Gambro-Hospal, France | AN69-based membrane, surface treated with a polyethyleneimine (PEI) and grafted with heparin | Adsorption Convection |
Endotoxin Cytokines |
|
| ||||
| MATISSE | Fresenius SE, Germany | Human serum albumin immobilised on polymethacrylate beads | Adsorption | Endotoxin |
|
| ||||
| CPFA | Bellco, Italy | Polyethersulfone Plasma filter with adsorption on an unselective hydrophobicresin cartridge, and a synthetic high-permeability polyethersulfone hemofilter for continuous hemofiltration | Adsorption Plasma filtration |
Cytokines |
|
| ||||
| Cytosorb | Cytosorbents, USA | Polystyrenedivinyl benzene copolymer beads with a biocompatible polyvinylpyrrolidone coating. | Adsorption Convection |
Cytokines |
2.1. Polymyxin B-Immobilized Cartridge (Toraymyxin 20-R, Toray Industries, Japan)
Polymyxin B is a cationic polypeptide antibiotic with activity against gram-negative bacteria and a high affinity to endotoxin, but its intravenous use has been limited due to nephrotoxicity and neurotoxicity [23]. Since 1994, Polymyxin B has been fixed and immobilized with polystyrene fiber in a hemoperfusion column Polymyxin B-immobilized cartridge (PMX) that allows endotoxin removal without the toxic effects of this antibiotic. This treatment has been widely used in Japan for septic shock due to gram-negative bacteria, and its use was authorized in Europe in 1998. Recent studies support the safety and efficacy of this treatment [16, 24–26].
2.2. LPS Adsorber (Alteco Medical AB, Sweden)
This medical device designed for extracorporeal use contains a series of porous polyethylene plates coated with a peptide specific to endotoxin and has a high adsorption capacity. It has been used in patients with septic shock [27–29]. Yaroustovsky et al. [28] compared LPS adsorber and PMX hemoperfusion in a small sample of patients with gram-negative sepsis. The authors did not find differences in outcome. However, due to limitations of the study, the authors concluded that further studies were necessary to clarify the efficacy of LPS adsorber.
2.3. OXiris (Gambro-Hospal, France)
This AN-69 (polysulfone and polyacrylonitrile) based membrane adsorbs a large spectrum of plasma inflammatory mediators such as endotoxin and cytokines [30, 31]. To date, clinical experience with this device is limited, but two trials are underway in septic patients [32]. The results of these two trials are crucial to determine its usefulness compared with the current standard of care.
2.4. MATISSE-Fresenius System (Fresenius SE, Germany)
Based on the endotoxin-binding abilities of human albumin, this adsorber contains human serum albumin immobilized on polymethacrylate beads. Although in vitro experiments were promising, phase 2 study results have been disappointing [33].
2.5. Coupled Plasma Filtration Adsorption, CPFA Bellco, Italy
This extracorporeal treatment is based on nonspecific adsorption of cytokines and other proinflammatory mediators onto a specially designed resin cartridge, coupled with hemofiltration. This device does not adsorb endotoxin. Some studies have shown interesting results regarding hemodynamics and respiratory parameters [34–36]. This is a promising therapy, although further studies are necessary to determine its usefulness in septic patients. One clinical trial, COMPACT 2, is underway to clarify whether adding high doses of CPFA to current clinical practice can reduce hospital mortality in septic shock patients (ClinicalTrials.gov number NCT01639664) [37].
2.6. CytoSorb (Cytosorbents Inc., USA)
This extracorporeal device removes cytokines through adsorption to a high-surface-area biocompatible porous polymer sorbent. This device does not target endotoxin, but it does rapidly eliminate several key cytokines by adsorption in both in vitro and in vivo experiments [38, 39]. This device is very promising, but more studies in septic patients are needed.
Due to the broad information existing about safety and efficacy of Polymyxin B-immobilized cartridge, we will review the immunological mechanisms described in this treatment.
3. Immunological Mechanisms Described for Polymyxin B-Immobilized Cartridge
Polymyxin B-immobilized cartridges (PMX) are designed to bind endotoxin. However, other mechanisms of immunomodulation have also been described. Whereas some of these mechanisms are derived from endotoxin elimination, others result from direct action on other inflammatory molecules and cells or from a combination of endotoxin elimination and direct action on these mediators. Table 2 summarizes these mechanisms.
Table 2.
Summary of mechanisms described for polymyxin B-immobilized cartridge hemoperfusion.
| Molecules | Description | Effect of PMX |
Clinical features after PMX | References |
|---|---|---|---|---|
| Endotoxin | Component of the external membrane of gram-negative microorganisms, recognized by immune cells | ↓ | Interruption of inflammatory cascade | [52–55, 58, 59, 62–64] |
|
| ||||
| IL-1; IL-6; IL-8; IL-9; IL-10; IL-12; IL-17; αTNF | Pro- and anti-inflammatory cytokines; their overproduction is deleterious in sepsis | ↓ | Decrease in the excessive systemic host inflammatory response to infection | [54, 61, 63, 68–70, 72, 88] |
|
| ||||
| Plasminogen activator inhibitor (PAI-1) | Component of the coagulation system that downregulates fibrinolysis in the circulation, favoring coagulation | ↓ | Regulation of fibrinolysis and reversal of the occurrence of sepsis-associated thrombosis | [54, 55, 61] |
|
| ||||
| Neutrophil elastase | Protease that hydrolyzes lung elastase and other proteins | ↓ | Reduction of pulmonary tissue destruction | [61, 71] |
|
| ||||
| High mobility group box protein 1, HMGB-1; receptor for advanced glycation end-products (RAGE), S100A12 |
HMBG-1 is a cytokine to trigger inflammatory mediators; RAGE is a receptor involved in HMBG-1 signaling; S100A12 is a mediator involved in acute lung injury | ↓ | Decrease in the excessive systemic host inflammatory response to infection | [63, 74, 102] |
|
| ||||
| Anandamide | Intrinsic cannabinoid that induces hypotension in septic shock | ↓ | Decrease in septic shock-associated hypotension | [78] |
|
| ||||
| Nitric oxide | Produces vasodilatation and hypotension | ↓ | Decrease in septic shock-associated hypotension | [79] |
|
| ||||
| Erythropoietin | Protein that controls red blood cells production, elevated in sepsis | ↓ | Prognostic biomarker in sepsis | [70] |
|
| ||||
| Troponin T | Protein found in cardiac muscle | ↓ | Decrease in myocardial cell damage | [80] |
|
| ||||
| Angiopoietin-1 and -2 | Angiopoietin-1 reduces pulmonary inflammation and permeability. Angiopoietin-2 interferes with angiopoietin-1, resulting in pulmonary inflammation and increased permeability | Balance | Decrease in acute lung injury | [75] |
|
| ||||
| Vascular endothelial growth factor (VEGF) | Growth factor involved in several acute and chronic lung diseases | ↓ | Improvement of lung function | [69] |
|
| ||||
| Monocytes, neutrophils, and lymphocytes | Immune cells involved in inflammatory response | ↓ | Decrease in the interaction between monocytes and functionally associated cells, decreasing inflammatory response, and decrease in neutrophil and lymphocyte response | [82, 83] |
|
| ||||
| Platelet activator factors (PAF) (P-selectin, β-Thromboglobulin, Platelet factor 4) | PAF stimulates platelets, increasing procoagulation status in sepsis | ↓ | Decrease inprothrombotic status | [52] |
|
| ||||
| HLA-DR and CD16 expression monocytes on granulocytes | Surface antigen expressions HLA-DR and CD-16 are decreased in sepsis | ↑ | Increasing in surface antigen expression on immune cells helps the recovery from immunoparalysis in sepsis | [56] |
|
| ||||
| CD4+CD25+Foxp3+ Treg | T-lymphocytes, responsible formaintaining immunological homeostasis and tolerance, are increased in sepsis | ↓ | Recovery from immunoparalysis in sepsis | [88] |
|
| ||||
| Apoptotic factors (Fas- and caspase-mediated) | Factors that activate cell programmed death of tubular cells | ↓ | Improvement in renal function by reduction of proapoptotic factors | [94] |
|
| ||||
| Metalloproteinase MMP9 | Protease involved in degradation of the basement membrane associated with the alveolar epithelium | ↓ | Decrease in alveolar destruction and improvement in respiratory function | [62, 101] |
IL: interleukin; PMX: polymyxin-B immobilized cartridge.
3.1. Endotoxin Removal
Endotoxin is a major component of the outer membrane of gram-negative microorganisms [40]. Immune cells recognize endotoxin and other bacterial compounds through the TLR, a group of transmembrane proteins that play crucial roles in the host defense against invading pathogens [41]. During a gram-negative infection, TLR-4 recognizes endotoxin and originates a systemic inflammatory response in sepsis with potentially fatal effects in hosts. As a consequence, proinflammatory molecules such as interleukin-1 (IL-1) and tumor necrosis factor alpha (TNFα) are released and generate other cell responses in the inflammatory cascade (Figure 1). This increase in cytokines is followed by a major expression of tissue factor, which activates coagulation, and by an increase in nitric oxide synthesis, which induces vasodilation [42]. Endotoxin levels are high in septic patients [43, 44], but they are also high in critical patients without sepsis, such as patients undergoing cardiopulmonary bypass and those with chronic heart failure, chronic kidney disease, and other medical conditions [44–47]. In critical patients without gram-negative infection, elevated endotoxin levels are related to translocation of gut bacterial antigens and endotoxin into the bloodstream due to gut barrier dysfunction [48–50].
Figure 1.
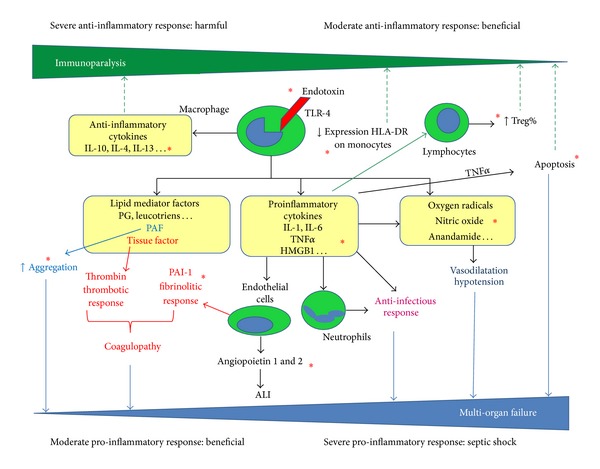
Proinflammatory and anti-inflammatory responses to endotoxin. Red asterisk: immunological mechanisms described for Polymyxin-B hemoperfusion in this review; TLR: toll-like receptor; IL: interleukin; Treg: T regulatory lymphocytes; TNFα: tumor necrosis factor alpha; HMGB1: high mobility group box protein 1; PAF: platelet activator factors; PAI: plasminogen activator inhibitor; ALI: acute lung injury.
Polymyxin B binds endotoxin through hydrophobic and ionic interactions. Polymyxin B's hydrophobic amino acids (Phe, Leu) form hydrophobic bonds with lipid A fatty acid in endotoxin, and the amino groups of Polymyxin B form ionic bonds with the negatively charged phosphate groups of lipid A [51]. This binding results in an antibiotic-endotoxin complex that is highly effective in neutralizing the deleterious effects of endotoxin.
Many studies have reported diverse benefits of PMX hemoperfusion in septic patients, including improved hemodynamics [24, 25, 52–60], increased ratio of partial pressure arterial oxygen and fraction of inspired oxygen (PaO2/FiO2) [24, 54, 55, 57, 58, 60, 61], decreased 28-day mortality [24, 52, 53, 59], and decreased endotoxin levels [52, 53, 55, 58, 59, 62–64]. In a multicenter study, Vincent et al. [25] found that PMX hemoperfusion was safe and improved cardiac and renal function due to sepsis or septic shock; however, they could not demonstrate a reduction in mortality or in endotoxin levels from baseline to the end of treatment. In a systematic review of 28 studies, Cruz et al. [65] concluded that PMX hemoperfusion was associated with lower mortality (RR 0.53, 95% CI: 0.43–0.65) and improvements in mean arterial pressure (MAP), use of inotropes, and PaO2/FiO2. In 17 of these studies in which endotoxin levels were measured, endotoxin levels decreased by 33% to 80% after PMX hemoperfusion [65]. More recently, the same authors published the EUPHAS study [24], a prospective multicenter randomized controlled trial that enrolled 64 patients with severe sepsis or septic shock who underwent emergency surgery for intra-abdominal infection. Patients were randomized to conventional therapy or to conventional therapy plus two sessions of PMX hemoperfusion. After the results of the scheduled interim, analysis revealed that PMX hemoperfusion significantly improved hemodynamics and organ dysfunction and reduced 28-day mortality; the study was discontinued because it was considered unethical to deprive high risk patients of a potentially beneficial therapy; however, early discontinuation resulted in a modest sample size. This study did not measure endotoxin. Two adequately powered prospective trials are underway, and the results of these trials should elucidate the benefit of endotoxin removal (ClinicalTrials.gov numbers NCT01046669 and NCT01222663) [66, 67].
3.2. Elimination of Cytokines and Inflammatory Molecules
Several studies report a reduction in cytokines and inflammatory molecules in patients' plasma after PMX hemoperfusion [54, 56, 61, 68–70].
3.2.1. Cytokines and Inflammatory Proteins
In patients with severe sepsis, Tani et al. [54] found reductions in endotoxin, TNFα, IL-6, IL-10, and plasminogen activator inhibitor-1 (PAI-1) activities after PMX hemoperfusion. In patients with ARDS, Kushi et al. [61] found a reduction in blood levels of PAI-1, neutrophil elastase (NE), and IL-8 after PMX hemoperfusion. NE is a protease that hydrolyzes lung elastin. In these patients, PaO2/FiO2 increased significantly after the treatment, and the authors related this increase to the elimination of IL-8 and NE. In another study, the same group reported a decrease in NE in 20 septic patients treated with PMX hemoperfusion [71]. In 12 patients with septic shock receiving conventional treatment plus two sessions of PMX hemoperfusion, Zagli et al. [72] found a decrease in IL6, IL10, and TNFα in patients' serum after the treatment, especially in survivors. Most authors attribute the decrease in cytokines and inflammatory molecules to the removal of endotoxin and to the effect of this removal on the inflammatory cascade.
3.2.2. High Mobility Group Box-1 Protein
Patients with sepsis have increased high mobility group box-1 protein (HMGB1), a cytokine secreted by immune cells that triggers inflammatory mediators [73]. The receptor for advanced glycation end-products (RAGE) is involved in HMGB1 signaling. The inhibition of the HMGB-1-RAGE axis could be an effective therapeutic strategy for septic shock. Nakamura et al. [63] compared IL-6, HMGB1, and RAGE in serum between 15 patients with septic shock treated with PMX hemoperfusion and healthy volunteers. The levels of the three molecules decreased after PMX hemoperfusion and correlated with a decrease in endotoxin. Abe et al. [74] studied the effects of PMX hemoperfusion on HMGB1 in patients with acute exacerbation of idiopathic pulmonary fibrosis. PMX hemoperfusion both significantly decreased the serum HMGB-1 level and improved the PaO2/FiO2 ratio. Moreover, HMGB-1 was detected in washing medium from the PMX column, suggesting that the decrease in this molecule was not only secondary to endotoxin removal but also to direct removal by the device. A recent study exploring the meaning of HMGB-1 levels in 60 patients with septic shock treated with PMX hemoperfusion found a significant positive correlation between the Sequential Organ Failure Assessment (SOFA) score and HMGB-1 level (P < 0.05). The authors concluded that HMGB-1 is a useful prognostic biomarker in sepsis-induced organ failure in patients undergoing PMX hemoperfusion, but formal establishment of the utility of HMGB-1 as a prognostic biomarker still remains to be performed [68].
3.2.3. Vascular and Coagulation Proteins
PAI-1, a marker of vascular endothelial cell activation elevated by endotoxin and cytokines, is one of the fibrinolysis inhibitory factors. PAI-1 levels decrease after PMX hemoperfusion, decreasing the stimulation of vascular endothelial cells [54, 55, 61]. PMX hemoperfusion may have a role in modulating fibrinolysis and inhibiting the development of ischemic organ dysfunction in sepsis.
Angiopoietin-1 is a positive regulator of blood vessel development, remodeling, and maturation. Angiopoietin-2 is a competitive inhibitor of angiopoietin-1. Angiopoietin-1 and -2 play a contributory role in the pathogenesis of acute lung injury (ALI) in septic patients. Angiopoietin-1 reduces pulmonary inflammation and permeability. Angiopoietin-2 interferes with angiopoietin-1, resulting in pulmonary inflammation and increased permeability. Ebihara et al. [75] reported that PMX hemoperfusion could ameliorate the angiopoietin balance in septic patients with ALI.
Vascular endothelial growth factor (VEGF) is a pluripotent growth and permeability factor that has a broad impact on endothelial cell function. VEGF also plays a role in several acute and chronic lung diseases [76]. Oishi et al. [69] recently studied nine patients with acute exacerbation of idiopathic pulmonary fibrosis treated with conventional therapy and PMX hemoperfusion 6 hours/day on two successive days. They found a high concentration of cytokines and VEGF in the eluate from used PMX cartridge fibers, and the clinical improvement in these patients correlated with the amount of VEGF in the eluate. This is the first study to demonstrate that cytokines and VEGF can be directly adsorbed by PMX hemoperfusion independently from endotoxin removal. The authors suggest that cytokines can bind to PMX hemoperfusion fibers directly through ionic/hydrophobic interactions like endotoxin or indirectly via heparin coated in the fibers.
3.2.4. Other Molecules
Anandamide is an intrinsic cannabinoid that has been related with hypotension in septic shock, although currently its direct link to sepsis is only established in a small patient population. Polymyxin-B directly binds anandamide in vitro [77]. One study in 24 patients with septic shock treated with PMX hemoperfusion found that anandamide levels decreased after PMX hemoperfusion in the nine patients who survived; the authors conclude that removal of anandamide by PMX hemoperfusion, whether directly or as a result of endotoxin elimination, could be key to successful septic shock treatment [78]. Further studies are necessary to elucidate the effect of PMX hemoperfusion on anandamide, in order to establish it as a useful treatment for hypotension.
Elevation of nitric oxide (NO) plays an important role in septic patients, producing vasodilatation and hypotension. Nakamura et al. [79] compared NO breakdown products in urine in 20 patients with PMX hemoperfusion, 15 patients with conventional therapy, and 20 healthy controls. They found that septic patients increased NO production and that PMX hemoperfusion reduced NO levels and thus increased blood pressure.
Troponin is a biomarker that may be elevated in septic patients as a result of subclinical myocardial cell damage. Nakamura et al. [80] found increased troponin T in septic patients compared to nonseptic patients and age-matched healthy controls; interestingly, troponin T decreased after PMX hemoperfusion P < 0.05.
Erythropoietin levels may be higher in patients with sepsis; erythropoietin levels decrease after PMX hemoperfusion and could be a prognostic indicator in patients with septic shock [70].
3.3. Removal of Cells and Phenotype Change
During sepsis, different populations of leukocytes are activated and change their adhesive phenotype. The capture of leukocytes through extracorporeal blood purification could alter the immune response to sepsis [81]. After ex vivo perfusion of heparinized blood from patients with sepsis and septic shock through PMX hemoperfusion in a laboratory circuit, Kumagai et al. [82] found significant decreases in neutrophils (78%), monocytes (70%), and lymphocytes (10%). This marked reduction in white blood cells should be attributed mostly to the reduction in the circulation of proinflammatory cytokines that induce cell activation and proliferation, as opposed to a direct effect of removal of these cells by the cartridge. Nishibori et al. [83] examined the PMX hemoperfusion filters after treating 4 patients with sepsis; PMX hemoperfusion bound monocytes from the peripheral blood leucocytes. PMX hemoperfusion could produce a beneficial effect by reducing the interaction between monocytes and functionally associated cells, including endothelial cells.
The inflammatory response in sepsis involves activation of platelets. High levels of platelet activator factor (PAF) have been observed in sepsis. Nakamura et al. [52] studied the effect of PMX hemoperfusion on platelet activation, comparing 30 patients treated with conventional therapy plus PMX hemoperfusion and 20 patients with conventional therapy alone. Survival was 60% in the group that received PMX hemoperfusion and 30% in the group that received only conventional treatment. Septic patients had increased PAF (P-selectin, platelet factor 4, and β-thromboglobulin), and PMX hemoperfusion reduced the levels of PAF.
3.4. Effect on Immunoparalysis
The human body undergoes a biphasic immunological reaction in sepsis. A proinflammatory reaction takes place, marked by the release of proinflammatory cytokines like TNFα, as a reaction to the bacterial toxins. On the other hand, a counter regulatory anti-inflammatory reaction arises. This phase acts as negative feedback on the inflammation by inhibiting the proinflammatory cytokines. The persistence of a marked compensatory anti-inflammatory response is called “immunoparalysis” (Figure 1). This pronounced immunosuppressive state adversely affects immune function, making the patient vulnerable to opportunistic infections [84]. These two phases of sepsis may occur simultaneously with a lasting anti-inflammatory response in later phases [85]. Most septic patients survive the initial proinflammatory phase, but they die during this second stage. Strategies to stimulate this immunoparalysis phase of sepsis as IFN-γ and granulocyte-macrophage colony-stimulating factor (GM-CSF) have been developed in animals, but extensive clinical studies are needed to test their safety and efficacy [86].
Recently, Ono et al. [56] showed that the expression of the surface antigens, HLA-DR on monocytes and CD16 on granulocytes, is extremely decreased in patients with septic shock and that PMX hemoperfusion beneficially increases this expression on these leukocytes. Thus, PMX hemoperfusion might help septic patients recover from immunoparalysis.
The regulatory T cells (Treg) that express CD4, CD25, and Foxp3 comprise a small percentage of the T-lymphocyte population in the immune system, but they are central to the maintenance of immunological homeostasis and tolerance. In septic patients, the percentage of Treg is increased, and this presumably contributes to sepsis-induced immunosuppression. Polymyxin-B induces Treg cell death in mice through the modulation of the purinergic P2X7 receptor [87]. Ono et al. [88] studied the effect of PMX hemoperfusion on the recovery from the immunosuppression owing to septic shock. Treg, IL-6, and IL-10 were higher in patients with septic shock than in patients with sepsis. After PMX hemoperfusion, Treg cells, Il-6, and IL-10 decreased. In survivors, the decrease in Treg cells was accompanied by an increase in CD4+ cells. Although further studies are necessary to confirm a causative relationship between Treg depletion and PMX hemoperfusion in septic patients, this mechanism could explain why PMX hemoperfusion can be useful in patients without endotoxemia or in those with gram-positive sepsis [89, 90]. The authors also suggest that the second PMX hemoperfusion treatment might provide additional benefits for recovery from immunoparalysis. This study sheds new light on the benefits of treating septic patients with PMX hemoperfusion beyond endotoxin removal.
Apoptosis, programmed cell death, is an energy-dependent process [91]. Endotoxin may cause an inappropriate activation of proapoptotic pathways in immune cells during sepsis, and this may contribute to the impaired immune response that characterizes sepsis [92]. Endotoxin can also cause apoptosis of renal tubular cells through Fas-mediated and caspase-mediated pathways [93]. Cantaluppi et al. [94] tested the hypothesis that PMX hemoperfusion might prevent gram-negative sepsis-induced acute renal failure by reducing the activity of proapoptotic circulating factors. They randomized 16 patients with gram-negative sepsis to receive standard care or standard care plus PMX hemoperfusion. Proapoptotic activity was significantly reduced in the plasma of the PMX hemoperfusion group, with decreases in Fas upregulation and caspase activity, and these patients also had improved renal function.
4. Usefulness in Acute Respiratory Failure
Several studies have found that PMX hemoperfusion has beneficial effects on oxygenation in patients with sepsis [24, 61, 65]. Moreover, PMX hemoperfusion has been successful in patients with influenza A infection [89, 95], ARDS in drug-induced injury [96, 97], interstitial pneumonia [19, 20, 98], and idiopathic fibrosis [18, 69, 74, 99]. Mechanisms other than endotoxin removal could explain the beneficial effects of PMX hemoperfusion in patients with respiratory failure.
Chemical mediators have an important role in the pathogenesis of ARDS, and decreasing them through direct or indirect removal could be beneficial in ARDS patients. Kushi et al. [61] found decreases in PAI1, neutrophil elastase (NE), and IL-8 in ARDS after PMX hemoperfusion. Abe et al. [74] studied the role of decreases in HMGB1 after PMX hemoperfusion in patients with acute exacerbation of idiopathic fibrosis. When the same authors investigated the effects of PMX hemoperfusion in a retrospective multicenter study of 160 patients with acute exacerbation of idiopathic pulmonary fibrosis or interstitial pneumonia, they found that the PaO2/FiO2 ratio significantly increased after PMX hemoperfusion [18]. They concluded that PMX hemoperfusion might be an effective adjunctive therapy for these patients, although the mechanisms underlying the benefits of the treatment are uncertain. Likewise, Hara et al. [20] reported that PMX hemoperfusion resulted in improved PaO2/FiO2 ratio 72 hours and 1 week after treatment in 33 patients with acute exacerbation of interstitial pneumonia. Tsushima et al. [100] treated 20 patients with ARDS with PMX hemoperfusion and compared the outcomes with a historical control group. They found improved PaO2/FiO2 ratio and survival; however, the methodology of the study limits its power to draw conclusions.
Collectively, the matrix metalloproteinases (MMP) are capable of degrading all kinds of extracellular matrix proteins. MMP-9 is a protease involved in the degradation of the basement membrane, a part of the extracellular matrix associated with the alveolar epithelium and vascular endothelium. MMP-9 is essential for the remodeling of basement membranes in various inflammatory lung diseases, including ARDS. Increased amounts of MMP-9 in the vasculature are likely to enhance vascular permeability and to facilitate cell homing and inflammatory remodeling. Nakamura et al. [62] studied the effect of PMX hemoperfusion on MMP levels in ARDS patients by treating 12 ARDS patients with two sessions of PMX hemoperfusion and comparing their laboratory data with those of healthy controls. After treatment, the PaO2/FiO2 ratio and hemodynamic parameters clearly improved. Patients with ARDS had significantly higher levels of MMP-9 than controls. After PMX hemoperfusion, MMP-9 decreased and chest X-ray findings improved. However, the precise mechanism is still unclear. The authors suggest the need for more studies to elucidate the beneficial effect of PMX hemoperfusion in ARDS. In a pilot study of 16 patients, Abe et al. [101] studied the effects of PMX hemoperfusion for acute exacerbation of interstitial pneumonia and demonstrated neutrophil adsorption and a decrease in MMP-9.
In recent years, the mediators S100A12 and RAGE have drawn attention as specific markers of ALI [102]. The expression of S100A12 in neutrophils increases in the presence of endotoxin. Takahashi et al. [103] studied the changes in serum S100A12 and RAGE after PMX hemoperfusion in postoperative septic shock. They found a significant decrease in S100A12 in serum after PMX hemoperfusion and an improvement in PaO2/FiO2 ratio but no decrease in RAGE. The authors attributed the decrease in S100A12 to the concomitant decrease in endotoxin.
As mentioned above, Oishi et al. [69] found cytokines and VEGF in the eluate from PMX hemoperfusion cartridges used to treat patients with acute exacerbation of pulmonary fibrosis, suggesting a new explanation for the improvement in oxygenation in nonseptic patients treated with PMX hemoperfusion.
5. Conclusions
In recent years, many studies have shown that PMX hemoperfusion is a promising strategy for immunomodulation in septic shock, and two ongoing clinical trials will be key in determining its usefulness.
Although most studies have focused on the removal of endotoxin as the principal mechanism through which PMX hemoperfusion improves outcome in sepsis, other studies have revealed mechanisms involving diverse immunological pathways through which PMX hemoperfusion could improve outcome not only in sepsis but also in non-septic respiratory failure. However, these studies are limited by their small samples, their observational and in some cases retrospective design, and the lack of control groups in many cases. Well-designed clinical investigations with larger samples are needed to confirm these findings.
It is interesting to note that the elimination of endotoxin brings about a reduction in many inflammatory molecules and cells involved in the inflammatory cascade. Endotoxin removal devices act at the onset of this complex cascade, and their benefits in terms of immunomodulation are encouraging. Only a part of the consequences of endotoxin elimination has been studied and summarized in this review. Future studies might reveal other mediators and cells involved in sepsis that might be altered after endotoxin removal.
Some of the studies reviewed here found mediators and cells in the eluate from PMX hemoperfusion cartridges or by direct examination of the filter. Further studies are necessary to elucidate how PMX hemoperfusion eliminates these molecules, whether through ionic/hydrophobic interactions like in endotoxin removal or indirectly via heparin that coats the fibers.
Additional mechanisms could potentially explain why PMX hemoperfusion can be beneficial in gram-positive sepsis or non-septic respiratory failure. Endotoxin can be elevated in other medical conditions apart from gram-negative infections, and its removal could also partially explain this benefit. The immunomodulating effects of PMX hemoperfusion in patients with interstitial pneumonia and acute exacerbations of pulmonary fibrosis are especially interesting, given the high mortality associated with these conditions. However, well-designed clinical trials are needed to assess the efficacy of PMX hemoperfusion in these medical conditions.
Future potential directions such as combination of different hemoperfusion devices to treat septic patients, in order to alter the host inflammatory response in more than one step, are currently speculative. Technically, it could be viable, but no experience has been reported to date.
In summary, antimicrobial therapy, surgical treatment of the focus of infection, and hemodynamic stabilization are crucial in the treatment of severe sepsis. PMX hemoperfusion is an effective adjunctive treatment in septic shock. It seems that PMX hemoperfusion might have other beneficial immunological mechanisms in addition to endotoxin removal; however, the limited evidence suggests that we must be cautious with other indications for PMX hemoperfusion, and future studies are necessary.
Disclosure
Esteban and Ferrer have received honorariums as scientific advisor to Ferrer Farma. Artigas has been invited and received honorariums to present conferences in symposiums organized by Ferrer Farma, Toray Co. and Thermo Fisher. Artigas has received honorariums as scientific advisor to Ferrer Farma, Almirall and Gambro Co.
References
- 1.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Critical Care Medicine. 2001;29(7):1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Dombrovskiy VY, Martin AA, Sunderram J, Paz HL. Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Critical Care Medicine. 2007;35(5):1244–1250. doi: 10.1097/01.CCM.0000261890.41311.E9. [DOI] [PubMed] [Google Scholar]
- 3.Kissoon N, Carcillo JA, Espinosa V, et al. World federation of pediatric intensive care and critical care societies: global sepsis initiative. Pediatric Critical Care Medicine. 2011;12(5):494–503. doi: 10.1097/PCC.0b013e318207096c. [DOI] [PubMed] [Google Scholar]
- 4.Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Medicine. 2013;39:165–228. doi: 10.1007/s00134-012-2769-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferrer R, Artigas A, Levy MM, et al. Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. Journal of the American Medical Association. 2008;299(19):2294–2303. doi: 10.1001/jama.299.19.2294. [DOI] [PubMed] [Google Scholar]
- 6.Levy MM, Dellinger RP, Townsend SR, et al. The surviving sepsis campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Critical Care Medicine. 2010;38(2):367–374. doi: 10.1097/CCM.0b013e3181cb0cdc. [DOI] [PubMed] [Google Scholar]
- 7.Esteban A, Frutos-Vivar F, Ferguson ND, et al. Sepsis incidence and outcome: contrasting the intensive care unit with the hospital ward. Critical Care Medicine. 2007;35(5):1284–1289. doi: 10.1097/01.CCM.0000260960.94300.DE. [DOI] [PubMed] [Google Scholar]
- 8.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. The New England Journal of Medicine. 2003;348(16):1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 9.Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006;124(4):783–801. doi: 10.1016/j.cell.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 10.Opal SM. The host response to endotoxin, antilipopolysaccharide strategies, and the management of severe sepsis. International Journal of Medical Microbiology. 2007;297(5):365–377. doi: 10.1016/j.ijmm.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 11.Da Silva AMT, Kaulbach HC, Chuidian FS, Lambert DR, Suffredini AF, Danner RL. Brief report: shock and multiple-organ dysfunction after self- administration of salmonella endotoxin. The New England Journal of Medicine. 1993;328(20):1457–1461. doi: 10.1056/NEJM199305203282005. [DOI] [PubMed] [Google Scholar]
- 12.McCloskey RV, Straube RC, Sanders C, Smith SM, Smith CR. Treatment of septic shock with human monoclonal antibody HA-1A: a randomized, double-blind, placebo-controlled trial. Annals of Internal Medicine. 1994;121(1):1–5. doi: 10.7326/0003-4819-121-1-199407010-00001. [DOI] [PubMed] [Google Scholar]
- 13.Angus DC, Birmingham MC, Balk RA, et al. E5 murine monoclonal antiendotoxin antibody in gram-negative sepsis: a randomized controlled trial. Journal of the American Medical Association. 2000;283(13):1723–1730. doi: 10.1001/jama.283.13.1723. [DOI] [PubMed] [Google Scholar]
- 14.Dellinger PR, Tomayko JF, Angus DC, et al. Efficacy and safety of a phospholipid emulsion (GR270773) in Gram-negative severe sepsis: results of a phase II multicenter, randomized, placebo-controlled, dose-finding clinical trial. Critical Care Medicine. 2009;37(11):2929–2938. doi: 10.1097/CCM.0b013e3181b0266c. [DOI] [PubMed] [Google Scholar]
- 15.Tidswell M, Tillis W, Larosa SP, et al. Phase 2 trial of eritoran tetrasodium (E5564), a Toll-like receptor 4 antagonist, in patients with severe sepsis. Critical Care Medicine. 2010;38(1):72–83. doi: 10.1097/CCM.0b013e3181b07b78. [DOI] [PubMed] [Google Scholar]
- 16.Zhou F, Peng Z, Murugan R, Kellum JA. Blood purification and mortality in sepsis: a meta-analysis of randomized trials. Critical Care Medicine. 2013;41(9):2209–2220. doi: 10.1097/CCM.0b013e31828cf412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taniguchi T, Sato K, Kurita A, Noda T, Okajima M. Efficacy of endotoxin adsorption therapy (polymyxin B hemoperfusion) for methicillin-resistant Staphylococcus aureus toxic shock syndrome. A case report about five patients. Minerva Anestesiologica. 2013;79(7):758–761. [PubMed] [Google Scholar]
- 18.Abe S, Azuma A, Mukae H, et al. Polymyxin B-immobilized fiber column (PMX) treatment for idiopathic pulmonary fibrosis with acute exacerbation: a multicenter retrospective analysis. Internal Medicine. 2012;51:1487–1491. doi: 10.2169/internalmedicine.51.6965. [DOI] [PubMed] [Google Scholar]
- 19.Enomoto N, Suda T, Uto T, et al. Possible therapeutic effect of direct haemoperfusion with a polymyxin B immobilized fibre column (PMX-DHP) on pulmonary oxygenation in acute exacerbations of interstitial pneumonia. Respirology. 2008;13(3):452–460. doi: 10.1111/j.1440-1843.2008.01290.x. [DOI] [PubMed] [Google Scholar]
- 20.Hara S, Ishimoto H, Sakamoto N, et al. Direct hemoperfusion using immobilized polymyxin B in patients with rapidly progressive interstitial pneumonias: a retrospective study. Respiration. 2011;81(2):107–117. doi: 10.1159/000321958. [DOI] [PubMed] [Google Scholar]
- 21.Nakamura T, Ushiyama C, Suzuki Y, et al. Combination therapy with polymyxin B-immobilized fibre haemoperfusion and teicoplanin for sepsis due to methicillin-resistant Staphylococcus aureus. Journal of Hospital Infection. 2003;53(1):58–63. doi: 10.1053/jhin.2002.1332. [DOI] [PubMed] [Google Scholar]
- 22.Winchester JF, Kellum JA, Ronco C, et al. Sorbents in acute renal failure and the systemic inflammatory response syndrome. Blood Purification. 2003;21(1):79–84. doi: 10.1159/000067860. [DOI] [PubMed] [Google Scholar]
- 23.Li J, Nation RL, Turnidge JD, et al. Colistin: the re-emerging antibiotic for multidrug-resistant Gram-negative bacterial infections. The Lancet Infectious Diseases. 2006;6(9):589–601. doi: 10.1016/S1473-3099(06)70580-1. [DOI] [PubMed] [Google Scholar]
- 24.Cruz DN, Antonelli M, Fumagalli R, et al. Early use of polymyxin B hemoperfusion in abdominal septic shock: the EUPHAS randomized controlled trial. Journal of the American Medical Association. 2009;301(23):2445–2452. doi: 10.1001/jama.2009.856. [DOI] [PubMed] [Google Scholar]
- 25.Vincent J-L, Laterre P-F, Cohen J, et al. A pilot-controlled study of a polymyxim B-immobilized hemoperfusion cartridge in patients with severe sepsis secondary to intra-abdominal infection. Shock. 2005;23(5):400–405. doi: 10.1097/01.shk.0000159930.87737.8a. [DOI] [PubMed] [Google Scholar]
- 26.Hirabayashi K, Shiohara M, Saito S, et al. Polymyxin-direct hemoperfusion for sepsis-induced multiple organ failure. Pediatric Blood and Cancer. 2010;55(1):202–205. doi: 10.1002/pbc.22447. [DOI] [PubMed] [Google Scholar]
- 27.Kulabukhov VV. Use of an endotoxin adsorber in the treatment of severe abdominal sepsis. Acta Anaesthesiologica Scandinavica. 2008;52(7):1024–1025. doi: 10.1111/j.1399-6576.2008.01677.x. [DOI] [PubMed] [Google Scholar]
- 28.Yaroustovsky M, Abramyan M, Popok Z, et al. Preliminary report regarding the use of selective sorbents in complex cardiac surgery patients with extensive sepsis and prolonged intensive care stay. Blood Purification. 2009;28(3):227–233. doi: 10.1159/000231988. [DOI] [PubMed] [Google Scholar]
- 29.Ala-Kokko TI, Laurila J, Koskenkari J. A new endotoxin adsorber in septic shock: observational case series. Blood Purification. 2011;32(4):303–309. doi: 10.1159/000330323. [DOI] [PubMed] [Google Scholar]
- 30.Rimmelé T, Assadi A, Cattenoz M, et al. High-volume haemofiltration with a new haemofiltration membrane having enhanced adsorption properties in septic pigs. Nephrology Dialysis Transplantation. 2009;24(2):421–427. doi: 10.1093/ndt/gfn518. [DOI] [PubMed] [Google Scholar]
- 31.Shum HP, Chan KC, Kwan MC, Yan WW. Application of endotoxin and cytokine adsorption haemofilter in septic acute kidney injury due to Gram-negative bacterial infection. Hong Kong Medical Journal. 2013 doi: 10.12809/hkmj133910. [DOI] [PubMed] [Google Scholar]
- 32.Honore PM, Jacobs R, Joannes-Boyau O, et al. Newly designed CRRT membranes for sepsis and SIRS—a pragmatic approach for bedside intensivists summarizing the more recent advances: a systematic structured review. ASAIO Journal. 2013;59:99–106. doi: 10.1097/MAT.0b013e3182816a75. [DOI] [PubMed] [Google Scholar]
- 33.Reinhart K, Meier-Hellmann A, Beale R, et al. Open randomized phase II trial of an extracorporeal endotoxin adsorber in suspected Gram-negative sepsis. Critical Care Medicine. 2004;32(8):1662–1668. doi: 10.1097/01.ccm.0000132902.54925.b5. [DOI] [PubMed] [Google Scholar]
- 34.Ronco C, Brendolan A, Lonnemann G, et al. A pilot study of coupled plasma filtration with adsorption in septic shock. Critical Care Medicine. 2002;30(6):1250–1255. doi: 10.1097/00003246-200206000-00015. [DOI] [PubMed] [Google Scholar]
- 35.Mao H-J, Yu S, Yu X-B, et al. Effects of coupled plasma filtration adsorption on immune function of patients with multiple organ dysfunction syndrome. International Journal of Artificial Organs. 2009;32(1):31–38. doi: 10.1177/039139880903200104. [DOI] [PubMed] [Google Scholar]
- 36.Formica M, Olivieri C, Livigni S, et al. Hemodynamic response to coupled plasmafiltration-adsorption in human septic shock. Intensive Care Medicine. 2003;29(5):703–708. doi: 10.1007/s00134-003-1724-0. [DOI] [PubMed] [Google Scholar]
- 37.ClinicalTrials.gov.COMbining Plasma-filtration and Adsorption Clinical Trial 2 (COMPACT2). NCT01639664. 2013, http://clinicaltrials.gov/ct2/show/NCT01639664.
- 38.Peng Z-Y, Carter MJ, Kellum JA. Effects of hemoadsorption on cytokine removal and short-term survival in septic rats. Critical Care Medicine. 2008;36(5):1573–1577. doi: 10.1097/CCM.0b013e318170b9a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kellum JA, Song M, Venkataraman R. Hemoadsorption removes tumor necrosis factor, interleukin-6, and interleukin-10, reduces nuclear factor-κB DNA binding, and improves short-term survival in lethal endotoxemia. Critical Care Medicine. 2004;32(3):801–805. doi: 10.1097/01.ccm.0000114997.39857.69. [DOI] [PubMed] [Google Scholar]
- 40.van der Poll T, Opal SM. Host-pathogen interactions in sepsis. The Lancet Infectious Diseases. 2008;8(1):32–43. doi: 10.1016/S1473-3099(07)70265-7. [DOI] [PubMed] [Google Scholar]
- 41.Takeda K. Evolution and integration of innate immune recognition systems: the Toll-like receptors. Journal of Endotoxin Research. 2005;11(1):51–55. doi: 10.1179/096805105225006687. [DOI] [PubMed] [Google Scholar]
- 42.Cohen J. The immunopathogenesis of sepsis. Nature. 2002;420(6917):885–891. doi: 10.1038/nature01326. [DOI] [PubMed] [Google Scholar]
- 43.Opal SM, Scannon PJ, Vincent J-L, et al. Relationship between plasma levels of lipopolysaccharide (LPS) and LPS- binding protein in patients with severe sepsis and septic shock. Journal of Infectious Diseases. 1999;180(5):1584–1589. doi: 10.1086/315093. [DOI] [PubMed] [Google Scholar]
- 44.Marshall JC, Foster D, Vincent J-L, et al. Diagnostic and prognostic implications of endotoxemia in critical illness: results of the MEDIC study. Journal of Infectious Diseases. 2004;190(3):527–534. doi: 10.1086/422254. [DOI] [PubMed] [Google Scholar]
- 45.Niebauer J, Volk H-D, Kemp M, et al. Endotoxin and immune activation in chronic heart failure: a prospective cohort study. The Lancet. 1999;353(9167):1838–1842. doi: 10.1016/S0140-6736(98)09286-1. [DOI] [PubMed] [Google Scholar]
- 46.Lin C-Y, Tsai I-F, Ho Y-P, et al. Endotoxemia contributes to the immune paralysis in patients with cirrhosis. Journal of Hepatology. 2007;46(5):816–826. doi: 10.1016/j.jhep.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 47.Gonçalves S, Pecoits-Filho R, Perreto S, et al. Associations between renal function, volume status and endotoxaemia in chronic kidney disease patients. Nephrology Dialysis Transplantation. 2006;21(10):2788–2794. doi: 10.1093/ndt/gfl273. [DOI] [PubMed] [Google Scholar]
- 48.Pathan N, Burmester M, Adamovic T, et al. Intestinal injury and endotoxemia in children undergoing surgery for congenital heart disease. American Journal of Respiratory and Critical Care Medicine. 2011;184(11):1261–1269. doi: 10.1164/rccm.201104-0715OC. [DOI] [PubMed] [Google Scholar]
- 49.Clark JA, Coopersmith CM. Intestinal crosstalk: a new paradigm for understanding the gut as the “motor” of critical illness. Shock. 2007;28(4):384–393. doi: 10.1097/shk.0b013e31805569df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cinel I, Dellinger RP. Advances in pathogenesis and management of sepsis. Current Opinion in Infectious Diseases. 2007;20(4):345–352. doi: 10.1097/QCO.0b013e32818be70a. [DOI] [PubMed] [Google Scholar]
- 51.Vesentini S, Soncini M, Zaupa A, Silvestri V, Fiore GB, Redaelli A. Multi-scale analysis of the Toraymyxin adsorption cartridge part 1: molecular interaction of polymyxin B with endotoxins. International Journal of Artificial Organs. 2006;29(2):239–250. doi: 10.1177/039139880602900210. [DOI] [PubMed] [Google Scholar]
- 52.Nakamura T, Ebihara I, Shoji H, Ushiyama C, Suzuki S, Koide H. Treatment with polymyxin B-immobilized fiber reduces platelet activation in septic shock patients: decrease in plasma levels of soluble P-selectin, platelet factor 4 and β-thromboglobulin. Inflammation Research. 1999;48(4):171–175. doi: 10.1007/s000110050442. [DOI] [PubMed] [Google Scholar]
- 53.Suzuki H, Nemoto H, Nakamoto H, et al. Continuous hemodiafiltration with polymyxin-B immobilized fiber is effective in patients with sepsis syndrome and acute renal failue. Therapeutic Apheresis. 2002;6(3):234–240. doi: 10.1046/j.1526-0968.2002.00416.x. [DOI] [PubMed] [Google Scholar]
- 54.Tani T, Hanasawa K, Kodama M, et al. Correlation between plasma endotoxin, plasma cytokines, and plasminogen activator inhibitor-1 activities in septic patients. World Journal of Surgery. 2001;25(5):660–668. doi: 10.1007/s002680020028. [DOI] [PubMed] [Google Scholar]
- 55.Ikeda T, Ikeda K, Nagura M, et al. Clinical evaluation of PMX-DHP for hypercytokinemia caused by septic multiple organ failure. Therapeutic Apheresis and Dialysis. 2004;8(4):293–298. doi: 10.1111/j.1526-0968.2004.00167.x. [DOI] [PubMed] [Google Scholar]
- 56.Ono S, Tsujimoto H, Matsumoto A, Ikuta S-I, Kinoshita M, Mochizuki H. Modulation of human leukocyte antigen-DR on monocytes and CD16 on granulocytes in patients with septic shock using hemoperfusion with polymyxin B-immobilized fiber. American Journal of Surgery. 2004;188(2):150–156. doi: 10.1016/j.amjsurg.2003.12.067. [DOI] [PubMed] [Google Scholar]
- 57.Mitaka C, Tsuchida N, Kawada K, Nakajima Y, Imai T, Sasaki S. A Longer duration of polymyxin b-immobilized fiber column hemoperfusion improves pulmonary oxygenation in patients with septic shock. Shock. 2009;32(5):478–483. doi: 10.1097/SHK.0b013e3181a2a978. [DOI] [PubMed] [Google Scholar]
- 58.Novelli G, Ferretti G, Poli L, et al. Clinical results of treatment of postsurgical endotoxin-mediated sepsis with polymyxin-B direct hemoperfusion. Transplantation Proceedings. 2010;42(4):1021–1024. doi: 10.1016/j.transproceed.2010.03.056. [DOI] [PubMed] [Google Scholar]
- 59.Nemoto H, Nakamoto H, Okada H, et al. Newly developed immobilized polymyxin B fibers improve the survival of patients with sepsis. Blood Purification. 2001;19(4):361–369. doi: 10.1159/000046966. [DOI] [PubMed] [Google Scholar]
- 60.Navarro R, Guerrero M, Gonzalez M, Quecedo L, Garcia A, Ramasco F. Description of the hemodynamic and respiratory effects of hemoperfusion treatment with polymyxin B in patients with abdominal septic shock. Revista Española de Anestesiología y Reanimación. 2013;60:344–347. doi: 10.1016/j.redar.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 61.Kushi H, Miki T, Okamaoto K, Nakahara J, Saito T, Tanjoh K. Early hemoperfusion with an immobilized polymyxin B fiber column eliminates humoral mediators and improves pulmonary oxygenation. Critical Care. 2005;9(6):R653–R661. doi: 10.1186/cc3815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nakamura T, Kawagoe Y, Matsuda T, et al. Effect of polymyxin B-immobilized fiber on blood metalloproteinase-9 and tissue inhibitor of metalloproteinase-1 levels in acute respiratory distress syndrome patients. Blood Purification. 2004;22(3):256–260. doi: 10.1159/000078494. [DOI] [PubMed] [Google Scholar]
- 63.Nakamura T, Sato E, Fujiwara N, Kawagoe Y, Maeda S, Yamagishi S-I. Suppression of high-mobility group box-1 and receptor for advanced glycation end-product axis by polymyxin B-immobilized fiber hemoperfusion in septic shock patients. Journal of Critical Care. 2011;26(6):546–549. doi: 10.1016/j.jcrc.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 64.Kojika M, Sato N, Yaegashi Y, et al. Endotoxin adsorption therapy for septic shock using polymyxin B-immobilized fibers (PMX): evaluation by high-sensitivity endotoxin assay and measurement of the cytokine production capacity. Therapeutic Apheresis and Dialysis. 2006;10(1):12–18. doi: 10.1111/j.1744-9987.2006.00340.x. [DOI] [PubMed] [Google Scholar]
- 65.Cruz DN, Perazella MA, Bellomo R, et al. Effectiveness of polymyxin B-immobilized fiber column in sepsis: a systematic review. Critical Care. 2007;11, article R47 doi: 10.1186/cc5780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.ClinicalTrials.gov. Safety and Efficacy of Polymyxin B Hemoperfusion, (PMX) for Septic Shock.EUPHRATES. NCT01046669. 2013, http://clinicaltrials.gov/ct2/show/NCT01046669.
- 67.ClinicalTrials.gov. Effects of hemoperfusion with a Polymyxin B membrane in peritonitis with septic shock (ABDO-MIX). NCT01222663. 2013, http://clinicaltrials.gov/ct2/show/NCT01222663.
- 68.Ueno T, Ikeda T, Ikeda K, et al. HMGB-1 as a useful prognostic biomarker in sepsis-induced organ failure in patients undergoing PMX-DHP. Journal of Surgical Research. 2011;171(1):183–190. doi: 10.1016/j.jss.2009.11.708. [DOI] [PubMed] [Google Scholar]
- 69.Oishi K, Mimura-Kimura Y, Miyasho T, et al. Association between cytokine removal by polymyxin B hemoperfusion and improved pulmonary oxygenation in patients with acute exacerbation of idiopathic pulmonary fibrosis. Cytokine. 2013;61:84–89. doi: 10.1016/j.cyto.2012.08.032. [DOI] [PubMed] [Google Scholar]
- 70.Nakamura T, Ebihara I, Shimada N, Koide H. Changes in plasma erythropoietin and interleukin-6 concentrations in patients with septic shock after hemoperfusion with polymyxin B-immobilized fiber. Intensive Care Medicine. 1998;24(12):1272–1276. doi: 10.1007/s001340050761. [DOI] [PubMed] [Google Scholar]
- 71.Kushi H, Miki T, Nakahara J, Okamoto K, Saito T, Tanjoh K. Hemoperfusion with an immobilized polymyxin B column reduces the blood level of neutrophil elastase. Blood Purification. 2006;24(2):212–217. doi: 10.1159/000090593. [DOI] [PubMed] [Google Scholar]
- 72.Zagli G, Bonizzoli M, Spina R, et al. Effects of hemoperfusion with an immobilized polymyxin-B fiber column on cytokine plasma levels in patients with abdominal sepsis. Minerva Anestesiologica. 2010;76(6):405–412. [PubMed] [Google Scholar]
- 73.Gibot S, Massin F, Cravoisy A, et al. High-mobility group box 1 protein plasma concentrations during septic shock. Intensive Care Medicine. 2007;33(8):1347–1353. doi: 10.1007/s00134-007-0691-2. [DOI] [PubMed] [Google Scholar]
- 74.Abe S, Hayashi H, Seo Y, et al. Reduction in serum high mobility group box-1 level by polymyxin b-immobilized fiber column in patients with idiopathic pulmonary fibrosis with acute exacerbation. Blood Purification. 2011;32(4):310–316. doi: 10.1159/000330325. [DOI] [PubMed] [Google Scholar]
- 75.Ebihara I, Hirayama K, Nagai M, et al. Angiopoietin balance in septic shock patients with acute lung injury: effect of direct hemoperfusion with polymyxin B-immobilized fiber. Therapeutic Apheresis and Dialysis. 2011;15(4):349–354. doi: 10.1111/j.1744-9987.2011.00963.x. [DOI] [PubMed] [Google Scholar]
- 76.Voelkel NF, Vandivier RW, Tuder RM. Vascular endothelial growth factor in the lung. American Journal of Physiology. 2006;290(2):L209–L221. doi: 10.1152/ajplung.00185.2005. [DOI] [PubMed] [Google Scholar]
- 77.Wang Y, Liu Y, Sarker KP, et al. Polymyxin B binds to anandamide and inhibits its cytotoxic effect. FEBS Letters. 2000;470(2):151–155. doi: 10.1016/s0014-5793(00)01313-2. [DOI] [PubMed] [Google Scholar]
- 78.Kohro S, Imaizumi H, Yamakage M, et al. Anandamide absorption by direct hemoperfusion with polymixin B-immobilized fiber improves the prognosis and organ failure assessment score in patients with sepsis. Journal of Anesthesia. 2006;20(1):11–16. doi: 10.1007/s00540-005-0366-5. [DOI] [PubMed] [Google Scholar]
- 79.Nakamura T, Kawagoe Y, Matsuda T, Koide H. Effect of polymyxin B-immobilized fiber on bone resorption in patients with sepsis. Intensive Care Medicine. 2004;30(9):1838–1841. doi: 10.1007/s00134-004-2357-7. [DOI] [PubMed] [Google Scholar]
- 80.Nakamura T, Ushiyama C, Shoji H, Koide H. Effects of hemoperfusion on serum cardiac troponin T concentrations using polymyxin B-immobilized fibers in septic patients undergoing hemodialysis. ASAIO Journal. 2002;48(1):41–44. doi: 10.1097/00002480-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 81.Rimmele T, Kaynar AM, McLaughlin JN, et al. Leukocyte capture and modulation of cell-mediated immunity during human sepsis: an ex vivo study. Critical Care. 2013;17(article R59) doi: 10.1186/cc12587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kumagai T, Takeyama N, Yabuki T, et al. Apheresis of activated leukocytes with an immobilized polymyxin B filter in patients with septic shock. Shock. 2010;34(5):461–466. doi: 10.1097/SHK.0b013e3181e14ca0. [DOI] [PubMed] [Google Scholar]
- 83.Nishibori M, Takahashi HK, Katayama H, et al. Specific removal of monocytes from peripheral blood of septic patients by polymyxin B-immobilized filter column. Acta Medica Okayama. 2009;63(1):65–69. doi: 10.18926/AMO/31855. [DOI] [PubMed] [Google Scholar]
- 84.Boomer JS, To K, Chang KC, et al. Immunosuppression in patients who die of sepsis and multiple organ failure. Journal of the American Medical Association. 2011;306(23):2594–2605. doi: 10.1001/jama.2011.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bosmann M, Ward PA. The inflammatory response in sepsis. Trends in Immunology. 2013;34:129–136. doi: 10.1016/j.it.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Leentjens J, Kox M, van der Hoeven JG, Netea MG, Pickkers P. Immunotherapy for the adjunctive treatment of sepsis: from immunosuppression to immunostimulation. Time for a paradigm change? American Journal of Respiratory and Critical Care Medicine. 2013;187:1287–1293. doi: 10.1164/rccm.201301-0036CP. [DOI] [PubMed] [Google Scholar]
- 87.Cappelli C, López X, Labra Y, et al. Polymyxin B increases the depletion of T regulatory cell induced by purinergic agonist. Immunobiology. 2012;217(3):307–315. doi: 10.1016/j.imbio.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 88.Ono S, Kimura A, Hiraki S, et al. Removal of increased circulating CD4+CD25+Foxp3+ regulatory T cells in patients with septic shock using hemoperfusion with polymyxin B-immobilized fibers. Surgery. 2013;153(2):262–271. doi: 10.1016/j.surg.2012.06.023. [DOI] [PubMed] [Google Scholar]
- 89.Takeda S, Munakata R, Abe S, et al. Hypercytokinemia with 2009 pandemic H1N1 (pH1N1) influenza successfully treated with polymyxin B-immobilized fiber column hemoperfusion. Intensive Care Medicine. 2010;36(5):906–907. doi: 10.1007/s00134-010-1830-8. [DOI] [PubMed] [Google Scholar]
- 90.Totsugawa T, Kuinose M, Yoshitaka H, et al. Intraoperative direct hemoperfusion with a polymyxin-B immobilized fiber column for treatment of infective endocarditis. General Thoracic and Cardiovascular Surgery. 2011;59(2):98–104. doi: 10.1007/s11748-010-0700-1. [DOI] [PubMed] [Google Scholar]
- 91.Wesche-Soldato DE, Swan RZ, Chung C-S, Ayala A. The apoptotic pathway as a therapeutic target in sepsis. Current Drug Targets. 2007;8(4):493–500. doi: 10.2174/138945007780362764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hotchkiss RS, Swanson PE, Freeman BD, et al. Apoptotic cell death in patients with sepsis, shock, and multiple organ dysfunction. Critical Care Medicine. 1999;27(7):1230–1251. doi: 10.1097/00003246-199907000-00002. [DOI] [PubMed] [Google Scholar]
- 93.Jo SK, Cha DR, Cho WY, et al. Inflammatory cytokines and lipopolysaccharide induce fas-mediated apoptosis in renal tubular cells. Nephron. 2002;91(3):406–415. doi: 10.1159/000064280. [DOI] [PubMed] [Google Scholar]
- 94.Cantaluppi V, Assenzio B, Pasero D, et al. Polymyxin-B hemoperfusion inactivates circulating proapoptotic factors. Intensive Care Medicine. 2008;34(9):1638–1645. doi: 10.1007/s00134-008-1124-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yatera K, Yamasaki K, Kawanami T, et al. A case of successful treatment with polymyxin B-immobilized fiber column direct hemoperfusion in acute respiratory distress syndrome after influenza A infection. Internal Medicine. 2011;50(6):601–605. doi: 10.2169/internalmedicine.50.4604. [DOI] [PubMed] [Google Scholar]
- 96.Yokoyama T, Tsushima K, Yamamoto H, et al. Polymyxin B-immobilized fiber column hemoperfusion treatment for drug-induced severe respiratory failure: report of three cases. Internal Medicine. 2010;49(1):59–64. doi: 10.2169/internalmedicine.49.2213. [DOI] [PubMed] [Google Scholar]
- 97.Sato N, Kojima K, Horio Y, et al. Successful treatment of severe amiodarone pulmonary toxicity with polymyxin B-immobilized fiber column direct hemoperfusion. Chest. 2013;143:1146–1150. doi: 10.1378/chest.12-0994. [DOI] [PubMed] [Google Scholar]
- 98.Ichiyasu H, Horio Y, Tsumura S, et al. Favorable outcome with hemoperfusion of polymyxin B-immobilized fiber column for rapidly progressive interstitial pneumonia associated with clinically amyopathic dermatomyositis: report of three cases. doi: 10.3109/14397595.2013.852847. Modern Rheumatology. In press. [DOI] [PubMed] [Google Scholar]
- 99.Seo Y, Abe S, Kurahara M, et al. Beneficial effect of polymyxin B-immobilized fiber column (PMX) hemoperfusion treatment on acute exacerbation of idiopathic pulmonary fibrosis. Internal Medicine. 2006;45(18):1033–1038. doi: 10.2169/internalmedicine.45.6018. [DOI] [PubMed] [Google Scholar]
- 100.Tsushima K, Kubo K, Koizumi T, et al. Direct hemoperfusion using a polymyxin B immobilized column improves acute respiratory distress syndrome. Journal of Clinical Apheresis. 2002;17(2):97–102. doi: 10.1002/jca.10019. [DOI] [PubMed] [Google Scholar]
- 101.Abe S, Seo Y, Hayashi H, et al. Neutrophil adsorption by polymyxin b-immobilized fiber column for acute exacerbation in patients with interstitial pneumonia: a pilot study. Blood Purification. 2010;29(4):321–326. doi: 10.1159/000287232. [DOI] [PubMed] [Google Scholar]
- 102.Kikkawa T, Sato N, Kojika M, et al. Significance of Measuring S100A12 and sRAGE in the Serum of Sepsis Patients with Postoperative Acute Lung Injury. Digestive Surgery. 2010;27(4):307–312. doi: 10.1159/000313687. [DOI] [PubMed] [Google Scholar]
- 103.Takahashi G, Hoshikawa K, Matsumoto N, et al. Changes in serum S100A12 and sRAGE associated with improvement of the PaO2/FiO2 ratio following PMX-DHP therapy for postoperative septic shock. European Surgical Research. 2011;47(3):135–140. doi: 10.1159/000330448. [DOI] [PubMed] [Google Scholar]


