Abstract
Pregnancy induced hypertension is a hypertensive disorder, which occurs in 5% to 7% of all pregnancies. These parturients present to the labour and delivery unit ranging from gestational hypertension to HELLP syndrome. It is essential to understand the various clinical conditions that may mimic preeclampsia and the urgency of cesarean delivery, which may improve perinatal outcome. The administration of general anesthesia (GA) increases morbidity and mortality in both mother and baby. The provision of regional anesthesia when possible maintains uteroplacental blood flow, avoids the complications with GA, improves maternal and neonatal outcome. The use of ultrasound may increase the success rate. This review emphasizes on the regional anesthetic considerations when such parturients present to the labor and delivery unit.
Keywords: Anesthesia, hypertension, pregnancy, regional
Introduction
Preeclampsia is a hypertensive disorder of gestation, complicating 5% to 7% of all pregnancies. It is characterized by new onset of hypertension (≥140/90 mmHg) and proteinuria that develops after 20 weeks of gestation and usually resolves within 48 h of fetal delivery. It can progress to a severe form in 25% of parturients when it is undiagnosed or untreated.[1] It increases both maternal and fetal morbidity with the occurrence of eclampsia in 0.04-0.05% of the affected parturients[2,3] with an estimated annual mortality rate of 50,000 parturients with preeclampsia world-wide.[4]
Parturients with pregnancy induced hypertension may present to the labor and delivery unit with or without a prior diagnosis of preeclampsia and may pose a significant anesthetic challenge. The administration of general anesthesia (GA) in such high risk parturients may cause exaggerated cardiovascular response to intubation leading to cerebral hemorrhage and edema, cardiovascular decompensation causing pulmonary edema; thereby increasing morbidity and mortality in both mother and child.[5,6] Similarly, an exaggerated pressor response to intubation may increase the maternal plasma catecholamine concentration, which in turn impairs the uteroplacental blood flow.[7,8,9]
The administration of regional anesthesia (RA) not only avoids the maternal complications with GA like difficult intubation, vasopressor response to intubation, but also improves uteroplacental blood flow and neonatal outcome. This review places emphasis on the regional anesthetic considerations in such parturients presenting to the labor and delivery unit. Electronic search strategies included searching the databases Ovid MEDLINE, Ovid EMBASE (both until Jan 2013) and the Cochrane Library using the key words pregnancy, preeclampsia, eclampsia, regional, and anesthesia and neuraxial.
Classification of Hypertension in Pregnancy
Parturients with high blood pressure fall into four categories, which include:
Gestational hypertension
Preeclampsia-eclampsia
Chronic hypertension or pre-pregnant hypertension
Preeclampsia superimposed on chronic hypertension.[10]
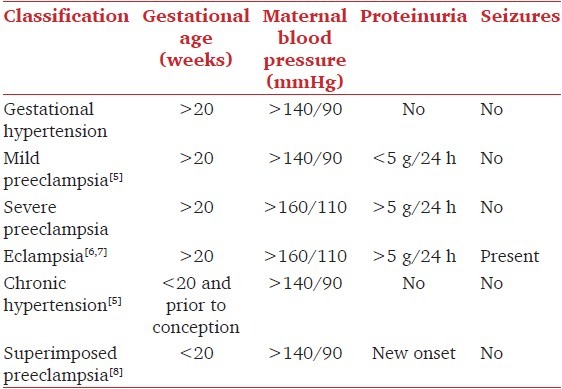
The clinical presentations of hypertension in pregnancy are described in Tables 1 and 2, which guide the attending anesthesiologist to administer safe anesthesia.[10,11,12,13]
Table 1.
Differences between mild and severe preeclampsia
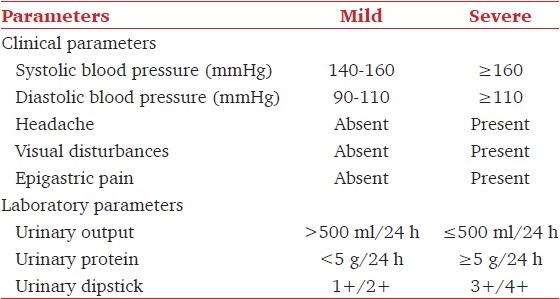
Table 2.
Classification of hypertension in pregnancy
Differential Diagnosis of Preeclampsia
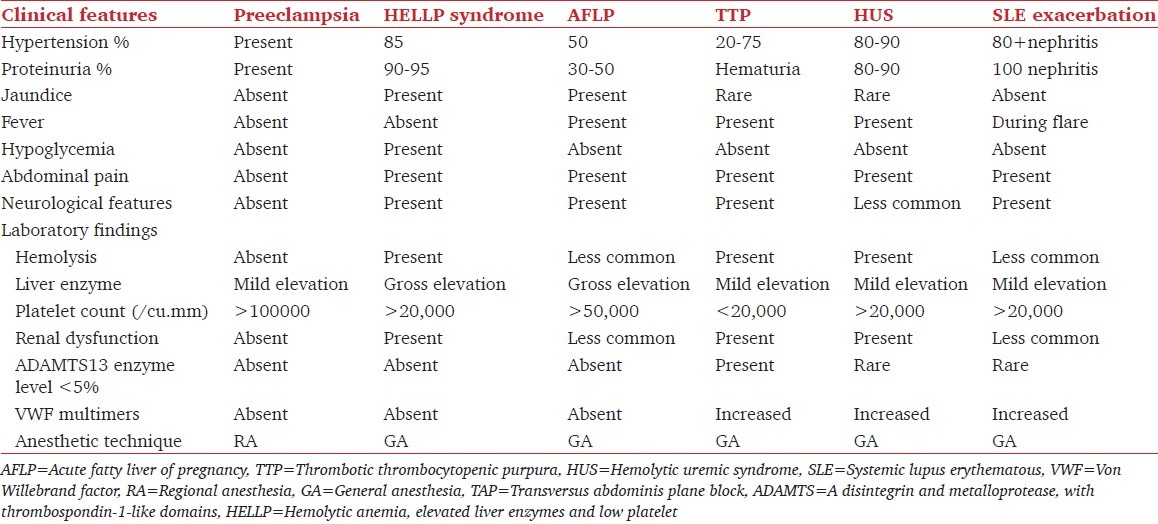
It is essential to understand the various medical and surgical conditions, which may mimic preeclampsia.[14] Similarly, preeclampsia can also be superimposed on one of these pathologies making the diagnosis more difficult [Table 3].
Table 3.
Differential diagnosis of preeclampsia and anesthetic implications[14]
Pathophysiology of Preeclampsia/Eclampsia
In normal pregnancy, the uterine blood flow is about 10% (500-600 ml/min) of cardiac output, with 80% of uterine blood flow normally supplying the placenta and the remaining 20% supplying the myometrium. In preeclampsia, there is an abnormal trophoblastic invasion of the maternal spiral arteries with impaired uteroplacental perfusion. There is a release of vasoactive factors into the maternal circulation, resulting in endothelial dysfunction, vasoconstriction and hypertension.[15] These parturients have an elevated thromboxane/prostacyclin ratio, factor VIII antigen and fibronectin prior to the onset of clinical manifestation.[16] Similarly, there is an exaggerated inflammatory response that affects every single organ in the body compared with normal pregnancy.[17] However, there is limited evidence to the role of nitric oxide in the pathophysiology and management of preeclampsia. The assessment of uterine arteries by Doppler studies has shown higher uterine artery resistance in preeclamptic parturients compared to normal parturients (RI = 0.59 [0.40-0.75] vs. 0.42 [0.3645 1]; P = 0.005).[18]
Effect of RA on Uteroplacental Blood Flow
Parturients admitted to the labor and delivery unit receive RA for labor analgesia, instrumental and operative deliveries. The commonly performed regional anesthetic techniques among parturients with preeclampsia include spinal anesthesia, epidural analgesia/anesthesia or combined spinal epidural (CSE) anesthesia.
Spinal anesthesia offers rapid onset, more reliable anesthetic with low local anesthetic (LA) requirement. Similarly, the addition of adjuvants prolongs the spinal anesthetic duration in addition to increased analgesic duration in the post-operative period. Hence, this technique has been widely used when these parturients present for cesarean section (CS) delivery. On the contrary, epidural analgesia/anesthesia offers top up doses, modification and extension of block through indwelling catheter with maintenance of hemodynamic stability compared to spinal anesthesia. The CSE anesthetic technique offers rapid onset, better quality of analgesia/anesthesia with the presence of epidural catheter allowing a top up for optimization and prolongation of spinal block. However, this technique is time consuming and technical difficulty is noted with inexperienced hands.
The administration of neuraxial anesthesia for labor or cesarean delivery reduces serum catecholamine level and improves uteroplacental blood flow. The sympathetic blockade that results from neuraxial anesthetic techniques has shown to improve intervillous blood flow in preeclamptic parturients by decreasing uteroplacental resistance.[19] In a study involving 10 parturients with preeclampsia and uterine flow abnormalities, a decrease in uterine artery resistance with the increase in uterine blood flow was described in parturients who received antepartum continuous epidural analgesia with 0.1% ropivacaine when compared to those preeclamptic parturients who did not receive epidural analgesia.[20] These physiologic effects of neuraxial anesthesia are potentially beneficial in preeclamptic states. The administration of labor epidural analgesia is associated with better neonatal acid base status compared to no analgesia and systemic opioids. Neuraxial techniques have been associated with better Apgar at 1 min and 5 min compared to systemic opioids; however, long-term effects on fetal brain development is not clear.[21]
Perinatal Outcome of Preeclamptic Parturients
Perinatal outcome in preeclampsia depends on the gestational age at onset, severity of the disease and preexisting medical conditions. The outcome is better in mild preeclampsia and with late onset (beyond 36 weeks) of gestation. On the contrary, with early-onset prior to 27 weeks of gestation, deterioration of maternal and fetal status is more often documented. In a retrospective analysis involving 46 severe preeclamptic parturients, a neonatal mortality rate of 57%, accompanied by a maternal complication rate of 30-67% were documented in parturients who were diagnosed with preeclampsia before 27 weeks of gestational age. Maternal morbidity was due to hemolytic anemia, elevated liver enzymes and low platelet count (HELLP) syndrome and placental abruption.[22]
Anesthetic Considerations for Labour Analgesia in Pregnancy-induced Hypertension
Neuraxial labor analgesic technique is considered as a gold standard technique for intrapartum labor analgesia. Its use has been greatly increased in recent years with better maternal and fetal outcomes. Epidural labor analgesia lowers maternal labor pain with higher satisfaction scores and has been shown to improve pulmonary and maternal cardiovascular physiology with better neonatal outcomes.[19,23,24] However, it is essential to rule out underlying coagulopathy or a significant drop in the trend of platelet count prior to performing neuraxial techniques.
Neuraxial labor epidural analgesia is provided through intermittent boluses, continuous infusion and patient controlled epidural analgesia (PCEA). PCEA is currently the standard of labor analgesic technique in North America and developed countries; it is well-accepted by parturients and obstetricians. In addition to continuous background infusion of LA, it allows the parturients to receive additional prefixed doses of epidural medication whenever they experience pain by pressing a demand button. A lock out time interval, which is set up during the infusion protects them from over dosage of LAs.[25,26,27]
In a retrospective analysis of 444 parturients with hypertensive disease, the administration of epidural labor analgesia did not increase the frequency of CS delivery, renal failure and pulmonary edema when compared with parturients who did not receive labor epidural analgesia.[28] Similarly, a meta-analysis involving 6700 parturients emphasized that there is no difference in the risk of CS delivery in women who received neuraxial labor analgesia versus systemic opioids (odds ratio: 1.03; 95% confidence interval 0.86-1.22).[29]
Anesthetic Considerations for Cesarean Delivery in PIH without HELLP Syndrome
The perioperative management of parturients with PIH presenting to labor and delivery suite has been described in Figure 1. Neuraxial anesthetic techniques are preferable to GA for elective cesarean delivery in the absence of HELLP syndrome. The provision of neuraxial anesthetic technique precludes the risk of aspiration, difficult and failed intubations, laryngoscopic response of intubation seen with general anesthetic techniques.
Figure 1.
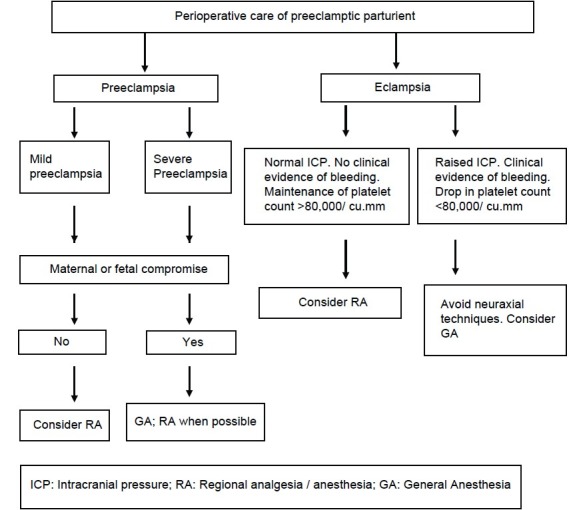
Perioperative care of parturient with preeclampsia
Spinal anesthesia
Spinal anesthesia is a generally preferred anesthetic technique as it is simple to perform; it provides rapid onset and a dense block. It also provides excellent post-operative analgesia when intrathecal opioids are used.[30,31,32] It has no effect on Apgar scores and umbilical artery pH in preeclampsia as along as the systolic blood pressure is maintained greater than 80% or more of the baseline.[33] The incidence of spinal induced hypotension and the vasopressor requirement were found to be two times lower in preeclamptic parturients when compared with normal parturients undergoing CS delivery.[34,35] The increased production of circulating factors with potent pressor effect and the increased sensitivity to vasopressor drugs in preeclampsia along with the use of hyperbaric bupivacaine (8-12 mg) with opioids could decrease the spinal induced hypotension in preeclamptic parturients.[34] Cardiac output monitoring after spinal anesthesia has shown that neither spinal anesthesia nor the use of phenylephrine to treat hypotension reduce cardiac output during CS delivery, further supporting its safety in preeclamptic parturients.[36]
Continuous spinal anesthesia offers the flexibility of titration of local anesthetic agents in small aliquots; thus, graded sympathetic block could be achieved with a lower degree of sympathectomy in these parturients.[37] However, the higher rate of infection, injury to nerve roots, postdural puncture headache and technical difficulty are potential pitfalls and this technique is not frequently used.[38,39]
Epidural anesthesia
Epidural anesthesia may be instituted in a step like fashion for non-emergency CS delivery with an infusion of 500-1000 ml intravenous crystalloid that will sufficiently minimize maternal hypotension just as with non-preeclamptic patients. In our institute, we administer incremental dose of 0.5% bupivacaine (3 ml) in a dose sufficient to obtain a T8/T10 dermatomal sensory level of analgesia with monitoring of maternal vital signs and fetal heart rate tracing. Once the epidural catheter has been proven functional with stable maternal hemodynamics and fetal heart rate tracing, surgical anesthesia may then be achieved to the T4 sensory dermatome necessary for cesarean delivery. In a prospective observational study involving 12 preeclamptic parturients undergoing elective cesarean delivery, preloading with crystalloids has not shown to decrease the incidence of maternal hypotension and changes in the uterine artery velocity waveforms were minimal when maternal systolic blood pressure were maintained 80% or more of baseline.[33] Similarly, in a recent retrospective review comparing two tertiary referral obstetric units has shown that preeclamptic parturients with liberal fluid administration had a higher incidence of acute pulmonary edema over parturients with restricted fluid administration during the perioperative period.[40] The use of fentanyl (>2 mcg/kg), a rapid and short-acting opioid, may increase the rapid onset and prolong the duration of anesthesia. The use of epinephrine-containing LAs has not shown altered Apgar scores and or umbilical blood gases.[41]
Combined spinal epidural anesthesia
CSE provides the reliability of spinal anesthesia and at the same time the flexibility of good postoperative pain relief through an epidural catheter infusion.[30,42] The epidural component of the CSE offers superior hemodynamic stability over spinal anesthesia. There is no difference in neonatal outcome between spinal and epidural anesthetic techniques.[43]
A small prospective, randomized study involving 30 women with severe preeclampsia undergoing elective cesarean delivery, the CSE technique was found to be a safe alternative to conventional epidural anesthesia.[44] In a prospective study involving 28 severe preeclamptic parturients undergoing elective cesarean delivery, a dose of intrathecal bupivacaine 7.5 mg with fentanyl 25 mcg was found to maintain better hemodynamic stability over parturients who had 10 mg of intrathecal bupivacaine with fentanyl 25 mcg and it was equally effective for elective CS delivery.[45] In a recent study involving 18 preeclamptic and normal parturients undergoing CS delivery, the ED50 of intrathecal bupivacaine was similar in both groups (4.7 mg of bupivacaine + 20 ug of fentanyl).[46]
Uneventful spinal anesthesia for elective cesarean delivery in severe preeclamptic parturients has been administered using bupivacaine in a dose range of 8-12.5 mg along with opioids including morphine 100 mcg, fentanyl 10-25 mcg and sufentanil 3-5 mcg.[34,35,43,47]
Anesthetic Considerations for Cesarean Delivery in PIH with HELLP Syndrome
Severe preeclampsia with HELLP syndrome poses a significant anesthetic challenge. Coagulopathy in these parturients s usually due to low platelet count and, less commonly, disseminated intravascular coagulation. The presence of coagulopathy precludes the provision of RA for CS delivery. Studies investigating coagulation in these parturients using thromboelastography described that there were no coagulopathies with the platelet count greater than 1,00,000/mm3. However, prompt coagulation evaluation is recommended with the platelet count less than 1,00,000/mm3.[48]
Similarly, the drop in trends of platelet count predisposes them at the risk epidural hematoma with neuraxial anesthetic technique. The current guidelines recommending a platelet count more than 100,000/mm3 to minimize the risk of epidural hematoma is of limited evidence.[49] The safe administration of neuraxial anesthetic techniques in parturients with platelet counts less than 100,000/mm3 has been reported.[50,51] Reported incidence of spinal hematoma in HELLP syndrome patients receiving regional techniques is negligible.[52] The incidence of spinal hematomas was highest in female orthopedic patients undergoing knee arthroplasty.[53] A survey on the incidence of severe neurological complications after neuraxial block showed a higher incidence (33/127) of spinal hematoma, out of which 2 were in HELLP syndrome patients. In a retrospective review of the incidence of spinal hematoma in parturients with HELLP syndrome has shown that safe administration of neuraxial anesthetic technique may be provided with a platelet count of 90,000/mm3 or more with a low threshold of GA with the platelet count of 60,000/mm3. The anesthetic technique may be decided at the discretion of anesthesiologist, urgency of CS delivery in parturients with the platelet count between 60,000 and 90,000/mm3.[54]
When GA is considered, rapid sequence intubation with the availability of difficult airway cart and drugs to control blood pressure may minimize the complications associated with GA. Drugs that are used to attenuate hemodynamic response to intubation include esmolol, fentanyl, remifentanil, alfentanil and lidocaine. However, it is up to the discretion of attending anesthesiologist to use the drug (s) with which they are most familiar.
Anesthetic Considerations for Emergency Cesarean Delivery
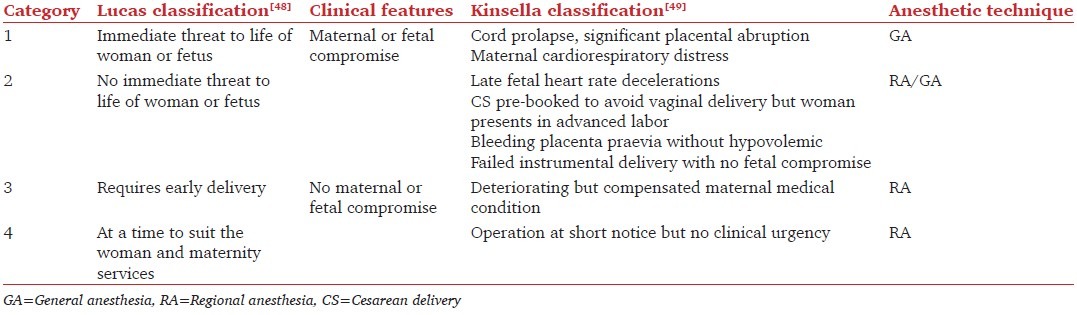
The anesthetic management of preeclamptic patients requiring emergency CS delivery depends on the severity of preeclampsia and maternal/fetal status. Parturients are classified into four categories depending on the urgency of delivery, maternal and fetal status during delivery [Table 4].[55,56]
Table 4.
Classification of urgency of cesarean delivery
General anesthesia
When there is an immediate threat to the mother or fetus [Category 1], GA with rapid sequence intubation may be considered over RA due to its rapid onset of anesthesia, control over the airway and potential for less hypotension than RA. However, a high degree of anticipation of difficult endotracheal intubation must be considered due to increased airway edema, short neck and large breasts that can obscure the laryngoscopic view during intubation. It is essential to keep the difficult airway cart available while planning GA. Similarly, with the pre-existing elevated blood pressure, techniques to attenuate the hemodynamic response to intubation with minimal effects on the fetus should be considered. The administration of magnesium sulfate pre-operatively could potentiate the duration of action and sensitivity of succinylcholine. Similarly, the uterine atony and coagulopathy from magnesium therapy may cause considerable intrapartum blood loss. Hence, a wide-bore intravenous access and blood products should be kept available prior to anesthesia.[41] The triennium report from the Center for Maternal and Child Enquiries, reported two cases of direct anesthetic deaths on administration of GA to parturients due to failure to ventilate the lungs and aspiration of gastric contents in the postoperative period.[57]
When there is a maternal or fetal compromise without any threat to either of them [Category 2], the management depends on the availability of time to perform or activate RA. The clinical assessment of maternal and fetal status along with a clear communication with the obstetrical team may play a vital role in the decision of the anesthetic technique. With the availability of time and no threat to either mother or fetus, an epidural top up of a pre-existing epidural catheter with rapid acting LA or a subarachnoid block with low dose LA and opioid may be considered. On the contrary, when there is a threat to mother or fetus with insufficient time to perform a regional anesthetic technique, GA with perioperative precautions may be considered over regional anesthetic technique.
Subarachnoid block with intrathecal opioid or CSE anesthetic technique may be considered over GA when there is no maternal or fetal compromise [Categories 3 and 4]. The administration of neuraxial anesthesia minimizes the risk of neonatal exposure to potentially depressant anesthetic drugs, decreases the risk of maternal pulmonary aspiration, promotes early ambulation and reduces the incidence of maternal thromboembolism. Similarly, the administration of titrated opioids along with LA during neuraxial anesthetic techniques offers postoperative analgesia and minimizes the consumption of systemic opioids.
The safety of spinal, epidural and CSE anesthesia for CS delivery in women with pre eclampsia has been described.[29,30,31,57] In a population based study involving 303,862 women who had undergone CS delivery, 8567 parturients had preeclampsia. In this study, GA for CS delivery was associated with an increased risk of maternal stroke when compared with neuraxial anesthesia in preeclamptic women.[58] In a retrospective study involving 116 preeclamptic parturients undergoing caesarean delivery, the authors described that a higher rate of neonatal asphyxia was noticed when GA was administered for CS delivery when compared with RA (P = 0.0006).[59] Similarly, the neonatal base deficit was significantly higher in severe preeclamptic parturients who had GA for CS delivery when compared to parturients who had spinal anesthesia.[60]
Transversus abdominis plane block
The TAP block, when used as part of a multimodal analgesic regimen, resulted in better analgesia and decreased supplemental opioid consumption after cesarean delivery. TAP block is a regional anesthetic technique that blocks T6-L1 nerve roots and can provide analgesia for lower abdominal procedures.[61] The administration of effective postoperative analgesia is of key importance in such parturients to facilitate early ambulation, child care including breast feeding, bonding of an infant to mother and prevention of postoperative morbidity.[62]
In a randomized controlled trial (RCT) involving 50 parturients undergoing CS delivery, bilateral TAP block using ropivacaine at the dose of 1.5 mg/kg has shown significant reduction of morphine consumption (66 ± 26 vs. 18 ± 14 mg, P > 0.001) in the first 48 h after surgery when compared to placebo.[63] In a recent meta-analysis involving 524 parturients undergoing elective CS delivery, the administration of TAP block significantly improved postoperative analgesia in women undergoing CS delivery who did not receive intrathecal morphine (ITM) and the value of TAP block in patients receiving ITM was not clear.[64]
Role of Ultrasound in Parturients Undergoing Neuraxial Procedures
Neuraxial regional anesthetic techniques are performed usually by palpating anatomical land marks.[65,66,67] The increase in weight gain along with edema secondary to preeclampsia may obscure anatomical landmarks and pose a technical challenge to obstetric anesthesiologists as the anatomical level may not be correlated accurately in these parturients. The use of ultrasound may be useful in identifying the landmarks and predicting the depth of the epidural space.[68]
Currently, there are prospective trials on the effectiveness of ultrasound in parturients. Imaging of the lumbar spine can be performed in both transverse and longitudinal planes. The transverse scanning of lumbar epidural space prior to the neuraxial block reliably predicts the needle insertion point and epidural space.[69,70] In an RCT of 300 parturients to assess the efficacy of ultrasound in labor epidural anesthesia, the use of ultrasound reduced the rate of puncture attempts significantly (P > 0.013). Similarly, the rate of dural puncture, aspiration of blood and development of postdural puncture headache were significantly lower in parturients who had prior scanning of the lumbar spine when compared with those parturients who were not scanned prior to neuraxial technique.[71] The visualization of the epidural space along with manipulation of needle directions is better appreciated with real time ultrasound over offline scanning of spine. High rate of accuracy with a lower number of attempts were described with real time ultrasound over offline scanning techniques.[72]
Complications of Neuraxial Technique in Preeclamptic Parturients
The risk of epidural hematoma must be weighed against the benefits of RA in women of preeclampsia, including better analgesia, decreased circulating catecholamines and improved uteroplacental perfusion. The true incidence of spinal hematoma following central neuraxial blockade in parturients is not well-documented and with under-reporting, it may well be higher than the estimated incidence.[73] The estimated incidence is 1 in 150,000 following epidural anesthesia and 1 in 220,000 after spinal anesthesia in the non-obstetric population.[74,75] In a retrospective analysis over 10 year period involving 1,260,000 spinal anesthesia and 4,50000 epidural anesthesia, the incidence of spinal epidural hematoma was documented to be 1:5400 in orthopedic patients as opposed to 1:200,000 in obstetrics. The obstetric epidural hematomas occurred in parturients with HELLP syndrome rather than in mild preeclampsia.[53] The engorged epidural venous plexus along with low platelet count in preeclamptic parturients predispose them to a higher risk of hematoma. Epidural hematoma causing paralysis in the immediate postoperative period has been described with preoperative platelet count of 71,000/mm3 in a parturient with preeclampsia after epidural anesthesia. This parturient recovered without any neurological deficit with early surgical intervention.[73] Hence, the performance of neuraxial anesthetic techniques in such high risk parturients with platelet count of 80,000/cu.mm and above may minimize the risk of hematoma and it is advisable to follow the trend of platelet count along with clinical signs of toxemia prior to neuraxial techniques.
Neuraxial anesthetic techniques may be avoided in pregnancy induced hypertension if there is concomitant thrombocytopenia and coagulopathy. About 30-50% cases of severe preeclamptic parturients have associated thrombocytopenia.[76] In a retrospective analysis of 100 preeclamptic parturients, 8% of parturients were found to have both thrombocytopenia and prolonged activated partial thromboplastin time (aPTT). The authors recommended that it was practical and cost-effective to screen for both platelet count and aPTT.[77]
Conclusions
Parturients with mild preeclampsia may safely undergo regional anesthetic procedures for labor analgesia and CS delivery. A thorough evaluation to detect underlying coagulopathy or thrombocytopenia is essential prior to considering regional anesthetic procedures in severe preeclamptic parturients. It may be safer to consider non-neuraxial techniques in eclamptic parturients with or without end organ damage.
Acknowledgment
The authors acknowledge Dr. Koshkin Arkady, Research fellow, Toronto Western Hospital, Toronto for his editorial assistance.
Footnotes
Source of Support: Department of Anesthesia, Toronto Western Hospital, University Health Network, University of Toronto, Toronto, Canada.
Conflict of Interest: None declared.
References
- 1.ACOG Committee on Practice Bulletins - Obstetrics. ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33. 2002 Jan;99:159–67. doi: 10.1016/s0029-7844(01)01747-1. [DOI] [PubMed] [Google Scholar]
- 2.Ness RB, Roberts JM. Epidemiology of hypertension. In: Lindheimer MD, Roberts JM, Cunningham FG, editors. Chesley's Hypertensive Disorders in Pregnancy. 2nd ed. Stamford Connecticut: Appleton and Lange; 1999. pp. 43–65. [Google Scholar]
- 3.Villar J, Say L, Gulmezoglu AM, Marialdi M, Lindheimer MD, Betran AP, et al. Pre-eclampsia eclampsia: a health problem for 2000 years. In: Critchly H, MacLean A, Poston L, Walker J, editors. Pre-eclampsia. London England: RCOG Press; 2003. pp. 189–207. [Google Scholar]
- 4.Duley L. Pre-eclampsia and the hypertensive disorders of pregnancy. Br Med Bull. 2003;67:161–76. doi: 10.1093/bmb/ldg005. [DOI] [PubMed] [Google Scholar]
- 5.Lawes EG, Downing JW, Duncan PW, Bland B, Lavies N, Gane GA. Fentanyl-droperidol supplementation of rapid sequence induction in the presence of severe pregnancy-induced and pregnancy-aggravated hypertension. Br J Anaesth. 1987;59:1381–91. doi: 10.1093/bja/59.11.1381. [DOI] [PubMed] [Google Scholar]
- 6.Loughran PG, Moore J, Dundee JW. Maternal stress response associated with caesarean delivery under general and epidural anaesthesia. Br J Obstet Gynaecol. 1986;93:943–9. doi: 10.1111/j.1471-0528.1986.tb08013.x. [DOI] [PubMed] [Google Scholar]
- 7.Gin T, O’Meara ME, Kan AF, Leung RK, Tan P, Yau G. Plasma catecholamines and neonatal condition after induction of anaesthesia with propofol or thiopentone at caesarean section. Br J Anaesth. 1993;70:311–6. doi: 10.1093/bja/70.3.311. [DOI] [PubMed] [Google Scholar]
- 8.Shnider SM, Wright RG, Levinson G, Roizen MF, Wallis KL, Rolbin SH, et al. Uterine blood flow and plasma norepinephrine changes during maternal stress in the pregnant ewe. Anesthesiology. 1979;50:524–7. doi: 10.1097/00000542-197906000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Jouppila P, Kuikka J, Jouppila R, Hollmén A. Effect of induction of general anesthesia for cesarean section on intervillous blood flow. Acta Obstet Gynecol Scand. 1979;58:249–53. doi: 10.3109/00016347909154043. [DOI] [PubMed] [Google Scholar]
- 10.Report of the national high blood pressure education program working group on high blood pressure in pregnancy. Am J Obstet Gynecol. 2000;183:S1–S22. [PubMed] [Google Scholar]
- 11.Cunningham FG, Leveno KL, Bloom SL, Hauth JC, Gilstrap LC, Wenstrom KD. Williams Obstetrics. 22nd ed. New York: McGraw-Hill Co; 2005. p. 1237. [Google Scholar]
- 12.Lindheimer MD, Conrad KP, Karumanchi SA. Renal physiology and disease in pregnancy. In: Alpern RJ, Hebert SC, editors. Seldin and Giebisch's the Kidney; Physiology and Pathophysiology. 4th ed. San Diego California: Academic Press Elsevier; 2008. pp. 2339–98. [Google Scholar]
- 13.Weinstein L. Syndrome of hemolysis, elevated liver enzymes, and low platelet count: A severe consequence of hypertension in pregnancy. Am J Obstet Gynecol. 1982;142:159–67. doi: 10.1016/s0002-9378(16)32330-4. [DOI] [PubMed] [Google Scholar]
- 14.Sibai BM. Imitators of severe pre-eclampsia/eclampsia. Clin Perinatol. 2004;31:835–52. doi: 10.1016/j.clp.2004.06.007. vii. [DOI] [PubMed] [Google Scholar]
- 15.Poston L. Maternal vascular function in pregnancy. J Hum Hypertens. 1996;10:391–4. [PubMed] [Google Scholar]
- 16.Rappaport VJ, Hirata G, Yap HK, Jordan SC. Anti-vascular endothelial cell antibodies in severe preeclampsia. Am J Obstet Gynecol. 1990;162:138–46. doi: 10.1016/0002-9378(90)90836-v. [DOI] [PubMed] [Google Scholar]
- 17.Redman CW, Sacks GP, Sargent IL. Preeclampsia: An excessive maternal inflammatory response to pregnancy. Am J Obstet Gynecol. 1999;180:499–506. doi: 10.1016/s0002-9378(99)70239-5. [DOI] [PubMed] [Google Scholar]
- 18.Simmons LA, Hennessy A, Gillin AG, Jeremy RW. Uteroplacental blood flow and placental vascular endothelial growth factor in normotensive and pre-eclamptic pregnancy. BJOG. 2000;107:678–85. doi: 10.1111/j.1471-0528.2000.tb13312.x. [DOI] [PubMed] [Google Scholar]
- 19.Jouppila R, Hollmén A. The effect of segmental epidural analgesia on maternal and foetal acid-base balance, lactate, serum potassium and creatine phosphokinase during labour. Acta Anaesthesiol Scand. 1976;20:259–68. doi: 10.1111/j.1399-6576.1976.tb05038.x. [DOI] [PubMed] [Google Scholar]
- 20.Ginosar Y, Nadjari M, Hoffman A, Firman N, Davidson EM, Weiniger CF, et al. Antepartum continuous epidural ropivacaine therapy reduces uterine artery vascular resistance in pre-eclampsia: A randomized, dose-ranging, placebo-controlled study. Br J Anaesth. 2009;102:369–78. doi: 10.1093/bja/aen402. [DOI] [PubMed] [Google Scholar]
- 21.Reynolds F. Labour analgesia and the baby: Good news is no news. Int J Obstet Anesth. 2011;20:38–50. doi: 10.1016/j.ijoa.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Bombrys AE, Barton JR, Nowacki EA, Habli M, Pinder L, How H, et al. Expectant management of severe preeclampsia at less than 27 weeks’ gestation: Maternal and perinatal outcomes according to gestational age by weeks at onset of expectant management. Am J Obstet Gynecol. 2008;199:247. doi: 10.1016/j.ajog.2008.06.086. e1-6. [DOI] [PubMed] [Google Scholar]
- 23.Lederman RP, Lederman E, Work B, Jr, McCann DS. Anxiety and epinephrine in multiparous women in labor: Relationship to duration of labor and fetal heart rate pattern. Am J Obstet Gynecol. 1985;153:870–7. doi: 10.1016/0002-9378(85)90692-1. [DOI] [PubMed] [Google Scholar]
- 24.Shnider SM, Abboud TK, Artal R, Henriksen EH, Stefani SJ, Levinson G. Maternal catecholamines decrease during labor after lumbar epidural anesthesia. Am J Obstet Gynecol. 1983;147:13–5. doi: 10.1016/0002-9378(83)90076-5. [DOI] [PubMed] [Google Scholar]
- 25.Campbell DC, Zwack RM, Crone LA, Yip RW. Ambulatory labor epidural analgesia: Bupivacaine versus ropivacaine. Anesth Analg. 2000;90:1384–9. doi: 10.1097/00000539-200006000-00023. [DOI] [PubMed] [Google Scholar]
- 26.Fettes PD, Moore CS, Whiteside JB, McLeod GA, Wildsmith JA. Intermittent vs continuous administration of epidural ropivacaine with fentanyl for analgesia during labour. Br J Anaesth. 2006;97:359–64. doi: 10.1093/bja/ael157. [DOI] [PubMed] [Google Scholar]
- 27.Collis RE, Plaat FS, Morgan BM. Comparison of midwife top-ups, continuous infusion and patient-controlled epidural analgesia for maintaining mobility after a low-dose combined spinal-epidural. Br J Anaesth. 1999;82:233–6. doi: 10.1093/bja/82.2.233. [DOI] [PubMed] [Google Scholar]
- 28.Hogg B, Hauth JC, Caritis SN, Sibai BM, Lindheimer M, Van Dorsten JP, et al. Safety of labor epidural anesthesia for women with severe hypertensive disease. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Am J Obstet Gynecol. 1999;181:1096–101. doi: 10.1016/s0002-9378(99)70088-8. [DOI] [PubMed] [Google Scholar]
- 29.Halpern SH, Leighton BL. Epidural analgesia and the progress of labor. In: Halpern SH, Douglas MJ, editors. Evidence-Based Obstetric Anesthesia. Oxford UK: Blackwell; 2005. pp. 10–22. [Google Scholar]
- 30.Sia AT, Fun WL, Tan TU. The ongoing challenges of regional and general anaesthesia in obstetrics. Best Pract Res Clin Obstet Gynaecol. 2010;24:303–12. doi: 10.1016/j.bpobgyn.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 31.Gogarten W. Spinal anaesthesia for obstetrics. Best Pract Res Clin Anaesthesiol. 2003;17:377–92. doi: 10.1016/s1521-6896(02)00116-7. [DOI] [PubMed] [Google Scholar]
- 32.Burns SM, Cowan CM. Spinal anaesthesia for caesarean section: Current clinical practice. Hosp Med. 2000;61:855–8. doi: 10.12968/hosp.2000.61.12.1485. [DOI] [PubMed] [Google Scholar]
- 33.Karinen J, Räsänen J, Alahuhta S, Jouppila R, Jouppila P. Maternal and uteroplacental haemodynamic state in pre-eclamptic patients during spinal anaesthesia for Caesarean section. Br J Anaesth. 1996;76:616–20. doi: 10.1093/bja/76.5.616. [DOI] [PubMed] [Google Scholar]
- 34.Aya AG, Mangin R, Vialles N, Ferrer JM, Robert C, Ripart J, et al. Patients with severe preeclampsia experience less hypotension during spinal anesthesia for elective cesarean delivery than healthy parturients: A prospective cohort comparison. Anesth Analg. 2003;97:867–72. doi: 10.1213/01.ANE.0000073610.23885.F2. [DOI] [PubMed] [Google Scholar]
- 35.Aya AG, Vialles N, Tanoubi I, Mangin R, Ferrer JM, Robert C, et al. Spinal anesthesia-induced hypotension: A risk comparison between patients with severe preeclampsia and healthy women undergoing preterm cesarean delivery. Anesth Analg. 2005;101:869–75. doi: 10.1213/01.ANE.0000175229.98493.2B. [DOI] [PubMed] [Google Scholar]
- 36.Dyer RA, Piercy JL, Reed AR, Lombard CJ, Schoeman LK, James MF. Hemodynamic changes associated with spinal anesthesia for cesarean delivery in severe preeclampsia. Anesthesiology. 2008;108:802–11. doi: 10.1097/01.anes.0000311153.84687.c7. [DOI] [PubMed] [Google Scholar]
- 37.Dresner M, Pinder A. Anaesthesia for caesarean section in women with complex cardiac disease: 34 cases using the Braun Spinocath spinal catheter. Int J Obstet Anesth. 2009;18:131–6. doi: 10.1016/j.ijoa.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 38.Arkoosh VA, Palmer CM, Yun EM, Sharma SK, Bates JN, Wissler RN, et al. A randomized, double-masked, multicenter comparison of the safety of continuous intrathecal labor analgesia using a 28-gauge catheter versus continuous epidural labor analgesia. Anesthesiology. 2008;108:286–98. doi: 10.1097/01.anes.0000299429.52105.e5. [DOI] [PubMed] [Google Scholar]
- 39.Drasner K, Smiley R. Continuous spinal analgesia for labor and delivery: A born-again technique? Anesthesiology. 2008;108:184–6. doi: 10.1097/01.anes.0000299427.33729.69. [DOI] [PubMed] [Google Scholar]
- 40.Thornton CE, von Dadelszen P, Makris A, Tooher JM, Ogle RF, Hennessy A. Acute pulmonary oedema as a complication of hypertension during pregnancy. Hypertens Pregnancy. 2011;30:169–79. doi: 10.3109/10641950902972140. [DOI] [PubMed] [Google Scholar]
- 41.Weitzner RM, Malinow AM. The eclamptic patient-Anesthestic management. Anaesthesiol Clin. 1998;16:323–30. [Google Scholar]
- 42.Lew E, Yeo SW, Thomas E. Combined spinal-epidural anesthesia using epidural volume extension leads to faster motor recovery after elective cesarean delivery: A prospective, randomized, double-blind study. Anesth Analg. 2004;98:810–4. doi: 10.1213/01.ane.0000101987.79454.bc. [DOI] [PubMed] [Google Scholar]
- 43.Visalyaputra S, Rodanant O, Somboonviboon W, Tantivitayatan K, Thienthong S, Saengchote W. Spinal versus epidural anesthesia for cesarean delivery in severe preeclampsia: A prospective randomized, multicenter study. Anesth Analg. 2005;101:862–8. doi: 10.1213/01.ANE.0000160535.95678.34. [DOI] [PubMed] [Google Scholar]
- 44.Berends N, Teunkens A, Vandermeersch E, Van de Velde M. A randomized trial comparing low-dose combined spinal-epidural anesthesia and conventional epidural anesthesia for cesarean section in severe preeclampsia. Acta Anaesthesiol Belg. 2005;56:155–62. [PubMed] [Google Scholar]
- 45.Jain K, Makkar JK, Yadanappudi S, Anbarasan I, Gander S. Two doses of spinal bupivacaine for caesarean delivery in severe preeclampsia: A pilot study. Int J Obstet Anesth. 2012;21:195–6. doi: 10.1016/j.ijoa.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 46.Tyagi A, Kakkar A, Kumar S, Sethi AK, Salhotra R. ED50 of hyperbaric bupivacaine with fentanyl for cesarean delivery under combined spinal epidural in normotensive and preeclamptic patients. Reg Anesth Pain Med. 2012;37:40–4. doi: 10.1097/AAP.0b013e318233c5f5. [DOI] [PubMed] [Google Scholar]
- 47.Hood DD, Curry R. Spinal versus epidural anesthesia for cesarean section in severely preeclamptic patients: A retrospective survey. Anesthesiology. 1999;90:1276–82. doi: 10.1097/00000542-199905000-00009. [DOI] [PubMed] [Google Scholar]
- 48.Sharma SK, Philip J, Whitten CW, Padakandla UB, Landers DF. Assessment of changes in coagulation in parturients with preeclampsia using thromboelastography. Anesthesiology. 1999;90:385–90. doi: 10.1097/00000542-199902000-00009. [DOI] [PubMed] [Google Scholar]
- 49.Bromage PR. Shnider SM, Levinson G. Anesthesia for Obstetrics. 3rd ed. Baltimore: Williams and Wilkins; 1993. Neurologic complications of regional anesthesia for obstetrics; pp. 443–4. [Google Scholar]
- 50.Beilin Y, Zahn J, Comerford M. Safe epidural analgesia in thirty parturients with platelet counts between 69,000 and 98,000 mm(-3) Anesth Analg. 1997;85:385–8. doi: 10.1097/00000539-199708000-00025. [DOI] [PubMed] [Google Scholar]
- 51.Frenk V, Camann W, Shankar KB. Regional anesthesia in parturients with low platelet counts. Can J Anaesth. 2005;52:114. doi: 10.1007/BF03018594. [DOI] [PubMed] [Google Scholar]
- 52.Vigil-De Gracia P, Silva S, Montufar C, Carrol I, De Los Rios S. Anesthesia in pregnant women with HELLP syndrome. Int J Gynaecol Obstet. 2001;74:23–7. doi: 10.1016/s0020-7292(01)00390-3. [DOI] [PubMed] [Google Scholar]
- 53.Moen V, Dahlgren N, Irestedt L. Severe neurological complications after central neuraxial blockades in Sweden 1990-1999. Anesthesiology. 2004;101:950–9. doi: 10.1097/00000542-200410000-00021. [DOI] [PubMed] [Google Scholar]
- 54.Khellaf M, Loustau V, Bierling P, Michel M, Godeau B. Thrombocytopenia and pregnancy. Rev Med Interne. 2012;33:446–52. doi: 10.1016/j.revmed.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 55.Lucas DN, Yentis SM, Kinsella SM, Holdcroft A, May AE, Wee M, et al. Urgency of caesarean section: A new classification. J R Soc Med. 2000;93:346–50. doi: 10.1177/014107680009300703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kinsella SM, Scrutton MJ. Assessment of a modified four-category classification of urgency of caesarean section. J Obstet Gynaecol. 2009;29:110–3. doi: 10.1080/01443610802585546. [DOI] [PubMed] [Google Scholar]
- 57.Cantwell R, Clutton-Brock T, Cooper G, Dawson A, Drife J, Garrod D, et al. Saving mothers’ lives: Reviewing maternal deaths to make motherhood safer: 2006-2008. The eighth report of the confidential enquiries into maternal deaths in the United Kingdom. BJOG. 2011;118(Suppl 1):1–203. doi: 10.1111/j.1471-0528.2010.02847.x. [DOI] [PubMed] [Google Scholar]
- 58.Huang CJ, Fan YC, Tsai PS. Differential impacts of modes of anaesthesia on the risk of stroke among preeclamptic women who undergo caesarean delivery: A population-based study. Br J Anaesth. 2010;105:818–26. doi: 10.1093/bja/aeq266. [DOI] [PubMed] [Google Scholar]
- 59.Ajuzieogu OV, Ezike HA, Amucheazi AO, Enwereji J. A retrospective study of the outcome of cesarean section for women with severe pre-eclampsia in a third world setting. Saudi J Anaesth. 2011;5:15–8. doi: 10.4103/1658-354X.76480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dasgupta S, Chakraborty B, Saha D, Ghosh D. Comparison of neonatal outcome in women with severe pre-eclampsia undergoing caesarean section under spinal or general anaesthesia. J Indian Med Assoc. 2011;109:166–70. [PubMed] [Google Scholar]
- 61.McDonnell JG, O’Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: A prospective randomized controlled trial. Anesth Analg. 2007;104:193–7. doi: 10.1213/01.ane.0000250223.49963.0f. [DOI] [PubMed] [Google Scholar]
- 62.Farragher RA, Laffey JG. Postoperative pain management following cesarean section. In: Shorten G, Carr D, Harmon D, editors. Postoperative pain management: an evidence-based guide to practice. 1st ed. Philadelphia PA: Saunders Elsevier; 2006. pp. 225–38. [Google Scholar]
- 63.McDonnell JG, Curley G, Carney J, Benton A, Costello J, Maharaj CH, et al. The analgesic efficacy of transversus abdominis plane block after cesarean delivery: A randomized controlled trial. Anesth Analg. 2008;106:186–91. doi: 10.1213/01.ane.0000290294.64090.f3. [DOI] [PubMed] [Google Scholar]
- 64.Mishriky BM, George RB, Habib AS. Transversus abdominis plane block for analgesia after cesarean delivery: A systematic review and meta-analysis. Can J Anaesth. 2012;59:766–78. doi: 10.1007/s12630-012-9729-1. [DOI] [PubMed] [Google Scholar]
- 65.Pysyk CL, Persaud D, Bryson GL, Lui A. Ultrasound assessment of the vertebral level of the palpated intercristal (Tuffier's) line. Can J Anaesth. 2010;57:46–9. doi: 10.1007/s12630-009-9208-5. [DOI] [PubMed] [Google Scholar]
- 66.Broadbent CR, Maxwell WB, Ferrie R, Wilson DJ, Gawne-Cain M, Russell R. Ability of anaesthetists to identify a marked lumbar interspace. Anaesthesia. 2000;55:1122–6. doi: 10.1046/j.1365-2044.2000.01547-4.x. [DOI] [PubMed] [Google Scholar]
- 67.Margarido CB, Mikhael R, Arzola C, Balki M, Carvalho JC. The intercristal line determined by palpation is not a reliable anatomical landmark for neuraxial anesthesia. Can J Anaesth. 2011;58:262–6. doi: 10.1007/s12630-010-9432-z. [DOI] [PubMed] [Google Scholar]
- 68.Chin KJ, Karmakar MK, Peng P. Ultrasonography of the adult thoracic and lumbar spine for central neuraxial blockade. Anesthesiology. 2011;114:1459–85. doi: 10.1097/ALN.0b013e318210f9f8. [DOI] [PubMed] [Google Scholar]
- 69.Balki M. Locating the epidural space in obstetric patients-ultrasound a useful tool: Continuing professional development. Can J Anaesth. 2010;57:1111–26. doi: 10.1007/s12630-010-9397-y. [DOI] [PubMed] [Google Scholar]
- 70.Balki M, Lee Y, Halpern S, Carvalho JC. Ultrasound imaging of the lumbar spine in the transverse plane: The correlation between estimated and actual depth to the epidural space in obese parturients. Anesth Analg. 2009;108:1876–81. doi: 10.1213/ane.0b013e3181a323f6. [DOI] [PubMed] [Google Scholar]
- 71.Grau T, Leipold RW, Conradi R, Martin E, Motsch J. Efficacy of ultrasound imaging in obstetric epidural anesthesia. J Clin Anesth. 2002;14:169–75. doi: 10.1016/s0952-8180(01)00378-6. [DOI] [PubMed] [Google Scholar]
- 72.Grau T, Leipold RW, Fatehi S, Martin E, Motsch J. Real-time ultrasonic observation of combined spinal-epidural anaesthesia. Eur J Anaesthesiol. 2004;21:25–31. doi: 10.1017/s026502150400105x. [DOI] [PubMed] [Google Scholar]
- 73.Yuen TS, Kua JS, Tan IK. Spinal haematoma following epidural anaesthesia in a patient with eclampsia. Anaesthesia. 1999;54:350–4. doi: 10.1046/j.1365-2044.1999.00705.x. [DOI] [PubMed] [Google Scholar]
- 74.Tryba M. Epidural regional anesthesia and low molecular heparin: Pro. Anasthesiol Intensivmed Notfallmed Schmerzther. 1993;28:179–81. doi: 10.1055/s-2007-998902. [DOI] [PubMed] [Google Scholar]
- 75.Stafford-Smith M. Impaired haemostasis and regional anaesthesia. Can J Anaesth. 1996;43:R129–41. doi: 10.1007/BF03011675. [DOI] [PubMed] [Google Scholar]
- 76.Valera MC, Parant O, Vayssiere C, Arnal JF, Payrastre B. Physiologic and pathologic changes of platelets in pregnancy. Platelets. 2010;21:587–95. doi: 10.3109/09537104.2010.509828. [DOI] [PubMed] [Google Scholar]
- 77.Metz J, Cincotta R, Francis M, DeRosa L, Balloch A. Screening for consumptive coagulopathy in preeclampsia. Int J Gynaecol Obstet. 1994;46:3–9. doi: 10.1016/0020-7292(94)90301-8. [DOI] [PubMed] [Google Scholar]


