Abstract
Background:
Paravertebral and inter pleural blocks (IPB) reduce post-operative pain and decrease the effect of post-operative pain on lung functions after breast surgery. This study was designed to determine their effect on lung functions and post-operative pain in patients undergoing modified radical mastectomy.
Materials and Methods:
A total of 120 American Society of Anesthesiologists physical status 1 and 2 patients scheduled to undergo breast surgery were randomly allocated to receive IPB (Group IPB, n = 60) or paravertebral block (PVB) (Group PVB, n = 60) with 20 ml of 0.5% bupivacaine pre-operatively. A standard protocol was used to provide general anesthesia. Lung function tests, visual analog scale (VAS) for pain at rest and movement, analgesic consumption were recorded everyday post-operatively until discharge.
Results:
Lung functions decreased on 1st post-operative day and returned to baseline value by 4th post-operative day in both groups. VAS was similar in both groups. There was no significant difference in the consumption of opioids and diclofenac in both groups. Complete block was achieved in 48 patients (80%) in paravertebral group and 42 patients (70%) in inter pleural group.
Conclusion:
To conclude, lung functions are well-preserved in patients undergoing modified radical mastectomy under general anesthesia supplemented with paravertebral or IPB. IPB is as effective as PVB for post-operative pain relief. PVB has the added advantage of achieving a more complete block.
Keywords: Inter pleural block, lung functions, mastectomy, paravertebral block
Introduction
Breast cancer surgeries are commonly performed under general anesthesia which is the standard technique, but is associated with acute post-operative pain further aggravated by the arm and shoulder movements.[1,2] Concomitant use of regional blocks can not only help to minimize pain, but also improves the pulmonary function and reduce narcotic requirement during the perioperative period.[3,4] Use of these techniques as part of a balanced anesthesia can help in preventing central sensitization and also decrease pulmonary complications.[5] Among the regional techniques such as intercostal nerve block, thoracic epidural, thoracic paravertebral block (PVB), and inter pleural block (IPB), the last two are commonly being used to provide intra and post-operative analgesia in patient undergoing modified radical mastectomy.[6,7]
Thoracic PVB results in somatic and sympathetic block of multiple contiguous thoracic dermatomes above and below the injection site. Pneumothorax, local anesthetic (LA) toxicity, spread of injection to the epidural space causing hypotension and bilateral block are some of the complications associated with it.[8] IPB produces ipsilateral somatic block of multiple thoracic dermatomes. Complications related to needle malposition like pneumothorax, intravascular and intra-bronchial infection can occur with IPB.[9,10]
This study was designed to evaluate the effect of thoracic PVB and IPB on post-operative lung functions, post-operative pain relief and analgesic requirements in patient undergoing modified radical mastectomy.
Materials and Methods
After obtaining institutional research and ethics committee approval, this randomized, double-blinded study was conducted between July 2009 and July 2011. A continuous sample of 124 American Society of Anesthesiologists physical status 1 and 2 patients of adult age group undergoing elective modified radical mastectomy under general anesthesia were recruited in the study after obtaining the informed consent. Patients with pre-existing respiratory diseases (tuberculosis, obstructive pulmonary disease, asthma, lung, and pleural infections), previous lung surgeries, co-existing cardiovascular diseases and history of allergy to LAs and bleeding diathesis were excluded from the study. All patients included in the study were randomly allocated to two groups, Group paravertebral (Group PVB, n = 60) and Group inter pleural (Group IPB, n = 60) by sealed envelope technique. A computer generated allocation sequence was used by a person other than the anesthesiologist involved in the study. All patients recruited for the study were familiarized with visual analog scale (VAS) score and bedside spirometry (Microloop10122, micro medical limited, Kent, England) and their baseline values were recorded.
All patients were pre-medicated with oral diazepam 10 mg on the night before and 2 h before surgery. In the operating room, baseline electrocardiogram, heart rate (HR), mean arterial pressure (MAP), and oxygen saturation (SpO2) were recorded. After securing an intravenous access, patients belonging to inter-pleural group were placed in lateral position with affected side facing up. IPB was performed after local infiltration of the skin (2 ml of 1% lignocaine) under complete aseptic conditions with an18 gauge Tuohy needle in 7th intercostal space, 10 cm lateral to the posterior midline, at the superior border of the rib. The interpleural space was identified by loss of resistance technique,[11] and 20 ml of 0.5% bupivacaine was injected after performing negative aspiration. Patients were then turned supine and the number of dermatomes blocked was assessed at 5 min interval until 20 min and then every min until 30 min by an independent observer.
In paravertebral group, PVB was performed opposite the third thoracic spine under aseptic precautions using the technique described by Eason and Wyatt in the sitting position.[12] Skin infiltration was performed with 2 ml of 1%lignocaine. Tuohy needle (18 gauge) used to identify the paravertebral space was introduced 2.5 cm lateral to the most cephalad aspect of the spinous process and advanced perpendicular to the skin in all planes until the transverse process of the vertebra below was located. Then, the needle was walked above the transverse process and advanced gently until there was a loss of resistance to the injection of air indicating that the needle tip has traversed the superior costo-transverse ligament into the paravertebral space. After negative aspiration, 20 ml of 0.5% bupivacaine was slowly injected over 2-3 min. The patient was turned to supine position and level of analgesia was assessed in the same manner as for inter-pleural group by pinprick method.
A sham puncture was produced at IPB or PVB site depending upon the group allocation of the subject and the dermatome level of sensory block was assessed on the side of surgery to blind the observer recording the parameters.
Anesthesia was induced with 2.5% thiopentone in a dose sufficient to abolish eyelash reflex. Tracheal intubation was facilitated with vecuronium bromide 0.1mg/kg. Anesthesia was maintained using 1 minimum alveolar concentration MAC of isoflurane and 66% of nitrous oxide in oxygen. Controlled ventilation of lungs was performed using a circle system with an Ohmeda 7,000 ventilator. Analgesia was supplemented with intravenous fentanyl (1g/kg) if there was any hemodynamic response (more than 20% increases in pulserate and blood pressure (BP) from the baseline) to surgical incision. At the end of the surgery, residual neuromuscular blockade was antagonized with a mixture of neostigmine (2.5 mg) and atropine (1.2 mg). The patient was transferred to post-operative recovery room after recording BP, HR, and SpO2.
VAS score was recorded at 0.5, 2, 4, 8, 12, and 24 h post-operatively and then every day until patient discharge. During the first 4 h after surgery, whenever the VAS was more than 4 or the patient complained of pain, rescue analgesia was provided with intravenous morphine (1.5 mg every 5 min till VAS was less than 3). After 4 h post-operatively, rescue analgesia was provided with injection. Diclofenac 50 mg for the next 2 days and tablet diclofenac 50 mg for next 5 days. Fentanyl, morphine, and diclofenac requirement was recorded daily for a period of1 week. The quality of the block was assessed by opioid and diclofenac requirement. Patients who required fentanyl intra-operatively, morphine during first 4 h post-operatively and diclofenac (before the scheduled dose at 6 PM) were considered to have a failed block. Those who required either fentanyl or morphine were considered to have a partial block and those who required neither fentanyl nor morphine were considered to have complete block. Lung functions were assessed daily at night 8 pm for 1 week by using hand held bedside pulmonary function test apparatus.
Sample size was calculated based on the Pilot study performed on 20 patients (10 in each group), which indicated that 8 patients in PVB group and 6 in IPB group had complete block. Therefore to demonstrate a 20% difference in the quality of block we needed to study 59 patients in either group to be able to reject the null hypothesis that the quality of the block is similar in both groups with probability (power) 0.8. The Type I error probability associated with this test of this null hypothesis was 0.05. We used continuity-corrected Chi-squared statistics to evaluate this null hypothesis.
The data collected were analyzed using the Statistical Package for the Social Sciences, version 16. Parametric and non-parametric data of the two groups were compared and analyzed using the unpaired student's t?test and Mann Whitney U?test respectively. Inter group differences between the variables recorded during the study period were analyzed by a two?way repeated measure analysis of variance using group as the independent samples factor and time as the repeated measurement factor. A?significant group?by?time interaction was followed by tests of significance using Tukey?s method to compare the two groups at various points in time. The Chi?square test was used for analysis of nominal data.-test and Mann Whitney U-test respectively. Inter group differences between the variables recorded during the study period were analyzed by a two-way repeated measure analysis of variance using group as the independent samples factor and time as the repeated measurement factor. A significant group-by-time interaction was followed by tests of significance using Tukey's method to compare the two groups at various points in time. The Chi-square test was used for analysis of nominal data. P > 0.05 was considered significant.
Results
A total of 124 patients, American society of Anaesthesiologists ASA physical status1and 2, scheduled for elective modified radical mastectomy between July 2009 and July 2011 were included in the study after obtaining approval from the Institutional Ethics Committee. One patient was not cooperative for intervention after being included in the inter-pleural group. Totally 123 patients underwent intervention according to their respective allocation. Among these two patients (1 in each group) in whom duration of surgery was longer than 4 h and one patient (1 in paravertebral group) who did not perform pulmonary function test PFT satisfactorily were excluded from subsequent analysis [Figure 1].
Figure 1.
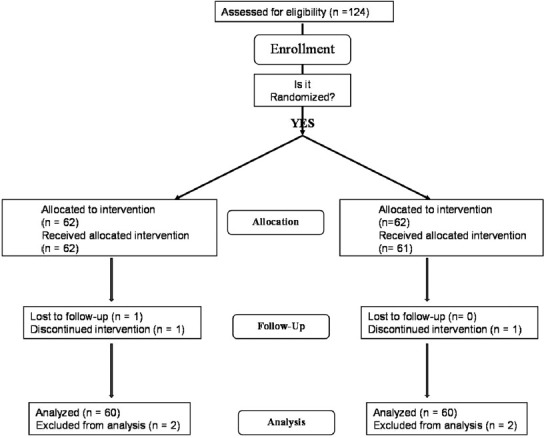
Consort flow chart
The physical characteristics, duration of surgery and baseline parameters were comparable in both the groups [Table 1]. There was no significant difference observed in block characteristics between the groups. Sensory block extended from T3 to T8 in both groups. First attempt success rate in paravertebral group (81%) was higher than in inter-pleural group (75%), but no significant difference was observed in first attempt success rate and number of attempts in both groups [Table 2]. Complete block was achieved in 48 patients (80%) in paravertebral group and 42 patients (70%) in inter-pleural group.
Table 1.
Physical characteristics, duration of surgery and baseline parameters of patients receiving paravertebral block and interpleural block for breast surgeries
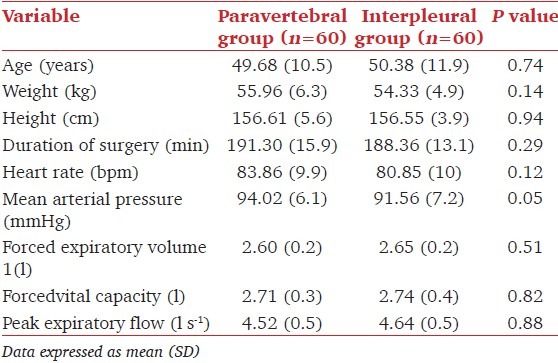
Table 2.
Characteristics of block in patients receiving paravertebral and interpleural block for breast surgeries
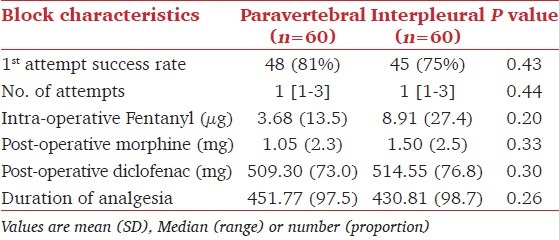
There was no significant difference in forced vital capacity FVC, forced expiratory volume FEV1, and peak expiratopry flow rate PEFR between the two groups. However, there was a slight decrease noticed in FEV1and FVC values from the baseline on the post-operative day1 in both groups. FEV1 and FVC returned to baseline values by post-operative day 5 and day 3 respectively in both groups. PEFR following a slight decrease on the post-operative day1 returned back to normal by post-operative day 4 [Figure 2].
Figure 2.
Change in forced expiratory volume1 FEV1, forced vital capacity FVC, and peak expiratory flow rate PEFR in patients receiving paravertebral(--•--) and interpleural(-▪-) block
VAS score at rest and with movement was similar in both groups throughout the study period [Figure 3]. Duration of post-operative pain relief was similar (paravertebral group 451.7 ± 97.5 min and inter-pleural group 430.81 ± 98.7 min) in both groups. Consequently, there was no significant difference in the consumption of intraoperative fentanyl and post-operative morphine in both groups. Nearly, 80%of patients in PVB group (48 out of 60) and 70% of patients in IPB group (42 out of 60) had a complete block. Both groups had an equal percentage (8%) of patients having failed block (5 out of 60) [Figure 4]. There was no significant difference between mean HR and MAP between both groups throughout the study [Figure 5].
Figure 3.
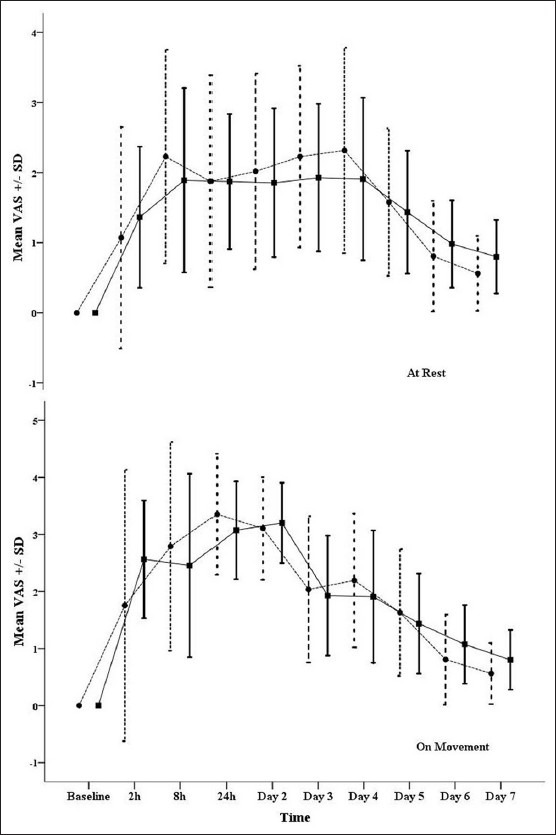
Mean visual analogue scale score at rest and on movement in patients receiving paravertebral (--•--) and inter pleural (-▪-) block
Figure 4.
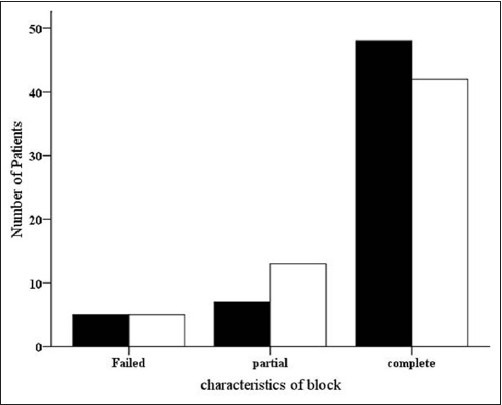
Characteristics of block in patients receiving paravertebral (▪) and inter pleural (▫) block
Figure 5.
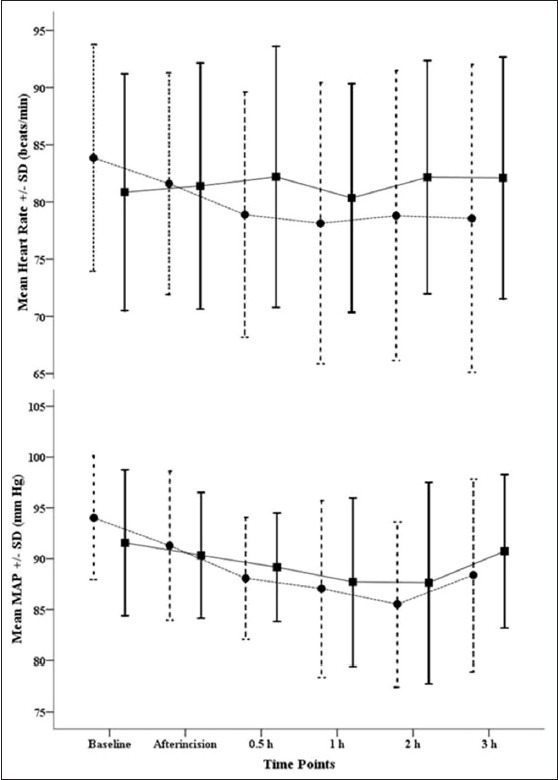
Change in mean heart rate and blood pressure in patients receiving paravertebral (--•--) and inter pleural (-▪-) block
Discussion
We have demonstrated that paravertebral and IPB provide satisfactory pain relief in patients undergoing breast cancer surgery. Decrease in intensity of post-operative pain and subsequent reduction in analgesic requirement during the 1st week after surgery may not only help in prevention of chronic post-mastectomy pain,[13] but may also decrease the pulmonary morbidity post-operatively.
In the present study, patients in PVB group had more complete block when compared to IPB group, but the total dose of opioids consumed were not significantly different. The small difference in fentanyl consumption may have been due to incomplete analgesia with IPB for axillary dissection, but this did not translate into acute post-operative pain as evidenced by similar morphine requirements in both groups. The ability to perform pulmonary function tests in the presence of a large chest wound is an objective measure of pain control.[14,15] Lung functions returned to near normal values by day2in both groups. The decrease in lung functions on day1 could be because of the higher concentration of LA used for the blocks. Clinical research has shown better lung functions with PVB when compared to IPB in thoracotomy patients because of higher loss of the drug through chest drain, presence of blood in the pleural cavity, increased absorption of drug by the inflamed pleura and dependent pooling of the drug affecting the function of the diaphragm with IPB,[15] However, in the absence of these factors as in our study PEFR took 4 days in both paravertebral (4.56 ± 0.45) and inter-pleural group (4.58 ± 0.53) to return back to baseline value (4.57 ± 0.45 in paravertebral and 4.59 ± 0.53 in inter-pleural).
Acute post-operative pain relief with PVB results from direct penetration of LA in to the neurological structures present within the paravertebral space because the spinal nerve lacks both epineurium and part of the perineurium and has a thin membranous root sheath which can be easily penetrated by LA.[5] Furthermore, relative avascularity of the paravertebral space limits anesthetic diffusion and allows prolonged sensory block and provides effective post-operative pain control.[16]
In IPB, LA deposited between the parietal and visceral pleura diffuses from the pleural cavity across the endothoracic and subserous fascia, and innermost inter-costals muscles to provide multiple unilateral intercostal blockade.[9,17] Analgesia with IPB occurs by reverse diffusion of LA to the subpleural space and this diffusion of LA from the pleural space to the intercostal nerves is limited by uptake of drug by the visceral pleura. The rapidity and extent of this uptake is highly unpredictable.[10,18,19] Furthermore, LA diffuses out through both layers of the pleura and gets deposited on the surfaces of lung, diaphragm, and pericardium thereby reducing the amount of LA acting on the intercostal nerves to produce pain relief for modified radical mastectomy.[20,21] This explains why the patient population in the PVB group had more complete block when compared to IPB.
PVB resulted in a complete block in 81% patients when compared to71% with IPB and it enabled effective anesthesia for axillary dissection. There is sufficient spread of LA towards lower cervical and upper thoracic paravertebral spaces with PVB,[22] but with IPB most of the injected LA collects at the lowest point of the pleural cavity in a gravity-dependent manner, and hence spread is highly dependent on body position and it does not always reach the T2 level to provide analgesia for axillary dissection.[9,23]
Effective block of the nociceptive afferent input with PVB removes the stimulus for the generation of central sensitization and along with the afferent blockade of the sympathetic chain results in a “total afferent block.” This characteristic total afferent block because of PVB is the most important factor that prevents the development of chronic pain.[24] None of patients from the current study were referred to the pain clinic with complaints of post-mastectomy pain until 3 months after the study. However, it is not possible to comment on the likely percentage of patients who would actually benefit from these blocks and be free of chronic post-mastectomy pain. Further studies having follow-up for at least a year are needed to establish the percentage relationship between adequacy of immediate post-operative pain relief with these blocks and chronic post-mastectomy pain.
To conclude Lung functions are well-preserved in patients undergoing modified radical mastectomy under general anesthesia supplemented with Paravertebral or IPB. IPB is as effective as PVB for post-operative pain relief. PVB has the added advantage of achieving a more complete block.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Klein SM, Bergh A, Steele SM, Georgiade GS, Greengrass RA. Thoracic paravertebral block for breast surgery. Anesth Analg. 2000;90:1402–5. doi: 10.1097/00000539-200006000-00026. [DOI] [PubMed] [Google Scholar]
- 2.Coveney E, Weltz CR, Greengrass R, Iglehart JD, Leight GS, Steele SM, et al. Use of paravertebral block anesthesia in the surgical management of breast cancer: Experience in 156 cases. Ann Surg. 1998;227:496–501. doi: 10.1097/00000658-199804000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boughey JC, Goravanchi F, Parris RN, Kee SS, Kowalski AM, Frenzel JC, et al. Prospective randomized trial of paravertebral block for patients undergoing breast cancer surgery. Am J Surg. 2009;198:720–5. doi: 10.1016/j.amjsurg.2008.11.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schnabel A, Reichl SU, Kranke P, Pogatzki-Zahn EM, Zahn PK. Efficacy and safety of paravertebral blocks in breast surgery: A meta-analysis of randomized controlled trials. Br J Anaesth. 2010;105:842–52. doi: 10.1093/bja/aeq265. [DOI] [PubMed] [Google Scholar]
- 5.Richardson J, Lönnqvist PA, Naja Z. Bilateral thoracic paravertebral block: Potential and practice. Br J Anaesth. 2011;106:164–71. doi: 10.1093/bja/aeq378. [DOI] [PubMed] [Google Scholar]
- 6.Richardson J, Sabanathan S, Mearns AJ, Shah RD, Goulden C. A prospective, randomized comparison of interpleural and paravertebral analgesia in thoracic surgery. Br J Anaesth. 1995;75:405–8. doi: 10.1093/bja/75.4.405. [DOI] [PubMed] [Google Scholar]
- 7.Richardson J, Lönnqvist PA. Thoracic paravertebral block. Br J Anaesth. 1998;81:230–8. doi: 10.1093/bja/81.2.230. [DOI] [PubMed] [Google Scholar]
- 8.Karmakar MK. Thoracic paravertebral block. Anesthesiology. 2001;95:771–80. doi: 10.1097/00000542-200109000-00033. [DOI] [PubMed] [Google Scholar]
- 9.Dravid RM, Paul RE. Interpleural block-part 1. Anaesthesia. 2007;62:1039–49. doi: 10.1111/j.1365-2044.2007.05183.x. [DOI] [PubMed] [Google Scholar]
- 10.Dravid RM, Paul RE. Interpleural block-part 2. Anaesthesia. 2007;62:1143–53. doi: 10.1111/j.1365-2044.2007.05181.x. [DOI] [PubMed] [Google Scholar]
- 11.Covino BG. Interpleural regional analgesia. Anesth Analg. 1988;67:427–9. [PubMed] [Google Scholar]
- 12.Eason MJ, Wyatt R. Paravertebral thoracic block-a reappraisal. Anaesthesia. 1979;34:638–42. doi: 10.1111/j.1365-2044.1979.tb06363.x. [DOI] [PubMed] [Google Scholar]
- 13.Kairaluoma PM, Bachmann MS, Rosenberg PH, Pere PJ. Preincisional paravertebral block reduces the prevalence of chronic pain after breast surgery. Anesth Analg. 2006;103:703–8. doi: 10.1213/01.ane.0000230603.92574.4e. [DOI] [PubMed] [Google Scholar]
- 14.Mann LJ, Young GR, Williams JK, Dent OF, McCaughan BC. Intrapleural bupivacaine in the control of postthoracotomy pain. Ann Thorac Surg. 1992;53:449–53. doi: 10.1016/0003-4975(92)90267-8. [DOI] [PubMed] [Google Scholar]
- 15.Kambam JR, Hammon J, Parris WC, Lupinetti FM. Intrapleural analgesia for post-thoracotomy pain and blood levels of bupivacaine following intrapleural injection. Can J Anaesth. 1989;36:106–9. doi: 10.1007/BF03011428. [DOI] [PubMed] [Google Scholar]
- 16.Weltz CR, Greengrass RA, Lyerly HK. Ambulatory surgical management of breast carcinoma using paravertebral block. Ann Surg. 1995;222:19–26. doi: 10.1097/00000658-199507000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brismar B, Pettersson N, Tokics L, Strandberg A, Hedenstierna G. Postoperative analgesia with intrapleural administration of bupivacaine-adrenaline. Acta Anaesthesiol Scand. 1987;31:515–20. doi: 10.1111/j.1399-6576.1987.tb02613.x. [DOI] [PubMed] [Google Scholar]
- 18.Reiestad F, Strømskag KE. Interpleural catheter in the management of postoperative pain: A preliminary report. Reg Anesth. 1986;11:89–91. [Google Scholar]
- 19.Murphy DF. Interpleural analgesia. Br J Anaesth. 1993;71:426–34. doi: 10.1093/bja/71.3.426. [DOI] [PubMed] [Google Scholar]
- 20.Higgins PC, Ravalia A. Interpleural anaesthesia for mastectomy. Anaesthesia. 2005;60:1150–1. doi: 10.1111/j.1365-2044.2005.04412.x. [DOI] [PubMed] [Google Scholar]
- 21.Frenette L, Boudreault D, Guay J. Interpleural analgesia improves pulmonary function after cholecystectomy. Can J Anaesth. 1991;38:71–4. doi: 10.1007/BF03009167. [DOI] [PubMed] [Google Scholar]
- 22.Karmakar MK, Kwok WH, Kew J. Thoracic paravertebral block: Radiological evidence of contralateral spread anterior to the vertebral bodies. Br J Anaesth. 2000;84:263–5. doi: 10.1093/oxfordjournals.bja.a013417. [DOI] [PubMed] [Google Scholar]
- 23.McKenzie AG, Mathe S. Interpleural local anaesthesia: Anatomical basis for mechanism of action. Br J Anaesth. 1996;76:297–9. doi: 10.1093/bja/76.2.297. [DOI] [PubMed] [Google Scholar]
- 24.Richardson J, Jones J, Atkinson R. The effect of thoracic paravertebral blockade on intercostal somatosensory evoked potentials. Anesth Analg. 1998;87:373–6. doi: 10.1097/00000539-199808000-00025. [DOI] [PubMed] [Google Scholar]


