Abstract
Background:
The role of clonidine as an adjuvant to local anesthetic agents in brachial plexus block (BPB) has been extensively studied. However, till date there has been no consensus about the ideal dose of clonidine for this purpose. This study was carried out to evaluate two doses of clonidine-1 and 2 g/kg, added to 0.5% bupivacaine, with regard to onset and duration of sensorimotor blockade, hemodynamic effects, postoperative analgesia, and adverse effects.
Materials and Methods:
Sixty adult patients undergoing upper limb surgeries were randomly allocated into two groups. Thirty patients received 1 g/kg clonidine (group I) and the rest received 2 g/kg clonidine (group II) added to 30 mL of 0.5% bupivacaine through nerve stimulator-guided supraclavicular BPB. The onset and duration of sensorimotor blockade, hemodynamic variables, duration of analgesia, level of sedation, and adverse effects was assessed.
Results:
The onset of sensorimotor block was earlier in group II (9.9 ± 4.1 min for sensory block and 13.2 ± 6.7 min for motor block) than in group I (15.9 ± 6.8 min for sensory block and 18.5 ± 7.8 min for motor block). The duration of analgesia was also prolonged in patients receiving the higher dose (21.0 ± 2.96 h vs. 14.9 ± 3.0 h). Although hemodynamics remained comparable in both the groups, incidence of hypotension and bradycardia was higher in group II as compared to group I. The sedation was clinically and statistically more in group II patients (43% vs. 17%).
Conclusion:
Higher dose of clonidine in BPB hastens the onset, prolongs the duration of sensorimotor blockade and postoperative analgesia without significant hemodynamic alterations. It also causes more sedation, which although ensures patient comfort in most cases, but might be undesirable in certain situations.
Keywords: Adjuvant, brachial plexus block, bupivacaine, clonidine, postoperative analgesia
Introduction
Peripheral nerve blocks have assumed a prominent role in modern anesthesia practice as they provide ideal operative conditions without any sedation or systemic hemodynamic effects.[1] Brachial plexus block (BPB) is a commonly used regional anesthetic technique for surgeries involving upper limb, especially orthopedic procedures. With advances in the field of surgery, surgical procedures have become more complex and the operating time has increased manifold with a consequent need to increase the duration of the BPB. To achieve this, many drugs have been used as adjuncts to the local anesthetics (LA). Clonidine is one of them, which is an2-adrenoceptor agonist with hypotensive, sedative, and analgesic properties.[2] It is, however, not free of adverse effects, the most commonly observed being dry mouth, sedation, hypotension, and bradycardia.[3,4]
However, till date, there has been no consensus about the ideal dose of clonidine as an adjunct to LA in the BPB. The present study was planned to evaluate two different doses of clonidine added to 0.5% bupivacaine−1 and 2 g/kg, with regards to onset and duration of sensorimotor blockade, hemodynamic variables, postoperative analgesia, and adverse effects.
Materials and Methods
The hospital ethical committee approved the prospective, double-blinded randomized study and a written informed consent from all the patients was obtained. Sixty adult patients (18-65 years) of either sex, weight range (40-90 kg), American Society of Anesthesiologists (ASA) grade I, II, scheduled for upper limb surgeries were randomly allocated by a computer generated randomization list into two groups. Patients were given supraclavicular BPB with 30 mL of 0.5% bupivacaine with clonidine as adjuvant in the dose of either 1 g/kg (Group I; n = 30) or 2 g/kg (Group II; n = 30) using a peripheral nerve stimulator. Patients having peripheral neuropathy or motor weakness, uncontrolled systemic illness, infection at the site of the block, history of coagulopathy or anticoagulant medication intake, hypersensitivity to any of the study drug and those with inadequate block were excluded from the study.
All patients were premedicated with oral diazepam 0.2 mg/kg on the night before surgery. In the operation theatre parameters recorded included heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), and oxygen saturation (SpO2) at baseline and every 15 min thereafter. BPB was performed by supraclavicular approach using peripheral nerve stimulator (Stimuplex DIG RC, B Braun Medical Inc., Malaysia) in all the patients by the same anesthesiologist who was blinded to the composition of the LA mixture.
The onset of sensory block was evaluated by the loss of temperature sense (by the cold test tube method)[5] in the forearm. Assessment of motor blockade was done using 3-point modified Bromage score[6]0 − normal motor function with full extension and flexion of elbow, wrist, and fingers, 1 − decreased motor strength, with ability to move only fingers, 2 − complete motor block with inability to move elbow, wrist, and fingers. Both intraoperative and postoperative sedation was rated by using the 4-point sedation score:[7]0 − awake, 1 − drowsy, 2 − sleeping but arousable on verbal command, 3 − sleeping and arousable only on tactile stimulation.
Duration of sensory and motor blockade was assessed every hour till the recovery of sensations by an anesthesiologist who was blinded to the study groups. Postoperative pain was assessed using the visual analog scale (VAS) (0 − no pain to 10 − worst pain)[8] every hour till the block lasted. The end-point of the study was time from performance of the block to the onset of pain as determined by VAS score of 4 or more. Rescue analgesia was provided with tramadol 2 mg/kg intravenous (IV). Postoperative vitals (HR, SBP, DBP, MAP, SpO2) were recorded every 2 h for the first 6 h and thereafter every 4 h till the need for rescue analgesia (tramadol 2 mg/kg IV). The incidence of side effects (bradycardia, hypotension, and sedation) was also recorded. Bradycardia was defined as a decrease in HR by 20% from the baseline value or an absolute HR > 50 beats per min; which was managed by 0.6 mg IV bolus of atropine. Hypotension was defined as fall in blood pressure by 20% from the baseline or an absolute MAP > 60 mm Hg; which was managed by a bolus of IV crystalloids or increments of mephentermine 3 mg IV.
Statistical analysis
Sample size was based on a pilot study of 10 patients and was selected to detect a projected difference of 20% in duration of postoperative analgesia between the groups, with a type I error of 0.05 and a power of 0.8. Statistical analysis was performed using SPSS (version 12.0; SPSS, Inc., Chicago, IL, USA) software and graphs were produced using Microsoft Excel for MAC 2011 (version 14.1.2). Parametric data were recorded as arithmetic mean ± standard deviation. Chi-square analysis was used to compare the qualitative variables. For the analysis of quantitative variables, student's paired t-test was used. A “P” > 0.05 was accepted as statistically significant.
Results
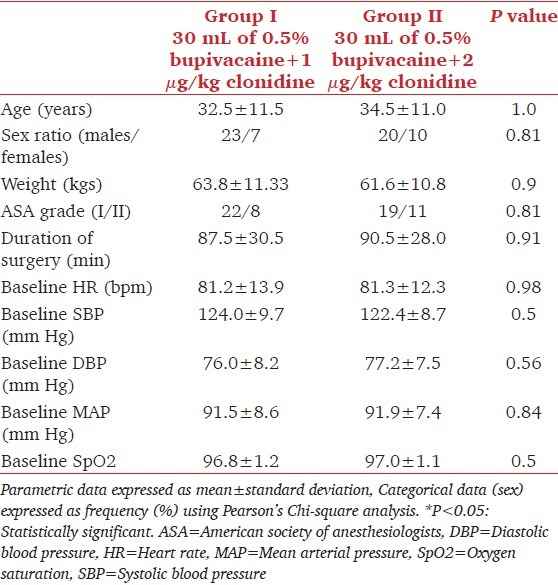
BPB was performed in 68 patients, out of which eight (five in group I and three in group II) were excluded due to incomplete block effect. A total of 60 patients (30 in each group) were included in the study. There was no statistically significant difference between the demographics (age, sex, weight, ASA grade, duration of surgery) and baseline vital signs (HR, SBP, DBP, MAP, and SpO2) of the two groups [Table 1].
Table 1.
Distribution of subjects according to demographic profile and vital signs
The onset of sensorimotor block was earlier in group II patients (9.9 ± 4.1 min for sensory block and 13.2 ± 6.7 min for motor block) than those in group I (15.9 ± 6.8 min for sensory block and 18.5 ± 7.8 min for motor block), which was statistically significant (P > 0.05) [Table 2]. No difference was noted in the hemodynamic parameters (mean HR, MAP, SpO2) before giving the block, throughout the surgery and postoperatively [Figures 1 and 2]. Sedation score of patients in group II were higher than those in group I intraoperatively and postoperatively and this was statistically significant (P > 0.05). Twenty-five (8.33%) patients in group I remained awake throughout the procedure. Out of the five patients who were sedated, four became awake within 2 h and one after 4 h. However, among group II patients, only 17 (56.67%) remained awake, whereas 13 patients showed evidence of sedation (sedation score 1 and above). This lasted for up to 4 h in all except one patient who became awake after 6 h [Figure 3].
Table 2.
Characteristics of sensory and motor block in group I and group II
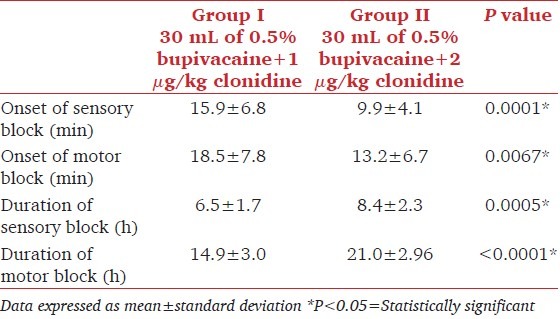
Figure 1.
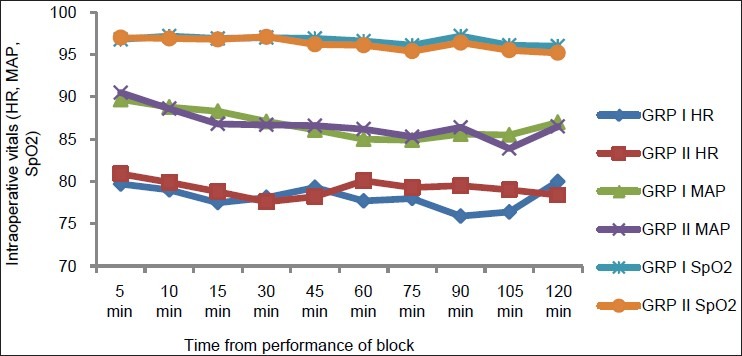
Comparison of intraoperative vitals (heart rate, mean arterial pressure, and oxygen saturation) in between group I and group II
Figure 2.
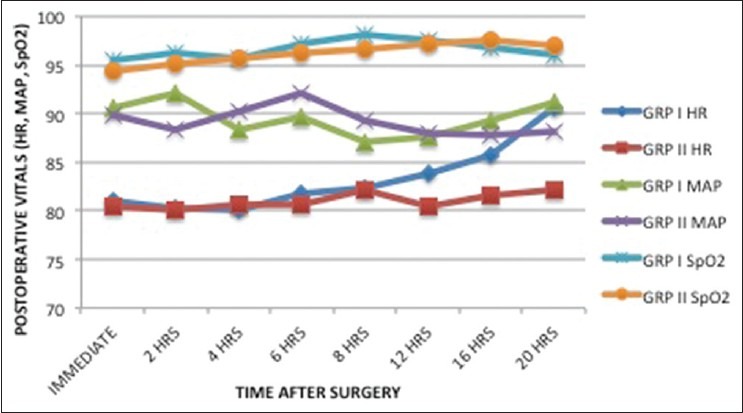
Comparison of postoperative vitals (heart rate, mean arterial pressure, and oxygen saturation) in between group I and group II
Figure 3.
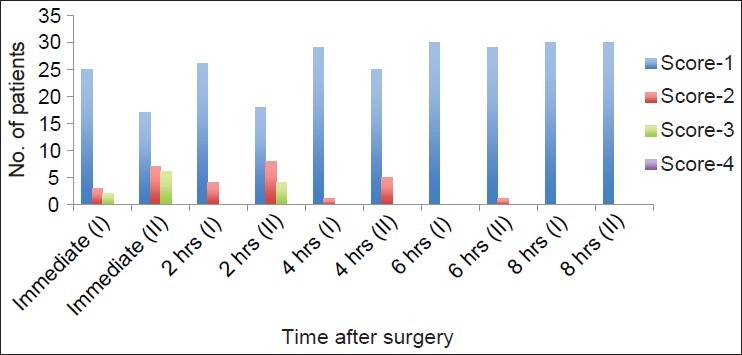
Distribution of patients according to sedation score
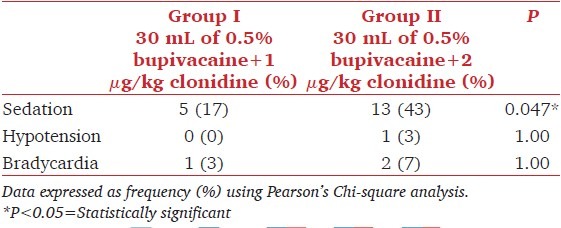
Motor blockade was complete after the block in both the groups. Twenty-nine (96.67%) patients in group I had recovered totally from the motor block by 8 h, whereas the corresponding Figure for group II was 22 (7.33%) [Figure 4]. The mean duration of motor blockade was longer in group II (8.4 ± 2.3 h) than in group I (6.5 ± 1.7 h), which was statistically significant (P > 0.05). Postoperative analgesia lasted for 21.0 ± 2.96 h in group II and 14.9 ± 3.0 h in group I, which was also statistically significant (P > 0.05) [Table 2]. Postoperative distribution of patients according to VAS ≥ 4 [Figure 5] shows that all patients in group I required rescue analgesia by 20 h, whereas in group II, the same was true only after 24 h. The incidence of adverse effects, namely sedation, bradycardia, and hypotension, was statistically higher in group II compared to group I (P > 0.05). The most advertent effect was noted on incidence of sedation which was 43% in group II compared to 16.7% in group I [Table 3].
Figure 4.
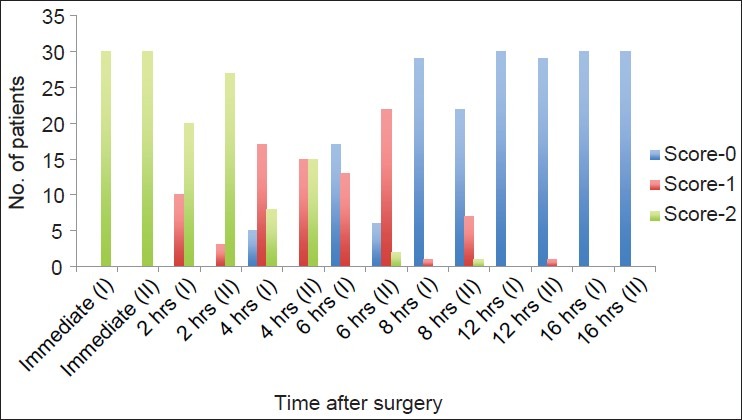
Distribution of patients according to modified Bromage score
Figure 5.
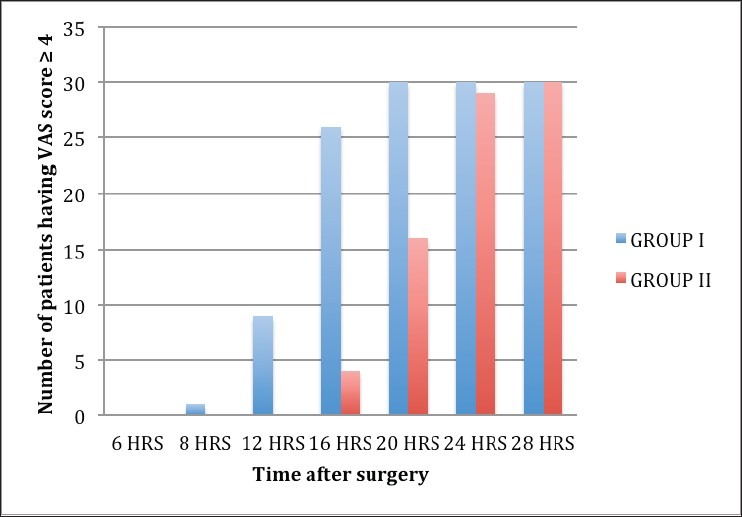
Postoperative distribution of patients according to visual analog scale (VAS) ≥4
Table 3.
Incidence of adverse effects in group I compared to group II
Discussion
Results of this prospective, randomized, double-blinded study demonstrate that adding 2 g/kg clonidine to 0.5% bupivacaine hastens the onset of sensorimotor block and prolongs the duration of postoperative analgesia more than 1 g/kg clonidine in BPB. Hemodynamics remained stable throughout the study period with both the doses. The higher dose causes more sedation, which although ensures patient comfort in most cases, but might be harmful in certain patients.
The role of clonidine as an adjuvant to LA in upper limb peripheral nerve blocks has been extensively studied.[6,9,10] Dose range of 30-300 g has been used in various studies[5,9,10,11,12,13] with up to 150 g doses being associated with minimal side effects.[9] But some authors have shown that clonidine even at such doses can cause significant hemodynamics compromise which challenges its use in peripheral nerve blocks in outpatients.[14] Besides, there is no study suggestive of any appropriate dose of clonidine according to weight/kg. Hence, the present study was undertaken to find the appropriate dose of clonidine used as an adjuvant to peripheral nerve blockade without significant adverse outcomes. We chose bupivacaine because controversy still exists about using clonidine as an adjuvant to long-acting LA such as ropivacaine and bupivacaine where in some studies support its addition to peripheral nerve block,[9,11,12] while others contradict it.[4,13,15,16]
In our study, the onset of sensory and motor block was earlier with the higher dose of clonidine (2 g/kg). Both Bernard and Macaire[5] and Iohom et al.,[17] have reported a faster onset of sensorimotor block with the use of clonidine as an adjuvant to LA than plain LA. However, Eledjam et al.,[9] Gaumann et al.,[6] Singelyn et al.,[8] El Saied et al.,[11] Murphy et al.,[10] Erlacher et al.,[18] and Hutschala et al.,[12] have reported that clonidine did not hasten the onset of block irrespective of the dosage used.
There was a dose-dependent prolongation of analgesia after neural blockade in our patients. This can be explained by the fact that clonidine increases potassium conductance and blocks the conduction of C and A fibers. Besides, clonidine also enhances lidocaine-induced inhibition of C-fiber compound action potential. Lipophilic nature of clonidine allows rapid absorption into cerebrospinal fluid and binding to 2-adrenoceptor of spinal cord causing blockade at primary afferent terminals (both spinal as well as peripheral nerve endings).[19] Similar to our study, both Hutschala et al.,[12] and El Saied et al.,[11] observed longer duration of analgesia and motor block with the use of clonidine as an adjuvant as compared to placebo. An increase in the duration of postoperative analgesia was also observed by Eledjam et al.[9] Bernard and Macaire et al.,[5] Iohom et al.,[17] and Iskandar et al.,[20] Singelyn et al.,[8] observed a linear increase in the duration of analgesia from 0.1 /kg to 0.5 /kg clonidine but not with 1 and 1.5 /kg, indicating no further increase in analgesia with increasing dose. Results contrary to our study were also reported by Sia and Lepri,[7] Gaumann et al.,[6] and Duma et al.[13] Prolonged motor blockade with higher clonidine dose is beneficial in long duration surgeries. However, it can be detrimental in ambulatory settings, wherein early mobilization causes early rehabilitation.
Sedative properties of clonidine are attributable to its lipophilic nature resulting in systemic absorption when administered perineurally,[3] Gaumann et al.,[6] and Bernard et al.,[5] reported significant sedation with the use of clonidine than with plain LA corroborating the results of our study. The same was, however, not observed by Eledjam et al.[9]
Hemodynamic parameters (HR, MAP, SpO2) remained stable at all times in most of the patients both intraoperatively and postoperatively in our study (one episode of bradycardia, no hypotension with 1 g/kg and two bradycardia, one hypotension with 2 g/kg). Stable hemodynamics was also reported by Singelyn et al.,[8] Bernard et al.,[5] El Saied et al.,[11] Murphy et al.,[10] Erlacher et al.,[18] Duma et al.,[13] and Iohom et al.,[17] while using clonidine in BPB. However, contrasting results were obtained in the study by Bernard et al.,[5] wherein a 30% fall in SBP was seen with 300 g, 20% fall with 90 g and 15% fall with 30 g clonidine. In the same study, 4 out of 14 patients had episodes of hypoxemia (SpO2> 90% lasting 20 s or more) with the highest dose of clonidine (300 g). Few transient episodes of bradycardia and hypotension were also observed by Sia and Lepri[7] and Iskandar et al.[20]
One of the limitations of our study was small sample size, but it had significantly important results, and we suggest future studies to be undertaken with a larger population size. Another limitation of our study was that we could have used per kg body weight dose of 0.5% bupivacaine as well. A total of 30 mL of 0.5% bupivacaine appears to be higher than safe dose limit in 40 kg patients. However, this is not true as the amount of systemic absorption of LA through BPB is very poor.[21] Another issue of concern is that prolongation of motor blockade by higher dose of clonidine though is useful for long duration surgeries, but it is detrimental in outpatient settings where early mobilization is desirable.
Conclusion
Higher dose of clonidine in BPB hastens the onset, prolongs the duration of sensorimotor blockade, and provides a longer pain-free period without significant hemodynamic alterations. However, it has more sedative potential that can be harnessed to allay patient anxiety and provide optimal intraoperative and postoperative patient comfort. But it might be undesirable in certain set of patients (geriatric, obese patients, and those with cardiorespiratory compromise).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Khanduri KC. Regional anaesthetic techniques for orthopaedic surgeries. Med J Armed Forces India. 2008;64:109. doi: 10.1016/S0377-1237(08)80048-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johr M. Clonidine in paediatric anaesthesia. Eur J Anaesthesiol. 2011;28:325–6. doi: 10.1097/EJA.0b013e3283453e90. [DOI] [PubMed] [Google Scholar]
- 3.McCartney CJ, Duggan E, Apatu E. Should we add clonidine to local anesthetic for peripheral nerve blockade. A qualitative systematic review of the literature? Reg Anesth Pain Med. 2007;32:330–8. doi: 10.1016/j.rapm.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 4.Culebras X, Van Gessel E, Hoffmeyer P, Gamulin Z. Clonidine combined with a long acting local anesthetic does not prolong postoperative analgesia after brachial plexus block but does induce hemodynamic changes. Anesth Analg. 2001;92:199–204. doi: 10.1097/00000539-200101000-00038. [DOI] [PubMed] [Google Scholar]
- 5.Bernard JM, Macaire P. Dose-range effects of clonidine added to lidocaine for brachial plexus block. Anesthesiology. 1997;87:277–84. doi: 10.1097/00000542-199708000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Gaumann D, Forster A, Griessen M, Habre W, Poinsot O, Della Santa D. Comparison between clonidine and epinephrine admixture to lidocaine in brachial plexus block. Anesth Analg. 1992;75:69–74. doi: 10.1213/00000539-199207000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Sia S, Lepri A. Clonidine administered, as an axillary block does not affect postoperative pain when given as the sole analgesic. Anesth Analg. 1999;88:1109–12. doi: 10.1097/00000539-199905000-00027. [DOI] [PubMed] [Google Scholar]
- 8.Singelyn FJ, Gouverneur JM, Robert A. A minimum dose of clonidine added to mepivacaine prolongs the duration of anesthesia and analgesia after axillary brachial plexus block. Anesth Analg. 1996;83:1046–50. doi: 10.1097/00000539-199611000-00025. [DOI] [PubMed] [Google Scholar]
- 9.Eledjam JJ, Deschodt J, Viel EJ, Lubrano JF, Charavel P, d’Athis F, et al. Brachial plexus block with bupivacaine: Effects of added alpha-adrenergic agonists: Comparison between clonidine and epinephrine. Can J Anaesth. 1991;38:870–5. doi: 10.1007/BF03036962. [DOI] [PubMed] [Google Scholar]
- 10.Murphy DB, McCartney CJ, Chan VW. Novel analgesic adjuncts for brachial plexus block: A systematic review. Anesth Analg. 2000;90:1122–8. doi: 10.1097/00000539-200005000-00023. [DOI] [PubMed] [Google Scholar]
- 11.El Saied AH, Steyn MP, Ansermino JM. Clonidine prolongs the effect of ropivacaine for axillary brachial plexus blockade. Can J Anaesth. 2000;47:962–7. doi: 10.1007/BF03024866. [DOI] [PubMed] [Google Scholar]
- 12.Hutschala D, Mascher H, Schmetterer L, Klimscha W, Fleck T, Eicgler HG, et al. Clonidine added to bupivacaine enhances and prolongs analgesia after brachial plexus block via a local mechanism in healthy volunteers. Eur J Anaesthesiol. 2004;21:198–204. doi: 10.1017/s0265021504003060. [DOI] [PubMed] [Google Scholar]
- 13.Duma A, Urbanek B, Sitzwohl C, Kreiger A, Zimpfer M, Kapral S. Clonidine as an adjuvant to local anaesthetic axillary brachial plexus block: A randomized, controlled study. Br J Anaesth. 2005;94:112–6. doi: 10.1093/bja/aei009. [DOI] [PubMed] [Google Scholar]
- 14.Buttner J, Ott B, Klose R. The effect of adding clonidine to mepivacaine. Axillary brachial plexus blockade. Anaesthetist. 1992;41:548–54. [PubMed] [Google Scholar]
- 15.Trifa M, Ben Khalifa S, Jendoubi A, Zribi N, Regaya T, Engelhardt T. Clonidine does not improve quality of ropivacaine axillary brachial plexus block in children. Paediatr Anaesth. 2012;22:425–9. doi: 10.1111/j.1460-9592.2012.03809.x. [DOI] [PubMed] [Google Scholar]
- 16.Dagher C, Yazigi A, Rkaibe N. Clonidine as adjuvant for bupivacaine in ilioinguinal block does not prolong postoperative analgesia in pediatric and also in adult patients. Paediatr Anesth. 2006;16:224–5. doi: 10.1111/j.1460-9592.2005.01809.x. [DOI] [PubMed] [Google Scholar]
- 17.Iohom G, Machmachi A, Diarra DP, Khatouf M, Boileau S, Dap F, et al. The effects of clonidine added to mepivacaine for paronychia surgery under axillary brachial plexus block. Anesth Analg. 2005;100:1179–83. doi: 10.1213/01.ANE.0000145239.17477.FC. [DOI] [PubMed] [Google Scholar]
- 18.Erlacher W, Schusching C, Koinig H, Marhofer P, Meliscek M, Mayer N, et al. Clonidine as adjuvant for mepivacaine, ropivacaine and bupivacaine in axillary, perivascular brachial plexus block. Can J Anaesth. 2001;48:522–5. doi: 10.1007/BF03016825. [DOI] [PubMed] [Google Scholar]
- 19.Madan R, Bharti N, Shende D, Khokhar SK, Kaul HL. A dose response study of clonidine with local anesthetic mixture for peribulbar block: A comparison of three doses. Anesth Analg. 2001;93:1593–7. doi: 10.1097/00000539-200112000-00056. [DOI] [PubMed] [Google Scholar]
- 20.Iskandar H, Benard A, Ruel-Raymond J, Cochard G, Manaud B. The analgesic effect of interscalene block using clonidine as an analgesic for shoulder arthroscopy. Anesth Analg. 2003;96:260–2. doi: 10.1097/00000539-200301000-00052. [DOI] [PubMed] [Google Scholar]
- 21.Stoelting RK. Pharmacology and physiology in anesthetic practice. 3rd ed. Philadelphia (PA): Lippincott-Raven; 1999. Local anesthetics; pp. 155–81. [Google Scholar]


