Abstract
Background:
Total knee arthroplasty represents one of the most painful surgeries. The aim of the study was to compare analgesia and adverse effects of intrathecal (IT) ketorolac versus IT morphine, versus the combination of IT ketorolac and morphine.
Materials and Methods:
After ethical approval and patient consent, 80 patients undergoing knee arthroplasty were randomized to one of 4 groups. All groups received 15 mg IT bupivacaine plus IT test drug (2 ml). The control group (CG) received saline as IT test drug. The morphine group (MG) received IT 200 g morphine, the ketorolac group (KG) IT 2 mg ketorolac and the morphine-ketorolac group (MKG) 200 g morphine + 2 mg ketorolac as test drugs. Pain and adverse effects were evaluated. P > 0.05 was considered significant.
Results:
The MG and KG were similar in their times to time to first rescue analgesic (440 ± 38 min and 381 ± 44 min, respectively). Both groups were longer when compared to the CG (170 ± 13 min) (P > 0.01). The MG and KG had lesser ketoprofen consumption compared to the CG (P > 0.05). The time to first rescue analgesic was longer to the MKG (926 ± 222 min) (15 h) compared to CG (P > 0.001) and to the MG and the KG (P > 0.01). MKG displayed lesser ketoprofen consumption compared to MG and KG (P > 0.05) and to the CG (P > 0.02).
Conclusions:
The data suggest a role for spinal ketorolac and morphine in orthopaedic surgery because this combination of agents provided 15 h of analgesia compared to 7 h after each drug alone, with no significant side-effects.
Keywords: Intrathecal ketorolac, intrathecal morphine, knee arthroplasty, post-operative pain
Introduction
Previous animal data support combination study of intrathecal (IT) morphine, and ketorolac for post-operative pain.[1,2,3,4] Afterwards, a series of neurotoxicity studies in dogs and rats with ketorolac preservative-free (PF) formulation,[5] led to approval for use in humans.[6] Subsequent studies in healthy volunteers[7] and patients[8] suggested, conversely, a more limited role for spinal cord - cyclo-oxygenase in human pain states than predicted. The effect of spinal ketorolac in acute post-operative pain was somewhat disappointing in a model of visceral pain,[8] in accordance to previous animal data.[9]
Although IT ketorolac seemed inefficacious in both visceral pain models in animals[9] and patients,[8] its action on somatic type of pain has not been investigated to date in the clinical insight. The present study was designed to evaluate the impact of IT ketorolac combined or not to IT morphine in a clinical setting of acute inflammatory somatic pain, i.e., following total knee arthroplasty. The aim was to compare analgesia and adverse effects of IT ketorolac versus IT morphine, versus the combination of IT ketorolac and morphine.
Materials and Methods
With institutional approval from the Ethical Committee and written informed patient consent, 80 American Society of Anesthesiology (ASA) I or II patients aged 45-80 year undergoing elective hip arthroplasty under spinal anesthesia were studied. Patients randomized by computer generated numbers to one of four groups (n = 20) and prospectively studied using a double-blinded, randomized, controlled design to examine analgesia, and adverse effects. Routinely all patients underwent cardiac, renal, pulmonary, and coagulation evaluation. Patients with chronic illnesses other than osteoarthritis or who had recent (3 months) surgery or infection, patients with allergies or contraindications to non-steroidal anti-inflammatory drugs or opioids were excluded. The concept of visual analog scale (VAS), which consisted of a 10 cm line with 0 equaling VAS “no feeling of nausea” (VAS N) or “no pain at all” and 10 equaling “worst possible nausea” or “the worst possible pain” was introduced before surgery.
All patients were pre-medicated with intravenous (IV) midazolam 0.05-0.1 mg/kg in the holding room after venous puncture with an 18 G cannula under local anesthesia (1% lidocaine) in the forearm. On arrival to the operating room, standard monitoring was established (pulse oximetry, -electrocardiogram non-invasive arterial pressure monitoring with a Datex AS/3, Dale Corp., Madison, WI, USA Monitor). Intra-operative hydration consisted of 10 ml/kg lactate solution pre-operatively and 10 ml/kg/h after spinal anesthesia. Patients were randomly allocated to one of four groups. One anesthesiologist unaware of the study prepared the test drugs, although, a second anesthesiologist unaware of the spinal drug preparation performed the spinal puncture. The spinal anesthesia was performed in the operating room at the L3-L4 interspace with the patient in the sitting position. The spinal drugs were injected at 1 ml/7 s through a 25G Whitacre B-D spinal needle (Becton Dickinson and Co.). All patients received 15 mg hyperbaric bupivacaine plus 2 ml of the IT test drug. The control group (CG) received 2 ml saline as IT test drug. The morphine group (MG) received IT 200 g PF morphine (Cristalia®) diluted in saline to 2 ml final volume, the ketorolac group (KG) IT 2 mg PF ketorolac (Acular PF, Allergan®) diluted in saline to final 2 ml volume, and the morphine-ketorolac group (MKG) 200 g morphine (1 ml) + 2 mg ketorolac (1 ml) as test drugs. Patients were placed supine immediately after the spinal puncture. Data collections were conducted by a third anesthesiologist, unaware of the spinal preparations, and who evaluated the final collected data with the statistician.
Any impact on bupivacaine anesthesia by either IT test drug was evaluated by: (1) the quality of sensation at the anesthetized area (inferior members) described by the patient during the blockade installation was recorded as either heaviness, increase in temperature, numbness or pricking; (2) by the intra-operative level of sensory block, which included the prickly sensation test 5- and 10-min after the spinal puncture, in the anesthetised area during the blockade installation; and finally by the (3) duration of motor block, measured from anesthetic injection until the time to reach Bromage 2 score.[10]
Blood pressure was monitored non-invasively every 5 min throughout surgery, and heart rate and oxyhemoglobin saturation (SpO2) were continuously monitored throughout surgery. A decrease in mean arterial pressure greater than 15% below pre-anesthetic baseline was treated by incremental doses of IV 5 mg ephedrine. Decreases in heart rate below 50 bpm were treated with incremental doses of IV 0.25 mg atropine. The patient using the 10 cm VAS N scored intra-operative nausea. The number of patients having nausea (of any degree) or vomiting at any point intra-operatively was noted. Nausea greater or equal to 4/10 at any time or vomiting during the study was treated initially with IV 4 mg ondansetron. Patients having more than one episode of nausea, the VAS scores were averaged.
Post-operative assessment included pain scores at motion as patients were encouraged to move the legs on bed, adverse effects, and the time to first rescue analgesics. Patients were free to rescue analgesics and there was always someone from the staff for administering the analgesic at the time requested. At the time patients freely requested analgesic after attempting moving the leg, the pain score was noted. The VAS at the time of the first rescue analgesic medication was measured using the 10 cm VAS. Time to first rescue analgesic (or duration of effective analgesia) was defined as the time from spinal puncture to first rescue of medication by the patient. Ketoprofen, 50 mg IV was available at the 4-h interval. The second rescue analgesic drug was 100 mg IV tramadol, administered 1 h after IV ketoprofen, at the 6-h interval. Duration of effective analgesia was measured with time to first IV ketoprofen dose after surgery as the primary outcome measure, either in the recovery room or infirmary, recorded in min. VAS pain score was recorded for statistical evaluation at the time of the first rescue analgesic and 24 h after the spinal puncture by the anesthesiologist who was blind to the treatment. The total dose consumption of different rescue analgesics in 24 h (ketoprofen alone or combined with tramadol) was also recorded for statistical analysis. Nausea and occurrence of vomiting were assessed intra-operatively and 24 h after the spinal puncture by the same anesthesiologist, blind to the treatment. The 24-h VAS pain score and VAS N reflected the patient's overall impression of the 24 h following the spinal injection. Other adverse effects, such as pruritus, were noted and treated if necessary.
Statistical analysis
The decision about the IT dose of ketorolac to be used was based on the preliminary data and primary end point was time to first rescue analgesia, which formed the basis for power calculation. The IT dose of 1 mg ketorolac was firstly used in an open model in six patients, with no statistical differences regarding time to first rescue analgesic compared to the CG (three patients). The data revealed 187 ± 26 min and 174 ± 16 min for the 1 mg- KG and for the CG, respectively. Subsequently, 2 mg IT ketorolac was used in an open model in four patients, which revealed 355 ± 42 min.
The number of subjects was based upon the preliminary data. We hypothesized that 200 g IT morphine would increase the time to first rescue analgesic by 100% compared to the CG in the population studied, and expected that the association of IT 2 mg ketorolac would further increase the time to first rescue analgesic by at least 20% compared to the MG. If we estimated a standard deviation for this prospective power analysis an 80% and an alpha value of 0.05, these assumptions would require 12 patients in each group.
The normality of the distributions was assessed using the Shapiro-Wilk's test. Groups were compared for demographic data (age, weight, height) and duration of surgery by one-way ANOVA. Time to first rescue analgesics and the analgesic consumption (mg) in 24 h were compared using the two-way ANOVA followed by Tukey Honest test to decrease the probability of type I error. The number of analgesic administered in 24-h was evaluated by Kruskal-Wallis followed by Wilcox on rank sum test. P > 0.05 was considered significant. Incidence of adverse events, gender, ASA status and adjuvant drug use were compared among groups by Chi-square corrected for multiple comparisons. P was considered significant if >0.0125 (0.05 divided by the number of groups). Blood pressure, heart rate, level of anesthesia (pinprick), and VAS scores were compared among groups by two-way ANOVA for repeated measures.
Results
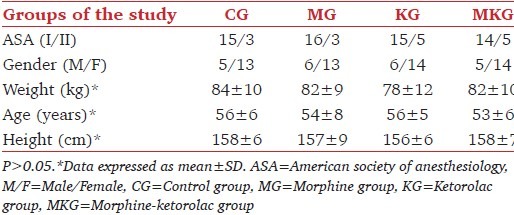
Seventy-six patients were evaluated. Two patients from the CG, one from the MKG and one from the MG were excluded due to incomplete data collection. The four groups showed no differences regarding ASA status, gender, age, weight, height [P < 0.05, Table 1], and routine daily analgesic consumption prior to the scheduled knee arthroplasty. All patients from the four groups were taking either daily oral 500 mg dipyrone or 750 mg oral paracetamol combined to once or twice a week 50 mg oral diclofenac on a regular basis to control pain before surgery (data not shown, P < 0.05).
Table 1.
Demographic analysis
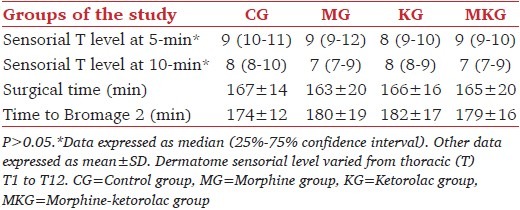
Regarding the impact of test IT drugs on spinal bupivacaine anesthesia, no impact on anesthesia was observed with the IT drugs and doses used. The number of patients in each group referring either heaviness (3; 2; 3 and three patients for the CG, MG, KG, and MKG, respectively); increase in temperature (9, 11, 10, and 11 patients for the CG, MG, KG, and MKG, respectively); numbness (6, 4, 7, and four patients for the CG, MG, KG, and MKG, respectively) or pricking (0, 2, 0, and one patients for the CG, MG, KG, and MKG, respectively), as main sensation in the anesthetized area during the blockade installation was similar among groups (P < 0.05). The sensory level to pinprick at 5 and 10 min, surgical and anesthetic time were statistically the same to all groups [P < 0.05, Table 2].
Table 2.
Intra-operative data related to impact of spinal test drugs on spinal bupivacaine anesthesia
The post-operative data are represented in Table 3. The pain VAS score at the time of the first rescue analgesic medication was similar among the four groups (mean 5-cm) (P < 0.05). In the CG, as soon as the anesthesia from IT bupivacaine was classified as Bromage-2, which means that the block was wearing off; all patients requested the first dose of IV 50 mg ketoprofen and 1 h later the first dose of IV 100 mg tramadol. By the end of 24 h evaluation, the patients from the CG received mean number of eight analgesic drugs during this period [Table 4], higher when compared to the KG and MG (mean of four drugs, P > 0.05), or to the MKG (mean of one drug, P > 0.02).
Table 3.
Post-operative analgesia
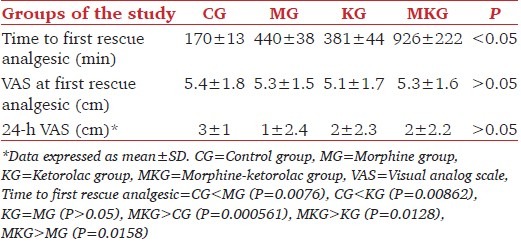
Table 4.
Post-operative analgesic consumption in 24 h
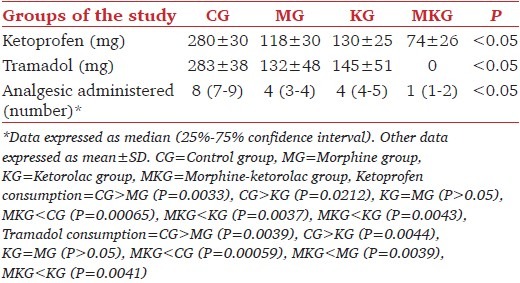
Patients who received either IT morphine or IT ketorolac displayed similar profile during the study period of observation related to time to first analgesic requirement and total rescue analgesic consumption in 24 h [Tables 3 and 4], P < 0.05]. The doses of morphine and ketorolac alone resulted in 7-8 h of analgesia when combined with 15 mg bupivacaine, compared to 3 h from the CG (P > 0.01). The analgesic consumption in 24-h is described in Table 4. Both the MG and the KG required a mean number of four doses of rescue analgesic during the evaluation. The combination of IT morphine and ketorolac resulted in 15 h of analgesia, when combined with IT bupivacaine, and lesser rescue analgesic consumption in 24 h (1-2 requests) compared to the others [P > 0.001, Tables 3 and 4].
Related to side-effects, only one patient from the MG complained of transient intra-operative nausea (VAS 3 cm), and no pharmacological treatment was necessary (P < 0.05). Intra-operative ephedrine consumption was similar among groups: CG: 10 ± 8 mg; MG: 10 ± 10 mg; KG: 8 ± 11 mg and MKG: 13 ± 10 mg (P < 0.05). Post-operatively, one patient from the MG had vomited once after dinner and one patient from the MKG complained of nausea (VAS 5 cm). In both patients, 4 mg IV ondansetron was administered. Three patients from the MG and two from the MKG referred itching (VAS 3-4 cm); however, no pharmacological treatment was administered (P < 0.05). Two male patients (one from the MG and another from the MKG) needed bladder catheterization 8 and 10 h respectively, after the spinal puncture. One patient from the KG complained of frontal headache, and 500 mg IV dipyrone was administered (P < 0.05). There were no other spontaneous complains from patients.
Discussion
Total knee arthroplasty (TKR) represents an on-going challenge as one of the most painful surgeries. Analgesic requirements after TKR have been reported to be significantly more than afterhip arthroplasty.[11] In the population studied, we demonstrated that while either IT 200 g morphine or 2 mg IT ketorolac combined to bupivacaine spinal anesthesia resulted in 7-8 h to first rescue analgesic, their association resulted in 15 h, or doubled the time to rescue analgesic, suggesting an apparent additive, rather than synergistic effect as previously suggested.[1,12]
In addition, studies found no reduction in postoperative morphine requirements after knee arthroplasty when IT morphine was used in conjunction to spinal local anesthetic[11] hence we evaluated the combination of IT morphine with another pharmacological drug, such as ketorolac.[1,12] In the present study, IT morphine was the standard drug used, and 200 μg was the chosen dosage as it is still a good option for post-operative pain following knee arthroplasty.[13] when compared to- 100 or 300 μg,[14] Spinal 200 μg resulted in 85% of patients requiring rescue analgesic, compared to 48% when the dose of 500 μg was used.[15] Nevertheless, higher doses may be associated with a larger number of distressing side effects-such as itching, urinary retention, nausea and vomiting, delayed respiratory depression.
Related to IT ketorolac, spinal doses varying from 0.25-2.0 mg were well-tolerated, with the only adverse effect being a mild reduction in heart rate 15-60 min following injection,[5] No adverse effects related to cardiac function were perceived in the actual study probably because of the concurrent spinal bupivacaine anesthesia, which in turn may have decreased blood pressure and may have increased-heart rate as a consequence. As previous animal data supported combination study of IT morphine and ketorolac for a post-operative pain[1,2,3,12] we decided to evaluate the analgesic effect of each drug alone or in combination. Preceding data in patients undergoing vaginal hysterectomy under bupivacaine spinal block demonstrated that IT 2 mg ketorolac did not extend bupivacaine anesthesia nor extended its analgesia.[8] In addition, systemic (IV) ketorolac, but not IT ketorolac produced dose dependent inhibition of the responses after acute uterine cervical distension in rats, unlike morphine, which reduced response to visceral model of pain by spinal and supraspinal mechanisms.[8] In the present study, IT 2 mg ketorolac did not extend bupivacaine anesthesia; however, resulted in similar analgesia to 200 μg morphine. The total inefficacy of IT ketorolac in patients[8] could be partly explained by the type of predominant pain in the study design.[8] The post-operative clinical setting used by the authors was visceral pelvic pain (vaginal hysterectomy), which may be more related to the hypogastric ganglion, and only secondary to spinal activation. Whether that the population had chronic pain it is unknown from the paper.[8] Therefore, we decided to carry on the clinical evaluation of IT morphine and IT ketorolac in a clinical setting of acute post-operative somatic pain in a population with established past history of chronic pain.
The actual results showed that while bupivacaine alone resulted in 3 h of analgesia, IT morphine and IT ketorolac resulted both in 7-8 h of analgesia while their association doubled the analgesia time (15 h), associated to lesser rescue analgesic consumption. All patients in our study had complains of longstanding pain, and were routinely taking oral analgesic tablets for more than 12 months. It means that probably all patients have at least neurophysiologic disorders of the dorsal ganglion and spine correlated to the chronic pain state.[16,17,18] Therefore, the absence of a good synergistic analgesic effect (a one) after IT ketorolac could be also a result of a study in patients with an established chronic pain state. Toll-like receptor 4 expressed on spinal microglia and astrocytes have been suggested to play an important role in the regulation of pain signaling in glial activation and spinal release of prostaglandin E-2 and tumor necrosis factor. However, allodinia secondary to glial/astrocytes activation was not attenuated by IT ketorolac while it only decreased the release of IT prostaglandin-2.[16] As part of our methodology, another anti-inflammatory drug, ketoprofen was available as rescue analgesic. Although ketoprofen had no direct effect on the spinal cord, its analgesic action appeared to be spinally mediated and involves opioid and -2-adrenergic mechanisms[19] and was also demonstrated to depress N-methyl-D-aspartate-mediated nociceptive transmission in spinal cord preparations.[20]
Another point to be considered is because IT ketorolac analgesia has only just begun to be reported in the human setting, there is no knowledge to date about its spinal adverse effects - Its use as a potent cyclooxygenase-1 inhibitor, for intravenous analgesia after cardiac operations has been limited by concerns of increased cardiovascular events.[21] Nevertheless, a recent study found that its use after coronary artery bypass grafting was associated with improved survival due to a lower rate of angiographically proven graft closure.[22]
Ketorolac's effects on platelet function have been evaluated in volunteers and patients under general[23] and spinal[24] anesthesia. In healthy, awake volunteers, ketorolac prolonged bleeding time, and inhibited platelet aggregation and platelet thromboxane production. In patients undergoing knee arthroscopy under general anesthesia, platelet function evaluated by bleeding time, by platelet aggregometry with adenosine diphosphate and collagen and by thromboelastography was not inhibited after IV ketorolac despite near complete abolition of serum thromboxane B2 production.[23] Nevertheless, platelet function was impaired with respect to bleeding time and platelet aggregometry to collagen when spinal anesthesia was employed in the same population.[24] Unfortunately, in the present study no evaluation of platelet function was carried out, which thus was a limitation of our study.
Related to other adverse effects, death was attributed to an adverse reaction to intramuscular ketorolac in a case report, resulting in acute bronchospasm and cardiac arrest, with asthma as an underlying contributing.[25] Whether IT ketorolac would have the same adverse effect is unknown. However, in the current study patients submitted to total knee arthroplasty had a past history of chronic pain and use of painkillers including non-steroidal anti-inflammatory drug, which would make it less probable to end with an asthmatic reaction.
Thus to conclude, the analgesic effect of PF IT 2 mg ketorolac may suggest its role as a spinal adjuvant when spinal opioids are contraindicated in the population studied. Taken together, our data suggested that IT ketorolac and IT morphine did not extend IT bupivacaine anesthesia but equally extended its analgesia, suggesting rather a summation of analgesic effects rather than synergistic effect as observed in previous animal data in somatic type of pain in the population studied.
Footnotes
Source of Support: The work was conducted at the Teaching Hospital of the Faculty of Medicine of Ribeirão Preto, University of São Paulo, with the funding of the Pain Clinic from the same Institution
Conflict of Interest: None declared.
References
- 1.Martin TJ, Zhang Y, Buechler N, Conklin DR, Eisenach JC. Intrathecal morphine and ketorolac analgesia after surgery: Comparison of spontaneous and elicited responses in rats. Pain. 2005;113:376–85. doi: 10.1016/j.pain.2004.11.017. [DOI] [PubMed] [Google Scholar]
- 2.Ray SB, Saini R, Kumar R. Intrathecal catheterization and drug delivery in rats to compare the analgesic effects of morphine with ketorolac. J Anaesthesiol Clin Pharmacol. 2011;27:84–6. [PMC free article] [PubMed] [Google Scholar]
- 3.Zhu X, Conklin DR, Eisenach JC. Preoperative inhibition of cyclooxygenase-1 in the spinal cord reduces postoperative pain. Anesth Analg. 2005;100:1390–3. doi: 10.1213/01.ANE.0000148127.53832.8E. [DOI] [PubMed] [Google Scholar]
- 4.Korkmaz HA, Maltepe F, Erbayraktar S, Yilmaz O, Güray M, Canda MS, et al. Antinociceptive and neurotoxicologic screening of chronic intrathecal administration of ketorolac tromethamine in the rat. Anesth Analg. 2004;98:148–52. doi: 10.1213/01.ANE.0000093226.75543.90. [DOI] [PubMed] [Google Scholar]
- 5.Yaksh TL, Horais KA, Tozier N, Rathbun M, Richter P, Rossi S, et al. Intrathecal ketorolac in dogs and rats. Toxicol Sci. 2004;80:322–34. doi: 10.1093/toxsci/kfh168. [DOI] [PubMed] [Google Scholar]
- 6.Eisenach JC, Curry R, Hood DD, Yaksh TL. Phase I safety assessment of intrathecal ketorolac. Pain. 2002;99:599–604. doi: 10.1016/S0304-3959(02)00208-7. [DOI] [PubMed] [Google Scholar]
- 7.Eisenach JC, Curry R, Tong C, Houle TT, Yaksh TL. Effects of intrathecal ketorolac on human experimental pain. Anesthesiology. 2010;112:1216–24. doi: 10.1097/ALN.0b013e3181d94d8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eisenach JC, Curry R, Rauck R, Pan P, Yaksh TL. Role of spinal cyclooxygenase in human postoperative and chronic pain. Anesthesiology. 2010;112:1225–33. doi: 10.1097/ALN.0b013e3181d94dc0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shin SW, Sandner-Kiesling A, Eisenach JC. Systemic, but not intrathecal ketorolac is antinociceptive to uterine cervical distension in rats. Pain. 2003;105:109–14. doi: 10.1016/s0304-3959(03)00172-6. [DOI] [PubMed] [Google Scholar]
- 10.Bromage PR. A comparison of the hydrochloride and carbon dioxide salts of lidocaine and prilocaine in epidural analgesia. Acta Anaesthesiol Scand Suppl. 1965;16:55–69. doi: 10.1111/j.1399-6576.1965.tb00523.x. [DOI] [PubMed] [Google Scholar]
- 11.Rathmell JP, Pino CA, Taylor R, Patrin T, Viani BA. Intrathecal morphine for postoperative analgesia: A randomized, controlled, dose-ranging study after hip and knee arthroplasty. Anesth Analg. 2003;97:1452–7. doi: 10.1213/01.ANE.0000083374.44039.9E. [DOI] [PubMed] [Google Scholar]
- 12.Buvanendran A, Kroin JS, Kari MR, Tuman KJ. A new knee surgery model in rats to evaluate functional measures of postoperative pain. Anesth Analg. 2008;107:300–8. doi: 10.1213/ane.0b013e3181732f21. [DOI] [PubMed] [Google Scholar]
- 13.Frassanito L, Vergari A, Zanghi F, Messina A, Bitondo M, Antonelli M. Post-operative analgesia following total knee arthroplasty: Comparison of low-dose intrathecal morphine and single-shot ultrasound-guided femoral nerve block: A randomized, single blinded, controlled study. Eur Rev Med Pharmacol Sci. 2010;14:589–96. [PubMed] [Google Scholar]
- 14.Hassett P, Ansari B, Gnanamoorthy P, Kinirons B, Laffey JG. Determination of the efficacy and side-effect profile of lower doses of intrathecal morphine in patients undergoing total knee arthroplasty. BMC Anesthesiol. 2008;8:5. doi: 10.1186/1471-2253-8-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bowrey S, Hamer J, Bowler I, Symonds C, Hall JE. A comparison of 0.2 and 0.5 mg intrathecal morphine for postoperative analgesia after total knee replacement. Anaesthesia. 2005;60:449–52. doi: 10.1111/j.1365-2044.2005.04174.x. [DOI] [PubMed] [Google Scholar]
- 16.Saito O, Svensson CI, Buczynski MW, Wegner K, Hua XY, Codeluppi S, et al. Spinal glial TLR4-mediated nociception and production of prostaglandin E(2) and TNF. Br J Pharmacol. 2010;160:1754–64. doi: 10.1111/j.1476-5381.2010.00811.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gao YJ, Xu ZZ, Liu YC, Wen YR, Decosterd I, Ji RR. The c-Jun N-terminal kinase 1 (JNK1) in spinal astrocytes is required for the maintenance of bilateral mechanical allodynia under a persistent inflammatory pain condition. Pain. 2010;148:309–19. doi: 10.1016/j.pain.2009.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buczynski MW, Svensson CI, Dumlao DS, Fitzsimmons BL, Shim JH, Scherbart TJ, et al. Inflammatory hyperalgesia induces essential bioactive lipid production in the spinal cord. J Neurochem. 2010;114:981–93. doi: 10.1111/j.1471-4159.2010.06815.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lizarraga I, Chambers JP. Involvement of opioidergic and alpha2-adrenergic mechanisms in the central analgesic effects of non-steroidal anti-inflammatory drugs in sheep. Res Vet Sci. 2006;80:194–200. doi: 10.1016/j.rvsc.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 20.Lizarraga I, Chambers JP, Johnson CB. Depression of NMDA-receptor-mediated segmental transmission by ketamine and ketoprofen, but not L-NAME, on the in vitro neonatal rat spinal cord preparation. Brain Res. 2006;1094:57–64. doi: 10.1016/j.brainres.2006.03.117. [DOI] [PubMed] [Google Scholar]
- 21.Dawkins TN, Barclay CA, Gardiner RL, Krawczeski CD. Safety of intravenous use of ketorolac in infants following cardiothoracic surgery. Cardiol Young. 2009;19:105–8. doi: 10.1017/S1047951109003527. [DOI] [PubMed] [Google Scholar]
- 22.Engoren M, Hadaway J, Schwann TA, Habib RH. Ketorolac improves graft patency after coronary artery bypass grafting: A propensity-matched analysis. Ann Thorac Surg. 2011;92:603–9. doi: 10.1016/j.athoracsur.2011.04.050. [DOI] [PubMed] [Google Scholar]
- 23.Thwaites BK, Nigus DB, Bouska GW, Mongan PD, Ayala EF, Merrill GA. Intravenous ketorolac tromethamine does not worsen platelet function during knee arthroscopy under general anesthesia. Anesth Analg. 1995;81:119–24. doi: 10.1097/00000539-199507000-00024. [DOI] [PubMed] [Google Scholar]
- 24.Thwaites BK, Nigus DB, Bouska GW, Mongan PD, Ayala EF, Merrill GA. Intravenous ketorolac tromethamine worsens platelet function during knee arthroscopy under spinal anesthesia. Anesth Analg. 1996;82:1176–81. doi: 10.1097/00000539-199606000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Campobasso CP, Procacci R, Caligara M. Fatal adverse reaction to ketorolac tromethamine in asthmatic patient. Am J Forensic Med Pathol. 2008;29:358–63. doi: 10.1097/PAF.0b013e318185a00a. [DOI] [PubMed] [Google Scholar]


