Abstract
Context:
Opioids are being increasingly used these days as adjuvants to local anesthetics in spinal anesthesia.
Aim:
The aim of this study is to compare the effects of adding sufentanil or fentanyl to low dose bupivacaine in spinal anesthesia for endoscopic urological procedures.
Settings and Design:
Prospective, randomized, double-blind study.
Materials and Methods:
A total of 90 elective endoscopic urological surgery patients, 40-80 years old, received spinal anesthesia with 7.5 mg hyperbaric bupivacaine 0.5% (Group A) or by adding sufentanil 10 g (Group B) or fentanyl 25 g (Group C) to 5 mg hyperbaric bupivacaine 0.5%. These groups were compared in terms of the quality of spinal anesthesia as well as analgesia.
Results:
The onset of sensory and motor blockade was significantly rapid in Group A as compared with Groups B and C. The maximum upper level of sensory block was higher in Group A patients than Groups B and C patients. Quality of analgesia was significantly better and prolonged in sufentanil group as compared with other two groups. Motor block was more intense and prolonged in Group A as compared with Groups B and C patients. Request for post-operative analgesic was significantly delayed in Group B patients.
Conclusions:
Spinal anesthesia for endoscopic urological procedures in elderly patients using low dose bupivacaine (5 mg) combined with 10 μg sufentanil is associated with a lower incidence of hemodynamic instability, better quality and prolonged duration as compared to that by adding 25 μg fentanyl.
Keywords: Adjuvants, bupivacaine, fentanyl, intrathecal, low dose spinal, sufentanil
Introduction
“Cocainization of the spinal cord” was first described by August Bier in 1899.[1] The technique has been refined since that time and has evolved into the modern concept of subarachnoid block (SAB). The safety of well-conducted spinal analgesia was attested by reports of thousands of carefully followed-up cases by the recognized authorities.[2] However, the use of local anesthetics in this technique, too, is not without complications such as hypotension, bradycardia, urinary retention and neurological injuries etc., Most of these complications are found to be dependent on the volume and dose of injected drug and the height of SAB.[3] By adding opioid as adjuvants, the dose of local anesthetics can be reduced to half thereby reducing the side-effects without unduly compromising the quality of analgesia.[4,5,6]
Most of patients presenting for endoscopic urological surgery are elderly, having a coexisting cardiac, pulmonary or some other co-morbid condition. To reduce the adverse hemodynamic effects associated with spinal block in these patients, a suitable adjuvant to low dose local anesthetics can help to provide the satisfactory spinal block without compromising safety.
Sufentanil as an adjuvant has been extensively compared with fentanyl in spinal and epidural labor analgesia with bupivacaine. The studies on these drug combinations, for endoscopic urological procedures are relatively unexplored. Our present study compared the effect of adding sufentanil (10 μg) or fentanyl (25μ g) to 5 mg bupivacaine 0.5% in endo-urological procedures in terms of the quality of spinal anesthesia and analgesia using visual analog scale (VAS).
Materials and Methods
In this randomized double-blind study, 90 patients in the age group of 50-80 years, belonging to American Society of Anesthesiologists (ASA) physical status I and II, scheduled for elective endoscopic urological surgery under spinal anesthesia, were included after approval by the hospital ethics committee. A written informed consent was obtained from each patient. Depending upon the nature of intrathecal drug used, these patients were randomized into three groups of 30 patients each, using computer generated randomization, as:
Group A: SAB with 0.5% hyperbaric bupivacaine 7.5 mg (1.5 ml)
Group B: SAB with 0.5% hyperbaric bupivacaine 5 mg (1 ml) + sufentanil 10 mg (0.2 ml) + isotonic saline 0.3 ml
Group C: SAB with 0.5% hyperbaric bupivacaine 5 mg (1 ml) + fentanyl 25 mg (0.5 ml).
All study drugs were made to a fixed volume of 1.5 ml and marked with a coded label by an anesthesiologist not involved with the conduct of anesthesia.
Patients with spinal deformities, local skin infection, coagulation disorders, impaired renal or liver functions, morbid obesity, neurological or mental disease, history of allergy to drugs to be used and opioid dependence were excluded from the study.
A thorough routine pre-anesthetic check-up comprising of general physical examination, systemic examination and routine investigations of all patients was conducted a day before surgery.
Anesthesia technique
All patients were given tablet diazepam 10 mg and tablet ranitidine 150 mg orally at night before surgery and tablet diazepam 5 mg with tablet ranitidine 150 mg orally in the morning on the day of surgery. Patients were kept nil orally for 6 h prior to surgery. After shifting the patient to the operating table, monitoring of heart rate, non-invasive blood pressure, respiratory rate and electrocardiography and oxygen saturation was started. An intravenous line was secured and patients were preloaded with isotonic saline 5 ml/kg body weight over a period of 15-20 min.
Under strict aseptic conditions, lumbar puncture was performed in a sitting position at the level of L 3-4 or L 4-5 intervertebral space using 26 G spinal needle, after infiltrating the skin with 0.5-1 ml of 2% lidocaine. After obtaining a free flow of cerebrospinal fluid, 1.5 ml study drug was injected intrathecally at approximately 0.25 ml/s and patient was made supine immediately.
Heart rate, non-invasive blood pressure, respiratory rate and oxygen saturation were recorded at 2 min intervals for 1st20 min from the time of injection of spinal solution and then after every 5 min until the completion of surgery. Episodes of perioperative hypotension (systolic blood pressure >90 mm of Hg or fall in systolic blood pressure <20% of baseline value) and bradycardia (heart rate >50 beats/min) were recorded. Hypotension was appropriately treated with incremental boluses of mephentermine (3 mg) intravenously and bradycardia was treated with atropine (0.6 mg) intravenously.
Level of sensory block was determined by pinprick test every 2 min until the maximum level has established after 4 consecutive tests. The maximum upper level of sensory block and the time taken to attain maximum upper level was recorded. Motor block of the lower extremities was assessed according to the modified Bromage scale.[7] The quality of intraoperative analgesia was assessed by a blind observer on 0-10 linear VAS at every 15 min following intrathecal injection of drug up to the end of surgery. Patients with inadequate block requiring supplement general anesthesia were excluded from the statistical analysis.
Post-operative assessment
Duration of sensory blockade was noted by assessing the level of sensory block after every 15 min until the time of regression to T12 level. Motor block was assessed and graded at the end of surgery and then at every 15 min interval, until full return of lower extremity motor function (score = 0). The quality of post-operative analgesia was assessed using a 0-10 linear VAS every 15 min until the first request of supplement analgesia. Regular monitoring of vital signs was performed. Side-effects such as nausea, vomiting, pruritus, sedation, respiratory depression (respiratory rate >10 breaths/min) or oxygen desaturation (SpO2>90%) or any other complication were noted.
Statistical analysis
Data was tabulated and analyzed using the analysis of variance and Chi-square test.
Results
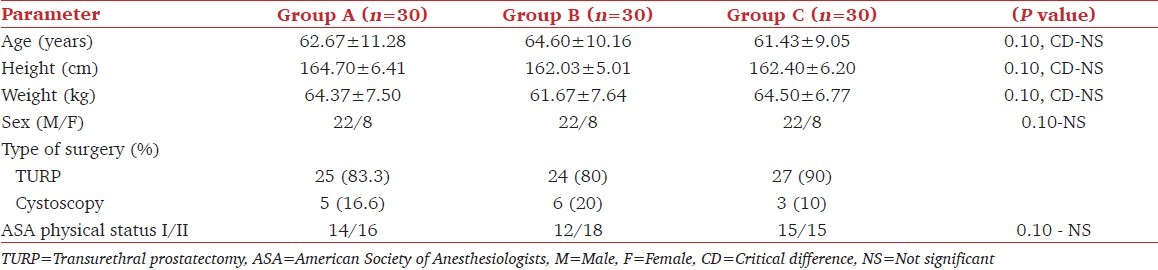
Patients in all three groups were statistically comparable as regards to age, sex, weight, height, type of surgery and ASA physically status [Table 1].
Table 1.
Demographic profile
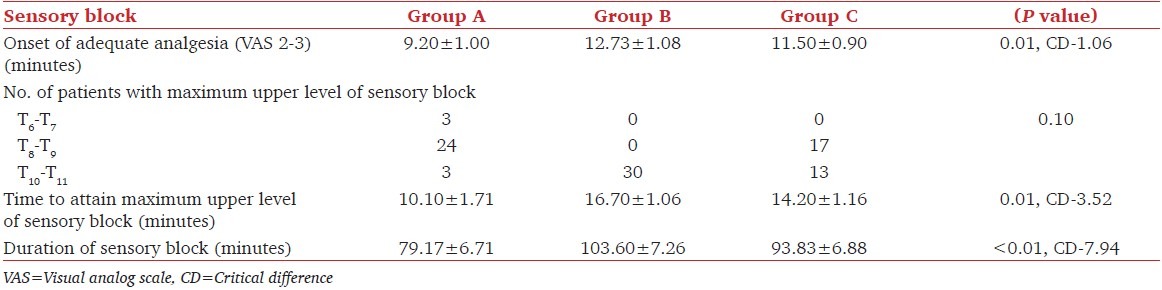
Onset of adequate analgesia as defined by the time between the administration of drug and the achievement of VAS of 2-3 was significantly early in Group A (9.20 ± 1.00 min) followed by Group C (11.50 ± 0.90 min) and then Group B (12.73 ± 1.08 min). Maximum upper level of sensory block in Group A was in the range of T8-T9, in Group B it was in a range of T10-T11 and in Group C was in the range of T8-T11. This difference was statistically significant. The time required to reach maximum height of the block was significantly more in Groups B and C as compared with Group A. However, there was no statistically significant difference between Groups B and C. The duration of sensory block in Groups B and C (103.60 ± 7.26 and 93.83 ± 6.88 min respectively) was significantly prolonged as compared to Group A (79.17 ± 6.71 min) [Table 2].
Table 2.
Sensory block characteristics
Onset of motor block was quicker in Group A as compared to Groups B and C [Figure 1]. In Group A, 43% patients had modified Bromage score of 3 and 57% patients had modified Bromage score of 2. Whereas, none of the patients in Groups B and C achieved grade 3 modified Bromage score and all patients achieved modified Bromage score of grade 2 only [Figure 2]. The duration of motor block was significantly prolonged in Group A as compared to Groups B and C, whereas there was no statistically significant difference between Groups B and C. Motor block completely weaned off at 60 min in Groups B and C and at 75 min in Group A [Table 3, and Figure 3].
Figure 1.
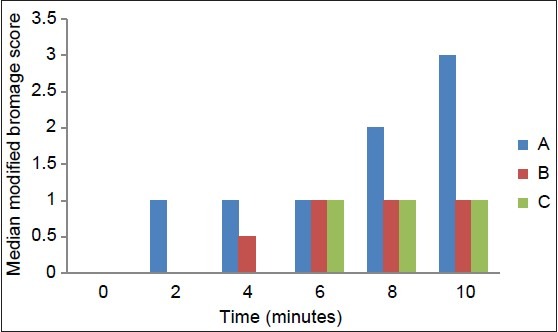
Motor block onset
Figure 2.
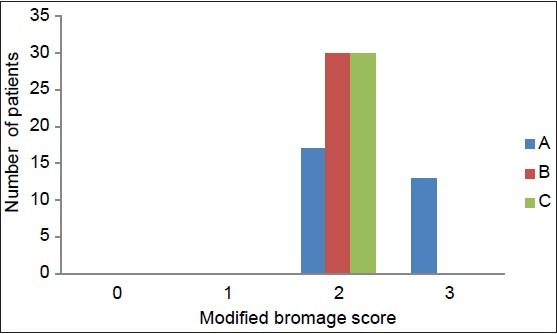
Quality of motor blockade
Table 3.
Motor block characteristics
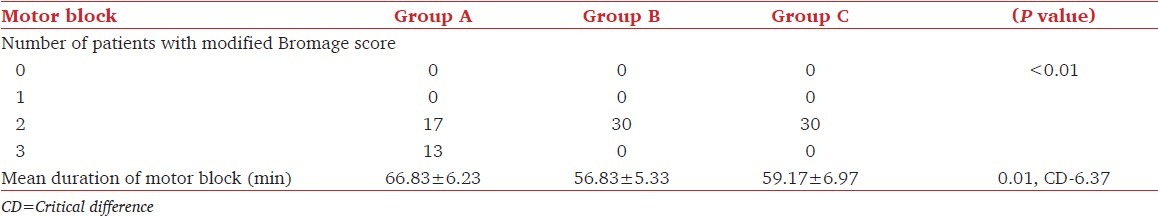
Figure 3.
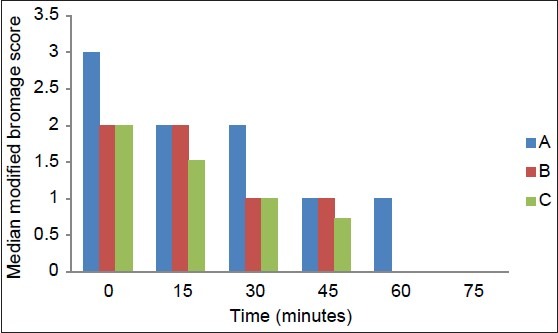
Motor block recovery
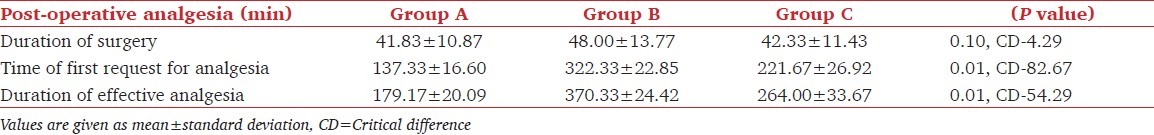
The duration of effective analgesia was taken as the time from the onset of adequate analgesia to the time of 1st request of analgesia (or VAS <4). The time to 1st post-operative analgesia request after arrival in the recovery room was significantly longer in Group B (322.33 ± 22.85 min) as compared to Group A (137.33 ± 16.60 min) and Group C (221.67 ± 26.92 min) [Table 4].
Table 4.
Post-operative analgesia
The baseline heart rate in all three groups was statistically comparable. There was an initial decrease in heart rate in first 10 min, which later settled. Overall trend in heart rate remained statistically comparable for the majority of time intervals in all the three groups intra-operatively. In post-operative period, there was a significant increase in the heart rate until the time for the need of rescue analgesic. This increase was significantly more and earlier in group A as compared to Groups B and C. Magnitude of increase (critical difference) was significantly lesser in Group B as compared to Group C [Figure 4].
Figure 4.
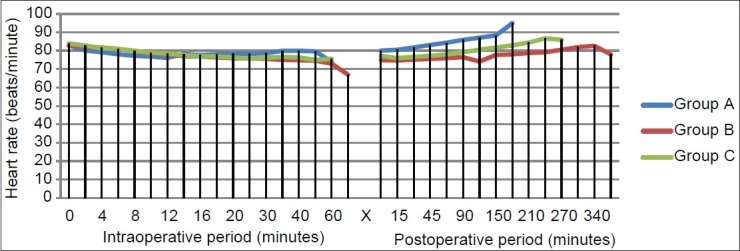
Perioperative heart rate trends
The baseline mean systolic blood pressure was comparable in all groups. There was a decrease in mean blood pressure in all groups for the first 10 min of study, which was statistically insignificant. Thereafter, the magnitude of decrease in blood pressure (critical difference) was significantly higher in plain bupivacaine group (6.21) followed by fentanyl (5.16) and sufentanil group (4.69). Post-operatively there was a trend of increase in mean blood pressure, which was statistically significant for initial 45 min especially in Group A, whereas mean blood pressure remained stable in Groups B and C post-operatively [Figure 5].
Figure 5.
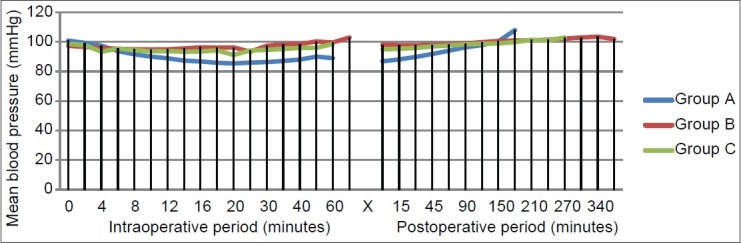
Perioperative mean blood pressure trends
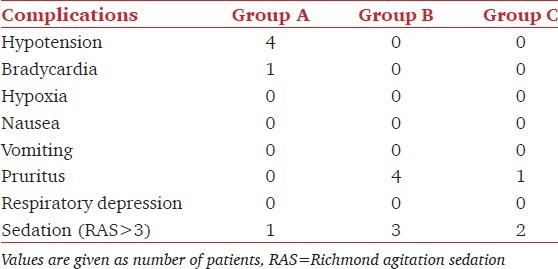
Perioperative side effects
Hypotension occurred in four patients in Group A while no patient in Groups B and C developed hypotension. Bradycardia was noted in only one patient in Group A. Incidence of pruritus was reported significantly higher in Group B (four patients) than Group C (one patient). No patient in Group A reported pruritus [Table 5]. None of patients in any group developed hypoxia or respiratory depression. Only six patients in our study were sedated to score 3 on Ramsay sedation scale (RSS) while the rest of the patients were sedated to score 2 on RSS.
Table 5.
Perioperative side-effects
Discussion
Patients presenting for endoscopic urological procedures like transurethral prostatectomy (TURP) under SAB usually have some coexisting cardiac, pulmonary or other co-morbid condition. It is imperative to limit the adverse hemodynamic and pulmonary effects associated with spinal block in these elderly patients. Using small doses of local anesthetics may limit these effects, but may not provide satisfactory analgesia. Opioids in conjunction with local anesthetics improve the quality of intraoperative analgesia and also prolong the duration of post-operative analgesia.[8] Morphine was the first opioid to be used intrathecally, but a wide variety of clinically relevant side-effects, especially respiratory depression limited its utility.[9] A favorable pharmacokinetic and pharmacodynamic profile of lipophilic opiates e.g. fentanyl and sufentanil, makes them better alternatives, because of a rapid uptake, faster onset and shorter duration of action. This minimizes the rostral migration of the drug to the respiratory center, avoiding delayed respiratory depression.[10] Sufentanil, a pure agonists is an N-4 thienyl derivative of fentanyl. It is considered to be more lipid soluble, a better receptor ligand and is 7-10 times more potent analgesic than fentanyl.[11]
In our study, the onset of adequate analgesia was delayed in sufentanil and fentanyl groups (12.73 and 11.50 min respectively) as compared with bupivacaine alone group (9.20 min). Cheng et al., and Palmer et al., in their studies observed that onset of analgesia was faster in fentanyl group as compared with sufentanil, when given intrathecally along with bupivacaine in labor analgesia.[12,13] Whereas, Ngiam and Fournier et al., concluded that both opioids had no significant difference in the onset of sensory blockade.[14,15]
Varying results have been seen regarding the sensory blockade level by various studies conducted until date. Our findings are at variance with that of Kim et al., who compared fentanyl and sufentanil with low dose bupivacaine in TURP.[16] They reported that the peak sensory block level was in the range of S1-T6 (mean L1) in fentanyl group and S1-T6 (mean T11) in sufentanil. Lo et al., also reported a significant higher blockade with sufentanil as compared to fentanyl and plain bupivacaine.[17] Our study is in consistence with that of Cheng et al., they reported a higher level of sensory block with fentanyl as compared to sufentanil.[12] In our study, the reasons for the increased block height in the bupivacaine alone group may be because of high dose (7.5 mg) of bupivacaine used as compared to low dose (5 mg) of bupivacaine when combined with fentanyl or sufentanil. The reasons for the increased block level in the fentanyl group compared with the sufentanil group may be related to the density of drug solution or opioid receptor affinities. Fentanyl and sufentanil have similar densities and the density of sodium chloride (0.9%) is higher than that of fentanyl or sufentanil. In our study, drug solution in sufentanil group contained 0.3 ml of normal saline making it denser than fentanyl group drug solution.
The time required to reach maximum height of the block was significantly more in sufentanil group (16.70 min) and fentanyl group (14.20 min) as compared to plain bupivacaine group (10.10 min). However, Kim et al., showed no significant difference in time to peak block level (15.4 min in fentanyl group and 15.1 min in sufentanil group).[16]
The duration of effective analgesia as defined by the time from intrathecal injection to the time of the first request for analgesia was 179.17 min in bupivacaine group, 370.33 min in bupivacaine-sufentanil group and 264.00 min in bupivacaine-fentanyl group. Trend toward longer analgesia with sufentanil than with fentanyl has also been supported by Ngiam et al., Lo et al., Nelson et al., in labor analgesia and cesarean section.[14,17,18]
Our study also highlighted the prolonged analgesic effect of addition of sufentanil to bupivacaine as compared to fentanyl. In a comparative trial in urological patients Donadoni et al., observed that intrathecal sufentanil (5 g) as a supplement to lignocaine provided a significant longer period of post-operative analgesia.[19]
Post-operatively, the VAS was significantly of higher values at all-time intervals in group receiving bupivacaine alone. Campbell et al., has also shown that VAS scores for pain were significantly higher in the bupivacaine alone group when compared to both sufentanil alone group and the bupivacaine-sufentanil group in labor analgesia.[6]
Addition of opioids to low dose bupivacaine definitely improves the analgesic effect and also leads to a significant beneficial effect of early ambulation because of minimal motor block. Kararmaz et al., demonstrated significantly prolonged motor block in plain bupivacaine group as compared to fentanyl with low dose bupivacaine in elderly patients undergoing TURP.[20] Lo et al., observed no significant variation in motor block characteristics in their study groups of combination of low dose bupivacaine (2.5 mg) with sufentanil (10 μg) and with fentanyl (10 μg) in combined spinal epidural.[17] Soni et al., also concluded that low dose intrathecal ropivacaine (3 mg) with sufentanil (10 μg) improved quality and duration of analgesia without impairing the motor strength during labor, to facilitate early ambulation.[21]
The use of sub anesthetic doses of local anesthetic is supported by the study conducted by Labbene et al. They suggested that the use of low dose bupivacaine (5 mg) when added to 25 μg fentanyl for endoscopic urological surgery results in short acting sensory block, without motor block and a lower incidence of cardiovascular side-effects as compared to either of 7.5 mg or 10 mg bupivacaine with 25 μg fentanyl.[22]
In our study, all three groups showed a slight decrease in heart rate intra-operatively, at all-time intervals. Only one patient in the plain bupivacaine group had an episode of significant bradycardia, which needed treatment in the form of inj. atropine intravenously.
The cardiovascular responses observed by Donadoni in his study groups of plain 5% heavy lignocaine (1.5 ml) with 1.5 ml normal saline and lignocaine (1.5 ml) in combination with sufentanil (5 μg), revealed a significant decrease in heart rate in the sufentanil group as compared to control group.[19] This difference, in their study was merely the result of a higher pre-operative rate in sufentanil group. Wang et al., explored the clinical efficacy of intrathecally administered low dose sufentanil - bupivacaine in TURP. They observed a significant decrease in heart rate in the combination group of sufentanil 5 μg with bupivacaine 7.5 mg in comparison to plain bupivacaine group and group administered sufentanil 7.5 μg and bupivacaine 7.5 mg intrathecally.[23]
In our study, 3 patients in Group A had hypotension, but no clinically significant hypotension was noted in other two groups. This is in accordance with the earlier study by Atallah et al., the combination of intrathecal low dose bupivacaine and fentanyl offers a reliable neuraxial block with stable hemodynamics.[24] Campbell et al., also reported no episode of hypotension when sufentanil in combination with bupivacaine was administered intrathecally.[6] Lo et al., in their study showed consistently lower blood pressure in sufentanil as compared to fentanyl group, which was statistically significant.[17] Olofsson et al., reported that low dose bupivacaine (7.5 mg) with sufentanil has shown to provide reliable anesthesia for the repair of hip fracture in the aged patients with few events of hypotension and little need for vasopressor support to maintain blood pressure.[7]
The administration of intrathecal opioids may provide the benefit in augmenting intraoperative and post-operative analgesia, but carries a risk of respiratory depression and oxygen desaturation. Many studies in the past have shown oxygen desaturation and respiratory depression as a frequent side effect of intrathecal sufentanil. There have been a several case report of respiratory arrest associated with intrathecal sufentanil.[25,26] However, in our study, no episode of respiratory depression or oxygen desaturation, occurred in any of the three group patients. Many studies on sufentanil as well as fentanyl have shown pruritus as the major side-effect.[27] Pruritus was noted in four patients of sufentanil group and one patient in fentanyl group in our study. Lo et al., also reported a higher incidence of pruritus in parturient receiving sufentanil (80%) than those receiving fentanyl (47%) intrathecally.[17]
A limitation of our study is that we have not used equipotent doses of fentanyl and sufentanil. The median effective doses (ED50) of intrathecal sufentanil and fentanyl are 2.6 and 14 μg respectively. And relative potency for intrathecal fentanyl to sufentanil in labor analgesia is 1:4.4 at the ED50 level. Therefore, intrathecal fentanyl 25 μg and sufentanil 5 μg could be considered as an equipotent dose.[16] However, we have used 10 μg sufentanil as has been used in various previous studies.[17,21,28]
To conclude, we opine that spinal anesthesia with low dose bupivacaine (5 mg) when combined with 10μ g sufentanil or 25 μg fentanyl provides adequate anesthesia for endoscopic urological procedures in elderly patients and is associated with a lower incidence of hemodynamic instability as compared to spinal anesthesia with 7.5 mg bupivacaine (0.5%) alone. We recommend sufentanil as an adjuvant to bupivacaine in spinal anesthesia for endoscopic urological procedures as it provides more effective and prolonged analgesia with less degree of motor block and a better hemodynamic stability as compared to fentanyl.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Bier A: Versuche uber cocainisirung des ruckenmarkes. (Experiments on the cocainization of the spinal cord) Deutsche Zeitschrift fur Chirurgie. 1899;51:361–9. [Google Scholar]
- 2.Dripps RD, Vandam LD. Long-term follow-up of patients who received 10,098 spinal anesthetics: Failure to discover major neurological sequelae. J Am Med Assoc. 1954;156:1486–91. doi: 10.1001/jama.1954.02950160016005. [DOI] [PubMed] [Google Scholar]
- 3.Lambert DH. Factors influencing spinal anesthesia. Int Anesthesiol Clin. 1989;27:13–20. doi: 10.1097/00004311-198902710-00004. [DOI] [PubMed] [Google Scholar]
- 4.Pert CB, Snyder SH. Opiate receptor: Demonstration in nervous tissue. Science. 1973;179:1011–4. doi: 10.1126/science.179.4077.1011. [DOI] [PubMed] [Google Scholar]
- 5.Maves TJ, Gebhart GF. Analgesic synergy between intrathecal opioids and local anesthetics. Anesth Analg. 1991;73:365–6. doi: 10.1213/00000539-199109000-00036. [DOI] [PubMed] [Google Scholar]
- 6.Campbell DC, Camann WR, Datta S. The addition of bupivacaine to intrathecal sufentanil for labor analgesia. Anesth Analg. 1995;81:305–9. doi: 10.1097/00000539-199508000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Olofsson C, Nygårds EB, Bjersten AB, Hessling A. Low-dose bupivacaine with sufentanil prevents hypotension after spinal anesthesia for hip repair in elderly patients. Acta Anaesthesiol Scand. 2004;48:1240–4. doi: 10.1111/j.1399-6576.2004.00504.x. [DOI] [PubMed] [Google Scholar]
- 8.Hunt CO, Naulty JS, Bader AM, Hauch MA, Vartikar JV, Datta S, et al. Perioperative analgesia with subarachnoid fentanyl-bupivacaine for cesarean delivery. Anesthesiology. 1989;71:535–40. doi: 10.1097/00000542-198910000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Bromage PR, Camporesi EM, Durant PA, Nielsen CH. Rostral spread of epidural morphine. Anesthesiology. 1982;56:431–6. doi: 10.1097/00000542-198206000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Singh C, Trikha A, Saxena A. Spinal Anaesthesia with bupivacaine and fentanyl. J Anaesth Clin Pharmacol. 1999;15:291–4. [Google Scholar]
- 11.Niemegeers CJ, Schellekens KH, Van Bever WF, Janssen PA. Sufentanil, a very potent and extremely safe intravenous morphine-like compound in mice, rats and dogs. Arzneimittelforschung. 1976;26:1551–6. [PubMed] [Google Scholar]
- 12.Cheng CJ, Sia AT, Lim EH, Loke GP, Tan HM. Either sufentanil or fentanyl, in addition to intrathecal bupivacaine, provide satisfactory early labour analgesia. Can J Anaesth. 2001;48:570–4. doi: 10.1007/BF03016834. [DOI] [PubMed] [Google Scholar]
- 13.Palmer CM, Cork RC, Hays R, Van Maren G, Alves D. The dose-response relation of intrathecal fentanyl for labor analgesia. Anesthesiology. 1998;88:355–61. doi: 10.1097/00000542-199802000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Ngiam SK, Chong JL. The addition of intrathecal sufentanil and fentanyl to bupivacaine for caesarean section. Singapore Med J. 1998;39:290–4. [PubMed] [Google Scholar]
- 15.Fournier R, Van Gessel E, Weber A, Gamulin Z. A comparison of intrathecal analgesia with fentanyl or sufentanil after total hip replacement. Anesth Analg. 2000;90:918–22. doi: 10.1097/00000539-200004000-00026. [DOI] [PubMed] [Google Scholar]
- 16.Kim SY, Cho JE, Hong JY, Koo BN, Kim JM, Kil HK. Comparison of intrathecal fentanyl and sufentanil in low-dose dilute bupivacaine spinal anaesthesia for transurethral prostatectomy. Br J Anaesth. 2009;103:750–4. doi: 10.1093/bja/aep263. [DOI] [PubMed] [Google Scholar]
- 17.Lo WK, Chong JL, Chen LH. Combined spinal epidural for labour analgesia: Duration, efficacy and side effects of adding sufentanil or fentanyl to bupivacaine intrathecally vs. plain bupivacaine. Singapore Med J. 1999;40:639–43. [PubMed] [Google Scholar]
- 18.Nelson KE, Rauch T, Terebuh V, D’Angelo R. A comparison of intrathecal fentanyl and sufentanil for labor analgesia. Anesthesiology. 2002;96:1070–3. doi: 10.1097/00000542-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Donadoni R, Vermeulen H, Noorduin H, Rolly G. Intrathecal sufentanil as a supplement to subarachnoid anaesthesia with lignocaine. Br J Anaesth. 1987;59:1523–7. doi: 10.1093/bja/59.12.1523. [DOI] [PubMed] [Google Scholar]
- 20.Kararmaz A, Kaya S, Turhanoglu S, Ozyilmaz MA. Low-dose bupivacaine-fentanyl spinal anaesthesia for transurethral prostatectomy. Anaesthesia. 2003;58:526–30. doi: 10.1046/j.1365-2044.2003.03153.x. [DOI] [PubMed] [Google Scholar]
- 21.Soni AK, Miller CG, Pratt SD, Hess PE, Oriol NE, Sarna MC. Low dose intrathecal ropivacaine with or without sufentanil provides effective analgesia and does not impair motor strength during labour: A pilot study. Can J Anaesth. 2001;48:677–80. doi: 10.1007/BF03016202. [DOI] [PubMed] [Google Scholar]
- 22.Labbene I, Lamine K, Gharsallah H, Jebali A, Adhoum A, Ghozzi S, et al. Spinal anesthesia for endoscopic urological surgery - low dose vs. varying doses of hyperbaric bupivacaine. Middle East J Anesthesiol. 2007;19:369–84. [PubMed] [Google Scholar]
- 23.Wang YC, Guo QL, Wang E, Zou WY. Spinal anesthesia with low dose sufentanil-bupivacaine in transurethral resection of the prostate. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2006;31:925–8. [PubMed] [Google Scholar]
- 24.Atallah MM, Shorrab AA, Abdel Mageed YM, Demian AD. Low-dose bupivacaine spinal anaesthesia for percutaneous nephrolithotomy: The suitability and impact of adding intrathecal fentanyl. Acta Anaesthesiol Scand. 2006;50:798–803. doi: 10.1111/j.1399-6576.2006.01063.x. [DOI] [PubMed] [Google Scholar]
- 25.Baker MN, Sarna MC. Respiratory arrest after second dose of intrathecal sufentanil. Anesthesiology. 1995;83:231–2. doi: 10.1097/00000542-199507000-00046. [DOI] [PubMed] [Google Scholar]
- 26.Katsiris S, Williams S, Leighton BL, Halpern S. Respiratory arrest following intrathecal injection of sufentanil and bupivacaine in a parturient. Can J Anaesth. 1998;45:880–3. doi: 10.1007/BF03012223. [DOI] [PubMed] [Google Scholar]
- 27.Wang Q, She SZ, Zhang YF, Lao JX, Jin YL. Effect of intrathecal administration of sufentanil at different doses on bupivacaine spinal anesthesia in gynecologic laparoscopy. Nan Fang Yi Ke Da Xue Xue Bao. 2008;28:1474–6. [PubMed] [Google Scholar]
- 28.Kaur M, Katyal S, Kathuria S, Singh P. A comparative evaluation of intrathecal bupivacaine alone, sufentanil or butorphanol in combination with bupivacaine for endoscopic urological surgery. Saudi J Anaesth. 2011;5:202–7. doi: 10.4103/1658-354X.82804. [DOI] [PMC free article] [PubMed] [Google Scholar]


