Abstract
Context:
Postoperative nausea and vomiting (PONV) is common after ambulatory surgery performed under general anesthesia. Anecdotal evidence suggests that caffeine may be useful in preventing PONV.
Aims:
The aim of the study was to determine efficacy of intravenous (IV) caffeine given prior to surgery is effective prophylaxis against PONV.
Settings and Design:
We conducted a prospective, randomized, double-blind, placebo-controlled study.
Subject and Methods:
Patients at moderate or high risk of PONV were randomized to receive IV caffeine (500 mg) or saline placebo during general anesthesia; all patients received dexamethasone and dolasetron.
Statistical analysis:
Statistical comparisons were tested using bivariable linear and logistic regression for each outcome and then adjusted for high/low risk.
Results:
Nausea in the postanesthesia care unit (PACU) was more common in the caffeine (16 of 62 patients) than the placebo group (seven of 69; P = 0.02). There were no significant differences in the use of rescue antiemetics in the PACU, in the incidence of nausea or vomiting over 24 h postoperatively, nor in other outcomes (headache, fatigue, or overall satisfaction) either in the PACU or at 24 h; time-to-discharge was similar for both groups.
Conclusion:
Caffeine was not effective in the prevention of PONV or headache, and did not improve time-to-discharge or patient satisfaction.
Keywords: Antiemetic prophylaxis, caffeine, postoperative nausea, postoperative vomiting
Introduction
Postoperative nausea and vomiting (PONV) is one of the most common complications associated with ambulatory surgery performed under general anesthesia.[1,2] The overall incidence of PONV during the first 24 h after surgery is approximately 30%, with considerable variability depending upon preoperative patient characteristics, factors related to the operation and anesthesia, and the intensity of pain and its management in the postoperative period.[3,4,5] For high-risk patients, the incidence may approach 80%.[3] Although rarely life-threatening, PONV is an unpleasant postoperative symptom. Patients with PONV may develop medical complications, consume more resources, require unplanned overnight admission to the hospital, and be less satisfied with the outcome of their surgery.[6]
The decision to provide antiemetic prophylaxis is based on the presence of risk factors for nausea and vomiting, as well as the potential for serious sequelae from vomiting.[6] Factors that contribute to an increased risk of PONV include history of motion sickness or previous PONV, female gender, perioperative opioid use, and nonsmoking status. Surgical procedure, anesthetic technique, and increased patient weight (possibly confounded by increased opioid use) also influence the risk of PONV.[4,5] Current standard practice entails use of a combination of antiemetics acting on multiple receptor types to reduce the incidence of PONV in high-risk patients.[6] Many antiemetic combinations have been tested; a currently popular regimen includes a serotonin antagonist (e.g., ondansetron or dolasetron) together with a corticosteroid (dexamethasone). Published studies suggest that combination therapy with dolasetron and dexamethasone may approach a 90% response rate (no nausea, no vomiting, and no use of rescue medication).[7,8]
Anecdotal evidence suggests that caffeine may be useful in the prevention of PONV. Caffeine is present in a number of analgesic preparations which are used in the prevention and treatment of headache and nausea in patients with migraine headache. Furthermore, caffeine withdrawal is associated with nausea and vomiting,[9] and has been shown to contribute to headache and fatigue following general anesthesia.[10,11,12] One of the authors cared for a patient who had experienced severe PONV following several prior anesthetics; this patient was convinced that intravenous (IV) caffeine had cured her PONV after multiple other drugs had failed. For a subsequent anesthetic, we treated this patient with prophylactic IV caffeine, 500 mg, in addition to our standard prophylactic therapy with dexamethasone and ondansetron; the patient had no nausea or vomiting.
We designed this study to test the hypothesis that IV caffeine, administered during general anesthesia in addition to standard antiemetic prophylaxis, would decrease the incidence of PONV in ambulatory surgery patients. We also hypothesized that caffeine would decrease postoperative headache and fatigue, reduce time to hospital discharge, and lead to increased patient satisfaction.
Materials and Methods
Outpatients scheduled for elective ambulatory surgery under general anesthesia were offered the opportunity to enroll in this prospective, randomized, double-blind, placebo-controlled study. The protocol was approved by the hospital's Committee on Clinical Investigations. Potential subjects were evaluated for the presence of four major risk factors for PONV: (1) Female gender, (2) nonsmoking status, (3) history of prior PONV or motion sickness, and (4) anticipated perioperative opioid use.[3] Only patients with at least two of the four major risk factors for PONV were consented for the study. Patients were asked how many cups of caffeinated beverages (coffee, tea, or soft drinks) they typically drank per day; customary daily caffeine intake was calculated assuming 100 mg caffeine per cup of coffee, 50 mg per cup of tea, and 30 mg per serving of soft drink.[13]
Following provision of written informed consent, patients were stratified by risk of PONV (two risk factors = moderate risk; three or four risk factors = high risk), and were randomized to receive either caffeine sodium benzoate, 500 mg in 2 ml (Bedford Laboratories, Bedford, Ohio) or saline placebo, 2 ml, administered as a single IV dose approximately 15 min before emergence from anesthesia.
All patients received a standardized general anesthetic, including midazolam (1-2 mg), fentanyl (50-250 g), propofol (100-300 mg), nitrous oxide, and sevoflurane or desflurane. If needed, muscle relaxation was provided by succinylcholine or vecuronium, and reversed with neostigmine and glycopyrrolate. All patients received our customary antiemetic prophylaxis consisting of dexamethasone, 8 mg, IV, just after induction and dolasetron, 12.5 mg, IV, approximately 15 min before the end of anesthesia. Patients at high risk of PONV (three or four risk factors) received additional prophylaxis at the discretion of the attending anesthesiologist (scopolamine patch or metoclopramide). In designing this study, we realized that the efficacy of our standard therapy might be sufficient to obscure any antiemetic benefit of caffeine, and that comparison with a control group receiving no antiemetic prophylaxis would have a higher probability of demonstrating an advantage for caffeine. However, inclusion of such a control group would be unethical, as modern standard practice mandates prophylaxis for high-risk patients.
The primary endpoint was the absence of nausea and vomiting and use of rescue antiemetic medication in the postanesthesia care unit (PACU) following surgery. Other outcomes measured in the PACU and again by phone 24 h postoperatively included nausea, vomiting, headache, fatigue, and overall patient satisfaction. Nausea and vomiting were recorded as number of episodes; other outcome variables were graded verbally on a scale from zero (none) - 10 (worst imaginable). Need for rescue antiemetic medication, as well as the length of stay in the PACU (Phase I and Phase II), were also noted.
We planned to include approximately 130 subjects based on a preliminary power calculation. This figure was arrived at using Blackwelder's scheme, assuming that the effect size would be small (0.10), the power would be 0.80, there would be four degrees of freedom, and the significance level would be 0.05.[14] We also assumed a dropout rate of about 10%.
The primary endpoint, the absence of nausea and vomiting in the PACU, was measured by chi-square test. The absence of nausea and vomiting over the first 24 h after surgery was also analyzed using the chi-square test. Secondary endpoints were analyzed using Fischer's exact tests, including verbal ratings of headache, alertness, fatigue, and satisfaction. Data analysis was done using Statistical Analysis Software (SAS).[15] Statistical comparisons were tested using bivariable linear and logistic regression for each outcome and then adjusted for high/low risk. Unadjusted and adjusted analyses were similar, so we report unadjusted results.
Results
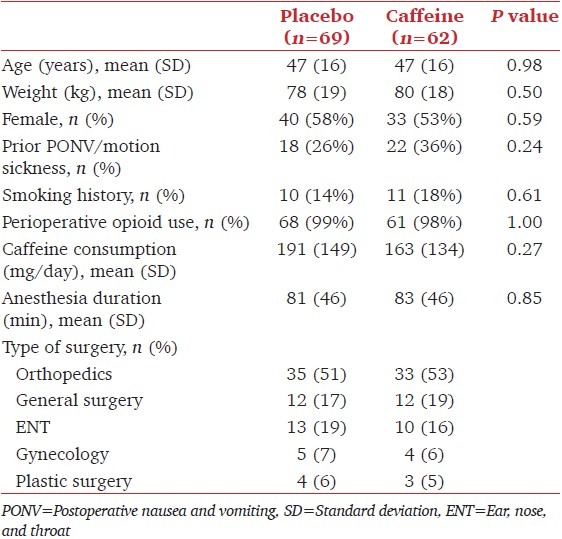
A total of 136 patients consented and were randomized; five were excluded from analyses because of protocol violations (one patient changed her mind after signing the consent form and therefore did not receive study drug, one patient did not receive general anesthesia, one patient was admitted overnight because of a change in the surgical procedure, and in two patients the anesthesia care provider failed to administer the drug at the appropriate time). Randomization resulted in demographically balanced arms with respect to age, weight, sex, prior PONV, smoking status, perioperative opiate use, customary daily caffeine consumption, anesthesia duration, and type of surgery [Table 1]. The proportion of high-risk subjects at entry was 66%. A majority of patients were females and nonsmokers. One high risk patient had a scopolamine patch placed preoperatively; another received metoclopramide, 10 mg IV.
Table 1.
Demographics
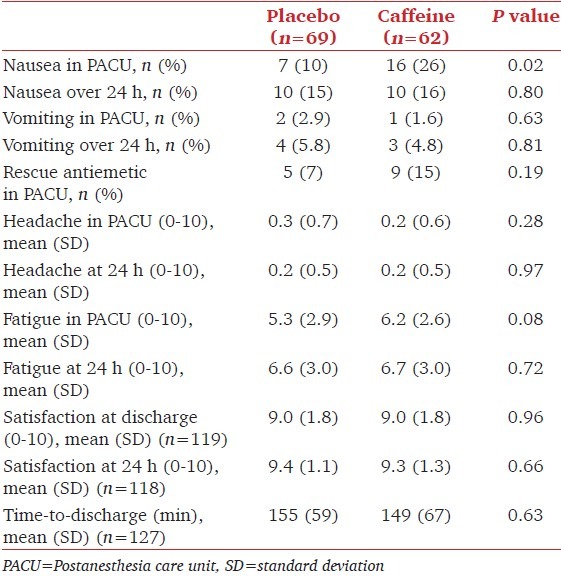
Nausea in the PACU was significantly more frequent among patients who had received IV caffeine (16 of 62 patients, 26%) than in patients who received placebo (seven of 69, 10%; P = 0.02), while vomiting in the PACU was uncommon in both groups (placebo, two of 69, 3%; caffeine, one of 62, 2%; P = 0.63). There were no significant differences in the use of rescue antiemetics in the PACU, nor in the incidence of nausea or vomiting over 24 h postoperatively [Table 2]. Overall, 73% of placebo group subjects experienced no nausea, vomiting, or need for rescue medications at any time. There were no significant differences in other outcomes (headache, fatigue, or satisfaction) either in the PACU or at 24 h; time-to-discharge was similar for both groups [Table 2].
Table 2.
Outcomes
Discussion
Contrary to our hypothesis, IV caffeine administered during general anesthesia in addition to standard antiemetic prophylaxis with dexamethasone and dolasetron, increased the incidence of postoperative nausea (but not vomiting) in ambulatory surgery patients. Furthermore, caffeine did not decrease postoperative headache and fatigue, reduce time-to-discharge, or lead to increased patient satisfaction.
The efficacy of our standard therapy with dexamethasone and dolasetron was relatively high (73%) in our study subjects, all of whom had at least two of four major risk factors for PONV, had no postoperative nausea, vomiting, or need for rescue medications. We cannot exclude the possibility that caffeine may exert a beneficial effect in the absence of other antiemetic prophylaxis; however, we considered withholding standard antiemetic prophylaxis in patients at high risk of PONV to be inconsistent with the current standard of care and therefore unethical. In addition, we included patients of both genders who had at least two risk factors as this was more representative of the general ambulatory population.
The dose of caffeine (500 mg) was selected as this is the same dose we have administered in attempts to prolong seizure duration in patients during electroconvulsive therapy; 500 mg caffeine appears to be a safe and effective dose for such patients. We administered this dose approximately 15 min before the end of surgery, the same time at which we customarily dose dolasetron. We cannot exclude the possibility that a different dose of caffeine, or a different time of administration might be more efficacious.
It is interesting that patients in the caffeine group experienced more nausea in the PACU than over 24 h. Together with our finding of a higher rate of nausea in the PACU in the caffeine group than with our customary antiemetic prophylaxis, this suggests a potential pro-emetic contribution of caffeine. Thus, our observations do not support our hypothesis that caffeine could decrease the incidence of PONV.
Conclusion
In this study in ambulatory surgery patients receiving standard antiemetic prophylaxis with dexamethasone and dolasetron during general anesthesia, IV caffeine did not decrease the incidence of PONV. Furthermore, caffeine did not decrease postoperative headache and fatigue, shorten time-to-discharge, or lead to increased patient satisfaction.
Acknowledgments
The authors thank Daniel W. Steinbrook, Anna T. R. Legedza, ScD, and Valerie Banner-Goodspeed for assistance with data analysis. Clinical Trials gov ID NCT00130026.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kapur PA. The big “little problem”. Anesth Analg. 1991;73:243–5. doi: 10.1213/00000539-199109000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Watcha MF, White PF. Postoperative nausea and vomiting. Its etiology, treatment, and prevention. Anesthesiology. 1992;77:162–84. doi: 10.1097/00000542-199207000-00023. [DOI] [PubMed] [Google Scholar]
- 3.Apfel CC, Laara E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting: Conclusions from cross-validations between two centers. Anesthesiology. 1999;91:693–700. doi: 10.1097/00000542-199909000-00022. [DOI] [PubMed] [Google Scholar]
- 4.Sinclair DR, Chung F, Mezei G. Can postoperative nausea and vomiting be predicted? Anesthesiology. 1999;91:109–18. doi: 10.1097/00000542-199907000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Gan TJ. Risk factors for postoperative nausea and vomiting. Anesth Analg. 2006;102:1884–98. doi: 10.1213/01.ANE.0000219597.16143.4D. [DOI] [PubMed] [Google Scholar]
- 6.Gan TJ, Meyer T, Apfel CC, Chung F, Davis PJ, Eubanks S, et al. Department of Anesthesiology, Duke University Medical Center. Consensus guidelines for managing postoperative nausea and vomiting. Anesth Analg. 2003;97:62–71. doi: 10.1213/01.ane.0000068580.00245.95. [DOI] [PubMed] [Google Scholar]
- 7.Henzi I, Walder B, Tramer MR. Dexamethasone for the prevention of postoperative nausea and vomiting: A quantitative systematic review. Anesth Analg. 2000;90:186–94. doi: 10.1097/00000539-200001000-00038. [DOI] [PubMed] [Google Scholar]
- 8.Apfel CC, Korttila K, Abdalla M, Kerger H, Turan A, Vedder I, et al. IMPACT Investigators. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. N Engl J Med. 2004;350:2441–51. doi: 10.1056/NEJMoa032196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fredholm BB, Battig K, Holmen J, Nehlig A, Zvartau EE. Actions of caffeine in the brain with special reference to factors that contribute to its widespread use. Pharmacol Rev. 1999;51:83–133. [PubMed] [Google Scholar]
- 10.Hampl KF, Schneider MC, Ruttimann U, Ummenhofer W, Drewe J. Perioperative administration of caffeine tablets for prevention of postoperative headaches. Can J Anaesth. 1995;42:789–92. doi: 10.1007/BF03011178. [DOI] [PubMed] [Google Scholar]
- 11.Nikolajsen L, Larsen KM, Kierkegaard O. Effect of previous frequency of headache, duration of fasting and caffeine abstinence on perioperative headache. Br J Anaesth. 1994;72:295–7. doi: 10.1093/bja/72.3.295. [DOI] [PubMed] [Google Scholar]
- 12.Weber JG, Klindworth JT, Arnold JJ, Danielson DR, Ereth MH. Prophylactic intravenous administration of caffeine and recovery after ambulatory surgical procedures. Mayo Clin Proc. 1997;72:621–6. doi: 10.1016/S0025-6196(11)63567-2. [DOI] [PubMed] [Google Scholar]
- 13. [Last accessed on 2008 Jan 8]. Available from: http://www.mayoclinic.com/health/caffeine/AN01211 .
- 14.Blackwelder WC. “Proving the null hypothesis” in clinical trials. Control Clin Trials. 1982;3:345–53. doi: 10.1016/0197-2456(82)90024-1. [DOI] [PubMed] [Google Scholar]
- 15.SAS version 9.1, Copyright 2002.2003 by SAS Institute Inc., Cary, NC, USA.


