Abstract
Spontaneous central vein thrombosis is a rare and potentially fatal condition in critical care setting. Activated protein C resistance due to homozygous factor V Leiden mutation is an exceptional cause of central venous thrombosis. We recently treated a healthy female student who presented with acute febrile illness, septic shock, and encephalopathy. Neck ultrasonography (USG) prior to an attempt of right internal jugular vein (IJV) cannulation revealed non compressibility of the vein along with absence of venous blood flow. Right IJV and subclavian vein thrombus was confirmed subsequently in USG Doppler by radiologist. Radiological evidence of distal pulmonary artery embolism in pulmonary angiography was also evident. Further investigations demonstrated homozygous Factor V Leiden mutation and activated factor C resistance and Dengue IgM positivity in our patient. Intravenous heparin followed by oral vitamin K anticoagulants (OVKA) aided in her recovery. Spontaneous intravascular thrombosis with activated protein C resistance and the relationship of acute Dengue infection were explored in our report.
Keywords: Activated protein C resistance, central neck vein, dengue infection, factor V Leiden mutation, thrombosis
Introduction
Spontaneous central vein thrombosis is a rare but potentially serious condition as it can present with a fatal pulmonary embolism.[1] It is often linked with deep neck infection, neoplastic and iatrogenic origin.[1] Activated protein C resistance (APC-R) due to homozygous factor V Leiden mutation is an exceptional cause of spontaneous central venous thrombosis. We describe here a right-sided internal jugular vein (IJV) and subclavian vein (SCV) thrombosis in a patient due to APC-R and homozygous Factor V Leiden mutation. Dengue immunoglobulin M (IgM) was eventually found positive. The relationship with dengue viral infection and APC-R with central vein thrombus has been explored.
Case Report
A 21-year-old non-obese female patient with no co-morbid illness was referred to our intensive care unit (ICU) from a private hospital with history of high grade fever with chills 8 days back with respiratory distress for 6 days and altered sensorium for 2 days. She was apparently healthy, unmarried, and had no history of hormone intake. She was intubated for altered sensorium and had already received mechanical ventilation for 48 hours. She was referred to us in a state of shock with vasopressors infusions on flow (dopamine through peripheral line). Additionally, she had edematous peripheries (right upper limb swelling was more as compared to the left). She had leukocytopenia (2,400/cmm), thrombocytopenia (20,000/cmm), and normal prothrombin time, activated partial thromboplastin, and thrombin times and fibrinogen levels. Neck ultrasonography (USG) prior to an attempt of right IJV cannulation revealed a non-compressible right IJV along with absence of venous flow in color Doppler strongly suggestive of right IJV thrombus. Her left IJV and SCV were compressible (checked by using linear ultrasound probe supraclavicularly) and patent, hence we inserted the central line in the left SCV for hemodynamic monitoring, fluid resuscitation and vasopressor use. Radiologists evaluated and confirmed right IJV thrombus with extension towards right SCV. Her lower limb Doppler study was, however, within normal limits. Echocardiography showed mild tricuspid regurgitation with ejection fraction <55% with mild dilatation of main pulmonary arteries. Urgent thoracic computed tomography (CT) angiography revealed left distal pulmonary artery thrombosis [Figure 1]. We immediately started unfractionated heparin (loading dose: 80 U/kg followed by continuous infusion @ 20 U/kg/hr.) to achieve a target activated partial thromboplastin time (APTT) of 2-2.5 times the normal. Further investigations demonstrated APC-R using the test kit STA -staclot APC-R (Diagnostica Stago, Asnieres, France) and genetic markers for thrombosis using polymerase chain reaction showed homozygous to Factor V Leiden mutation. After achieving the target APTT, oral vitamin K anticoagulants (OVKA) in the form of warfarin 5 mg was started along with the heparin to aim international normalized ratio (INR) of 2-2.5. We achieved target INR within next 5 days. Then, heparin was stopped and warfarin was continued. Her other supportive management included fluids, sedation, vasopressors, broad spectrum antibiotics, enteral nutrition, and mechanical ventilation. In the meantime, Dengue IgM Enzyme-linked immunosorbent assay (ELISA) (Dengue IgM capture ELISA, PanBio, Australia) was also found to be positive. Within the next week her hemodynamic status improved and she could be weaned off from the ventilator. After the shock recovered, we did thrombophilia testing of this patient [Table 1]. Her swelling of the right upper limb was regressed gradually. But, her right IJV and SCV thrombus persisted with partial recanalization in follow up USG [Figure 2]. She was discharged on oral warfarin treatment. She is now under our follow-up. Importantly, her father, mother, and younger sister underwent factor 5 Leiden mutation test which was tested negative.
Figure 1.

Computer tomography angiography scan of thorax coronal view showing pulmonary artery thrombus (arrowed)
Table 1.
Thrombosis screening in our patient
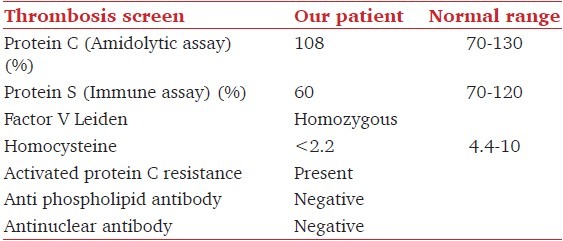
Figure 2.
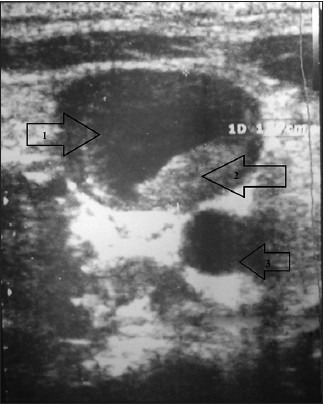
USG scan of right IJV (1) showing presence of partial thickness thrombus (2) and right carotid artery (3) (follow up pictures)
Discussion
APC-R is an autosomal dominant abnormality leading to thrombophilia due to point mutation (position 1691) in the Factor V gene.[1,2] With this mutation, Factor V becomes unresponsive to proteolytic action of activated protein C. Thus protein C resistance occurs and resulting in uninhibited coagulation and intravascular thrombosis. The clinical picture is of spontaneous intravascular thrombosis at an early age (>45 years) in an unusual venous site or pulmonary embolism or recurrence.[1] Hence after radiological confirmation of right IJV thrombus and thoracic CT angiography, thrombophilia testing was initiated. Age of the patient and unusual venous site thrombus with distal pulmonary artery thrombus prompted us to send thrombophilia testing for secondary prevention.[3]. Additionally, we did testing for homocysteine levels which were very low in our patient. Epidemiological studies have proved that increased homocysteine level is a risk for venous thrombosis,[4] but the recent evidence has also challenged this concept.[5]
Antibodies against Dengue antigen nonstructural protein 1 (NS1) can cross-react with endothelial cells, leading to endothelial activation and expression of more cytokine, chemokines, and adhesion molecules, resulting in widespread endothelial cell damage.[6] Dengue virus infected endothelial cells can inhibit prostacyclin release and intensify von Willebrand Factor release from endothelial cells.[6,7] These can lead to increase platelet plugging and intravascular thrombosis. Similar intravascular thrombosis is also known with sepsis of any cause.[8] In our case, we believe that central venous thrombosis was due to dengue infection mediated endothelial injury or dengue virus sepsis syndrome induced.
Venous thromboembolism in patients with Factor V Leiden mutation related heritable thrombophilias is managed with anticoagulants.[1] OVKA, like warfarin, are preferred with a target INR of 2.5 (range 2.0-3.0).[9] The duration of anticoagulant therapy (3-6 months) is based on the risk factors, no of events, recurrence, and area of involvement.[9] After a first episode, like in this case, the British Committee recommends anticoagulation for 6 months.[9]
Conclusion
This case report elaborates about a rare incidence of spontaneous central vein thrombosis in a patient of ACP-R. The relation between dengue infections and dengue viral sepsis with spontaneous thrombosis in a predisposed patient was also explored. This case report also emphasizes the significance of USG as fortuitous detection of central vein thrombosis during USG for venous access.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Mnejja M, Hammami B, Bougacha L, Jemal L, Chakroun N, Chakroun A, et al. Internal jugular vein thrombosis by protein C activated resistance. Eur Ann Otorhinolaryngol Head Neck Dis. 2011;128:269–7. doi: 10.1016/j.anorl.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 2.Bertina RM, Koeleman BP, Koiser T, Rosendaal FR, Dirven RJ, de Ronde H, et al. Mutation in the blood coagulation factor V associated with resistance to activated protein C. Nature. 1994;369:64–7. doi: 10.1038/369064a0. [DOI] [PubMed] [Google Scholar]
- 3.Middeldorp S. Evidence-based approach to thrombophilia testing. J Thromb Thrombolysis. 2011;31:275–81. doi: 10.1007/s11239-011-0572-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Homocysteine Studies Collaboration. Homocysteine and risk of ischemic heart disease and stroke. JAMA. 2002;288:2015–22. doi: 10.1001/jama.288.16.2015. [DOI] [PubMed] [Google Scholar]
- 5.Fay WP. Homocysteine and thrombosis: Guilt by association? Blood. 2012;119:2977–8. doi: 10.1182/blood-2012-01-401513. [DOI] [PubMed] [Google Scholar]
- 6.Basu A, Chaturvedi UC. Vascular endothelium: The battlefield of dengue viruses. FEMS Immunol Med Microbiol. 2008;53:287–99. doi: 10.1111/j.1574-695X.2008.00420.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jiang L, Guo H, Fang D. Effect of dengue virus infection on the production of ET-1 and PGI2 by human vascular endothelial cells. Zhonghua Shi Yan He Lin Chuang Bing Du Xue Za Zhi. 1999;13:239–42. [PubMed] [Google Scholar]
- 8.Levi M. Disseminated intravascular coagulation. Crit Care Med. 2007;35:2191–5. doi: 10.1097/01.ccm.0000281468.94108.4b. [DOI] [PubMed] [Google Scholar]
- 9.Baglin T, Gray E, Greaves M, Hunt BJ, Keeling D, Machin S, et al. British Committee for Standards in Haematology. Clinical guidelines for testing for heritable thrombophilia. Br J Haematol. 2010;149:209–20. doi: 10.1111/j.1365-2141.2009.08022.x. [DOI] [PubMed] [Google Scholar]


