Abstract
Background
Ischaemic heart disease (IHD) is the leading cause of death worldwide. The World Health Organisation (WHO) collects mortality data coded using the International Statistical Classification of Diseases (ICD) code.
Methods
We analysed IHD deaths world-wide between 1995 and 2009 and used the UN population database to calculate age-specific and directly and indirectly age-standardised IHD mortality rates by country and region.
Results
IHD is the single largest cause of death worldwide, causing 7,249,000 deaths in 2008, 12.7% of total global mortality. There is more than 20-fold variation in IHD mortality rates between countries. Highest IHD mortality rates are in Eastern Europe and Central Asian countries; lowest rates in high income countries. For the working-age population, IHD mortality rates are markedly higher in low-and-middle income countries than in high income countries.
Over the last 25 years, age-standardised IHD mortality has fallen by more than half in high income countries, but the trend is flat or increasing in some low-and-middle income countries. Low-and-middle income countries now account for more than 80% of global IHD deaths.
Conclusions
The global burden of IHD deaths has shifted to low-and-middle income countries as lifestyles approach those of high income countries. In high income countries, population ageing maintains IHD as the leading cause of death. Nevertheless, the progressive decline in age-standardised IHD mortality in high income countries shows that increasing IHD mortality is not inevitable. The 20-fold mortality difference between countries, and the temporal trends, may hold vital clues for handling IHD epidemic which is migratory, and still burgeoning.
Keywords: Ischaemic heart disease, Coronary heart disease, Mortality, Trends
1. Introduction
Ischaemic heart disease (IHD) is the leading cause of death worldwide [1–4], placing a major economic and resource burden on health and public health systems. High income countries have seen declines in mortality rates from IHD [5–10], but elsewhere the picture is less favourable, with continued high IHD mortality [11]. Reliable information describing time-trends in IHD mortality is essential to understand and monitor the disease [12]. In this article we provide an overview of the global epidemiology of IHD mortality using data submitted by individual member states to the World Health Organisation. The data cover the period 1995 to 2009, and are more complete for some countries than for others. We have analysed the data to allow identification of country-specific and broad regional trends.
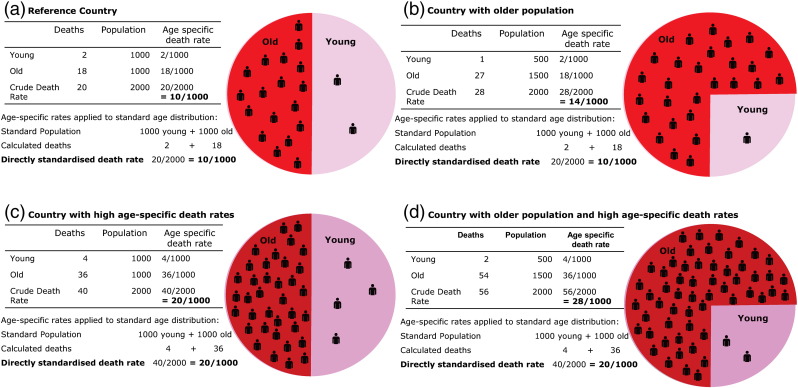
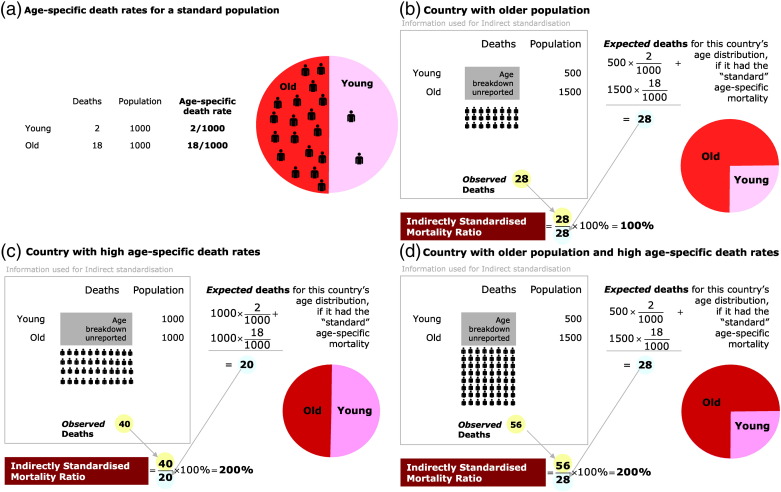
We present absolute IHD burden, along with directly and indirectly standardised IHD mortality rates. Absolute burden reflects the total number of deaths a health system has to deal with, which will tend to be larger in more populous countries. Standardised rates are preferable for comparing countries because they remove the effects of population size and age structure. The most comprehensive standardisation is direct standardisation (Fig. 1), which requires age-specific data for both the number of deaths in each country and its population size. In many countries age-specific data on deaths from IHD are not available, but the UN does provide modelled estimates of age-specific population counts for all countries. Indirect standardisation (Fig. 2) divides the deaths observed in a country, by the deaths expected if that country had the same age-specific death rates as a population group chosen to be the standard for comparison. We present indirectly standardised ratios for countries where direct standardisation is not possible due to lack of age-specific death data.
Fig. 1.
(a) A standard population of 2000 people, distributed equally amongst "young" (under 60 years) and "old" (60 years and older) groups which have different death rates. This distribution of ages will be used as the "standard" in the other panels. (b) A country with the same age-specific risks, but whose population is older. Crude death rate is higher because a greater proportion of people are in the high-risk age group. However, age-standardisation prevents the ageing artefact by reconstituting a population of the "standard" age distribution, to obtain the same standardised death rate as (a). (c) A country which, compared with (a), has double the death rate at each age group. Crude death rates, and age-standardised death rates are doubled (d) A country with double the age-specific mortality and an older population. Crude mortality is very much higher but age-standardised mortality, which reconstitutes a standard distribution of ages, is only twice that of panel (a).
Fig. 2.
If a country reports age-specific population but only total IHD deaths (without an age breakdown), it is not possible to calculate directly standardised mortality rates. Instead, by making the assumption that the age relationship of mortality is a scaled-up or scaled-down version of that of a standard population, it is possible to calculate an indirectly standardised mortality ratio expressing the country's mortality relative to that of the standard population. Panels (b), (c) and (d) calculate the indirectly standardised mortality ratio for the same country data as the corresponding panels in Figure 1, but with the age breakdown of deaths concealed.
2. Methods
2.1. Data sources
IHD mortality data (ICD9 codes 410–414 and ICD10 codes I20–25) between 1995 and 2009 were extracted from the online World Health Organisation (WHO) mortality database [13] and from WHO publications [14,15]. These data comprise all deaths registered by national civil registration systems which were submitted to WHO, with underlying cause of death coded by the relevant national authority using the International Statistical Classification of Diseases and Related Health Problems (ICD) 9th or 10th revision [16]. In some countries data were only available for parts of this time period: in these cases the available years are shown. Population data were from UN population estimates also available online [17]. For comparisons by region and country income group, we have used 2001 data from the WHO, which are the most complete.
2.2. Statistics
2.2.1. Age-specific and age-standardised mortality rates
Age specific mortality rates for each five year age group are presented. In addition we present directly standardised IHD mortality rates (standardised to WHO world standard population) [18] to allow comparison of mortality rates between countries. We also present indirectly standardised ratios for countries where direct standardisation is not possible, by calculating deaths expected if a country had the same age-specific death rate as the standard population (defined here as the average age-specific mortality rates in 2001 of the UK, USA, Canada, France and Germany).
The authors of this manuscript have certified that they comply with the principles of ethical publishing in the International Journal of Cardiology.
These authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
3. Results
3.1. Burden of IHD worldwide in 2008
In 2008 there were 7,249,000 deaths from IHD, accounting for 12.7% of all global deaths. India and China together had over 2 million deaths or over 30% of the world's total IHD burden (Table 1). Large numbers of deaths were also seen in the Russian Federation (659,000) and in USA (445,800) reflecting their large population sizes.
Table 1.
Global burden of IHD deaths (thousands).
| High income countries |
East Asia and Pacific |
Europe and Central Asia |
Latin American and the Caribbean |
Middle East and North Africa |
South Asia |
Sub-Saharan Africa |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rank | Country | Number | Rank | Country | Number | Rank | Country | Number | Rank | Country | Number | Rank | Country | Number | Rank | Country | Number | Rank | Country | Number |
| 1 | USA | 445.8 | 1 | China | 1040.6 | 1 | Russian Federation | 659.5 | 1 | Brazil | 133.9 | 1 | Iran | 88.0 | 1 | India | 1248.0 | 1 | Nigeria | 71.6 |
| 2 | Germany | 155.8 | 2 | Indonesia | 242.8 | 2 | Ukraine | 338.1 | 2 | Mexico | 77.0 | 2 | Egypt | 78.8 | 2 | Pakistan | 195.5 | 2 | Ethiopia | 43.5 |
| 3 | Japan | 105.5 | 3 | Myanmar | 58.2 | 3 | Turkey | 81.2 | 3 | Argentina | 36.4 | 3 | Morocco | 33.7 | 3 | Bangladesh | 163.4 | 3 | Sudan | 39.2 |
| 4 | United Kingdom | 92.3 | 4 | Philippines | 57.8 | 4 | Romania | 56.7 | 4 | Colombia | 27.7 | 4 | Iraq | 26.7 | 4 | Afghanistan | 30.9 | 4 | Dem Republic Congo | 27.0 |
| 5 | Italy | 87.8 | 5 | Thailand | 53.3 | 5 | Belarus | 56.1 | 5 | Venezuela | 21.2 | 5 | Yemen | 17.7 | 5 | Nepal | 21.1 | 5 | South Africa | 20.5 |
| 6 | Poland | 79.0 | 6 | Malaysia | 22.7 | 6 | Uzbekistan | 51.7 | 6 | Cuba | 18.2 | 6 | Algeria | 14.7 | 6 | Sri Lanka | 15.9 | 6 | Tanzania | 19.1 |
| 7 | Spain | 43.5 | 7 | Cambodia | 9.1 | 7 | Kazakhstan | 48.3 | 7 | Chile | 9.8 | 7 | Syrian Arab Republic | 14.3 | 7 | Bhutan | 0.9 | 7 | Côte d'lvoire | 14.9 |
| 8 | France | 42.6 | 8 | Lao People's Republic | 5.7 | 8 | Bulgaria | 23.1 | 8 | Dominican Republic | 9.7 | 8 | Tunisia | 10.1 | 8 | Maldives | 0.1 | 8 | Uganda | 13.5 |
| 9 | Canada | 42.0 | 9 | Papua New Guinea | 4.5 | 9 | Georgia | 20.0 | 9 | Peru | 9.2 | 9 | Libyan Arab Jamahiriya | 6.7 | 9 | Kenya | 13.5 | |||
| 10 | Hungary | 33.6 | 10 | Mongolia | 1.1 | 10 | Serbia | 17.5 | 10 | Honduras | 6.2 | 10 | Lebanon | 5.9 | 10 | Ghana | 13.1 | |||
| 11 | Czech Republic | 28.5 | 11 | Fiji | 0.8 | 11 | Azerbaijan | 16.3 | 11 | El Salvador | 4.9 | 11 | Jordan | 4.7 | 11 | Mozambique | 12.9 | |||
| 12 | Australia | 24.9 | 12 | Timor-Leste | 0.5 | 12 | Republic of Moldova | 16.2 | 12 | Ecuador | 4.4 | 12 | Djibouti | 0.8 | 12 | Cameroon | 11.3 | |||
| 13 | Saudi Arabia | 20.9 | 13 | Solomon Islands | 0.2 | 13 | Lithuania | 14.9 | 13 | Guatemala | 4.4 | 13 | Malawi | 9.4 | ||||||
| 14 | Republic of Korea | 20.5 | 14 | Samoa | 0.1 | 14 | Kyrgyzstan | 12.9 | 14 | Uruguay | 4.0 | 14 | Angola | 7.6 | ||||||
| 15 | Slovakia | 18.4 | 15 | Vanuatu | 0.1 | 15 | Turkmenistan | 11.7 | 15 | Paraguay | 3.1 | 15 | Madagascar | 7.4 | ||||||
| 16 | Sweden | 17.0 | 16 | Tonga | 0.1 | 16 | Armenia | 10.5 | 16 | Jamaica | 3.1 | 16 | Somalia | 7.1 | ||||||
| 17 | Austria | 14.6 | 17 | Latvia | 9.9 | 17 | Nicaragua | 3.1 | 17 | Zambia | 6.9 | |||||||||
| 18 | Belgium | 13.9 | 18 | Tajikistan | 6.7 | 18 | Haiti | 2.9 | 18 | Guinea | 5.7 | |||||||||
| 19 | Greece | 13.1 | 19 | Bosnia and Herzegovina | 5.5 | 19 | Costa Rica | 2.8 | 19 | Chad | 5.3 | |||||||||
| 20 | Netherlands | 12.7 | 20 | Albania | 5.4 | 20 | Panama | 1.7 | 20 | Zimbabwe | 5.2 | |||||||||
| 21 | Croatia | 12.3 | 21 | Montenegro | 0.6 | 21 | Guyana | 0.9 | 21 | Burkina Faso | 5.1 | |||||||||
| 22 | Finland | 11.4 | 22 | Suriname | 0.4 | 22 | Benin | 4.1 | ||||||||||||
| 23 | Portugal | 10.4 | 23 | St Vincent and Grenades | 0.1 | 23 | Mali | 4.0 | ||||||||||||
| 24 | Switzerland | 9.8 | 24 | Belize | 0.1 | 24 | Niger | 3.7 | ||||||||||||
| 25 | Denmark | 6.7 | 25 | Saint Lucia | 0.1 | 25 | Burundi | 3.6 | ||||||||||||
| 26 | Norway | 6.0 | 26 | Grenada | 0.1 | 26 | Senegal | 3.5 | ||||||||||||
| 27 | New Zealand | 5.7 | 27 | Rwanda | 3.4 | |||||||||||||||
| 28 | Ireland | 5.3 | 28 | Togo | 2.9 | |||||||||||||||
| 29 | Estonia | 4.9 | 29 | Republic | 2.8 | |||||||||||||||
| 30 | Singapore | 4.7 | 30 | Congo | 2.1 | |||||||||||||||
| 31 | Israel | 4.7 | 31 | Sierra Leone | 1.8 | |||||||||||||||
| 32 | Slovenia | 2.4 | 32 | Liberia | 1.6 | |||||||||||||||
| 33 | Oman | 2.2 | 33 | Eritrea | 1.5 | |||||||||||||||
| 34 | Trinidad and Tobago | 1.7 | 34 | Mauritius | 1.4 | |||||||||||||||
| 35 | Kuwait | 1.2 | 35 | Lesotho | 1.4 | |||||||||||||||
| 36 | United Arab Emirates | 1.2 | 36 | Namibia | 1.3 | |||||||||||||||
| 37 | Cyprus | 1.0 | 37 | Mauritania | 1.2 | |||||||||||||||
| 38 | Malta | 0.7 | 38 | Guinea-Bissau | 1.0 | |||||||||||||||
| 39 | Luxemberg | 0.5 | 39 | Botswana | 0.8 | |||||||||||||||
| 40 | Iceland | 0.4 | 40 | Gabon | 0.8 | |||||||||||||||
| 41 | Equatorial Guinea | 0.4 | 41 | Swaziland | 0.7 | |||||||||||||||
| 42 | Bahrain | 0.2 | 42 | Gambia | 0.7 | |||||||||||||||
| 43 | Qatar | 0.2 | 43 | Comoros | 0.3 | |||||||||||||||
| 44 | Barbados | 0.2 | 44 | Cape Verde | 0.2 | |||||||||||||||
| 45 | Bahamas | 0.1 | 45 | Principe | 0.1 | |||||||||||||||
| 46 | Brunei Darussalam | 0.1 | ||||||||||||||||||
Data from the World Health Organisation 2008. Ranked by country burden.
Worldwide in 2001 [15], IHD was the leading cause of death in both low-and-middle income countries (11.8% of all deaths) and high income countries (17.3% of all deaths). At that time IHD was the leading cause of death in all but two world regions: Sub-Saharan Africa and East Asia and the Pacific. IHD was the leading cause of death in Europe and Central Asia (29.7% of total deaths), Middle East and North Africa (16.9% of total deaths), South Asia (13.6% of total deaths) and Latin America (10.9% of total deaths). In contrast, in Sub-Saharan Africa IHD was the eighth cause of death after HIV/AIDS, malaria, lower respiratory tract infections, diarrhoeal disease, perinatal conditions, measles, cerebrovascular disease, accounting for only 3.2% total deaths. In East Asia and the Pacific, IHD was the third leading cause of death accounting for 8.8% of total deaths.
3.2. Impact of age on IHD mortality
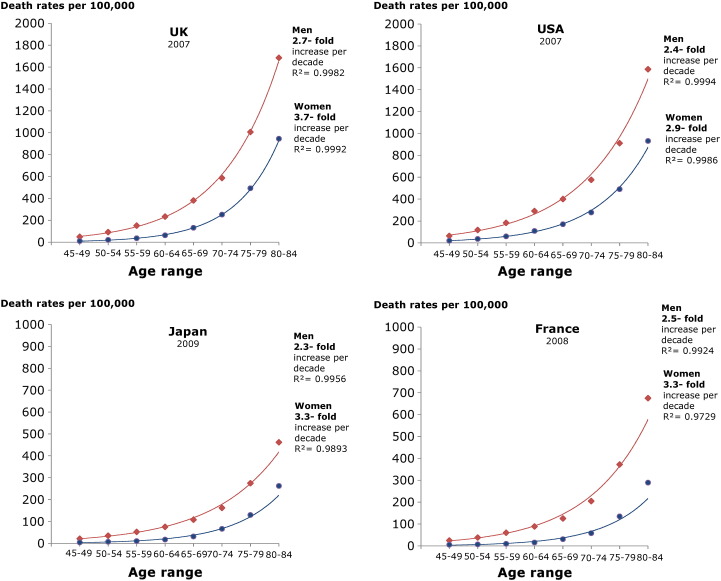
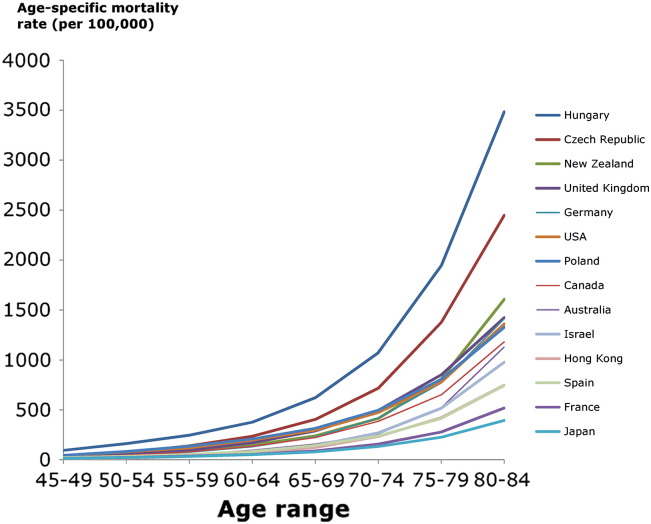
Fig. 3 shows the progressive increase in IHD mortality with age in 4 selected countries: UK, USA, Japan and France. In the years illustrated, women have a lower IHD mortality rate than men. There is a progressive increase in IHD mortality with age, which fits an exponential trend. In these countries, chosen for illustration because they have complete data, there is a 2.3 to 2.7-fold increase in IHD mortality for every decade of life for men and a 2.9 to 3.7-fold increase for women. Fig. 4 illustrates that the exponential rise in mortality with age is present in all countries regardless of starting mortality level or country income level.
Fig. 3.
Change in mortality with age in UK, USA, Japan and France.
Fig. 4.
IHD mortality by population age group for selected countries. Age-specific mortality rate for selected countries. The most recent year of available data between 2005 and 2009 is displayed.
3.3. Age specific mortality rates from IHD in 2001
Age specific mortality rates for IHD were higher in low-and-middle income countries than in high income countries (Tables 2a and 2b). For older ages highest rates were seen in Europe and Central Asia, South Asia and the Middle East and North Africa. For example, for men in the age range 80 years and over the death rates per 100,000 population were 8598 in Europe and Central Asia, 3758 in Middle East and North Africa and 3644 in South Asia. Meanwhile in high income countries the rate was 2253 per 100,000 population.
Table 2a.
Age specific death rates from IHD in 2001 (Male).
| Regions | Age specific death rates from IHD (per 100,000 population) |
|||||||
|---|---|---|---|---|---|---|---|---|
| 0–4 | 5–14 | 15–29 | 30–44 | 45–59 | 60–69 | 70–79 | 80 + | |
| Low income countries | ||||||||
| East Asia and Pacific | 1 | 1 | 3 | 15 | 79 | 304 | 779 | 1606 |
| Europe and Central Asia | 0 | 0 | 6 | 89 | 517 | 1591 | 3571 | 8598 |
| Latin America and Caribbean | 0 | 0 | 3 | 17 | 126 | 414 | 939 | 1956 |
| Middle East and North Africa | 0 | 0 | 5 | 45 | 304 | 956 | 2156 | 3758 |
| South Asia | 2 | 2 | 5 | 35 | 302 | 1005 | 2207 | 3644 |
| Sub-Saharan Africa | 0 | 0 | 1 | 14 | 139 | 526 | 1345 | 2291 |
| High income countries | ||||||||
| High income countries | 0 | 0 | 1 | 13 | 91 | 298 | 805 | 2253 |
Data from the World Health Organisation.
Table 2b.
Age specific death rates from IHD in 2001 (Female).
| Age Specific Death Rates from IHD (per 100,000 population) |
||||||||
|---|---|---|---|---|---|---|---|---|
| Regions | 0–4 | 5–14 | 15–29 | 30–44 | 45–59 | 60–69 | 70–79 | 80 + |
| Low income countries | ||||||||
| East Asia and Pacific | 0 | 0 | 3 | 8 | 47 | 227 | 647 | 1776 |
| Europe and Central Asia | 0 | 0 | 2 | 16 | 132 | 666 | 2261 | 7911 |
| Latin America and Caribbean | 0 | 0 | 1 | 7 | 55 | 223 | 567 | 1758 |
| Middle East and North Africa | 0 | 0 | 2 | 16 | 137 | 587 | 1565 | 3618 |
| South Asia | 2 | 1 | 9 | 25 | 163 | 790 | 1945 | 3217 |
| Sub-Saharan Africa | 0 | 0 | 1 | 6 | 86 | 410 | 1041 | 2212 |
| High income countries | ||||||||
| High income countries | 0 | 0 | 0 | 3 | 23 | 107 | 401 | 1789 |
Data from the World Health Organisation.
The difference in mortality between regions was even more marked for premature IHD mortality in the working-age population (defined as those aged < 60 years). In men this was again highest in Europe and Central Asia and then Middle East and North Africa and South Asia. For example, in men in the age range 45–59 years the death rate in Europe and Central Asia was 517 per 100,000 population, in Middle East and North Africa 304 and in South Asia 302. By contrast in high income countries, the IHD death rate in the same age group was 91 per 100,000 population, less than one-fifth of the mortality seen in low-and-middle income Europe and Central Asia.
3.4. Time trends in age-standardised IHD mortality rates
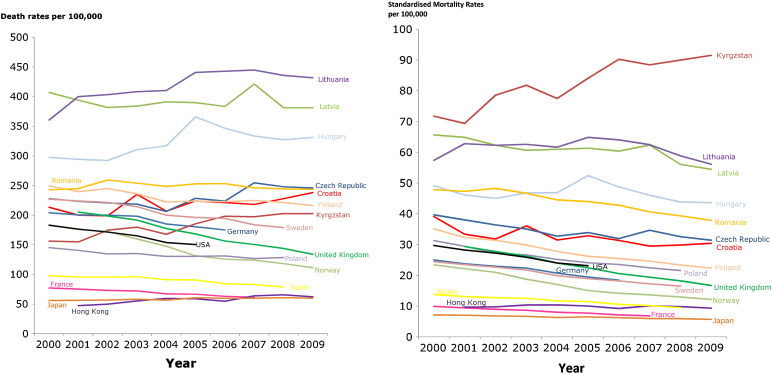
Time series of directly-standardised IHD mortality rates between 2000 and 2009 (standardised to the WHO world standard population) are shown for selected countries with available data in Table 3.
Table 3.
Age-standardised IHD mortality for selected countries between 2000 and 2009. Data directly standardised to WHO world standard population.
| Standardised mortality rates from ischaemic heart disease (per 100,000 population) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | |
| Australia | 21.7 | 20.4 | 18.9 | 17.7 | 16.6 | 13.5 | ||||
| Austria | 23.7 | 21.8 | 19.9 | 19.4 | 18.8 | 18.5 | 17.1 | 17.3 | ||
| Bulgaria | 34.3 | 31.8 | 29.1 | 27.0 | ||||||
| Canada | 22.9 | 21.3 | 20.0 | 19.5 | 18.1 | |||||
| Croatia | 39.1 | 33.4 | 31.8 | 36.1 | 31.5 | 32.8 | 31.3 | 29.5 | 29.8 | 30.4 |
| Cyprus | 16.7 | 17.6 | 15.9 | 18.5 | 15.7 | |||||
| Czech Republic | 39.7 | 38.0 | 36.4 | 35.1 | 32.7 | 33.9 | 31.9 | 34.7 | 32.5 | 31.4 |
| Denmark | 21.8 | 21.7 | 18.8 | 17.5 | 16.2 | 14.7 | 13.5 | |||
| Egypt | 14.9 | 17.3 | 22.6 | 23.4 | 20.1 | |||||
| Estonia | 67.8 | 66.3 | 63.1 | 59.9 | 55.1 | 50.4 | 48.8 | 46.1 | 42.0 | |
| Finland | 35.1 | 32.3 | 31.4 | 29.8 | 27.8 | 26.2 | 25.5 | 24.6 | 23.3 | 22.4 |
| France | 9.9 | 9.4 | 8.9 | 8.6 | 8.0 | 7.7 | 7.1 | 6.8 | ||
| Germany | 25.0 | 23.7 | 22.9 | 22.3 | 20.7 | 19.4 | 18.4 | |||
| Hong Kong | 9.6 | 9.7 | 10.3 | 10.4 | 10.0 | 9.2 | 10.1 | 9.8 | 9.3 | |
| Hungary | 49.1 | 46.1 | 45.0 | 46.8 | 46.9 | 52.4 | 48.7 | 46.0 | 43.8 | 43.6 |
| Iceland | 23.1 | 21.2 | 22.3 | 19.3 | 21.6 | 17.5 | 16.2 | 16.8 | 16.4 | |
| Israel | 18.8 | 16.8 | 15.3 | 15.0 | 12.9 | 12.4 | 12.2 | 12.5 | ||
| Japan | 7.1 | 7.0 | 6.8 | 6.7 | 6.3 | 6.5 | 6.2 | 6.0 | 5.9 | 5.7 |
| Kuwait | 26.4 | 27.9 | 27.0 | 25.3 | 25.2 | 30.2 | ||||
| Kyrgyzstan | 71.8 | 69.4 | 78.6 | 81.8 | 77.5 | 84.1 | 90.2 | 88.4 | 90.0 | 91.5 |
| Latvia | 65.6 | 64.9 | 62.3 | 60.7 | 61.0 | 61.3 | 60.4 | 62.3 | 56.1 | 54.5 |
| Lithuania | 57.4 | 62.8 | 62.3 | 62.6 | 61.7 | 64.9 | 64.0 | 62.5 | 58.9 | 56.1 |
| Luxembourg | 18.3 | 16.4 | 15.9 | 18.7 | 16.1 | 13.3 | 15.4 | 13.1 | 12.1 | |
| Malta | 35.4 | 33.9 | 30.8 | 30.9 | 26.5 | 30.2 | 27.9 | 24.0 | 24.7 | |
| Netherlands | 18.9 | 17.2 | 16.2 | 15.4 | 13.5 | 12.6 | 11.3 | 10.3 | 9.6 | 8.9 |
| New Zealand | 27.5 | 27.7 | 26.1 | 24.2 | 23.8 | 20.8 | 20.1 | 19.1 | ||
| Norway | 23.4 | 22.1 | 20.9 | 18.7 | 17.0 | 15.0 | 14.1 | 13.6 | 12.9 | 12.2 |
| Poland | 31.3 | 29.4 | 27.2 | 26.6 | 25.2 | 24.1 | 23.5 | 22.4 | 21.5 | |
| Romania | 47.8 | 47.3 | 48.3 | 46.6 | 44.5 | 44.0 | 42.8 | 40.6 | 39.3 | 37.9 |
| Serbia | 28.7 | 28.0 | 28.7 | 28.7 | 28.1 | 31.4 | 30.4 | 27.9 | 27.3 | 26.5 |
| Slovakia | 59.0 | 53.9 | 52.4 | 53.2 | 52.5 | 50.8 | ||||
| Slovenia | 20.8 | 20.0 | 17.6 | 18.3 | 16.5 | 16.0 | 14.0 | 13.9 | 14.4 | 13.3 |
| Spain | 13.7 | 13.1 | 12.7 | 12.5 | 11.7 | 11.5 | 10.6 | 10.1 | 9.5 | |
| Sweden | 24.5 | 23.5 | 22.7 | 21.7 | 19.9 | 18.9 | 18.2 | 17.2 | 16.5 | |
| United Kingdom | 29.3 | 27.7 | 26.2 | 24.0 | 22.4 | 20.6 | 19.4 | 18.2 | 16.7 | |
| USA | 29.7 | 28.2 | 27.2 | 25.9 | 24.0 | 23.1 | ||||
Age-standardisation is essential when comparing countries, as shown in Fig. 5a and b which contrast the crude and age-standardised mortality trends amongst the same set of countries. A decrease in age-standardised mortality rates is seen in most countries in Western Europe, but countries in Eastern Europe have a flat pattern (Croatia, Serbia, Slovakia, Hungary and Czech Republic) and an increasing trend can be seen in some Central Asian countries (e.g. Kyrgyzstan).
Fig. 5.
(a). Changes in crude annual mortality rates from ischaemic heart disease for selected Countries between 2000 and 2009. (b). Changes in directly standardised annual mortality rates from ischaemic heart disease for selected Countries between 2000 and 2009.
In the majority of countries for which age-specific data are available, there has been a steady decline in IHD death rates between 2000 and 2009. These data tend to be for high income countries. Reporting of time trends in IHD mortality is limited for most low-and-middle income countries.
3.5. Extended analysis across 177 countries: standardised mortality ratios
In order to compare a more comprehensive set of low, middle and high income countries that do not have complete age-specific IHD death data, we use indirectly standardised IHD mortality ratios presented in Table 4. Countries are ranked by their 2008 IHD mortality ratio. The spectrum is wide, with some countries such as Turkmenistan, Afghanistan and Ukraine having a mortality ratio that is approximately 20-fold that of other countries such as Japan.
Table 4.
Indirectly standardised mortality ratios (SMR)a for IHD for all WHO member states ranked by country SMR in 2008.
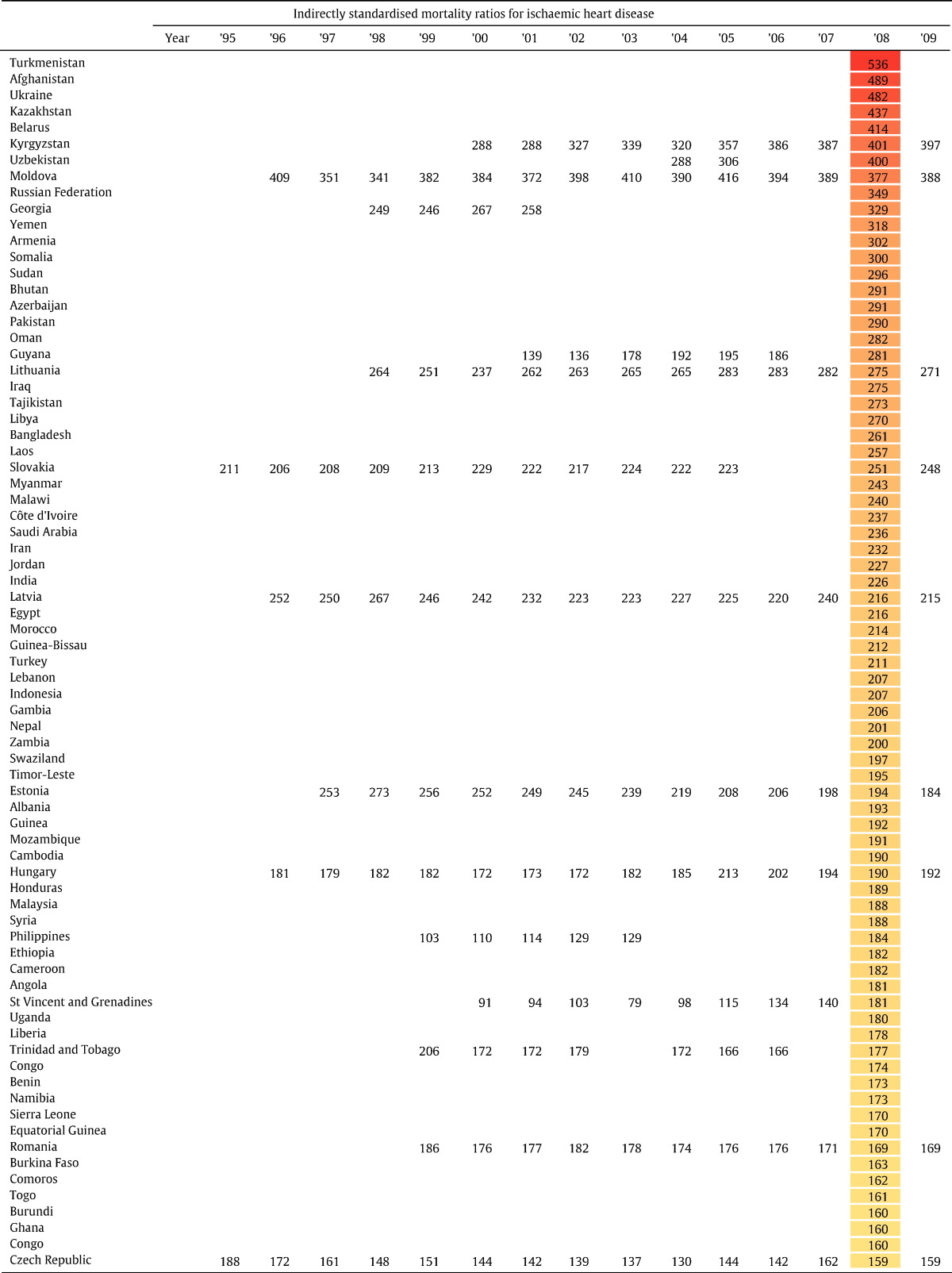
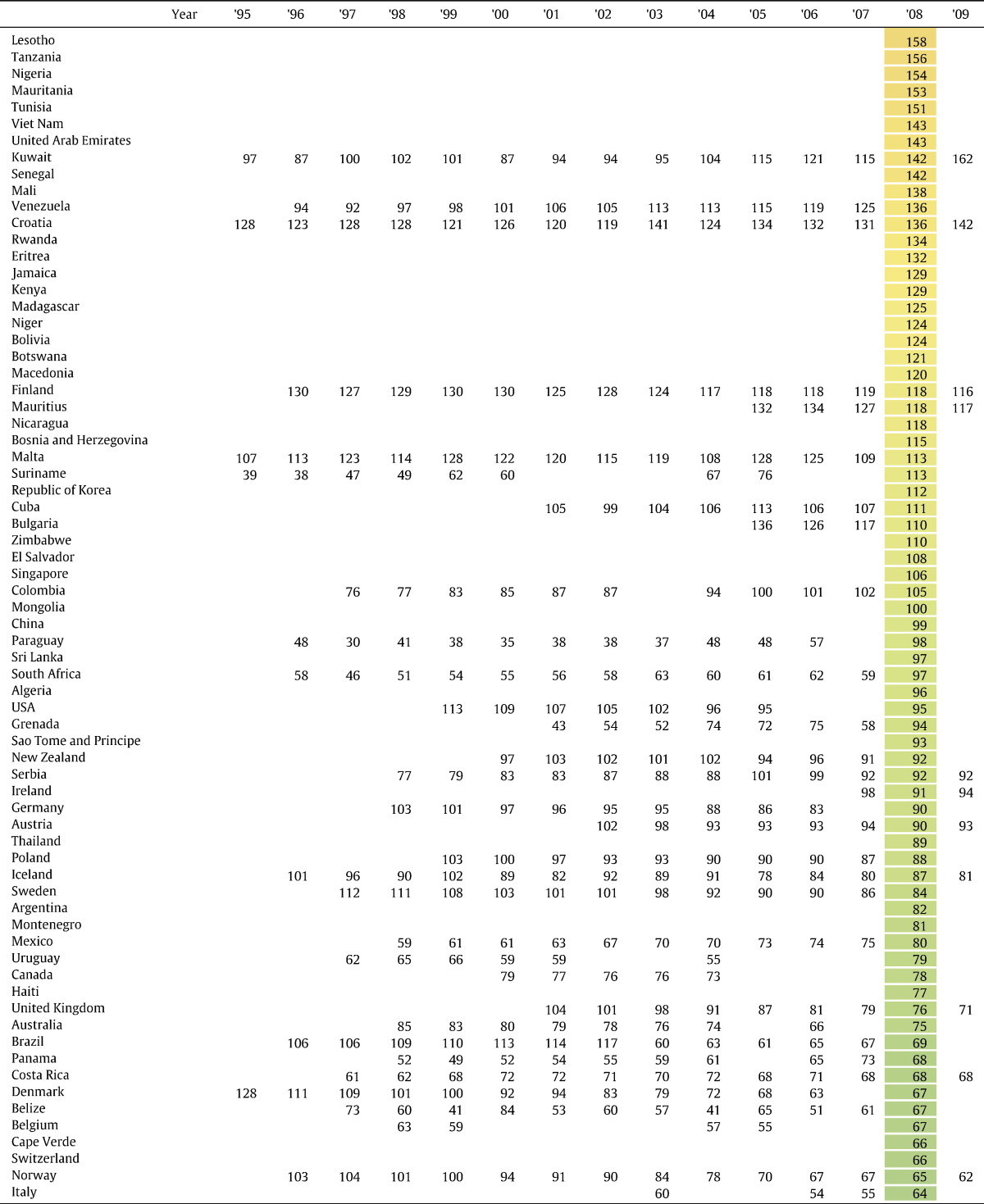
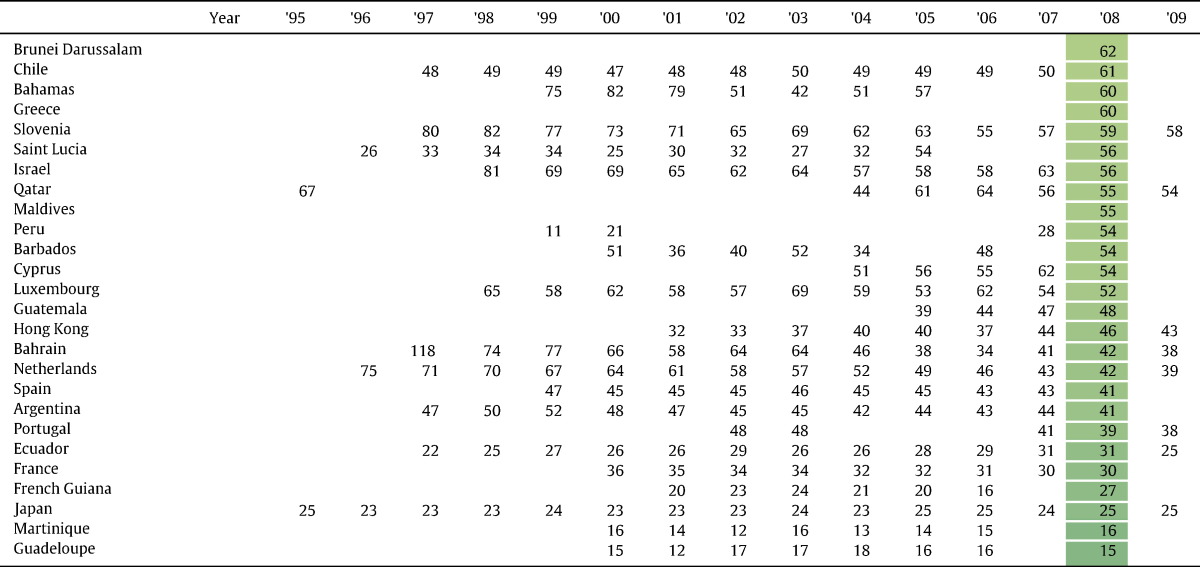
Standard population is defined as the average age-specific mortality rates of the UK, USA, Canada, France and Germany in 2001.
4. Discussion
IHD has been, and continues to be, the single largest cause of death in the world. This is because the majority of the world's population lives in low-and-middle income countries, where IHD mortality rates are often flat or increasing, and total populations are growing.
Overall, age-standardised mortality has fallen significantly in many high income countries since the early 1980s [19]. However, the age effect on IHD mortality is so strong that high income countries, which have older and ageing populations, have a total mortality burden which remains high and is falling only slowly over time.
The larger populations and higher age-specific death rates for IHD in low-and-middle income countries mean that they already account for the majority of global IHD deaths and will bear the brunt of the IHD epidemic in the years to come. Moreover the combined effect of population growth and ageing is so strong that despite all current efforts, total numbers of IHD deaths worldwide are increasing.
Of the many factors that contribute to the favourable trend in IHD mortality in high income countries, three may be particularly important [20]. Firstly, policy changes may favour risk factor modification, such as decreased exposure to tobacco smoke [21] and improvement in primary prevention strategies [22,23] (e.g. hypertension control [24–26]). Second, rapid response times and improved treatments (such as thrombolysis and primary angioplasty) for acute IHD events may lead to reduced IHD case-fatality [27]. Third, secondary prevention, which may further reduce mortality, is making more headway in implementation in wealthier countries [28].
The contribution of these factors to the decreasing mortality rates from IHD is complex. The WHO MONICA (MONitoring trends and determinants In CArdiovascular disease) study [29,30] reported that between the mid-1980s and 1990s, on average two thirds of the decline in mortality from IHD could be attributed to a decline in coronary event rates and one third to decreasing case-fatality. A more recent study by Smolina et al. [31] during the 2000s in England reported just over half of the decline in IHD mortality could be attributed to a decline in event rates and just less than half to improved survival at thirty days.
The increasing mortality in some countries in Eastern Europe is likely to reflect a combination of continued high exposure to cardiovascular risk factors (including tobacco smoke [32]) and inadequate prevention strategies e.g. poor control of hypertension [33,34]. In addition, evidence suggests a positive association between excess alcohol consumption in Eastern European countries and increased mortality from cardiovascular disease [35]. Unfortunately, data are sparse for many areas of the world e.g. Latin America, Africa that are likely to be incurring continued unfavourable trends in IHD mortality due to rapid urbanisation and the shifting focus of tobacco companies and processed food and drinks manufacturers to low-and-middle income regions [36]. Rapid urbanisation has been positively associated with risk factors related to IHD [37] e.g. smoking, high BMI, poor blood pressure control and lower physical activity. Without accurate baseline mortality data it will be difficult to target prevention strategies for the future.
5. Limitations
A major limitation to our analysis of world-wide IHD trends is the paucity of data from certain geographical areas such as Latin America and Africa. The majority of data currently reported to the WHO is from high income countries with poor representation from low-and-middle income countries.
Despite the existence of the WHO ICD coding system which tries to standardise cause of death coding, there may still be differences in reporting patterns between countries, for example in the handling of deaths where multiple causes may have contributed, or where background medical information is scarce. In addition the validity of the ICD code assigned may vary from place to place. This may lead to either over or under-reporting of death due to ischaemic heart disease. In addition, the uncertainty around cause of death coding may be exaggerated in low-and-middle income countries, as some large countries such as India and China have not implemented fully comprehensive death registration systems but rely on sample surveillance for vital statistics [38,39].
Although low-and-middle income countries will struggle more than high income countries to find resources to target IHD prevention, it is in these countries that the impact could be greatest as they have the highest age-specific death rates in younger people. IHD contributes substantially to premature mortality in these populations, and reducing IHD mortality will increase the lifespan of working-age populations, and may therefore have an important effect on economic growth [40]. Not all preventative strategies will be prohibitively expensive. For example generic aspirin and statins are available cheaply, and government initiatives to reduce smoking need not be financially demanding [41]. While we acknowledge that many low-and-middle income countries may have competing healthcare priorities, this paper highlights the burden of IHD, and the critical need to target preventative and treatment interventions for IHD in these areas. It is particularly important that we do not hastily assume intervention in these countries would be futile, since they now bear the majority of the global burden of IHD deaths [42,43]. The impact of prevention and treatment strategies has been projected for non-communicable diseases in low-and-middle income countries and can potentially reduce age standardised death rates by 2% per year [44].
6. Conclusion
This paper illustrates mortality trends from IHD between 1995 and 2009 derived from WHO international data. IHD mortality rises sharply with age and IHD thus remains the leading cause of death even in high income countries where age-standardised death rates have fallen by as much as 50% in the last 25 years, as their populations age. In addition, premature mortality (at age < 60 years) from IHD is far from trivial, and age-specific death rates in the working age population are much higher in low-and-middle income countries than high income countries. This, combined with the large number of persons at risk in this age group in low-and-middle income countries, makes IHD a particular challenge for these countries.
Rising trends in IHD mortality are not inevitable as the declining age-standardised mortality rates in many high income countries demonstrate. Reliable information is the first step to successful initiatives to tackle this potentially tractable but currently uncontrolled epidemic. The opportunities are great because — unlike many other causes of death — the susceptibility of IHD to prevention and treatment is exquisite.
Footnotes
Funding sources and disclosures: DPF (FS/010/083) was supported by the British Heart Foundation. PA is supported by a Wellcome Trust Clinical PhD Fellowship 092853/Z/10/Z.
References
- 1.http://www.who.int/whosis/whostat/2008/en/index.html
- 2.Xu J.Q., Kochanek K.D., Murphy S.L., Tejada-Vera B. vol. 58 no. 19. National Center for Health Statistics; Hyattsville, MD: 2010. Deaths: final data for 2007. (National vital statistics reports). [PubMed] [Google Scholar]
- 3.Scarborough P., Wickramasinghe K., Bhatnagar P., Rayner M. British Heart Foundation; London: 2011. Trends in coronary heart disease 1961–2011. [Google Scholar]
- 4.Rosamond W., Flegal K., Furie K. Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117(4):e25–e146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 5.Scarborough P., Bhatnagar P., Wickramasinghe K., Smolina K., Mitchell C., Rayner M. British Heart Foundation; 2010. Coronary heart disease statistics. [Google Scholar]
- 6.Allender S., Scarborough P., Peto V. European Heart Network; Brussels: 2008. European cardiovascular disease statistics 2008. [Google Scholar]
- 7.Uemura K., Pisa Z. Trends in cardiovascular disease mortality in industrialized countries since 1950. World Health Stat Q. 1988;41:155–178. [PubMed] [Google Scholar]
- 8.Ragland K.E., Selvin S., Merrill D.W. The onset of decline in ischemic heart disease mortality in the United States. Am J Epidemiol. 1988;127:516–531. doi: 10.1093/oxfordjournals.aje.a114827. [DOI] [PubMed] [Google Scholar]
- 9.Tunstall-Pedoe H., Kuulasmaa K., Mähönen M., Tolonen H., Ruokokoski E., Amouyel P. Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet. 1999;353(9164):1547–1557. doi: 10.1016/s0140-6736(99)04021-0. [DOI] [PubMed] [Google Scholar]
- 10.Rodríguez T., Malvezzi M., Chatenoud L. Trends in mortality from coronary heart and cerebrovascular diseases in the Americas: 1970–2000. Heart. 2006;92(4):453–460. doi: 10.1136/hrt.2004.059295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levi F., Chatenoud L., Bertuccio P., Lucchini F., Negri E., La Vecchia C. Mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world: an update. Eur J Cardiovasc Prev Rehabil. 2009;16(3):333–350. doi: 10.1097/HJR.0b013e328325d67d. [DOI] [PubMed] [Google Scholar]
- 12.Roger V.L. Epidemiology of myocardial infarction. Med Clin North Am. 2007;91(4):537–552. doi: 10.1016/j.mcna.2007.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organisation statistical Information System WHO mortality database. http://www.who.int/healthinfo/statistics/mortality
- 14.http://www.who.int/evidence/bod
- 15.Lopez A.D., Mathers C.D., Ezzati M., Jamison D.T., Murray C. The burden of disease and mortality by condition: data, methods, and results for 2001. 2001. Global burden of disease and risk factors. Chapter 3. [PubMed] [Google Scholar]
- 16.World Health Organisation . World Health Organisation; 1992. International statistical classification of disease and related health problems. 10th revision. [Google Scholar]
- 17.http://esa.un.org/unpd/wpp/Excel-Data/population.htm
- 18.Ahmad O.B., Boschi-Pinto C., Lopez A.D., Murray C., Lozano R., Inoue M. World Health Organization; 2001. Age standardisation of rates: a new WHO standard. (GPE discussion paper series: no.31EIP/GPE/EBD). [Google Scholar]
- 19.Levi F., Lucchini F., Negri E., La Vecchia C. Trends in mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world. Heart. 2002;88(2):119–124. doi: 10.1136/heart.88.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goldman L. The decline in coronary heart disease: determining the paternity of success. Am J Med. 2004;117:274–276. doi: 10.1016/j.amjmed.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Yusuf S., Hawken S., Ounpuu S. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case–control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 22.Ezzati M., Hoorn S.V., Rodgers A. Estimates of global and regional potential health gains from reducing multiple major risk factors. Lancet. 2003;362(9380):271–280. doi: 10.1016/s0140-6736(03)13968-2. [DOI] [PubMed] [Google Scholar]
- 23.Kuulasmaa K., Tunstall-Pedoe H., Dobson A. Estimation of contribution of changes in classic risk factors to trends in coronary event rates across the WHO MONICA project populations. Lancet. 2000;355:675–687. doi: 10.1016/s0140-6736(99)11180-2. [DOI] [PubMed] [Google Scholar]
- 24.WHO Monica project Ecological analysis of the association between mortality and major risk factors of cardiovascular disease. Int J Epidemiol. 1994;23:505–516. doi: 10.1093/ije/23.3.505. [DOI] [PubMed] [Google Scholar]
- 25.MacMahon S., Peto R., Cutler J. Blood pressure, stroke, and coronary heart disease. Part 1. Prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet. 1990;335:765–774. doi: 10.1016/0140-6736(90)90878-9. [DOI] [PubMed] [Google Scholar]
- 26.Collins R., Peto R., MacMahon S. Blood pressure, stroke, and coronary heart disease. Part 2. Short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological context. Lancet. 1990;335:827–838. doi: 10.1016/0140-6736(90)90944-z. [DOI] [PubMed] [Google Scholar]
- 27.Tunstall-Pedoe H., Vanuzzo D., Hobbs M. Estimation of contribution of changes in coronary care to improving survival, event rates, and coronary heart disease mortality across the WHO MONICA project populations. Lancet. 2000;355:688–700. doi: 10.1016/s0140-6736(99)11181-4. [DOI] [PubMed] [Google Scholar]
- 28.Yusuf S., Islam S., Chow C.K. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet. 2011;378(9798):1231–1243. doi: 10.1016/S0140-6736(11)61215-4. [DOI] [PubMed] [Google Scholar]
- 29.Tunstall-Pedoe H for the WHO MONICA Project . WHO; 2003. MONICA monograph and multimedia sourcebook: world's largest study of heart disease, stroke, risk factors, and population trends 1979–2002. [ http://whqlibdoc.who.int/publications/2003/9241562234] [Google Scholar]
- 30.Rosamond W.D., Chambless L.E., Folsom A.R. Trends in the incidence of myocardial infarction and in mortality due to coronary heart disease, 1987 to 1994. N Engl J Med. 1998;339:861–867. doi: 10.1056/NEJM199809243391301. [DOI] [PubMed] [Google Scholar]
- 31.Smolina K., Wright F.L., Rayner M., Goldacre M.J. Determinants of the decline in mortality from acute myocardial infarction in England between 2002 and 2010: linked national database study. BMJ. 2012;344:d8059. doi: 10.1136/bmj.d8059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roberts B., Gilmore A., Stickley A. Changes in smoking prevalence in 8 countries of the former Soviet Union between 2001 and 2010. Am J Public Health. 2012;102(7):1320–1328. doi: 10.2105/AJPH.2011.300547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roberts B., Stickley A., Balabanova D., Haerpfer C., McKee M. The persistence of irregular treatment of hypertension in the former Soviet Union. J Epidemiol Community Health. 2012;66(11):1079–1082. doi: 10.1136/jech-2011-200645. [DOI] [PubMed] [Google Scholar]
- 34.Kotseva K., Wood D., De Backer G. Cardiovascular prevention guidelines in daily practice: a comparison of EUROASPIRE I, II, and III surveys in eight European countries. Lancet. Mar 14, 2009;373(9667):929–940. doi: 10.1016/S0140-6736(09)60330-5. [DOI] [PubMed] [Google Scholar]
- 35.Ramstedt M. Fluctuations in male ischaemic heart disease mortality in Russia 1959–1998: assessing the importance of alcohol. Drug Alcohol Rev. 2009;28(4):390–395. doi: 10.1111/j.1465-3362.2009.00059.x. [DOI] [PubMed] [Google Scholar]
- 36.Stuckler D., McKee M., Ebrahim S., Basu S. Manufacturing epidemics: the role of global producers in increased consumption of unhealthy commodities including processed foods, alcohol, and tobacco. PLoS Med. 2012;9(6):e1001235. doi: 10.1371/journal.pmed.1001235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.http://www.who.int/bulletin/volumes/88/4/09-065847/en/index.html
- 38.http://unstats.un.org/unsd/vitalstatkb/KnowledgebaseArticle50391.aspx
- 39.http://unstats.un.org/unsd/vitalstatkb/Attachment476.aspx
- 40.Abegunde D.O., Mathers C.D., Adam T., Ortegon M., Strong K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370(9603):1929–1938. doi: 10.1016/S0140-6736(07)61696-1. [DOI] [PubMed] [Google Scholar]
- 41.Beaglehole R., Bonita R., Horton R. Priority actions for the non-communicable disease crisis. Lancet. 2011;377(9775):1438–1447. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]
- 42.Lim S.S., Gaziano T.A., Gakidou E. Prevention of cardiovascular disease in high-risk individuals in low-income and middle-income countries: health effects and costs. Lancet. 2007;370(9604):2054–2062. doi: 10.1016/S0140-6736(07)61699-7. [DOI] [PubMed] [Google Scholar]
- 43.Asaria P., Chisholm D., Mathers C., Ezzati M., Beaglehole R. Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet. 2007;370(9604):2044–2053. doi: 10.1016/S0140-6736(07)61698-5. [DOI] [PubMed] [Google Scholar]
- 44.Strong K., Mathers C., Leeder S., Beaglehole R. Preventing chronic diseases: how many lives can we save? Lancet. 2005;366(9496):1578–1582. doi: 10.1016/S0140-6736(05)67341-2. [DOI] [PubMed] [Google Scholar]