Abstract
Objectives
The knee can be injected at different anatomic sites with or without image-guidance. We undertook a systematic review to determine the accuracy of intra-articular knee injection (IAKI) and whether this varied by site, use of image-guidance, and experience of injectors, and whether accuracy of injection, site, or use of image-guidance influenced outcomes following IAKIs.
Methods
Medline, Embase, AMED, CINAHL, Web of Knowledge, Cochrane Central Registers for Controlled Trials up to Dec 2012 were searched for studies that evaluated either accuracy of IAKIs or outcomes related to accuracy, knee injection sites, or use of image-guidance. Within-study and between-study analyses were performed.
Results
Data from 23 publications were included. Within-study analyses suggested IAKIs at the superomedial patellar, medial midpatellar (MMP), superolateral patellar (SLP) and lateral suprapatellar bursae sites were more accurate when using image-guidance than when blinded (ranges of pooled risk difference 0.09–0.19). Pooling data across studies suggested blinded IAKIs at the SLP site were most accurate (87%) while MMP (64%) and anterolateral joint line (ALJL) sites were (70%) least accurate. Overall about one in five blinded IAKIs were inaccurate. There was some evidence that experience of the injector was linked with improved accuracy for blinded though not image-guided injections. Based on a small number of studies, short but not longer-term outcomes for ultrasound-guided were found to be superior to blinded IAKIs.
Conclusions
Image-guided IAKIs are modestly more accurate than blinded IAKIs especially at the MMP and ALJL sites. Blinded injections at SLP site had good accuracy especially if performed by experienced injectors. Further studies are required to address the question whether accurate localization is linked with an improved response.
Keywords: Osteoarthritis of the knee, Clinical trials, Injection, Aspiration, Accuracy, Systematic review
Introduction
The knee is one of the commonest target joints for intra-articular injection therapy [1–4]. There are a number of possible anatomic injection sites [5–7]. Clinicians' choice of technique is often influenced by their experience and training.
It seems likely that increased accuracy of localization of the injection within the joint should improve treatment response. However, unlike shoulder injections where there is established evidence for using image-guided injections [1,8–12], the evidence base for needle-guidance during intra-articular knee injections (IAKI) is weaker. It remains uncertain whether approaches for localization such as using air arthrogram [13,14], fluoroscopy [15], ultrasound [16,17], and magnetic resonance imaging (MRI) [18] actually improve IAKI accuracy. Also it remains unclear whether improved accuracy is associated with better clinical response.
We undertook a systematic review with the aim of determining—(i) the accuracy of IAKI and whether this varied by site, imaging, and experience of injectors and, (ii) whether accuracy, site of injection, or the use of image-guidance were linked with therapeutic response. We also undertook a meta-analysis of the accuracy of “blinded” (without image-guidance) vs guided IAKI (with image-guidance).
Methods
Search strategies
Publications that looked at accuracy of IAKIs or clinical outcome associated with intra-articular needle placement, delivered blinded or guided, or at varying knee injection sites were identified from searching six databases up to Dec 2012: Medline (1948 onwards), Embase (1974 onwards), AMED (1985 onwards), Cumulative Index to Nursing and Allied Health Literature (CINAHL) Plus (1937 onwards), Web of Science (1950 onwards), and the Cochrane Central Registers for Controlled Trials. The databases were searched individually for all possible terms and combination of terms to accommodate differences in their search engines. All medical subject-heading searches (MeSH) were explored when possible. The key terms used in combination (“AND”) were knee, intra-articular, injection, aspiration, trials, and accuracy.
Study selection criteria
In this review, injection “sites” refer to specific areas in the knee for needle entry and injection “approaches” refer to techniques of delivering the injections or aspirations including angling of the needle or position of the knee, flexed or extended. Guided IAKIs included any needle-guidance techniques to assist getting into the joint such as injections or aspirations aided by ultrasound, fluoroscopy, or air-arthrography. For assessing accuracy of IAKI, we included studies that used participants with knee osteoarthritis (OA), inflammatory arthritis, mixed samples of OA and inflammatory arthritis, those without knee pathologies, and cadavers. For formal comparison of blinded and guided IAKI, we included studies that used at least two treatments arms; one delivering blinded injection at a particular site and another using guided injection at the same site, allowing within-study comparison. We found that most studies provided information about one treatment arm only. To maximize utilization of the available data, we therefore included a between-study comparison of the various injection sites pooling the accuracy of blinded and guided IAKIs separately. There were too few data to look at outcome in relation to accuracy and knee injection sites; however, we were able to pool data in relation to the influence of image-guidance on outcome. Outcome measures relating to treatment response were not specified a priori.
Knee joint injection accuracy
Accurate IAKI occurs when the needle is placed within the intra-capsular joint space and inaccurate injection when the needle is placed extra-articularly or gets embedded into other intra-capsular tissues such as plica. To determine the accuracy of IAKI, a number of approaches are available such as injection of contrast or air with radiography [13,14], sonography [19] or fluoroscopy [20], magnetic resonance imaging (MRI) [18], surgical confirmation of intra- or extra-articular placement of drugs [21,22], and for aspiration successful removal of synovial fluid. There is no gold standard for assessing accuracy of IAKI. It is recognized that all these techniques are subject to a degree of observer error in evaluation of the images while surgical confirmation is too invasive for routine use. In this review, we included all studies that made an independent attempt to corroborate intra-articular placement including successful aspiration of synovial fluid. For this review, the results on accuracy of the sites of injection were tabulated by injection site and also whether image-guidance was used or not. We did not look separately at accuracy by method of image-guidance.
Quality assessment
For randomized controlled trials (RCTs), study quality was graded using the Jadad score [23]. Concealment to treatment allocation was scored as adequate, inadequate, or unclear if there was insufficient information to make the judgment [24]. For observational studies, “Strengthening the Reporting of Observational Studies in Epidemiology” (STROBE) checklist of 22 items was used to assess quality [25] with close reference to further elaboration and explanation of the criteria given in another publication of the STROBE statement [26]. For non-RCT, quality was assessed using the “Transparent Reporting of Evaluations with Non-randomized Designs” (TREND) checklist [27]. The data were extracted independently by two reviewers (N.M. and M.J.P.). Two assessors (N.M. and M.J.C.) independently assessed and scored the publications for quality and reached consensus in cases of disagreement.
Data extraction and analyses
A fixed-effects meta-analysis was used to pool those studies that evaluated a specific injection site under both blinded and guided conditions within the same trial (within-study analyses). Heterogeneity in trial outcomes was assessed using the I2 statistic. Results of other studies evaluating accuracy of specific injection sites were also pooled (between-study analyses). Accuracy was assessed as the percentage of those injected in which the injection was correctly localized. For within-study comparisons, difference in accuracy (guided vs blinded) was assessed using absolute risk difference (ARD) with associated 95% confidence intervals (CI), where the risk ratio is the “risk” of an accurate injection in the guided group to the “risk” of an accurate injection in the blinded group. For between-study comparisons, difference in accuracy between groups was assessed also using the chi-square statistic and relative risk (RR). We used a fixed-effects meta-analysis to pool data looking at outcomes in relation to use of image-guidance (ultrasound). Results were considered significant if p-values were less than 0.05 (two sided) or if the 95% CI of the RR and ARD did not include one and zero, respectively.
Results
Search outcome
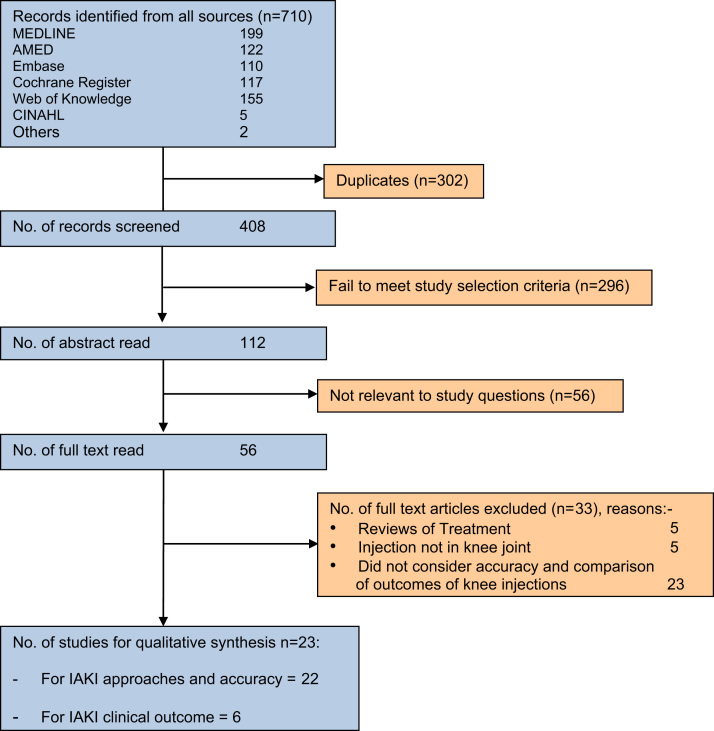
From all databases, 710 publication records were retrieved and 302 duplicates eliminated (Fig. 1). Text-words from 408 records were screened, and of these, 296 records failed to meet study selection criteria. Of the 112 abstracts read, 56 were not relevant and were excluded. A further 56 full-text articles were read for eligibility. Of these 33 were rejected for not evaluating accuracy of IAKI sites, blinded or guided IAKIs, or clinical outcome associated with intra-articular needle placement. Twenty-three publications finally met the inclusion criteria (Fig. 1); some of these addressed accuracy only, others both accuracy and treatment outcome (Table 1).
Fig. 1.
Summary of search results.
Table 1.
Published papers
| Authors | Phenotype | Intervention | Method for assessing accuracy | Assessment |
| Balint et al. [34] | Knee OA and RA | Aspiration of synovial fluid | Successful aspiration | Accuracy: blinded (unknown site) vs ultrasound-guided (via LSB) |
| Bliddal [13] | Knee OA | Steroid/local anesthetic/air | Air on XR | Accuracy and outcome: blinded vs air-arthrography guided via SLP |
| Bum Park et al. [35] | Knee OA | Hyaluronic acid | XR + contrast | Accuracy: blinded vs ultrasound-guided via LSB |
| Chavez-Chiang et al. [28] | Knee OA | Steroid/local anesthetic | Ultrasound | Treatment outcome: blinded injection via LMP and LJL (knee extended)Accuracy: ultrasound-guided via LJL (knee flexed) |
| Cunnington et al. [2] | Inflammatory arthritis | Aspiration of synovial fluid | XR + contrast | Accuracy and outcome: blinded vs ultrasound-guided |
| Curtiss et al. [36] | Cadaveric knees | Methylene blue | Dissection | Accuracy: blinded (SLP) vs ultrasound-guided (LSB) |
| Esenyel et al. [21] | Cadaveric knees | Methylene blue | Dissection | Accuracy: blinded injection via MJL, MMP, LJL, and LMP |
| Glattes et al. [14] | Knees needing injection | Local anesthetic | XR + contrast “Squishing sound” test | Accuracy: blinded injection via SLP |
| Im et al. [37] | Knee OA | Hyaluronic acid | XR + contrast | Accuracy: blinded vs ultrasound-guided via MMP |
| Jackson et al. [15] | Knee OA | Hyaluronic acid | Fluoroscopy | Accuracy: blinded injection via AM, AL, and LMP |
| Jones et al. [4] | Knee OA and RA | Steroid | XR + contrast | Accuracy and outcome: blinded injection |
| Lopes et al. [31] | Inflammatory arthritis | Steroid | XR + contrast | Accuracy and outcome: blinded injection |
| Luc et al. [32] | Knee OA | Local anesthetic | XR + contrast “Backflow of fluid” test | Accuracy: blinded injection via SLP |
| Myung et al. [38] | Knee OA | Hyaluronic acid | Fluoroscopy | Accuracy: blinded vs fluoroscopy-guided via SMP |
| Park et al. [39] | Knee OA | Steroid/local | XR + contrast | Accuracy: ultrasound-guided via MMP, LMP, and SLP |
| Qvistgaard et al. [19] | Knee OA | Hyaluronic acid/local anesthetic/air | Air on ultrasound image | Accuracy: ultrasound-guided via SLP |
| Shah and Wright [33]a | Knee OA | Steroid | Dissection | Outcome: blinded M vs IFP injection |
| Shah and Wright [33]b | Cadaveric knees | Methylene blue | Accuracy: blinded injection via IFP | |
| Sibbitt et al. [40] | Knee OA and RA | Aspiration of synovial fluid | Successful aspiration | Accuracy and outcome: blinded vs ultrasound-guided aspiration via LSB |
| Sibbitt Jr et al. [41] | Knee OA | Steroid/local anesthetic | – | Outcome: blinded vs ultrasound-guided via AMJL |
| Toda and Tsukimura [29] | Knee OA | Hyaluronic acid | XR + contrast | Accuracy and outcome: blinded injection via MJL (flexed 30◦), MJL (flexed 90◦), and LMP |
| Waddell et al. [20] | Non-arthritic kneesc | Methylene blue | XR + contrast | Accuracy: fluoroscopy-guided via ALJL |
| Wiler et al. [30] | Effused knees | Aspiration of synovial fluid | Successful aspiration | Accuracy and outcome: blinded vs ultrasound-guided |
| Wind and Smolinski [22] | Knees undergoing arthroscopy | Hyaluronic acid/methylene blue | Arthroscopy | Accuracy: blinded injection via SMP, SLP, and LJL |
Abbreviations: OA, osteoarthritis; RA, rheumatoid arthritis; M, medial; L, lateral; MP, medial patellar; IFP, infrapatellar; AM, anteromedial; AL, anterolateral; MMP, medial midpatellar; SMP, superomedial patellar; MJL, medial joint line; LMP, lateral midpatellar; SLP, superolateral patellar; LJL, lateral joint line; LSB, lateral suprapatellar bursa.
Trial comparing outcomes of knee injections delivered at two sites in 36 patients.
Trial to determine infrapatellar injection accuracy using four OA cadaveric knees.
Six of the 11 participants had a history of knee complaints. Shaded row: within-study analyses.
Twelve of 23 studies were RCTs, three non-RCTs, and eight observational studies. Twenty-two publications addressed accuracy of IAKIs and/or aspiration, seven assessed accuracy of IAKIs at different sites [14,15,21,22,28–30], four at one injection site [20,31–33], and 13 compared blinded and guided IAKIs [2,13,19,20,28,30,34–40]. Of the six studies that reviewed clinical outcomes, one was pertaining to accuracy of IAKI [29], two compared between different knee injection sites [28,33], and three compared outcomes between guided and blinded IAKIs [40,41] (Table 1). In two papers, the injection site was not specified during blinded IAKIs [2,4]. There were also two studies that investigated knee injections performed at the same site but using different approaches depending on the angling of the needle or the position of the knee, flexed or extended [28,29]; though in one of these studies, the accuracy relating to each approach was not formally assessed [28]. In three papers [14,20,30] the authors were contacted to provide clarity relating to accuracy and injection sites. The required information was obtained for one of the studies [20]; in the others [14,30], site of knee injections was designated as unknown.
Data quality
For the 12 RCTs, only five had Jadad scores of three and above [2,29,35–37] and were deemed as high-quality trials [42] and five had adequate allocation concealment [2,29,35,36,39] (see Supplementary Tables S1–S3). Others were single-blinded trials where either patients or injectors were not blinded to the intervention groups. For the observational studies, seven of eight studies fulfilled 10–18 of the 22 STROBE criteria [4,13,19,21,31,32,38], while all three non-randomized trials had TREND scores of 10–15 of 22 [14,15,34] (see Supplementary Tables S1–S3).
Knee joint injection sites and approaches
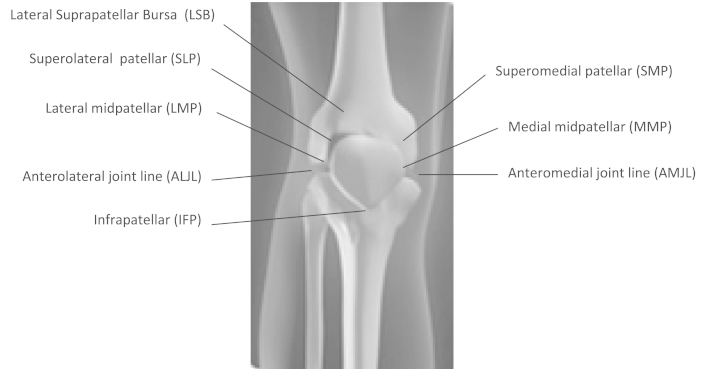
Publications included in this review sometimes used different terms to describe the sites of injections, but by using the enclosed descriptions of how the injections were performed including diagrams or pictures, we were able to identify eight different injection sites. These included medial injection techniques such as over the anteromedial joint line (AMJL), medial midpatellar (MMP), and superomedial patellar (SMP) and lateral injection techniques over the anterolateral joint line (ALJL), lateral midpatellar (LMP), superolateral patellar (SLP), lateral suprapatellar bursa (LSB), and also infrapatellar (IFP) (Fig. 2). In five publications sites were classified as “unknown.” Infrapatellar site was used least and evaluated in one publication only.
Fig. 2.
Injection sites in knee.
Thirteen approaches at eight sites were described during blinded IAKIs. For anteromedial joint line injection, the needle was inserted within the portal formed by inferomedial patellar border, patellar tendon, and medial tibial plateau, directing the needle toward intercondylar notch with the knee extended [21] or flexed 30° [29] or 90° [15,29]. With the medial midpatellar, the injection was made between patella and patellar groove of femur at mid medial patellar junction with the knee extended [21,33,37,39]. The superomedial patellar injection was performed with the needle inserted in a 45° cephalomedial to caudolateral direction between the femoral condyle and the lateral border of patella at the superior one-third margin of the patella with the knee extended [38].
In contrast, the anterolateral joint line injection could be performed using four approaches with the needle inserted within the portal formed by inferolateral patellar border, patellar tendon, and lateral tibial plateau directing the needle towards intercondylar notch with the knee flexed [15,21] or directing the needle toward medial femoral condyle with the knee extended [28] or flexed between 30° and 40° [20] or flexed to 90° [28]. For lateral midpatellar approach, the injection was made between patella and patellar groove of femur at mid lateral patellar junction with the knee in an extended position [15,21,39]. In the superolateral patellar injection, the needle was inserted 1 cm above and 1 cm lateral to superolateral margin of patella in a 45° angle cephalolateral to caudomedial direction with the knee extended [14,22,29,32,39]. During lateral knee injection into the suprapatellar bursa, the needle was inserted from superolateral aspect of patella, one-fingerbreadth above and one-fingerbreadth lateral to the patella with the knee extended [35,40]. The infrapatellar injection was performed over the lateral condyle of tibia with the needle directed upwards and medially while the knee was in a flexed position [33].
For studies that performed guided IAKIs, two medial sites, MMP [37,39] and SMP [38] and four lateral sites, ALJL [20,28], LMP [39], SLP [13,39], and LSB [2,19,34–36,40] were used. The lateral sites were more commonly used during guided IAKIs while blinded injections were more frequently delivered through medial sites.
Within-study analyses
Guided vs blinded IAKIs
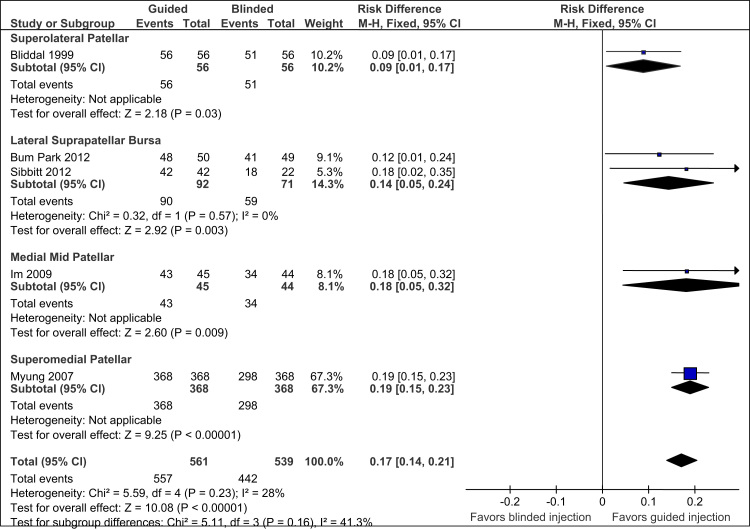
Five studies were included in the within-study analyses and these involved four injection sites (Fig. 3).
Fig. 3.
Forest plot—Injection accuracy of guided vs blinded knee injections.
Statistical heterogeneity of the five pooled studies was small (I² = 28%). For the two pooled studies on LSB using ultrasound-guided IAKIs, there was no statistical heterogeneity (I² = 0%). Guided IAKIs at MMP, SMP, LSB, and SLP sites were found to be significantly more accurate (ranges pooled ARD 0.09–0.19; p < 0.05) than their respective blinded injections (Fig. 3). The accuracy of medial sites (ranges of pooled ARD 0.18–0.19) was improved to a greater extent than the lateral sites (pooled ARD ranges 0.09–0.14) by guided injections. Of all the four sites, compared to a blinded injection, accuracy at SLP showed least improvement following image-guidance using air-arthrography.
Between-study analyses
Accuracy: Influence of injection site, image-guidance, and experience of clinician
Blinded
Of the three medial sites at which blinded injections were performed, the SMP site was linked with greatest accuracy of injection (82%), followed by AMJL (74%) and MMP (64%) (Table 2). One publication reported that injections performed at AMJL with knees flexed to 30° was more accurate (p = 0.035) than knees flexed to 90° [29].
Table 2.
Accuracy of blinded and guided knee injections
| Blinded knee approach: accuracy, no. out of total (%) |
Guided knee approach: accuracy, no. out of total (%) |
|||||||||||||||
| Lead author |
Medial injections |
Lateral injections |
Unknown | Medial injections |
Lateral injections |
Unknown | ||||||||||
| AMJL | MMP | SMP | ALJL | LMP | SLP | LSB | IFP | MMP | SMP | ALJL | LMP | SLP | LSB | |||
| Balint et al. [34] | 4/10 (40) | 18/19 (95) | ||||||||||||||
| Bliddal [13] | 51/56 (91) | 56/56 (100) | ||||||||||||||
| Bum Park et al. [35] | 41/49 (84) | 48/50 (96) | ||||||||||||||
| Chavez-Chiang et al. [28] | 74/76 (97) | |||||||||||||||
| Cunnington et al. [2] | 27/33 (82) | 32/35 (91) | ||||||||||||||
| Curtiss et al. [36] | 31/40 (78) | 40/40 (100) | ||||||||||||||
| Esenyel et al. [21] | 57/78 (73) | 44/78 (56) | 66/78 (85) | 58/78 (74) | ||||||||||||
| Glattes et al. [14] | 20/20 (100) | |||||||||||||||
| Im et al. [37] | 34/44 (77) | 43/45 (96) | ||||||||||||||
| Jackson et al. [15] | 60/80 (75) | 57/80 (71) | 74/80 (93) | |||||||||||||
| Jones et al. [4] | 39/59 (66) | |||||||||||||||
| Lopes et al. [31] | 37/37 (100) | |||||||||||||||
| Luc et al. [32] | 32/33 (97) | |||||||||||||||
| Myung et al. [38] | 298/368 (81) | 368/368 (100) | ||||||||||||||
| Park et al. [39] | 30/40 (75) | 41/43 (95) | 43/43 (100) | |||||||||||||
| Qvistgaard et al. [19] | 184/184 (100) | |||||||||||||||
| Shah and Wright [33] | 4/4 (100) | |||||||||||||||
| Sibbitt et al. [40] | 18/22 (82) | 42/42 (100) | ||||||||||||||
| Toda and Tsukimura [29] | 74/100 (74) | 35/50 (70) | ||||||||||||||
| Waddell et al. [20] | 20/20 (100) | |||||||||||||||
| Wiler et al. [30] | 25/27 (93) | 37/39 (95) | ||||||||||||||
| Wind and Smolinski [22] | 40/43 (93) | 19/44 (43) | 39/44 (89) | |||||||||||||
| SUBTOTAL | 191/258 (74) | 78/122 (64) | 338/411 (82) | 142/202 (70) | 132/158 (84) | 225/260 (87) | 59/71 (83) | 4/4 (100) | 115/149 (77) | 73/85 (86) | 368/368 (100) | 94/96 (98) | 41/43 (95) | 99/99 (100) | 364/370 (98) | 37/39 (95) |
| TOTAL | 607/791 (77) | 562/695 (81) | 115/149 (77) | 441/453 (97) | 598/608 (98) | 37/39 (95) | ||||||||||
| GRAND TOTAL | 1284/1635 (79) | 1076/1100 (98) | ||||||||||||||
Abbreviations: AMJL, anteromedial joint line; MMP, medial midpatellar; SMP, superomedial patellar; ALJL, anterolateral joint line; LMP, lateral midpatellar; SLP, superolateral patellar; LSB, lateral suprapatellar bursa; IFP, infrapatellar.
Of the four lateral sites at which blinded injections were performed, the SLP site was linked with greatest accuracy of injection (87%), followed by LMP (84%), LSB (83%), and ALJL (70%) (Table 2).
Guided
Of the two medial sites investigated during guided IAKIs, the SMP site was linked with greatest accuracy (100%) while MMP improved to 86% with image-guidance (Table 2). Based on a pooled study comparison, IAKIs at the MMP (ARD 0.22; 95% CI, 0.10–0.33; p = 0.0005) and SMP sites (ARD 0.18; 95% CI, 0.14–0.22; p < 0.0001) were significantly more accurate using image-guidance than when given blinded (Table 3). No studies evaluated the AMJL site.
Table 3.
Accuracy of knee injection: influence of site and image-guidance—Relative and absolute risk difference*
| Knee injection site | Relative risk (95% confidence Interval) | Absolute risk difference (95% confidence interval) | Chi squared2, p-value |
|---|---|---|---|
| Medial midpatellar (guided vs blind) | 1.34 (1.15–1.57) | 0.22 (0.10–0.33) | 12.17, p = 0.0005 |
| Superomedial patellar (guided vs blind) | 1.22 (1.16–1.27) | 0.18 (0.14–0.22) | 72.03, p < 0.0001 |
| Anterolateral joint line (guided vs blind) | 1.39 (1.27–1.53) | 0.28 (0.20–0.35) | 30.03, p < 0.0001 |
| Lateral midpatellar (guided vs blind) | 1.14 (1.04–1.26) | 0.12 (0.001–0.20) | 3.91, p = 0.05 |
| Superolateral patellar (guided vs blind) | 1.15 (1.10–1.21) | 0.13 (0.10–0.18) | 14.73, p = 0.0001 |
| Lateral suprapatellar bursa (guided vs blind) | 1.18 (1.07–1.32) | 0.15 (0.08–0.26) | 35.44, p < 0.0001 |
| Medial knee injections as a group (guided vs blind) | 1.27 (1.21–1.32) | 0.21 (0.17–0.24) | 92.13, p < 0.0001 |
| Lateral knee injections as a group (guided vs blind) | 1.22 (1.17–1.26) | 0.17 (0.14–0.20) | 101.48, p < 0.0001 |
| Guided vs Blinded injections as a group | 1.24 (1.21–1.27) | 0.19 (0.17–0.21) | 124.54, p < 0.0001 |
| Blinded knee injections: lateral vs medial as a group | 1.05 (1.00–1.12) | 0.04 (0.00–0.08) | 3.75, p = 0.05 |
| Guided knee injections: lateral vs medial as a group | 1.01 (0.99–1.03) | 0.01 (−0.01 to 0.03) | 1.29, p = 0.3 |
Relative risk is the proportionate difference in accuracy of injections (between groups as defined in each row) while absolute risk difference is the absolute difference in accuracy.
Pooling data across studies (Table 2), all four lateral sites (ALJL, LMP, SLP, and LSB) had excellent accuracy, 95–100%, when performed guided, though the best lateral site was still the SLP. Based on a pooled study comparison, there was a significant improvement in the accuracy of injections at LSB and SLP sites (pooled ARD 0.13–0.15; p ≤ 0.0001) while LMP site also improved (ARD 0.12; 95% CI 0.001–0.20; p = 0.05) with image-guidance (Table 3). IAKIs at ALJL were highly more accurate when guided (ARD 0.28; 95% CI, 0.20–0.35; p < 0.0001) (Table 3).
Experience
Blinded
Of four publications, only one study was designed formally to investigate the impact of injectors' experience on the accuracy of IAKI. The study found that the injector's experience influenced the accuracy rate of blinded injections at the SLP site; accuracy rate of 55% (95% CI 34–74) for the less experienced injector compared to 100% (95% CI 81–100) for the more experienced injector [36]. Luc et al. [32], however, in their trial of 33 knee injections reported a similar accuracy for blinded injections at the SLP site for a clinical fellow (96%) and experienced rheumatologist (100%). Two other publications that included “unknown” sites of blinded knee injections found similar accuracy irrespective of the level of experience, seniority, and training [2,4].
Guided
Similar accuracy was found for less experienced junior clinicians and injectors with more experience during guided IAKIs [2,32]. Cunnington et al. [2] reported 91% accuracy when a research fellow performed the injections using sonographic-guidance while Luc et al. [32] reported 100% accuracy when a medical fellow used “backflow of injected fluid” during IAKIs to confirm intra-articular placement of needles.
Outcome
Because of small numbers and differences in study design, it was not possible to pool data from those studies that looked at outcome associated with either accuracy or site of injection. There were three studies that reported outcomes related to use of image-guidance (using ultrasound); one was conducted on subjects with knee OA without effusion [41], another on OA and RA knees with effusion [40], and a third in knees with effusion [30]. Figure 4 shows the forest plots for two of these studies that suggested better pain reductions at 2 weeks with guided IAKIs [40,41]; no outcome data on pain was available in the third [30]. There was no difference in longer-term pain-relief, though duration of response was a month longer with ultrasound-guidance [41]. Using volume of synovial fluid aspirated as the outcome, image-guidance was associated with greater volume aspirated (see Fig. 4).
Fig. 4.
Forest plot—Outcome of guided vs blinded knee injections.
Discussion
In this systematic review, blinded IAKIs overall were reasonably accurate, in particular the lateral injection sites. The use of needle-guidance improved the accuracy of IAKIs significantly. There was, however, insufficient evidence to suggest that increased accuracy of knee injections resulted in an improved therapeutic outcome. The use of ultrasound-guided IAKIs though may lead to better short-term benefit.
We found good accuracy with most lateral approaches even when performed blinded, suggesting clinicians have a choice when selecting injection sites over the lateral aspect of the knee. However, due to a relatively low accuracy of ALJL injection when undertaken blinded (70%), we suggest it might be better undertaken with image-guidance. We also found the MMP was the least accurate site for both blinded and guided injections. A possible explanation for this is that with the approach the needle may engage with the medial knee plica or fat pad [3,43]. Medial injections with a partially flexed knee are deemed anecdotally least successful, more painful, and most likely to be loculated [43,44]. However, although there were few studies, our review did not find any significant difference in accuracy when injections were performed with the knee in extension or flexion.
Accuracy of injection for ultrasound-guided injections was not improved except with injection of the anterior lateral joint line site
The experience of injectors may influence the accuracy of blinded injections [4,36] though further studies are needed. In contrast, image-guided knee injections can be delivered accurately independent of the injector's experience (including junior clinicians with a short training period) [2,32]. This perhaps indicates that delivering an injection blinded using anatomical palpation may require experiential learning.
From the pooled data across studies, all four lateral sites (ALJL, LMP, SLP, and LSB) had excellent accuracy, 95–100%, when performed guided though the best lateral site was SLP. Both within-study and between-study analyses found that guided injections, irrespective of sites of injection, to be more accurate than blinded injections. Overall it can be estimated that approximately one in five blinded injections are inaccurate. Other reviews have found similar findings with respect to accuracy of blinded vs guided injections [45] and blinded injections at the LMP and AMJL sites [46]. Daley et al. [1] pooled seven papers evaluating three knee injection sites and a total of 429 injections but excluded trials investigating accuracy of IAKIs performed on cadaveric knees. Our review included more papers that have been published since then, pooling results from 22 studies, evaluating accuracy of eight injection sites, and totaling 2735 knee injections. Herman [46] though, who included cadaveric samples, found a lower accuracy for the MMP [56% (95% CI 45–66)] and ALJL sites [67% (95% CI 43–91)] but higher accuracy for the SLP [91% (95% CI 84–99)] and SMP sites [93% (95% CI 81–98)]. The reason for the differences in values could be due to the smaller number of publications available at the time of their review and unlike Hermans [46], our review grouped injections performed over the lateral joint line as ALJL irrespective of the degree of flexion or extension of the knees.
In this review, guided injections were undertaken primarily using ultrasound. Only three of the 15 publications that evaluated accuracy of IAKIs used other guided techniques such as air-arthrography [13] and fluoroscopy [20,38]. When analysis of accuracy of IAKIs was assessed for ultrasound-guided injections only, accuracy of all sites remained the same with the exception of the ALJL site where accuracy reduced slightly to 97%. The SMP site has not been evaluated for accuracy, perhaps reflecting the difficulty of the ultrasound technique when performed over the medial aspect of the knee.
In two studies, ultrasound was used to both guide and assess accuracy. In one, confirmation of accuracy was determined by the appearance of an injected volume of air (air bubble) within the knee joint on the ultrasound image [19]. A limitation of this method though is that the evidence of placement lasts only a few seconds as the air bubbles soon dissolve and disappear. The other trial did not describe how accuracy was determined [28]. The exclusion of these two studies from the analysis did not, however, affect the results.
Few studies identified in this review attempted to correlate accuracy of knee injection with treatment outcome. Indeed there was only one trial on knee OA; this trial reported better outcome for accurate injections when compared to inaccurate IAKIs [29]. Two other studies [2,4] evaluated outcomes of accurate IAKIs together with outcomes from other joints injections (including shoulder, elbow, wrist, ankle, finger, and acromioclavicular joints) making it difficult to assess outcome specifically at the knee joint. Accuracy of injection varies at different joint sites and for studies that pooled data across many joints, it might have been more informative if treatment outcome was reported by joint [2,4,47]. For trials that used a mixed sample of OA and RA such as that by Sibbitt et al. [40], it would have been helpful also if the therapeutic response in the OA group was presented separately from the RA group as it is possible that disease type may have influenced outcome. In a separate trial, compared to those whose injections were targeted within the joint, there was no difference in outcome in those where the injection was delivered extra-articularly [48].
There were also only two studies that compared outcome between different knee injection sites but found no difference between those sites [28,33], that is, between LMP and ALJL [28] and IFP and medial knee injections [33], though in the latter study the IFP site was associated with less frequent joint aspiration and worse patients' perceived improvement [33].
For outcome relating to IAKIs, the best studied issue has been a comparison of outcomes of ultrasound-guided vs blinded injections, though accuracy of these injections was not assessed. From the few studies, ultrasound-guided injections resulted in better aspiration [40] and short-term therapeutic benefit than blinded IAKIs [40,41].
There are a number of limitations to be considered when interpreting the results of this review. First, there were relatively few studies that permitted within-study analyses of the accuracy of blinded vs guided injections. There was, however, little evidence of statistical heterogeneity of the pooled studies suggesting a low risk of bias. Second, we included studies investigating the accuracy of IAKIs performed on cadavers [21,36] where it may be argued that altered tissue properties could affect the outcome (accuracy of injection). However, the use of knee dissections to verify accurate placement of injected materials provide direct evidence in contrast to relying on interpretation of the spread of contrast material on radiographs during imaging to deduce intra-articular placement. We analyzed our data by including and excluding cadaveric studies and found accuracy for SLP and LSB to be comparable while for ALJL and LMP to be slightly higher if the cadaveric studies were excluded. Third, it is possible that accuracy of injection sites could also be influenced by the method of assessment of injection accuracy (including observer variability), though generally there was a trend for greater accuracy irrespective of the assessment method.
Conclusion
Blinded IAKIs can be performed with reasonably good accuracy, though accuracy does vary by injection site and is improved with needle-guidance. Injectors' experience may influence the accuracy of blinded injections. Further studies are required to address the question whether accurate localization is linked with an improved clinical outcome.
Acknowledgments
The Research into Osteoarthritis in Manchester (ROAM) research team Arthritis Research UK
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-No Derivative Works License, which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
This review was funded by a program grant from Arthritis Research UK (Grant Number 18676). Nasimah Maricar is funded by a Clinical Doctoral Fellowship award from the National Institute for Health Research.
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.semarthrit.2013.04.010.
Appendix A. Supplementary materials
Supplementary Material
References
- 1.Daley E.L., Bajaj S., Bisson L.J., Cole B.J. Improving injection accuracy of the elbow, knee, and shoulder: does injection site and imaging make a difference? A systematic review. Am J Sports Med. 2011;39:656–662. doi: 10.1177/0363546510390610. [DOI] [PubMed] [Google Scholar]
- 2.Cunnington J., Marshall N., Hide G., Bracewell C., Isaacs J., Platt P. A randomized, double-blind, controlled study of ultrasound-guided corticosteroid injection into the joint of patients with inflammatory arthritis. Arthritis Rheum. 2010;62:1862–1869. doi: 10.1002/art.27448. [DOI] [PubMed] [Google Scholar]
- 3.Gnanadesigan N., Smith R.L. Knee pain: osteoarthritis or anserine bursitis? J Am Med Dir Assoc. 2003;4:164–166. doi: 10.1097/01.JAM.0000064461.69195.58. [DOI] [PubMed] [Google Scholar]
- 4.Jones A., Regan M., Ledingham J., Pattrick M., Manhire A., Doherty M. Importance of placement of intra-articular steroid injections. BMJ. 1993;307:1329–1330. doi: 10.1136/bmj.307.6915.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Courtney P., Doherty M. Joint aspiration and injection and synovial fluid analysis. Best Pract Res Clin Rheumatol. 2009;23:161–192. doi: 10.1016/j.berh.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Lockman L.E. Practice tips. Knee joint injections and aspirations: the triangle technique. Can Fam Physician. 2006;52:1403–1404. [PMC free article] [PubMed] [Google Scholar]
- 7.Zuber T.J. Knee joint aspiration and injection. Am Fam Physician. 2002;66:1497–1507. [PubMed] [Google Scholar]
- 8.Esenyel C.Z., Esenyel M., Yesiltepe R., Ayanoglu S., Bulbul M., Sirvanci M. The correlation between the accuracy of steroid injections and subsequent shoulder pain and function in subacromial impingement syndrome. Acta Orthop Traumatol Turc. 2003;37:41–45. [PubMed] [Google Scholar]
- 9.Eustace J.A., Brophy D.P., Gibney R.P., Bresnihan B., FitzGerald O. Comparison of the accuracy of steroid placement with clinical outcome in patients with shoulder symptoms. Ann Rheum Dis. 1997;56:59–63. doi: 10.1136/ard.56.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Partington P.F., Broome G.H. Diagnostic injection around the shoulder: hit and miss? A cadaveric study of injection accuracy. J Shoulder Elbow Surg. 1998;7:147–150. doi: 10.1016/s1058-2746(98)90226-9. [DOI] [PubMed] [Google Scholar]
- 11.Souza P.M., Aguiar R.O., Marchiori E., Bardoe S.A. Arthrography of the shoulder: a modified ultrasound guided technique of joint injection at the rotator interval. Eur J Radiol. 2010;74:e29–e32. doi: 10.1016/j.ejrad.2009.03.020. [DOI] [PubMed] [Google Scholar]
- 12.Yamakado K. The targeting accuracy of subacromial injection to the shoulder: an arthrographic evaluation. Arthroscopy. 2002;18:887–891. doi: 10.1053/jars.2002.35263. [DOI] [PubMed] [Google Scholar]
- 13.Bliddal H. Placement of intra-articular injections verified by mini air-arthrography. Ann Rheum Dis. 1999;58:641–643. doi: 10.1136/ard.58.10.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glattes R.C., Spindler K.P., Blanchard G.M., Rohmiller M.T., McCarty E.C., Block J.A. Simple, accurate method to confirm placement of intra-articular knee injection. Am J Sports Med. 2004;32:1029–1031. doi: 10.1177/0363546503258703. [DOI] [PubMed] [Google Scholar]
- 15.Jackson D.W., Evans N.A., Thomas B.M. Accuracy of needle placement into the intra-articular space of the knee. J Bone Joint Surg Am. 2002;84:1522–1527. doi: 10.2106/00004623-200209000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Di S.L., Paoloni M., Ioppolo F., Dimaggio M., Di R.S., Santilli V. Ultrasound-guided aspiration and corticosteroid injection of Baker's, cysts in knee osteoarthritis: a prospective observational study. Am J Phys Med Rehabil. 2010;89:970–975. doi: 10.1097/PHM.0b013e3181fc7da2. [DOI] [PubMed] [Google Scholar]
- 17.Hurdle M.F. In: Ultrasound-guided knee injections atlas of ultrasound-guided procedures in interventional pain management. Narouze S.N., editor. Springer; New York: 2011. pp. 331–334. [Google Scholar]
- 18.Tarhan S., Unlu Z. Magnetic resonance imaging and ultrasonographic evaluation of the patients with knee osteoarthritis: a comparative study. Clin Rheumatol. 2003;22:181–188. doi: 10.1007/s10067-002-0694-x. [DOI] [PubMed] [Google Scholar]
- 19.Qvistgaard E., Kristoffersen H., Terslev L., Danneskiold-Samsoe B., Torp-Pedersen S., Bliddal H. Guidance by ultrasound of intra-articular injections in the knee and hip joints. Osteoarthritis Cartilage. 2001;9:512–517. doi: 10.1053/joca.2001.0433. [DOI] [PubMed] [Google Scholar]
- 20.Waddell D., Estey D., Bricker D.C., Marsala A. Viscosupplementation under fluoroscopic control. Am J Med Sports. 2001;3:237–241. [Google Scholar]
- 21.Esenyel C., Demirhan M., Esenyel M., Sonmez M., Kahraman S., Sinel B. Comparison of four different intra-articular injection sites in the knee: a cadaver study. Knee Surg Sports Traumatol Arthrosc. 2007;15:573–577. doi: 10.1007/s00167-006-0231-6. [DOI] [PubMed] [Google Scholar]
- 22.Wind W.M., Jr., Smolinski R.J. Reliability of common knee injection sites with low-volume injections. J Arthroplasty. 2004;19:858–861. doi: 10.1016/j.arth.2004.02.042. [DOI] [PubMed] [Google Scholar]
- 23.Jadad A.R., Moore R.A., Carroll D. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 24.Schulz K.F., Chalmers I., Hayes R.J., Altman D.G. Empirical Evidence of Bias. J Am Med Assoc. 1995;273:408–412. doi: 10.1001/jama.273.5.408. [DOI] [PubMed] [Google Scholar]
- 25.von E.E., Altman D.G., Egger M., Pocock S.J., Gotzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 26.Vandenbroucke J.P., Ev E.l.m., Altman D.G., Gotzsche P.C., Mulrow C.D., Pocock S.J. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007;147:573–577. doi: 10.7326/0003-4819-147-8-200710160-00010-w1. [DOI] [PubMed] [Google Scholar]
- 27.Des J., Lyles C., Crepaz N. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health. 2004;94:361–366. doi: 10.2105/ajph.94.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chavez-Chiang C.E., Sibbitt W.L., Jr., Band P.A., Chavez-Chiang N.R., Delea S.L., Bankhurst A.D. The highly accurate anteriolateral portal for injecting the knee. Sports Med Arthrosc Rehabil Ther Technol. 2011;3:6. doi: 10.1186/1758-2555-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Toda Y., Tsukimura N. A comparison of intra-articular hyaluronan injection accuracy rates between three approaches based on radiographic severity of knee osteoarthritis. Osteoarthritis Cartilage. 2008;16:980–985. doi: 10.1016/j.joca.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 30.Wiler J.L., Costantino T.G., Filippone L., Satz W. Comparison of ultrasound-guided and standard landmark techniques for knee arthrocentesis. J Emerg Med. 2010;39:76–82. doi: 10.1016/j.jemermed.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 31.Lopes R.V., Furtado R.N.V., Parmigiani L., Rosenfeld A., Fernandes A.R.C., Natour J. Accuracy of intra-articular injections in peripheral joints performed blindly in patients with rheumatoid arthritis. Rheumatology (Oxford) 2008;47:1792–1794. doi: 10.1093/rheumatology/ken355. [DOI] [PubMed] [Google Scholar]
- 32.Luc M., Pham T., Chagnaud C., Lafforgue P., Legre V. Placement of intra-articular injection verified by the backflow technique. Osteoarthritis Cartilage. 2006;14:714–716. doi: 10.1016/j.joca.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 33.Shah K.D., Wright V. Intra-articular hydrocortisone in osteo-arthrosis. Ann Rheum Dis. 1967;26:316–318. doi: 10.1136/ard.26.4.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Balint P.V., Kane D., Hunter J., McInnes I.B., Field M., Sturrock R.D. Ultrasound guided versus conventional joint and soft tissue fluid aspiration in rheumatology practice: a pilot study. J Rheumatol. 2002;29:2209–2213. [PubMed] [Google Scholar]
- 35.Bum Park Y., Ah Choi W., Kim Y.K., Chul Lee S., Hae Lee J. Accuracy of blind versus ultrasound-guided suprapatellar bursal injection. J Clin Ultrasound. 2012;40:20–25. doi: 10.1002/jcu.20890. [DOI] [PubMed] [Google Scholar]
- 36.Curtiss H.M., Finnoff J.T., Peck E., Hollman J., Muir J., Smith J. Accuracy of ultrasound-guided and palpation-guided knee injections by an experienced and less-experienced injector using a superolateral approach: a cadaveric study. PM R. 2011;3:507–515. doi: 10.1016/j.pmrj.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 37.Im S.H., Lee S.C., Park Y.B., Cho S.R., Kim J.C. Feasibility of sonography for intra-articular injections in the knee through a medial patellar portal. J Ultrasound Med. 2009;28:1465–1470. doi: 10.7863/jum.2009.28.11.1465. [DOI] [PubMed] [Google Scholar]
- 38.Myung J.S., Lee J.W., Lee J.Y. Usefulness of fluoroscopy-guided intra-articular injection of the knee. J Korean Radiol Soc. 2007;56:563–567. [Google Scholar]
- 39.Park Y., Lee S.C., Nam H.S., Lee J., Nam S.H. Comparison of sonographically guided intra-articular injections at 3 different sites of the knee. J Ultrasound Med. 2011;30:1669–1676. doi: 10.7863/jum.2011.30.12.1669. [DOI] [PubMed] [Google Scholar]
- 40.Sibbitt W., Kettwich L., Band P., Chavez-Chiang N., Delea S., Haseler L.J. Does ultrasound guidance improve the outcomes of arthrocentesis and corticosteroid injection of the knee? Scand J Rheumatol. 2012;41:66–72. doi: 10.3109/03009742.2011.599071. [DOI] [PubMed] [Google Scholar]
- 41.Sibbitt W.L., Jr., Band P.A., Kettwich L.G., Chavez-Chiang N.R., Delea S.L., Bankhurst A.D. A randomized controlled trial evaluating the cost-effectiveness of sonographic guidance for intra-articular injection of the osteoarthritic knee. J Clin Rheumatol. 2011;17:409–415. doi: 10.1097/RHU.0b013e31823a49a4. [DOI] [PubMed] [Google Scholar]
- 42.Moher D., Pham B., Jones A. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet. 1998;352:609–613. doi: 10.1016/S0140-6736(98)01085-X. [DOI] [PubMed] [Google Scholar]
- 43.Roberts N.W., Hayes C.W., Breitbach S.A., Owen J. Dry taps and what to do about them: a pictorial essay on failed arthrocentesis of the knee. Am J Med. 1996;100:461–464. doi: 10.1016/s0002-9343(97)89524-1. [DOI] [PubMed] [Google Scholar]
- 44.Schumacher H.R. Aspiration and injection therapies for joints. Arthritis Rheum. 2003;49:413–420. doi: 10.1002/art.11056. [DOI] [PubMed] [Google Scholar]
- 45.Daley E.L., Bajaj S., Bisson L.J., Cole B.J. Improving injection accuracy of the elbow, knee, and shoulder: does injection site and imaging make a difference? A systematic review. Am J Sports Med. 2011:39. doi: 10.1177/0363546510390610. [DOI] [PubMed] [Google Scholar]
- 46.Hermans J., Bierma-Zeinstra S.M., Bos P.K., Verhaar J.A., Reijman M. The most accurate approach for intra-articular needle placement in the knee joint: a systematic review. [Review] Semin Arthritis Rheum. 2011;41:106–115. doi: 10.1016/j.semarthrit.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 47.Sibbitt W.L., Band P.A., Chavez-Chiang N.R., Delea S.L., Norton H.E., Bankhurst A.D.A. Randomized controlled trial of the cost-effectiveness of ultrasound-guided intraarticular injection of inflammatory arthritis. J Rheumatol. 2011;38:252–263. doi: 10.3899/jrheum.100866. [DOI] [PubMed] [Google Scholar]
- 48.Sambrook P.N., Champion G.D., Browne C.D., Cairns D., Cohen M.L., Ray R.O. Corticosteroid injection for osteoarthritis of the knee: peripatellar compared to intra-articular route. Clin Exp Rheumatol. 1989;7:609–613. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material