Abstract
[Purpose] The aim of the present study was to investigate the effect of balance training with visual biofeedback on balance, body symmetry, and function among individuals with hemiplegia following a stroke. [Subjects and Methods] The present study was performed using a randomized controlled clinical trial with a blinded evaluator. The subjects were twenty adults with hemiplegia following a stroke. The experimental group performed balance training with visual biofeedback using Wii Fit® together with conventional physical therapy. The control group underwent conventional physical therapy alone. The intervention lasted five weeks, with two sessions per week. Body symmetry (baropodometry), static balance (stabilometry), functional balance (Berg Balance Scale), functional mobility (Timed Up and Go test), and independence in activities of daily living (Functional Independence Measure) were assessed before and after the intervention. [Results] No statistically significant differences were found between the experimental and control groups. In the intragroup analysis, both groups demonstrated a significant improvement in all variables studied. [Conclusion] The physical therapy program combined with balance training involving visual biofeedback (Wii Fit®) led to an improvement in body symmetry, balance, and function among stroke victims. However, the improvement was similar to that achieved with conventional physical therapy alone.
Key words: Postural balance, Stroke, Visual biofeedback
INTRODUCTION
Stroke causes sensory-motor impairment, leading to balance problems, falls, and considerable functional limitation1). Balance is associated with the motion of the body in a static posture, which is maintained through sensory-motor interactions. The control of balance depends on sensory information (visual, vestibular, and somatosensorial), which triggers motor actions2). A stroke leads to the incapacity to perform different tasks of extreme importance to daily living3).
Hemiplegia is the most common result of a stroke4). Body asymmetry and difficulty transferring weight to the paretic side affect the capacity to maintain postural control, impeding the orientation and stability necessary for proper movement of the trunk and limbs5,6,7,8,9).
Visual biofeedback is a rehabilitation method that can be used during static balance training, offering the patient visual information on the position of the center of gravity within the range of stability as the patient stands on a pressure plate. Upon changing the center of gravity on the support base, the individual can view the movement of the body on a monitor. Visual biofeedback stimulates proprioceptive information that may be negatively affected in stroke victims10). Novel biofeedback resources are currently being developed for balance training. One such device, Wii Fit® from Nintendo®, simulates the body movements of an individual during play activities that require balance and displays the results on a television screen.
A systematic review revealed a limited number of randomized controlled clinical trials addressing the effect of balance training with the use of visual biofeedback. The evidence suggests that this modality is beneficial, especially in terms of body symmetry, but little has been reported with regard to balance and function in stroke victims.
The aim of the present study was to assess balance, body symmetry, and function among individuals with hemiplegia due to a stroke performing to conventional physical therapy alone or in combination with balance training using visual biofeedback.
SUBJECTS AND METHODS
This study received approval from the Human Research Ethics Committee of the Universidade Nove de Julho (Brazil) under process number 312133, in compliance with Resolution 196/96 of the Brazilian Health Board. All individuals agreed to participate in the study and signed a statement of informed consent.
A randomized controlled clinical trial was carried out at the physical therapy clinic of the Universidade Nove de Julho (Brazil). The sample was made up of individuals with chronic sequelae stemming from a stroke who met the following inclusion criteria: weekly physical therapy sessions at the institution, the ability to remain in an orthostatic position without support, absence of osteoarticular deformities, and the ability to understand the visual biofeedback. Individuals with associated diseases not pertinent to the physiopathology of stroke were excluded from the study.
Following the initial evaluation and fulfillment of the eligibility criteria, the participants were randomly allocated to an experimental group (conventional physical therapy plus balance training with visual biofeedback using the Wii Fit® interaction program from Nintendo®) and a control group (conventional physical therapy alone). Randomization numbers were generated from a randomization table at a central office. A series of numbered, sealed, opaque envelopes was used to ensure confidentiality. Each envelop contained a card stipulating to which group the individual would be allocated.
Evaluations of balance, body symmetry, and function were performed before and after the intervention by an evaluator who was blinded to which group the subjects belonged. Anthropometric characteristics (body mass, stature, and body mass index) were first determined. The evaluation was carried out on a single day, and the order of administration of the measures was determined by lots.
Functional balance was assessed using the Berg Balance Scale11,12,13), functional mobility was assessed using the Timed Up and Go test (TUGT)14), and independence in activities of daily living was assessed using the Functional Independence Measure15).
For assessment of static balance (stabilometric exam) and body symmetry (baropodometric exam), a pressure plate was used (Medicapteurs®, Fusyo® model) that had 2300 pressure sensors with a precision of 0.1 mm and an acquisition frequency of 40 Hz. This platform records oscillations from the center of pressure (COP) in the anteroposterior and mediolateral directions. In the same exam, the platform measures body symmetry by recording mean peak plantar pressure. The data were recorded and interpreted using the Fusyo Analysis® program. During the test, the subject remained in orthostatic position on the pressure plate, was barefoot, kept the arms alongside the body and staring at a fixed point marked on the wall at a distance of one meter at the height of the glabella of each individual, with an unrestricted width of the foot base and the heels in alignment. Data acquisition was performed for 30 seconds under each condition (eyes open and eyes closed).
For the stabilometric exam, the oscillation of the COP on the mediolateral (X) and anteroposterior (Y) axes was defined using the method described by Winter16):
| • Delta X (∆X) = maximal oscillation of the COP in the X direction in mm = maximal COPX − minimal COPX; |
| • Delta Y (∆Y) = maximal oscillation of the COP in the Y direction in mm = |
| • maximal COPY − minimal COPY. |
The area of total displacement of the COP was defined as:
| • Displacement area = (∆X)* (∆Y) (mm2). |
The intervention was carried out over a five-week period, with two sessions per week. Conventional physical therapy sessions lasted 60 minutes, and balance training lasted 30 minutes.
Conventional physical therapy involved stretching, joint movement, muscle strengthening, static and dynamic balance training, and the training of functional activities. These procedures were performed in accordance with the physical therapy sessions in which the individuals were already participating.
The sessions in the experimental group involved conventional physical therapy and 30 minutes of balance training with visual biofeedback using the Wii Fit® program, which reproduces real movements in virtual actions. This equipment consists of a platform, referred to as the Wii Balance Board®, which has sensors that measure weight and center of gravity. Wii Fit® has 40 types of balance exercises. However, for the present study, only three were selected: plataformas, pesca bajo cero, and la cuerda floja. The degree of difficulty is based on the interaction with the exercises, with the patient going on to the next level after successfully completing the previous level. Each exercise lasted 10 minutes, with a rest interval between exercises based on the physical conditioning of each patient.
For the statistical analysis, the Kolmogorov-Smirnov test was used to determine the distribution of the sample, using the parametric test in the analysis of the pressure plate data and the nonparametric test in the analysis of the functional capacity scales. Paired and unpaired t tests were used for the intra and intergroup comparisons, respectively. The GraphPad InStat program (version 3.5, 2000, Windows 95) was used for the statistical analysis, with the level of significance set at 5% (p < 0.05).
RESULTS
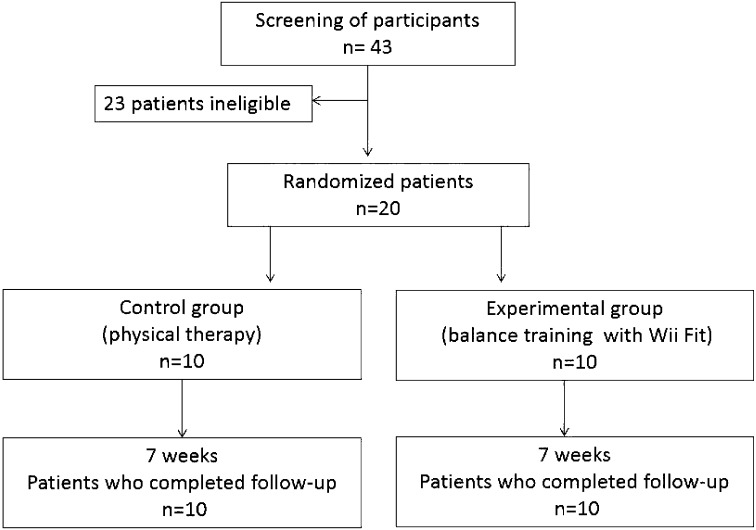
Analyses were performed for 43 participants (Fig. 1). Personal characteristics of the participants are presented in Table 1. There was no statistically significant difference between the groups for personal characteristics.
Fig. 1.
Flowchart of the study based on CONSORT
Table 1. Characteristics of the individuals in the experimental group and control group.
| Groups | ||
| Experimental | Control | |
| Individuals (n) | 10 | 10 |
| Age (years) | 65.2 (12.5) | 63.5 (14.5) |
| Body mass (Kg) | 62.7 (8.2) | 76.5 (5.3) |
| Height (m) | 1.58 (3.1) | 1.63 ( 2.4) |
| BMI (Kg/m2) | 19.4 (2.8) | 22.4 (1.5) |
| Time since stroke (months) | 12.3 (7.1) | 15.2 (6.6) |
| Males/females | 5/5 | 4/6 |
| Type of stroke (ischemic/hemorrhagic) | 9/1 | 9/1 |
| Affected side (right/left) | 6/4 | 7/3 |
| Predominance (brachial/cural) | 4/6 | 8/2 |
| Brunnstrom stage | 3.7 (0.6) | 3.6 (0.8) |
mean and standard deviation
Table 2 displays the results of the variables before and after intervention, with the values expressed as the mean and standard deviation. The results demonstrate greater control of static and dynamic balance, lesser time needed for the execution of orthostatic mobility, and improved performance in the execution of functional activities after the intervention in both the experimental and control groups. The intergroup analysis revealed no statistically significant differences between groups (p > 0.05).
Table 2. Result before and after intervention in the experimental group and control group.
| Experimental group | Control group | |||
| Before | After | Before | After | |
| Peak plantar pressure on the paretic side (g/cm2) | 1138.2 (333.3) | 1309.5 (260.1)* | 1232.1 (182.1) | 1319.7 (194.6)* |
| Peak plantar pressure on the non-paretic side (g/cm2) | 1465.7 (285.2) | 1350.4 (243.6)* | 1490.9 (196.1) | 1357.0 (185.4)* |
| Mediolateral oscillation with open eyes (cm) | 4.55 (0.55) | 2.87 (0.93)* | 4.3 (1.69) | 3.13 (1.81)* |
| Mediolateral oscillation with closed eyes (cm) | 5.40 (0.51) | 3.97 (0.94)* | 5.17 (2.07) | 3.64 (1.97)* |
| Anterior-posterior oscillations with open eyes (cm) | 1.18 (0.06) | 1.13 (0.08)* | 1.18 (0.13) | 1.12 (0.08)* |
| Anterior-posterior oscillations with closed eyes (cm) | 1.48 (0.27) | 1.35 (0.27)* | 1.26 (0.15) | 1.18 (0.07)* |
| Oscillations from the center of pressure with open eyes (cm) | 4.93 (1.74) | 2.96 (1.37)* | 4.55 (2.15) | 2.92 (1.80)* |
| Oscillations from the center of pressure with closed eyes (cm) | 7.49 (2.69) | 5.00 (2.09)* | 6.16 (3.72) | 3.71 (2.52)* |
| Berg Balance Scale | 39.6 (6.43) | 41.9 (6.91)* | 37.2 (5.22) | 42.2 (4.80)* |
| Timed Up and Go test (s) | 27.9 (8.22) | 24.3 (8.64)* | 28.1 (3.10) | 25.2 (2.78)* |
| Functional independence measure | 4.91 (0.96) | 6.12 (0.68)* | 4.80 (0.63) | 5.72 (0.67)* |
mean and standard deviation. *Dependent t-test p<0.05
Body symmetry was assessed using baropodometry, measuring the mean peak plantar pressure (PP) on the paretic and non-paretic sides. In the pre-intervention assessment, the paretic side differed significantly from the non-paretic side (p < 0.001), whereas no significant difference between sides was found in the post-intervention period (p > 0.05), as all individuals in both groups demonstrated more symmetrical distribution of PP following treatment. Moreover, both groups exhibited an increase in PP on the paretic side (experimental group − p < 0.05; control group − p > 0.05) and a decrease in PP on the non-paretic side (experimental group − p > 0.05; control group − p < 0.01) following treatment.
Both groups exhibited a reduction in mediolateral oscillations of the COP following treatment, thereby demonstrating greater orthostatic control. The control group achieved greater improvement with the eyes open (p < 0.001) than with the eyes closed (p < 0.05), whereas the experimental group exhibited lesser mediolateral oscillation after treatment under both conditions (eyes open and closed) (p < 0.001).
Both groups exhibited a reduction in anteroposterior oscillations of the COP following treatment. The control group achieved greater orthostatic control with the eyes both open and closed (p < 0.05), whereas the experimental group achieved a greater reduction in anteroposterior oscillation with the eyes closed (p < 0.01) than with the eyes open (p < 0.05).
The total area of oscillation of the COP underwent a reduction following treatment in the control group, with different degrees of reduction when the eyes were open (p < 0.001) and closed (p < 0.05). The same degree of reduction in body oscillations occurred in the experimental group following treatment with the eyes open and closed (p < 0.001). These findings demonstrate that both interventions led to lesser body oscillation and, consequently, greater orthostatic control.
DISCUSSION
The aim of the present study was to assess the effect of the use of Wii Fit® as a visual biofeedback resource for balance training in patients with chronic sequelae stemming from a stroke. Both the experimental group (conventional physical therapy + balance training with Wii Fit®) and control group (conventional physical therapy alone) demonstrated improvements in body symmetry, static and functional balance, functional mobility, and independence in activities of daily living. However, the intergroup analysis revealed no statistically significant differences between groups at the end of the five-week intervention.
Wii Fit® balance training is a virtual reality technology that simulates the learning of a real activity and allows an increase in training intensity, providing three-dimensional feedback through visual, sensory, and auditory stimulation. This new technology allows the practitioner to interact with a computer-generated scenario (a virtual world), making corrections in the execution of a task. There are few studies on the inclusion of virtual reality systems in neurological rehabilitation, and randomized clinical trials are needed to determine the viability, safety, efficacy, and value of such systems in patients during physical therapy16).
With Wii exercises, the information displayed on the television screen offers positive reinforcement, facilitating improvement in the execution of the tasks. A study carried out in Canada assessing upper limb function in the performance of activities of daily living concluded that Wii exercises constitute real, easy, safe activities that have the potential to improve motor function in stroke victims17).
A study carried out by Walker10) compared conventional physical therapy with physical therapy combined with visual biofeedback on patients following a stroke and found no significant differences between groups, as both exhibited motor improvements, as determined by the three measures employed–the Berg Balance Scale, TUGT, and Gait Speed test. Geiger18) compared conventional physical therapy with visual biofeedback in hemiparetic patients and found no differences between interventions, as determined by the Berg Balance Scale and TUGT. Both aforementioned studies used the Balance Master program as the visual biofeedback, for which the individual stands on a pressure plate and executes body movements without moving the support base while a computer screen displays the body movement that should be executed. The activities are the same as those performed in the Wii program. What differentiates these resources is the illustration on the screen (the visual biofeedback of each program).
Srivastava19) also carried out a study on stroke victims using the Balance Master program, in which the patients carried out activities with visual biofeedback for twenty minutes five times a week for four weeks. Forty-five patients between 22 and 65 years of age with a mean time of 16 months elapsed since stroke were evaluated using the Berg Balance Scale and Barthel Index, which demonstrated significant improvements in both balance and function. In the study by Cho et al., the best results after balance training with virtual reality were observed in functional balance (increase of 4 points in BBS) and TUGT (−1.3 seconds). These results are similar to these in the present study, in which it was observed that there was an increase of 1 point in BBS and 3.6 seconds in TUGT.
Rehabilitation institutions often do not offer visual biofeedback resources, which cost more than conventional physical therapy. However, this situation is changing, and many institutions are investing in such resources, as patients demonstrate greater motivation when sessions involve fun activities with therapeutic objectives. The Wii program is less expensive than the Balance Master program and is easier to transport. Therefore, recent studies have preferred the use of the Wii for orthostatic balance training20).
There are as yet no studies assessing psychosocial factors in this type of intervention. As emotional behavior is known to be affected after a stroke21), addressing this alteration in rehabilitation could offer further benefits.
Leisure activities constitute a fundamental human right and an important factor to quality of life. Individuals with physical disabilities often do not participate in such activities. Thus, virtual reality can serve as a form of rehabilitation associated to leisure, as patients perceive this technique as pleasant and successful. Moreover, the participants in the present study demonstrated clear preferences with regard to motivation and learning, performing the virtual reality tasks in a coherent fashion and with a high degree of interest throughout the intervention period. Virtual reality appears to provide various opportunities and motivation for leisure activities among young adults with physical disabilities. Ease of use and adaptability make this a viable option for such patients21).
The Nintendo Wii Balance Board® is one of the more recent virtual reality programs researched and analyzed, as it precisely detects performance during a standing posture. A recent study carried out with two individuals with multiple physical disabilities analyzed the capacity to actively adjust standing posture based on visual stimuli. The data demonstrated a significant increase in the length of time in maintaining postural control in both participants22).
Improvements in motor function following a stroke occur as the result of spontaneous recovery, learning, and practice due to reorganization of the brain. Studies suggest that this process is strengthened by specific intensive tasks. Virtual reality biofeedback has emerged as a new computer-assisted paradigm that allows greater training intensity while providing sensory feedback. More than mere play, use of this technology can provide neuroplasticity23).
A literature review carried out by Barclay-Goddard24) and published in the Cochrane Library reported that visual or auditory biofeedback in combination with the use of a pressure plate leads to greater static balance control, but has no impact on functional independence. The patients in seven clinical trials achieved a more balanced orthostatic position, but with no improvement in balance during functional activities
Based on the findings of the present study, physical therapy patients should perform both static balance exercises as well as functional exercises, applying the static balance acquired through visual biofeedback training to functional activities. The review carried out by Barclay-Goddard24) does not address balance training combined with conventional physical therapy, which also includes training sessions in activities of daily living.
A recent study determined the efficacy of the Wii Balance Board® in comparison with a pressure plate in the acquisition of orthostatic balance with the eyes open and eyes closed as well as with a one-foot and two-foot stance16). The evaluation was carried out on 30 healthy individuals (mean age: 23.7 ± 5.6 years) with no lower-limb impairment in sessions lasting approximately one and a half hours over a 14-day period, totaling 24 hours of training. The study demonstrated the efficacy and validity of the Wii Balance Board® in the acquisition of balance control during exercises in the two-foot stance with the eyes open, although it did in the one-foot stance with the eyes closed.
Visual biofeedback in combination with physical training may also enhance the effects of motor training, as similar mechanisms may be involved in Wii exercises. One randomized study assessed the viability, safety, and efficacy of Wii exercises with regard to the improvement in recovery of upper limbs in 20 stroke victims aged 18 to 85 years, with motor deficit and less than six months since stroke. The authors compared the use of the Wii with conventional therapy carried out in eight 60-minute sessions over a two-week period and concluded that the Wii is valid and efficacious for use in neurological rehabilitation25).
The present study related balance training with visual biofeedback to body symmetry and distribution of plantar pressure. No other studies addressing these aspects were found in the literature.
All participants in both groups in the present study exhibited greater balance control, body symmetry, and functional independence in activities of daily living following the intervention. Both forms of treatment had the same therapeutic objectives, and both groups of stroke victims exhibited motor improvements. This demonstrates that visual biofeedback with a virtual reality program can achieve significant results in neurological rehabilitation and may be adopted as a resource in physical therapy. It is likely that a longer adaptation and execution period with the Wii Fit® could lead to even more significant results.
Thus, the Wii Fit® program provides positive results in physiotherapeutic rehabilitation and constitutes a further resource for treatment, as this interactive, fun resource may allow greater motivation during physical therapy sessions. Nonetheless, conventional physical therapy maintains its importance, as the group submitted to this type of treatment also achieved a significant improvement in the aspects evaluated in the present study.
A recent study reported that traditional physical therapy can be boring, which lowers motivation and reduces adherence to treatment, thereby providing limited benefits to patients with balance disorders22). Thus, the aim of the present study was to train balance using the Wii Balance Board in patients with acquired encephalopathy. The sample was made up of 11 men and six women with a mean age of 47.3 ± 17.8 years and chronicity of the condition ranging from 10 to 19 months. The patients were trained in 20 one-hour sessions. Assessments were performed using the Berg Balance Scale. The present study demonstrates that such training is viable, safe, and potentially effective in enhancing balance in the standing position, suggesting that the Wii Balance Board is a safe, effective alternative for individuals with acquired encephalopathy. There is an increasing use of virtual exercises as a new physiotherapeutic resource, and the results of the present study demonstrate the high degree of acceptability on the part of patients regarding such exercises26).
Some limitations of the present study should be pointed out, especially with regard to sample size. The study was carried out with a convenience sample (patients from a specific physical therapy clinic) composed of only 20 individuals. Further studies should be conducted with a sample based on a specific sample calculation and patient follow-up to determine whether the benefits of the intervention are maintained over time.
Acknowledgments
We gratefully acknowledge the financial support from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and Coordenação de Aperfeiçoamento de pessoal de Nível Superior (CAPES).
References
- 1.Dean CM, Rissel C, Sharkey M, et al. : Exercise intervention to prevent falls and enhance mobility in community dwellers after stokes. BMC Neurol, 2009, 9: 38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mann L, Kleinpaul JF, Mota CB, et al. : Body balance and exercise: a systematic review. Motriz, 2009, 15: 713–722 [Google Scholar]
- 3.Carvalho AC, Vanderlei LC, Bofi TC, et al. : Project hemiplegia: a model of group physical tehrapy of chronic hemiplegic patients. Arq Cienc Saude, 2007, 14: 161–168 [Google Scholar]
- 4.Soares AV, Hochmuller AC, Silva P, et al. : Biofeedback for training of standing balance in post-stroke hemiparetic patients: a preliminary study. Fisioter Pesqui, 2009, 16: 132–136 [Google Scholar]
- 5.Gomes BM, Nardoni GC, Lopes PG, et al. : The effect of global postural reeducation technique in a hemiparetic stroke patient. Acta Fisiatr, 2006, 13: 103–108 [Google Scholar]
- 6.Nordin E, Rosendahl E, Olsson LL: Timed Up & Go Test: Reliability in older people dependent in activities of daily living. Phys Ther, 2006, 86: 646–655 [PubMed] [Google Scholar]
- 7.Cruz KC, Diogo MJ: Evaluation the quality of life in elderly with stroke: a exploratory and transversal study. Acta Paul Enferm, 2009, 22: 666–672 [Google Scholar]
- 8.Kairy D: A postural adaptation test for stroke patients. Disabil Rehabil, 2003, 25: 127–135 [DOI] [PubMed] [Google Scholar]
- 9.Ryerson S, Byl NN, Brow DA, et al. : JM. Altered trunk position sense and relation to balance functions in people post-stroke. J Neurol Phys Ther, 2008, 32: 14–20 [DOI] [PubMed] [Google Scholar]
- 10.Walker C, Brouwer B: Culham. EG. Use of visual feedback in retraining balance following acute stroke. Phys Ther, 2000, 80: 886–895 [PubMed] [Google Scholar]
- 11.Berg KO, Wood-Dauphinee SL, Williams JI, et al. : Measuring balance in the elderly: validation of an instrument. Can J Public Health, 1992, 83: S7–S11 [PubMed] [Google Scholar]
- 12.Mackintosh SF, Hill KD, Dodd KJ, et al. : Balance score and a history of falls in hospital predict recurrent falls in the 6 months following stroke rehabilitation. Arch Phys Med Rehabil, 2006, 87: 1583–1589 [DOI] [PubMed] [Google Scholar]
- 13.Horak FB, Henry SM, Shumway-Cook A: Postural perturbations: new insights for treatment of balance disorders. Phys Ther, 1997, 77: 517–533 [DOI] [PubMed] [Google Scholar]
- 14.Podsiadlo D, Richardson S: The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc, 1991, 39: 142–148 [DOI] [PubMed] [Google Scholar]
- 15.Hamilton BB, Laughlin JA, Fiedler RC, et al. : Interrater reliability of the 7-level Functional Independence Measure (FIM). Scand J Rehabil Med, 1994, 26: 115–119 [PubMed] [Google Scholar]
- 16.Winter DA: Human balance and posture control during standing and walking. Gait Posture, 1995, 3: 193–214 [Google Scholar]
- 17.Crosbie JH, Lennon S, Basford JR, et al. : Virtual reality in stroke rehabilitation: still more virtual than real. Disabil Rehabil, 2007, 29: 1139–1146 [DOI] [PubMed] [Google Scholar]
- 18.Geiger RA, Allen JB, O'Keefe J, et al. : Balance and mobility following stroke: effects of physical therapy interventions with an without biofeedback/forceplate training. Phys Ther, 2001, 81: 995–1005 [PubMed] [Google Scholar]
- 19.Srivastava A, Taly AB, Gupta A, et al. : T. Post-stroke balance training: role of force platform with visual feedback technique. J Neurol Sci, 2009, 287: 89–93 [DOI] [PubMed] [Google Scholar]
- 20.Clark RA, Bryant AL, Pua Y, et al. : Validity and reliability of the Nintendo Wii Balance Board for assessment of standing balance. Gait Posture, 2010, 31: 307–310 [DOI] [PubMed] [Google Scholar]
- 21.McManus JA, Craig AM, Langhorne P, et al. : Does behaviour modification offect post-stroke risk factor control. Clin Rehabil, 2009, 23: 99–105 [DOI] [PubMed] [Google Scholar]
- 22.Yalon-Chamovitz S, Weiss PL: Virtual reality as a leisure activity for young adults with physical and intellectual disabilities. Res Dev Disabil, 2008, 29: 273–287 [DOI] [PubMed] [Google Scholar]
- 23.Shih CH, Shih CT, Chu CL: Assisting people with multiple disabilities actively correct abnormal standing posture with a Nintendo Wii Balance Board through controlling environmental stimulation. Res Dev Disabil, 2010, 31: 936–942 [DOI] [PubMed] [Google Scholar]
- 24.Barclay-Gooddark R, Stevenson TJ, Poluha W, et al. : Force platform Feedback for standing training after stroke. Cochrane Database Syst Rev, 2004, 18: CD004129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Celnik P, Webster B, Glasser DM, et al. : Effects of action observation on physical training after stroke. Stroke, 2008, 39: 1814–1820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gil-Gómez JA, Lloréns R, Alcañiz M, et al. : Effectiveness of a Wii balance board-based system (eBaViR) for balance rehabilitation: a pilot randomized clinical trial in patients with acquired brain injury. J Neuroeng Rehabil, 2011, 8: 30 [DOI] [PMC free article] [PubMed] [Google Scholar]