Abstract
BACKGROUND
Using regulatory focus theory, an intervention of daily weight loss-sustaining messages was developed and tested for acceptability, feasibility, and efficacy on helping people sustain weight loss.
METHODS
Participants (n = 120) were randomized to a promotion, prevention, or an attention-control text message group after completion of a weight loss program. Participants completed baseline assessments, and reported their weight at 1 and 3 months postbaseline.
RESULTS
Participants found the message content and intervention acceptable and valuable. A minimum of one message per day delivered at approximately 8:00 am was deemed the optimal delivery time and frequency. The sustained weight loss rate at month 3 for the control, promotion, and prevention groups was 90%, 95%, and 100%, respectively. Medium-to-large effects were observed for the promotion and prevention groups at month 1 and for prevention at month 3 relative to controls. The mean weight loss for promotion and prevention was 15 pounds, compared with 10 in the controls at month 3.
CONCLUSION
A clinically significant decrease in mean weight, higher rate of sustained weight loss, and medium-to-large effects on sustained weight loss occurred in the promotion and prevention interventions. Tools such as this text message-based intervention that are constructed and guided by evidence-based content and theoretical constructs show promise in helping people sustain healthy behaviors that can lead to improved health outcomes.
Keywords: Behavior change, Informatics, mHealth, Mobile health, Obesity, SMS, Text messaging, Weight loss
Obesity is a serious problem affecting one third of Americans,1 and is associated with multiple chronic diseases.2 Many people with obesity are successful at initial weight loss, but only 1 in 6 successfully sustain weight loss.3 Due to low cost and ubiquity of mobile phones,4 health care communicated through mobile technology, “mHealth,” may be able to serve as an effective medium to reach individuals directly and facilitate and motivate weight loss behaviors. mHealth has the potential to serve as a platform to quickly deliver information directly to people across geographic boundaries with content targeted to their weight loss needs that can serve as cues to action; targeted health information and cues to action are strategies to encourage change and sustain healthy behaviors.5,6
These characteristics of mHealth make it an ideal tool to aid in chronic illness management and maintenance of healthy behaviors such as weight loss. Preliminary studies on smoking, diabetes management, and weight loss initiation suggest that one such mHealth tool, text messaging, has positive short-term behavioral and clinical outcomes.7–10 However, in order to leverage mHealth as a tool to promote behavior change, we must understand how to deliver targeted information, appropriate frequency and timing of delivery, how much to deliver, and most importantly, provide relevant content that motivates and promotes self-regulation to sustain progress towards a goal.
Regulatory focus theory contends that people use 2 kinds of strategies to work toward goals: approach-based (promotion) or avoidance-based (prevention).11,12 Approach-based strategies promote success to reach a goal, while avoidance-based strategies prevent failure to reach a goal. The approach that people tend to habitually use is known as their regulatory focus. Although individuals use both strategies, some goals are viewed more favorably when the strategy matches the individual’s preference of promotion or prevention. This match increases the likelihood to feel motivated to initiate and sustain behavior change.13
The purpose was to evaluate the acceptability, feasibility, and efficacy of daily text messages using regulatory focus theory to help individuals sustain weight loss. We hypothesized that participants randomized to either a promotion- or prevention-framed weight loss message intervention group would have an increased likelihood of sustained weight loss compared with a general health message group.
METHODS
Study Design
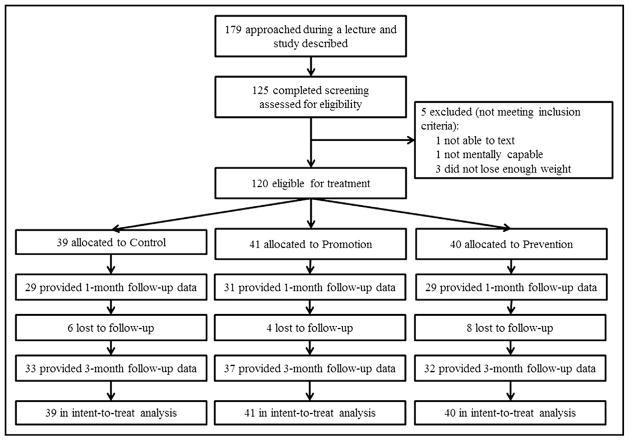
We conducted an exploratory randomized controlled trial using mixed methods, with data collected at baseline, and 1 month and 3 months post baseline. Permuted block randomization with a block size of 3 was used by the research coordinator to assign 120 participants to 1 of the 3 following message intervention groups: promotion-framed (n = 41), prevention-famed (n = 40), or general health message control group (n = 39; see Figure). Effect sizes specific to text message-based interventions and sustained weight loss were unknown. Therefore, a primary focus of this exploratory study was to estimate effect sizes for text message-based interventions. A sample size of 120 (40 per arm) provided a reasonable sample size, accounting for attrition, to explore treatment effects on sustained weight loss and to estimate true effect sizes for planning future research.14
Figure 1.
The primary outcomes were acceptability, defined as the perceived usefulness of the intervention; feasibility, defined as the ability to automatically transmit daily weight loss-sustaining messages that people would read; and sustained weight loss. With Duke University institutional review board approval, clients who received treatment at a residential weight loss management program that provides education, practical behavioral strategies, and ongoing support to make long-term changes, the Duke Diet and Fitness Center (DFC), participated in this study.
Participants
We recruited participants during a final self-management class at the DFC; those interested and who met the inclusion criteria self-selected to stay after class. For eligibility, individuals had to own a mobile phone, be able to receive text messages, and have lost 5% of their body weight since entering the DFC. Participants who signed an informed consent were oriented to the study, and completed baseline surveys. Participants were excluded if they were not mentally capable.
Interventions and Attention-Control
Participants received a daily message for 30 days following the weight loss program. Messages were set in a queue and automatically delivered from a Web-based software program daily at 8:00 am in participants’ respective time zones.15 The software program created a message delivery log and we checked it daily to ensure appropriate message delivery. Participants in the intervention groups received messages that targeted regular physical activity,16,17 a low-calorie healthy diet,18 and monitoring of body weight16,19,20; behaviors needed to sustain weight loss.16–20 Messages in the promotion-framed intervention group focused on promoting success and rewarding oneself, while prevention-framed messages focused on preventing failure and avoiding temptations.
Message creation, framing, and software development are reported in a pilot study.15 To eliminate the possible confounders of simply receiving a daily message regardless of content and the novelty effect of technology, participants randomized to the control group received general health messages over a standard-of-care control group.
Procedures and Measures
At baseline, we collected height, weight, demographic characteristics, text message use, and regulatory focus through the Regulatory Focus Questionnaire.21 At 1 and 3 months post baseline, participants self-reported their weight to the researcher via text message. Following the 3-month self-report of weight, participants received $30 for participation. Additionally, following the intervention at 1 month post baseline, participants were asked through an e-mail to undergo a telephone interview to discuss the perceived usefulness of and their attitudes toward the intervention and message content,22 technical difficulties and barriers, and how often they read the messages for intervention fidelity.23 We followed-up to nonresponders with a telephone call. With participants’ permission, interviews were recorded and transcribed for analysis.
The Regulatory Focus Questionnaire,21 an 11-item 2-factor scale with established reliability and validity, was used to determine whether participants were innately promotion or prevention. Item scores range from −2 to +2. Positive scores suggest promotion preference and negative scores suggest prevention.
The primary efficacy outcome was sustained weight loss, expressed as a dichotomous outcome at each time point (0 = not sustained, 1 = sustained). This outcome was determined using self-reported weight at each assessment point. In accordance with the American College of Sports Medicine,24 sustaining weight loss was defined as a change of ≤5 pounds or <3% change in weight following a weight loss program. The accuracy of self-reported weight has been demonstrated in Internet-based weight loss programs and has been shown to be comparable with observed weight and significantly correlated at 0 and 6 months (r = 0.996 and 0.996, respectively).25
Data Analyses
Statistical analyses were performed using SAS Version 9.3 (SAS Institute Inc., Cary, NC). Nondirectional statistical tests were performed, with the significance level set at .05 due to the exploratory nature of the study. Nonparametric methods were applied as needed when assumptions were not met.
Baseline Analyses
Descriptive statistics were used to summarize demographic characteristics. Chi-squared and Kruskal-Wallis tests were used to evaluate between-group baseline differences and to identify covariates.
Primary Efficacy Analyses
Sustaining weight loss was analyzed by examining both intent-to-treat cases and evaluable cases only. For the intent-to-treat analysis, all participants randomized to an intervention were analyzed according to the intervention to which they were assigned regardless of adherence or completion. For the evaluable case analysis, only data that were reported by participants were analyzed. Intervention effects on sustaining weight loss were examined using 2 × 3 Fisher’s exact tests at months 1 and 3, followed by a priori 2 × 2 Fisher’s exact test pairwise comparisons.
For the intent-to-treat analyses, missing data were handled by imputing predicted weights based on the individual’s estimated trajectory of weight. Predicted values were derived from the random coefficients regression conducted to evaluate weight change. The imputed score was used to determine the absence/presence of sustained weight loss.
Secondary Efficacy Analyses
Between-treatment differences in the trajectory of weight at baseline, month 1, and month 3 were examined using a random coefficients regression model. The fixed effects were group, time, and group-by-time, while random effects were participants and participants-by-time. A priori contrasts evaluated treatment differences at each assessment. Unadjusted and adjusted means derived from the trajectory model were calculated.
Feasibility and Acceptability Analyses
Content analysis and descriptive statistics were used to examine the feasibility and acceptability of the interventions. Interview data were collected until the point of saturation (no new information obtained) and analyzed using content analysis, a data reduction technique, to look for recurring themes in the interviews using ATLAS Ti Version 7 (Scientific Software Development, Berlin, Germany). Using 2 reviewers for inter-rater reliability, the content analysis involved dividing text into segments of information and the classification of patterns into code segments. Inferences made from the codes were collapsed into themes.26
RESULTS
Baseline Characteristics
We recruited 120 participants from May 2011 to February 2012 (Figure). Most participants were white (94%), college educated (81%), and financially stable (80%). A majority was female (59%), currently working (58%), and almost half were married (48%). The mean weight was 247.5 (SD = 61.8) pounds and mean body mass index was 38.1 (SD 7.8). Significant group differences in baseline characteristics were not observed (P >.05; Table 1). The sample was comparable with the DFC population with regard to weight (M = 248.1, SD = 72.7), age (M = 52.0, SD = 15.5), and sex (56% female).
Table 1.
Baseline Characteristics
| Characteristic | Control (n = 39) | Promotion (n = 41) | Prevention (n = 40) | P-Value |
|---|---|---|---|---|
| Weight in lbs. (mean ± SD) | 239.6 ± 50.4 | 250.8 ± 67.8 | 252.3 ± 65.6 | .76 |
| BMI (mean ± SD) | 37.3 ± 6.3 | 38.6 ± 8.6 | 38.4 ± 8.4 | .92 |
| Age, in years (mean ± SD) | 54.8 ± 15.9 | 51.0 ± 12.9 | 54.3 ± 15.5 | .21 |
| Number in household (mean ± SD) | 1.8 ± 0.7 | 2.0 ± 0.8 | 1.9 ± 0.7 | .62 |
| Sex (n, % female) | 25 (64%) | 26 (63%) | 20 (50%) | .35 |
| Race (n, % white) | 37 (95%) | 36 (88%) | 40 (100%) | .06 |
| Ethnicity (n, % Hispanic/Latino) | 4 (11%) | 3 (7%) | 3 (8%) | .80 |
| College degree or greater (n, %) | 32 (82%) | 31 (78%) | 34 (85%) | .69 |
| Married or partnered (n, %) | 18 (46%) | 19 (48%) | 20 (50%) | .94 |
| Currently working (n, %) | 20 (53%) | 22 (56%) | 25 (64%) | .58 |
| Financially stable (n, %) | 32 (82%) | 31 (78%) | 32 (80%) | .88 |
| Regulatory focus (mean ± SD) | 0.30 ± 0.87 | 0.16 ± 0.74 | 0.25 ± 0.93 | .87 |
BMI = body mass index.
For race, 1 = white and 0 = other. For ethnicity, 1 = Latino and 0 = not Latino. For education, 1 = college degree and 0 = less than a college degree. For work status, 1 = currently working, 0 = not currently working or retired. For financial status, 1 = financially well off, “After paying the bills, you still have money for the special things you want,” 0 = not having extra money. For marital status, 1 = married or partnered, 0 = divorced, widowed, or never married. Household was collapsed to 3 categories of 1, 2, and 3 or more people living in the household. Statistical methods were chi-squared tests for categorical measures and Kruskal-Wallis Tests due to non-normality issues for continuous variables.
Study Adherence
The 1-month postbaseline survey indicated that most participants (74%) read the messages immediately. Among those who didn’t, most read it when they got time (20%). Nearly all participants read the entire message when they received it (95%). Among the 120 randomized participants, 102 (85%) completed the study and reported their weight at month 3 (control 85%, promotion 90%, prevention 80%; Table 2). Attrition rates did not differ between groups at month 3 (Fisher’s, P = .43). Participants reported no problems with texting their self-reported weight.
Table 2.
Sustained Weight Loss and Reported Weight
| Assessment | Total | Control | Promotion | Prevention | P-Value |
|---|---|---|---|---|---|
| Sustained Weight Loss | |||||
| Intent-to-treat cases | |||||
| N | 120 | 39 | 41 | 40 | |
| Month 1 | 118 (98%) | 37 (95%) | 41 (100%) | 40 (100%) | .10a |
| Month 3 | 114 (95%) | 35 (90%) | 39 (95%) | 40 (100%) | .08b |
| Evaluable cases | |||||
| N | 89 | 29 | 31 | 29 | |
| Month 1 | 87 (98%) | 27 (93%) | 31 (100%) | 29 (100%) | .21a |
| N | 102 | 33 | 37 | 32 | |
| Month 3 | 96 (94%) | 29 (88%) | 35 (95%) | 32 (100%) | .13a |
| Reported weight, in lbs. | |||||
| Adjusted means (n) | 120 | 39 | 41 | 40 | .99a |
| Baseline | 247.5 ± 61.3 | 239.6 ± 50.6 | 250.2 ± 67.7 | 252.3 ± 64.7 | |
| Month 1 | 235.0 ± 59.4 | 232.2 ± 51.0 | 240.3 ± 64.8 | 242.5 ± 62.1 | |
| Month 3 | 234.3 ± 57.9 | 229.7 ± 52.1 | 235.3 ± 62.4 | 237.9 ± 59.8 | |
| Unadjusted means | |||||
| Baseline | 247.5 ± 61.8 | 239.6 ± 50.4 | 250.2 ± 68.2 | 252.3 ± 65.6 | |
| Month 1 | 235.0 ± 59.5 | 226.7 ± 47.9 | 234.2 ± 62.8 | 244.1 ± 66.7 | |
| Month 3 | 232.6 ± 60.1 | 227.2 ± 51.6 | 232.7 ± 64.3 | 237.9 ± 64.5 | |
N = Number of participants with weight data; sustained weight loss presented as n (%) of N. Reported weight summarized using the mean ± SD. Adjusted means are based on estimated trajectory scores at each assessment derived from the random coefficients regression model for repeated measurements, while the unadjusted means are provided for the evaluable cases. The P-values for sustained weight loss are based on the overall 2 × 3 Fisher’s exact test at each assessment, while the P-value for weight are for the group-by-time2 interactions evaluated using random coefficients regression models for repeated measurements. A priori pairwise comparisons results were as follows:
: control = promotion = prevention;
: promotion = control, prevention > control, promotion = prevention.
Primary Efficacy Outcome: Sustained Weight Loss
The rate of sustained weight loss exceeded 87% in all 3 groups at months 1 and 3 (Table 2) for both the intent-to-treat and evaluable cases. The lowest rate of sustained weight loss was observed in the control group. The intent-to-treat analysis indicated no significant group differences in sustained weight loss at month 1 (P = .10) or month 3 (P = .08). A priori comparisons demonstrated no significant differences in sustained weight loss between the groups in the intent-to-treat cases at month 1 (P >.05). The sustained weight loss rate in the prevention group, however, was significantly greater than that in controls at month 3 (P = .05), but the other groups did not differ (P >.05).
The evaluable cases analysis also indicated no significant group differences in sustained weight loss at month 1 (Fisher’s, P = .21) or month 3 (Fisher’s, P = .13). A priori comparisons demonstrated no significant differences in sustained weight loss between groups at month 1 or month 3 (Fisher’s, P >.05). Although the difference between prevention and control was not significant in the intent-to-treat analysis, the rate for prevention tended to be higher (100% vs 88%, P = .11). The smaller sizes in the evaluable case analyses likely reduced the statistical power of the tests.
Table 3 presents the intervention effect sizes for sustained weight loss based on pairwise comparisons for the intent-to-treat and evaluable cases. Cohen w effect sizes27 were used to evaluate the magnitude of difference and clinical significance of the findings. At month 1, medium effects of 0.33 or greater were observed between each active intervention and controls for the intent-to-treat and evaluable cases. Medium-to-large effects were demonstrated between the prevention and control groups at month 3 for the intent-to-treat (w = 0.48) and evaluable (w = 0.52) cases. The results indicate the clinical significance of the prevention intervention relative to the control condition.
Table 3.
Cohen w Effect Sizes for Sustained Weight Loss
| Pairwise Comparisons | Month 1 | Month 3 |
|---|---|---|
| Intent-to-treat | ||
| Promotion vs control | 0.33 | 0.21 |
| Prevention vs control | 0.33 | 0.48 |
| Promotion vs prevention | 0.00 | 0.32 |
| Evaluable cases | ||
| Promotion vs control | 0.39 | 0.24 |
| Prevention vs control | 0.39 | 0.52 |
| Promotion vs prevention | 0.00 | 0.33 |
Cohen w effects: 0.10 to 0.29 = small; 0.30 to 0.49 = medium; 0.50 or greater = large.
Secondary Efficacy Outcome: Self-Reported Weight
The trajectory analysis indicated a significant quadratic pattern of decrease in weight in all 3 groups for the intent-to-treat and evaluable cases (Table 2). However, significant group or group-by-treatment interaction effects were not demonstrated in either analysis. The results of the trajectory analysis for the intent-to-treat cases were as follows: linear time: P <.0001; quadratic time: P = .0002; group: P = .62; group-by-time: P = .70; group-by-time2: P = .99. Similar results were found for the evaluable cases: linear time: P <.0001; quadratic time: P = .0002; group: P = 0.60; group-by-time: P = 0.61; group-by-time2: P = 0.94.
The 3 groups did not differ significantly in weight at baseline, month 1, or month 3 (P >.05). The mean change in weight relative to baseline was not statistically significant at month 1 and month 3 (P >.05). However, at month 3, the controls lost, on average, 9.7 pounds (SD = 15.1), while the promotion and prevention groups lost, on average, 14.6 (SD = 16.6) and 15.3 (SD = 14.5) pounds, respectively.
Qualitative Analysis: Usefulness and Attitudes
Interviews were conducted until the point of saturation (n = 60) at 1 month post baseline and included those who may have dropped out by the 3-month postbaseline measure. Interviews indicated that the participants enjoyed receiving messages on their mobile phones. A majority (42; 91%) preferred receiving messages on their mobile phone due to accessibility and convenience, “because my cell phone is always on me.” Six major themes arose from the participants’ impression of the intervention (Table 4). The text messages served as a cue to action and helped them overcome barriers and “stay on track.”
Table 4.
Qualitative Themes and Subthemes (n = 60)
| Theme | Description | Verbatim Exemplars | |
|---|---|---|---|
| 1. | Cue to action | The intervention helped participants to stay focused, mindful, establish a daily routine, stay on track, feel motivated, and acted as a daily reminder for their weight loss program | “The day I received the messages I stopped exercise. I missed like 4 days because of my business. And I said you have to make the time. And I planned to continue and not stop.” |
| Overcome barriers | The intervention helped participants overcome barriers | “There were times you know when I would fall off plan and I would go back and scroll [through the messages]” | |
| 2. | Enjoyable | Participants liked the intervention and some reported missing the daily messages | “When I got home and started getting those messages from you, I got so fired up and that phone went beep-beep and I went shooting out of here every morning to see the message of the day, fabulous … to me that was the best!” |
| 3. | Useful | Participants felt the text message intervention was a useful tool for maintaining weight loss | “The usefulness of a daily reminder every morning, the bell goes off at some point, and you look at it and realize what you are doing.” |
| 4. | Importance of content | Participants would like a mix of content ranging from diet, exercise, monitoring, motivation, and behavioral strategies | “When I got the couple messages I guess you send on exercise, I wanted to you know go and exercise or I wanted to walk at least 3 or 4 times a week.” |
| Tailoring | Participants felt the content should be tailored to their needs | “I would want to tailor the messages to the things that I was struggling most with” | |
| Resource for information | Participants felt the messages served as a resource for diet and exercise information | “I don’t plan on going back to Duke for a while. So it’s kind of like, the texts are here, and I can just fall back on that” | |
| 5. | Support | The intervention was a support tool, added a connection to Duke, and made them feel they were paid attention to | “I love the idea of getting a text message every day, it was sort of like somebody out there cares” |
| 6. | Duration | Participants would like the weight loss intervention to be extended beyond 30 days | “I wish there was a way I could keep getting them” |
Almost all of the interviewed participants would like at least one message per day (n = 59; 98%), with over half (n = 37; 62%) reporting they would like up to 2 messages per day. Participants also spoke about how receiving a message in the morning (8:00 am) helped to keep them motivated for the day. Nineteen of the 60 participants specifically mentioned sharing the messages.
DISCUSSION
Findings for sustained weight loss indicated that the overall rate of sustained weight loss was 98% after 1 month and 95% after 3 months. A higher proportion of participants sustained their weight loss in the 2 active intervention groups when compared with the control condition. Clinically meaningful effects on sustained weight loss were observed for the promotion and prevention arms relative to controls after month 1. Interestingly, the effect of the prevention intervention further increased at month 3. Furthermore, the medium-to-large effects of 0.48 to 0.52 of the prevention arm at 3 months post baseline were greater than the reported effect sizes of 0.25 to 0.30 for weight loss in the published findings from Web-based interventions.28,29 Thus, the study provided evidence of the efficacy of the prevention and promotion text messages on sustained weight loss.
All 3 groups showed a significant decrease in weight, on average, over the 3 months. Although the change in weight was not statistically significant among the 3 interventions, the average weight loss in the promotion and prevention groups after 3 months was approximately 15 pounds, compared with 9.7 pounds in the controls. Taken together, these findings indicate a clinically significant reduction and maintenance of weight loss in the 2 active interventions, particularly prevention. The results are consistent with the literature, which suggests that prevention-framed messages may be better for people who are attempting to sustain healthy behaviors.30,31
Consistent with the literature, these findings demonstrate that text messaging is a feasible and acceptable mode for weight loss interventions.10,32 Most participants felt there was significant value in receiving text messages that promote weight loss-sustaining behaviors. According to participants, once a day at 8:00 am was deemed as the most appropriate frequency and timing because weight loss is a daily challenge, and it helped motivate them for the remainder of the day. The message framing between promotion and prevention did not impact the self-reported favorability or acceptability of the messages.
Limitations
Most participants were from an affluent and educated background, white non-Hispanic, and not representative of the general US population, which limits generalizability of the findings. The definition for sustaining weight loss was based upon a national guideline and research on weight loss at 12 months.24 This study examined weight loss 3 months post baseline after a 1-month intervention.
Baseline report of weight at the clinic may differ from self-report of weight at home. The accuracy of self-reported weight, however, has been demonstrated in Internet-based weight loss treatment programs and has been shown to be comparable with observed weight.25 Finally, although study noncompletion occurred, the 15% attrition rate is comparable with that reported for computer-based weight loss interventions.25
This exploratory study was designed to evaluate direction and magnitude of effects of the promotion and prevention interventions on sustained weight loss. With a sample size of 40 per arm, an effect size of 0.48 or greater (Cohen w values representing high-medium to large effects) was needed to achieve at least 80% statistical power to detect true difference in proportions using 2 × 2 Fisher’s exact tests with a 2-tailed significance level at .05. Interestingly, the prevention versus control comparison indicated a 10% absolute difference in sustained weight loss rates in the intent-to-treat cases, which corresponded to an effect size of 0.48. This clinically significant effect also was statistically significant. Although a larger effect of 0.52 was demonstrated in the evaluable cases, the 12% absolute differences in the prevention and control groups was not statistically significant due to the smaller samples. Thus, the study lacked adequate power for the overall comparison of the 3 interventions and for the a priori comparisons of sustained weight loss when small-to-medium effects were observed.
Implications for Practice
With obesity reaching epidemic proportions and the high relapse rate of those who fail to sustain weight loss, an increase of up to 10% of people who are able to sustain weight loss through such an intervention could have considerable benefit. Furthermore, tools such as this text message weight loss intervention have the potential to be implemented in the clinical setting as a low-cost way to extend weight loss programs.
CONCLUSION
Communication technologies such as mobile phones may serve as an effective medium to deliver affordable health promotion and disease prevention care to an array of people due to their ubiquity and penetration into people’s everyday lives. However, emerging and promising technologies must be matched with content that successfully resonates and motivates people to change and sustain behaviors. Our findings demonstrate that it is not only feasible and acceptable to use text messaging as a health care delivery platform, but that participants find it useful and were overall positive towards this mHealth intervention. Markedly, there was a clinically significant decrease in mean weight, and a greater proportion of people sustained weight loss in the promotion and prevention message groups. Notably, effect sizes demonstrated a medium-to-large effect of the promotion and prevention interventions on sustaining weight loss.
CLINICAL SIGNIFICANCE.
This mHealth intervention was feasible, acceptable, and efficacious on sustaining recent weight loss.
Medium-to-large effects were observed for the promotion and prevention message groups at month 1 and for the prevention group at month 3.
Month 3 mean weight loss for the intervention groups was 15 pounds, compared with 10 in the controls.
A daily text message at 8:00 am was at the optimal delivery time and frequency to sustain weight loss.
Acknowledgments
Funding: This research was supported by a Duke University Health System Information Technology Fellowship, a National Research Service Award (1F31 NR012599) from the National Institutes of Health (NIH), National Institute of Nursing Research, and a Department of Veterans Affairs Health Services Research and Development Office of Academic Affiliations nursing postdoctoral research award (TPP-21-021), to the first author. HBB was supported by a Research Career Scientist award from the Department of Veterans Affairs Office of Health Services Research and Development RCS-08-027. The content is solely the responsibility of the authors and does not necessarily represent the official views of Duke University, the NIH, or the US Department of Veterans Affairs.
We thank William Tatum, Jeffrey Hess, and Lucie Knapp for their support.
Footnotes
Conflict of interest: None.
Authorship: All work herein is original. All authors meet the criteria for authorship, including acceptance of responsibility for the scientific content of the manuscript.
References
- 1.National Center for Health Statistics. Health, United States, 2008 with Chartbook. Hyattsville, MD: Centers for Disease Control and Prevention; 2009. [Google Scholar]
- 2.Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88. doi: 10.1186/1471-2458-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kraschnewski JL, Boan J, Esposito J, et al. Long-term weight loss maintenance in the United States. Int J Obes (Lond) 2010;34(11):1644–1654. doi: 10.1038/ijo.2010.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.CTIA Wireless Association. CTIA Semi-Annual Wireless Industry Survey. Washington, DC: 2012. Available at: http://ctia.org/media/press/body.cfm/prid/2216. [Google Scholar]
- 5.Dijkstra A, De Vries H. The development of computer-generated tailored interventions. Patient Educ Couns. 1999;36:193–203. doi: 10.1016/s0738-3991(98)00135-9. [DOI] [PubMed] [Google Scholar]
- 6.Kreuter MW, Wray RJ. Tailored and targeted health communication: strategies for enhancing information relevance. Am J Health Behav. 2003;27(Suppl 3):S227–S232. doi: 10.5993/ajhb.27.1.s3.6. [DOI] [PubMed] [Google Scholar]
- 7.Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med. 2009;36(2):165–173. doi: 10.1016/j.amepre.2008.09.040. [DOI] [PubMed] [Google Scholar]
- 8.Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemed J E Health. 2009;15(3):231–240. doi: 10.1089/tmj.2008.0099. [DOI] [PubMed] [Google Scholar]
- 9.Lim MS, Hocking JS, Hellard ME, Aitken CK. SMS STI: a review of the uses of mobile phone text messaging in sexual health. Int J STD AIDS. 2008;19(5):287–290. doi: 10.1258/ijsa.2007.007264. [DOI] [PubMed] [Google Scholar]
- 10.Patrick K, Raab F, Adams MA, et al. A text message-based intervention for weight loss: randomized controlled trial. J Med Internet Res. 2009;11(1):e1. doi: 10.2196/jmir.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higgins ET. Self-discrepancy: a theory relating self and affect. Psychol Rev. 1987;94(3):319–340. [PubMed] [Google Scholar]
- 12.Higgins ET. Making a good decision: value from fit. Am Psychol. 2000;55(11):1217–1230. [PubMed] [Google Scholar]
- 13.Spiegel S, Grant-Pillow H, Higgins ET. How regulatory fit enhances motivational strength during goal pursuit. Eur J Soc Psychol. 2004;34(1):39–54. [Google Scholar]
- 14.Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage J. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry. 2006;63:484–489. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]
- 15.Shaw RJ, Bosworth HB, Hess JC, et al. Development of a theoretically driven mHealth short message service (SMS) application for sustaining weight loss. JMIR mHealth uHealth. 2013;1(1):e5. doi: 10.2196/mhealth.2343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baum JG, Clark HB, Sandler J. Preventing relapse in obesity through posttreatment maintenance systems: comparing the relative efficacy of two levels of therapist support. J Behav Med. 1991;14:287–302. doi: 10.1007/BF00845456. [DOI] [PubMed] [Google Scholar]
- 17.Schoeller DA, Shay K, Kushner RF. How much physical activity is needed to minimize weight gain in previously obese women? Am J Clin Nutr. 1997;66:551–556. doi: 10.1093/ajcn/66.3.551. [DOI] [PubMed] [Google Scholar]
- 18.Jeffery RW, Bjornson-Benson WM, Rosenthal BS, Lindquist RA, Kurth CL, Johnson SL. Correlates of weight loss and its maintenance over two years of follow-up among middle-ages men. Prev Med. 1984;13:155–168. doi: 10.1016/0091-7435(84)90048-3. [DOI] [PubMed] [Google Scholar]
- 19.Kramer FM, Jeffery RW, Forster JL, Snell MK. Long-term follow-up of behavioural treatment for obesity: patterns of weight gain among men and women. Int J Obes Relat Metab Disord. 1989;13:124–136. [PubMed] [Google Scholar]
- 20.Wadden TA, Letizia KA. Predictors of attrition and weight loss in patients treated by moderate and severe caloric restriction. In: Wadden TA, Itallie TB, editors. Treatment of the Seriously Obese Patient. New York: Guilford; 1992. pp. 383–410. [Google Scholar]
- 21.Higgins ET, Friedman RS, Harlow RE, Idson LC, Ayduk ON, Taylor A. Achievement orientations from subjective histories of success: promotion pride versus prevention pride. Eur J Soc Psychol. 2001;31(1):3–23. [Google Scholar]
- 22.Kreuter MW, Oswald DL, Bull FC, Clark EM. Are tailored health education materials always more effective than non-tailored materials. Health Educ Res. 2000;15(3):305–315. doi: 10.1093/her/15.3.305. [DOI] [PubMed] [Google Scholar]
- 23.Borrelli B, Sepinwall D, Ernst D, et al. A new tool to assess treatment fidelity and evaluation of treatment fidelity across 10 years of health behavior research. J Consult Clin Psychol. 2005;73(5):852–860. doi: 10.1037/0022-006X.73.5.852. [DOI] [PubMed] [Google Scholar]
- 24.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41(2):459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 25.Harvey-Berino J, Krukowski RA, Buzzell P, Ogden D, Skelly J, West DS. The accuracy of weight reported in a web-based obesity treatment program. Telemed J E Health. 2011;17(9):696–699. doi: 10.1089/tmj.2011.0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Neuendorf KA. The Content Analysis Guidebook. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 27.Braunstein JW. [Accessed July 12, 2012.];How to calculate effect size for dissertation students and researchers. 2007 Available at: http://www.researchconsultation.com/how-to-calculate-effect-size-help.asp.
- 28.Portnoy DB, Scott-Sheldon LA, Johnson BT, Carey MP. Computer-delivered interventions for health promotion and behavioral risk reduction: A meta-analysis of 75 randomized controlled trials, 1988–2007. Prev Med. 2009;47(1):3–16. doi: 10.1016/j.ypmed.2008.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Franz MJ, VanWormer JJ, Crain AL, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107(10):1755–1767. doi: 10.1016/j.jada.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 30.Fuglestad PT, Rothman AJ, Jeffery RW. Getting there and hanging on: the effect of regulatory focus on performance in smoking and weight loss interventions. Health Psychol. 2008;27(3 Suppl):S260–S270. doi: 10.1037/0278-6133.27.3(suppl.).s260. [DOI] [PubMed] [Google Scholar]
- 31.Kim Y. The role of regulatory focus in message framing in anti-smoking advertisements for adolescents. J Advert. 2006;35(1):115–143. [Google Scholar]
- 32.Shaw R, Bosworth H. Short message service (SMS) text messaging as an intervention medium for weight loss: a literature review. Health Informatics J. 2012;18(4):235–250. doi: 10.1177/1460458212442422. [DOI] [PMC free article] [PubMed] [Google Scholar]