Abstract
To date, existing studies focus largely on the economic detriments of malaria. However, if we are to create suitable incentives for larger-scale, more sustained anti-malaria efforts from a wider group of stakeholders, we need a much better understanding of the economic benefits of malaria reduction and elimination. Our report seeks to rectify this disjuncture by showing how attaining the funding needed to meet internationally agreed targets for malaria elimination would, on conservative assumptions, generate enormous economic improvements. We use a cost-benefit analysis anchored in Global Malaria Action Plan projections of malaria eradication based on fully met funding goals. By calculating the value of economic output accrued caused by work years saved and subtracting the costs of intervention, we find that malaria reduction and elimination during 2013–2035 has a 2013 net present value of US $208.6 billion.
Introduction
There is a long way to go in the fight against malaria.
This disease is a leading cause of death and ill-health in the developing world.1 According to the World Health Organization (WHO), there were more than 219 million cases of malaria in 2010, claiming 660,000 lives.1 Research by the Institute for Health Metrics and Evaluation suggests that the death toll could be much higher, at 1.2 million annually.2 Concentrated in the poorest regions of the world, notably sub-Saharan Africa, malaria not only exacts a heavy human toll in the areas where it is most prevalent but is also highly corrosive of the broader economic fabric of these regions. In the most heavily affected regions, malaria accounts for 40% of public health spending,3 sapping already-scarce resources and impeding long-term human capital formation.
Our study differs from previous investigations by seeking to measure the tangible economic gains that reducing the incidence of malaria would bring about, rather than focusing on economic detriments of malaria. Using the techniques of cost-benefit analysis, we covered all WHO regions to project the global economic benefits of combating malaria through to 2035. Findings from this study should help to clarify incentives for investment in malaria control and elimination based on business and public finance considerations.
Materials
A number of studies have sought to quantify the economic impact of malaria. Roughly speaking, they can be divided into four research strands.
The first strand uses statistics and econometrics to identify the impact of malaria on economic growth. McCarthy and others found that the negative growth impact of malaria exceeded 0.25% per annum for 25% of countries they studied, mainly those in sub-Saharan Africa, although the impact was significantly higher in the worst affected regions.4 Malaria reduces growth directly by incapacitating the workforce and indirectly through effects such as reduced labor mobility, less scope for specialization, and poorer skills matching.5 Gallup and Sachs found that malaria-intensive countries grew by 1.3% less per person per year during 1965–1990, in comparison with malaria-free countries with similar socioeconomic characteristics.6 Reductions in malaria were associated with higher economic growth in both studies.
The second strand analyzes the effects of malaria on human capital development, particularly educational outcomes. Malaria contracted during pregnancy can result in anemia, premature birth, and low birth weight, leading to reduced cognitive ability and physical development in children, which affect educational attainment in later life.6 An examination of the effects of malaria on female educational attainment in Paraguay and Sri Lanka found that every 10% decrease in malaria incidence leads to 0.1 years of additional schooling, and an increase in the chance of being literate of 1–2% points.7
The third strand of research uses surveys and site studies to assess the costs of preventing and treating malaria in particular locations. For example, site studies in Rwanda, Burkina Faso, Chad, and the Republic of the Congo found that a case of malaria in 1987 cost $1.83 in disease control and treatment and $8.01 in lost working time in 1987 US dollars.8
The fourth research strand evaluates the cost-effectiveness of various tools in the fight against malaria. Prevention programs such as insecticide-treated nets and indoor residual spraying cost between $11 and $34 per disability adjusted life year (DALY) saved in 2006 dollars,9 while treating an incidence of malaria costs between $5.84 and $30.26 (in 2009 dollars) depending on the complexity of the case.10
Although the existing literature illuminates the economic impact of malaria, it does not bring together the evidence around costs and benefits in a comprehensive way. To create incentives for greater anti-malaria efforts from a wider group of stakeholders at the national and international levels, we need a better understanding of the tangible economic benefits of investing in malaria control and elimination. This is the aim of our report. More specifically, if the funding needed to meet internationally agreed targets for malaria elimination were sustained, what would be the economic benefit of this investment?
Methods
The basic economic case for malaria eradication rests on the economic output that would be generated if individuals were not killed or incapacitated by malaria and they were therefore able to enter or remain in the productive workforce. Our approach is as follows. First, we estimate the numbers of work years saved as a result of interventions to eradicate malaria. We base our estimates on the difference between a business as usual (counterfactual) scenario of malaria incidences and an intervention scenario of decreasing malaria incidences anchored in a long-term blueprint for eradication set out in the Roll Back Malaria (RBM) Global Malaria Action Plan (GMAP), first published in 2008. Historical experience of the impact of malaria guides our conversion from incidences into years that would otherwise be lost because of death or disability. We take account of factors such as limitations of anti-malaria coverage, treatment success rates, and the recurrence of the disease. Second, we attach an economic value to these saved years using the output per person of working age in the different regions, incorporating forecasts of future productivity growth. Third, we subtract the costs of anti-malaria interventions to derive a net benefit figure for each year. Finally, we sum all of the net benefits over a 22-year period and discount this figure to express the result in present-value terms.
Outlining the trajectory of malaria incidences in response to intervention.
Potential time paths of malaria reduction in response to intervention are identified in the GMAP. Aspiring to eliminate malaria globally by approximately 2030, the plan outlines three stages of malaria elimination: scale-up, control, and elimination.
The GMAP (2008) assumed that the scale-up stage would last for two years during 2008–2010. By the end of the scale-up stage, a utilization rate of 80% is reached, meaning that 80% of the population at risk uses locally appropriate malaria prevention methods. In reality, longstanding logistical problems in the countries most affected by malaria will mean that the scale-up lasts longer than expected. The worst-affected countries have struggled to make progress in scaling up health interventions, with ownership rates of insecticide-treated nets falling below 50% in countries such as Chad and the Democratic Republic of the Congo despite 10 years of concerted international efforts.11 The high risk of reversals in coverage can also slow progress. For example, previous assumptions about distributing one net for every two persons have left odd-numbered households short of nets,12 and procurement problems have reversed use rates even in fast-improving countries such as Rwanda.13 In our analysis, we assume that the scale-up stage will reach the 80% utilization threshold in 2015 instead of 2010 to reflect slower-than-expected progress. In the years preceding 2015, we assume a utilization rate of 60%, which is a level consistent with penetration of home management of malaria across heavily affected countries.14
Regions where malaria prevalence is less than 5 cases/1,000 persons (including the Americas, Europe, and Western Pacific throughout the period of our analysis) are considered to be in the elimination stage and are expected to see small annual reductions in malaria incidences of 0–0.5%. We assume an average annual reduction of 0.25%.
Regions more heavily affected by malaria, namely Africa, Southeast Asia, and the Eastern Mediterranean, enter the control stage after the scale-up stage. According to modeling by Cibulskis and recent country experiences, an 80% utilization rate can reduce malaria incidences by 75% over a five-year period.15 We therefore assume that Africa, Southeast Asia, and the Eastern Mediterranean will experience a 75% linear reduction in incidences during 2015–2020.
The rapid reduction of malaria incidences during the control stage places Southeast Asia and the Eastern Mediterranean in the elimination stage by 2020. Africa, however, will remain heavily affected by malaria, and remains in the control phase throughout our analysis period. Only in 2035 will Africa reach the 5/1,000 benchmark necessary for transition into the elimination stage.
Outlining the counterfactual scenarios.
We also construct counterfactual regional trajectories to estimate future malaria incidences in the absence of intervention programs such as those envisaged in the GMAP. We assume that each WHO region continues to see a decrease in malaria incidences at a rate largely consistent with that experienced during 2005–2010. This decrease equates to an annual decrease of 1.7–2.2% for Africa and Southeast Asia during 2010–2035.
Malaria conditions worsened in Eastern Mediterranean during 2005–2010; there was a 5.6% annual increase in malaria incidences. In our model, we assume that the backwards slide will continue at this rate until 2015. From there, we apply a 1.7% annual decrease rate in malaria incidences for the Eastern Mediterranean, which is consistent with the world average during 2005–2010.
In regions in which malaria is not a significant concern, we assume an annual reduction of 0.25% for the counterfactual scenario, which is consistent with the assumption behind the intervention scenario.
Next, we derive from these assumed future incidences the number of work years saved from malaria.
Deriving work years saved.
The WHO uses the DALY, a standard measure combining the number of years of life lost because of disease-related mortality and healthy years lost because of disability in the case of survival, to measure the historic burden of malaria. We convert our assumed future incidences (in the intervention and counterfactual scenarios) into DALYs by using the ratio between incidences in 2004 (GMAP) and DALYs in 2004 (WHO, the most recent data available). (Over the period of our analysis, we therefore assume that this ratio remains constant, as does the constituent balance between years lost because of mortality and years lost because of disability.) Subtracting the DALYs in the intervention scenario from the DALYs in the counterfactual scenario gives the total number of DALYs averted in each year through intervention. We then make three adjustments to convert them from DALYs to work years saved from malaria.
First, we apply an intervention coverage rate of 60% in the scale-up stage and 80% thereafter. This adjustment, which adds considerable conservatism to assumptions of the GMAP, reflects the fact that not all malaria cases can be reached. Under the counterfactual, we assume that, without more active intervention, the coverage rate remains 60% throughout the period.
Second, we apply an intervention success rate of 50% which reflects that mosquitoes can develop resistance to insecticides and that drugs may be ineffective counterfeits or otherwise substandard.16 This rate again embodies a more conservative stance than that of the GMAP (Table 1).
Table 1.
Success rate by intervention for combating malaria*
| Intervention method | Success rate, % |
|---|---|
| Long-lasting insecticidal nets | 50 |
| Indoor residual spraying | 60 |
| Intermittent preventive treatment in pregnancy | 56 |
Source: Global Malaria Action Plan (2008).
Third, we apply an individual recurrence rate of 40%. This rate reflects that the same person may contract malaria more than once in the same year, leading to a number of malaria incidences significantly higher than the number of persons affected. To prevent an overestimation of the benefits of malaria intervention, we assume 2.5 cases of malaria/person/year. According to WHO, a person with malaria can have ≤ 5 cases in a year. Thus, we average the minimum number of annual malaria cases (0) with the maximum of 5 cases to get an average of 2.5 cases/person/year. The individual recurrence rate of 40% is derived by dividing 1 person by 2.5 average annual cases.
Identifying economic benefits.
Next, we identify the appropriate economic value of the individual work years saved. At the simplest level, this value can be measured in terms of the economic output of each person of working age: real gross domestic product (GDP) divided by the working-age population of a region. Productivity will grow over time as populations get healthier, especially in developing economies where there is also significant potential for economic catch-up. To reflect this finding, we expand GDP per person of working age by the average productivity growth forecast over the period up to 2035 at five-year intervals (Table 2).
Table 2.
GDP per person of working age and projected productivity growth*
| GDP per working age person (US $, 2009 constant prices) | 2010 level | 2010–2015 growth, % | 2015–2020 growth, % | 2020–2025 growth, % | 2025–2030 growth, % |
|---|---|---|---|---|---|
| Africa | 3,176 | 1.45 | 2.40 | 2.19 | 2.47 |
| The Americas | 44,428 | 2.85 | 3.00 | 2.65 | 2.56 |
| Southeast Asia | 3,171 | 3.43 | 3.50 | 3.59 | 3.73 |
| Europe | 46,319 | 1.40 | 2.63 | 2.51 | 2.23 |
| Eastern Mediterranean | 10,726 | 1.78 | 2.51 | 2.39 | 2.35 |
| Western Pacific | 13,020 | 4.31 | 4.72 | 4.64 | 4.84 |
Source: United Nations Population Division, Oxford Economics, and authors' analysis. GDP = gross domestic product.
We calculate productivity growth using the formula
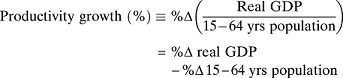 |
To arrive at the net benefits of combating malaria, we must also allow for costs of malaria intervention. According to the profile of intervention costs set out by GMAP, there are four components to anti-malaria expenditure: prevention, case management (diagnosis and treatment), program costs (such as monitoring and evaluation, training, and infrastructure), and research and development expenses. In our model, the net benefits are calculated by deducting the GMAP costs (updated by RBM in May 2012) from the gross benefits (increased economic output).
The net economic benefits of combating malaria occur over a 22-year period (during 2013–2035) into the future. Because far-off benefits are usually perceived as less valuable than those occurring today or in the near future, we discount the future net benefits of malaria intervention to their value today. By discounting and accumulating the future benefits in each year, we obtain the net present value (NPV) of malaria interventions
Here, t represents time and n = 21, reflecting the fact that the benefits are spread over 22 years (with 2013 representing year 0) in our analysis. The term r represents the annual discount rate: the degree to which society values current benefits over benefits received one year later. A high discount rate indicates that a society has strong preferences for benefits now, with the perception of future benefits decaying rapidly with time. For public investment projects, it is standard to adopt a lower discount rate, reflecting the societal nature of the benefits, the wider spillover effects, and the long-term nature of the investment. We adopt a 3% discount rate, consistent with that of similar studies, such as those by Hanson K and others, 2004; Laxminarayan 2004; and Goodman C and others, 2000.17–19
Results
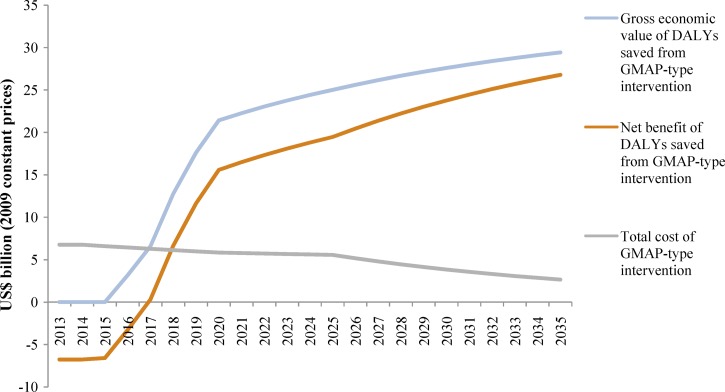
Using the methods above, our study estimates the economic output gains from tackling malaria to be US $208.6 billion in net present value terms. The profile of net benefits is heavily front-loaded: although the cost of intervention is broadly flat, the annual gross and net benefits increase rapidly in the near term (Table 3) because of greater incidence reduction (Figure 1).
Table 3.
Cost of malaria intervention*
Source: Global Malaria Action Plan (2008) and Roll Back Malaria (2012).
Authors' estimates. Cost needed for 2015 has been revised upwards by RBM in May 2012 from $5,837 million envisioned in the GMAP (2008) to $6,597 million in the Resource Mobilization Strategy for the 2012–2015 Phase of Implementation of the GMAP. This revision reflects a 13% increase. We inflate GMAP (2008) estimates for 2020 and 2025 by the same degree to reflect that GMAP (2008) cost estimates may have been too low. For the years between these periods, we interpolate annual costs in a linear fashion for each five-year interval. As for the period between 2025 and 2030, we extrapolate costs using the average annual change during the period between 2020 and 2025.
Figure 1.
Profile of cost and benefit of malaria elimination (2013–2035). DALYs = disability adjusted life years; GMAP = Global Malaria Action Plan.
Discussion
The compelling economic case for fighting malaria underscores the social and ethical merits of eradicating this disease. Malaria eradication would confer much wider development benefits than the economic output quantified in our analysis and do much to alleviate poverty in the developing world. At the household level, families in developing regions often need to divert spending towards medicine at the expense of other basic needs. Reducing the disease incidence can therefore increase disposable income and consumption. At the national level, lightening the load of malaria would mitigate the strains on public health systems and free up resources for social improvements. In Rwanda, 19% of the recurrent budget was directed to malaria in recent years.20 Public healthcare spending in Tanzania on malaria equated to 3.4% of the GDP in 2010.21 If this expenditure could have been directed to education, the total education budget of this country would have increased by 65%.21
Businesses also stand to benefit from a malaria-free world. The most straightforward benefits arise from lower costs of hiring, reductions in absenteeism, and increases in employee productivity. In a global survey of 8,000 business leaders from more than 100 countries, more than 20% reported that malaria harms their business. Among respondents from sub-Saharan Africa, this share was 72%, and approximately 40% reported serious detriments.22 Malaria eradication can foster the market development, entrepreneurship, and investment needed to accelerate economic growth in some of the poorest regions of the world.
Collaboration between international agencies, businesses, and governments will be crucial in overcoming infrastructural and institutional constraints in many of the malaria-burdened regions. Cross-sector collaboration is also needed for development of innovative financing models that will be required to increase malaria expenditure in the face of constrained government spending. Malaria bonds provide one example. An innovative financing mechanism still on the drawing board, the objective of malaria bonds is to raise funds for disease control from private investors, particularly the up-front investment needed to kick-start malaria control schemes. Issued and repaid by governments (and international donors), funds raised from such schemes would be allocated to organizations implementing malaria interventions on a pay-for-performance basis, with the aim that improved efficiencies in program delivery would deliver a premium to investors.23
Establishing the economic case for malaria elimination offers a practical first step to unlocking investment opportunities. The use of economic arguments also extends well beyond the realm of economists. Epidemiologists, ethnographers, and many others could deploy economic arguments to galvanize greater anti-malaria efforts. We hope that greater awareness of the economic case for eradication will better serve the humanitarian imperative of ridding the world of malaria.
Footnotes
Authors' addresses: Mark Purdy, Matthew Robinson, Kuangyi Wei, and David Rublin, Accenture Institute for High Performance, London EC3M 3BD, UK, E-mails: mark.purdy@accenture.com, matthew.c.robinson@accenture.com, kuangyi.wei@accenture.com, and david.rublin@accenture.com.
References
- 1.World Health Organization . Malaria Fact Sheet. 2012. http://www.who.int/mediacentre/factsheets/fs094/en/ Available at. Accessed January 10, 2013. [Google Scholar]
- 2.Murray CJ, Rosenfeld LC, Lim SS, Andrews KG, Foreman KJ, Haring D, Fullman N, Naghavi M, Lozano R, Lopez AD. Global malaria mortality between 1980 and 2010: a systematic analysis. Lancet. 2012;379:413–431. doi: 10.1016/S0140-6736(12)60034-8. [DOI] [PubMed] [Google Scholar]
- 3.Attaran A, Narasimhan V. Roll back malaria? The scarcity of international aid for malaria control. Malar J. 2003;2:8. doi: 10.1186/1475-2875-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCarthy FD, Wolf H, Wu Y. The Growth Costs of Malaria. 2000. http://www.nber.org/papers/w7541.pdf National Bureau of Economic Research working paper 7541. Available at. Accessed April 14, 2013. [Google Scholar]
- 5.Sachs J, Malaney P. The economic and social burden of malaria. Nature. 2002;415:680–685. doi: 10.1038/415680a. [DOI] [PubMed] [Google Scholar]
- 6.Gallup JL, Sachs JD. The economic burden of malaria. Am J Trop Med Hyg. 2001;64:85–96. doi: 10.4269/ajtmh.2001.64.85. [DOI] [PubMed] [Google Scholar]
- 7.Lucas AM. Malaria eradication and educational attainment: evidence from Paraguay and Sri Lanka. Am Economic J–Applied Economics. 2010;2:46–71. doi: 10.1257/app.2.2.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shepard DS, Ettling MB, Brinkmann U, Sauerborn R. The economic cost of malaria in Africa. Trop Med Parasitol. 1991;423:199–203. [PubMed] [Google Scholar]
- 9.Breman J, Mills A, Snow RW, Mulligan J-A, Lengeler C, Mendis K, Sharp B, Morel C, Marchesini P, White NJ, Steketee RW, Doumbo OK. Conquering Malaria. Disease Control Priorities in Developing Countries. Second edition. New York: Oxford University Press; 2006. [Google Scholar]
- 10.White MT, Conteh L, Cibulskis R, Ghani AC. Costs and cost-effectiveness of malaria control interventions–a systematic review. Malar J. 2011;10:337. doi: 10.1186/1475-2875-10-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sabot O, Moonen B, Yamey G, Jones A, Cohen J, Santos A, Ward A, Reidy M, Higbie M. Maintaining the Gains in Global Malaria Control. 2011. http://globalhealthsciences.ucsf.edu/sites/default/files/content/ghg/e2pi-maintaining-the-gains.pdf Clinton Health Access Initiative. Available at. Accessed May 10, 2013. [Google Scholar]
- 12.Erskine M, Lynch M. Quantification for Universal Coverage. 2011. http://www.alma2015.org/sites/default/files/docs/alma_unicef_quant_021411.pdf African Leaders Malaria Alliance. Available at. Accessed May 10, 2013. [Google Scholar]
- 13.Clinton Health Access Initiative . Maintaining the Gains in Global Malaria Control. 2011. http://globalhealthsciences.ucsf.edu/sites/default/files/content/ghg/e2pi-maintaining-the-gains-country-briefs.pdf Available at. Accessed May 10, 2013. [Google Scholar]
- 14.Ajayi IO, Browne EM, Garshong B, Bateganya F, Yusuf B, Agyei-Baffour P, Doamekpor L, Balyeku A, Munguti K, Cousens S, Pagnoni F. Feasibility and acceptability of artemisinin-based combination therapy for the home management of malaria in four African sites. Malar J. 2008;7:6. doi: 10.1186/1475-2875-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cibulskis R. WHO Informal Consultation on Global Malaria Control and Elimination: A Technical Review. Geneva: World Health Organization; 2008. [Google Scholar]
- 16.Nayyar GML, Breman JG, Newton PN, Herrington J. Poor-quality antimalarial drugs in Southeast Asia and sub-Saharan Africa. Lancet Infect Dis. 2012;12:488–496. doi: 10.1016/S1473-3099(12)70064-6. [DOI] [PubMed] [Google Scholar]
- 17.Hanson K, Goodman C, Lines J, Meek S, Bradley D, Mills A. The Economics of Malaria Control Interventions. 2004. http://whqlibdoc.who.int/publications/2004/2940286159.pdf The Global Forum for Health Research, January 2004. Available at. Accessed May 10, 2013. [Google Scholar]
- 18.Laxminarayan R. Act now or later? Economics of malaria resistance. Am J Trop Med Hyg. 2004;71:187–195. [PubMed] [Google Scholar]
- 19.Goodman C, Coleman P, Mills A. Economic Analysis of Malaria Control in Sub-Saharan Africa. 2009. http://www.givewell.org/files/DWDA%202009/Analysis/Economic%20Analysis%20of%20Malaria%20Control%20in%20Sub-Saharan%20Africa.pdf The Global Forum for Health Research, May 2000. Available at. Accessed May 10, 2013. [DOI] [PubMed] [Google Scholar]
- 20.United Kingdom Department for International Development . Malaria: Burden and Interventions. 2010. http://www.dfid.gov.uk/Documents/prd/malaria-evidence-paper.pdf Available at. Accessed May 14, 2013. [Google Scholar]
- 21.United Republic of Tanzania Ministry of Finance . Government Budget for Financial year 2011–2012. Calculation Based on the Total Education Budget of Financial Year 2010–2011. 2011. http://nexus.som.yale.edu/ph-tanzania/sites/nexus.som.yale.edu.ph-tanzania/files/imce_imagepool/Tz_Budget_2011_2012.pdf Available at. Accessed May 14, 2013. [Google Scholar]
- 22.World Economic Forum . Business and Malaria: A Neglected Threat. 2006. https://members.weforum.org/pdf/MalariaReport.pdf Available at. Accessed October 1, 2012. [Google Scholar]
- 23.World Health Organization . World Malaria Report 2011. Geneva: World Health Organization; 2011. http://www.who.int/malaria/world_malaria_report_2011/9789241564403_eng.pdf Available at. Accessed September 6, 2012. [Google Scholar]