Abstract
Background
Information on trauma-related deaths in low and middle income countries is limited but needed to target public health interventions. Data from a health and demographic surveillance system (HDSS) were examined to characterise such deaths in rural western Kenya.
Methods And Findings
Verbal autopsy data were analysed. Of 11,147 adult deaths between 2003 and 2008, 447 (4%) were attributed to trauma; 71% of these were in males. Trauma contributed 17% of all deaths in males 15 to 24 years; on a population basis mortality rates were greatest in persons over 65 years. Intentional causes accounted for a higher proportion of male than female deaths (RR 2.04, 1.37-3.04) and a higher proportion of deaths of those aged 15 to 65 than older people. Main causes in males were assaults (n=79, 25%) and road traffic injuries (n=47, 15%); and falls for females (n=17, 13%). A significantly greater proportion of deaths from poisoning (RR 5.0, 2.7-9.4) and assault (RR 1.8, 1.2-2.6) occurred among regular consumers of alcohol than among non-regular drinkers. In multivariate analysis, males had a 4-fold higher risk of death from trauma than females (Adjusted Relative Risk; ARR 4.0; 95% CI 1.7-9.4); risk of a trauma death rose with age, with the elderly at 7-fold higher risk (ARR 7.3, 1.1-49.2). Absence of care was the strongest predictor of trauma death (ARR 12.2, 9.4-15.8). Trauma-related deaths were higher among regular alcohol drinkers (ARR 1.5, 1.1-1.9) compared with non-regular drinkers.
Conclusions
While trauma accounts for a small proportion of deaths in this rural area with a high prevalence of HIV, TB and malaria, preventive interventions such as improved road safety, home safety strategies for the elderly, and curbing harmful use of alcohol, are available and could help diminish this burden. Improvements in systems to record underlying causes of death from trauma are required.
Introduction
Globally, injuries account for one quarter of all deaths among people aged 15 to 49 years [1,2]. The public health implications of injuries are well documented in high income countries but have been raised as an important concern also in rural areas of low and middle income countries (LMIC) [3]. Causes of trauma-related death align with gender. Worldwide, injury accounts for approximately half of all mortality among young males aged 10 to 24 years [2]. Available data in LMIC suggest males are at greatest risk of all injury-related deaths, with violence and road traffic injuries (RTI) predominating [3]. Less frequent trauma-related deaths, such as suicide and burns, are also important causes of concern [3,4], and under-documentation of trauma associated with gender-related interpersonal violence has been raised as a public health priority [5].
By 2030, RTI are projected to be the fourth leading cause of death globally [6]. However, the pattern of trauma-related deaths is less well documented in LMIC making it difficult to understand needs or develop and strengthen public health interventions [7-9]. In South Africa, examination of deaths in a rural demographic surveillance site found that injury was responsible for 9% of deaths across all ages, with the predominating causes being homicide, RTI, and suicides [10]. Other types of traumatic injuries in impoverished communities involve living, working and travelling in less safe environments, with few preventative interventions, and minimal access to quality treatment and rehabilitation [11]. In Kenya, as in many other countries of sub-Saharan Africa (SSA), trauma is thought to be an important contributor to premature death in rural communities [12]. However, documentation of trauma deaths outside hospital settings is often limited. Better understanding of the scope and cause of trauma-related deaths in rural areas of SSA is possible through the use of verbal autopsy conducted in health and demographic surveillance systems (HDSS). In western Kenya, the Kenya Medical Research Institute (KEMRI)/US Centers for Disease Control and Prevention (CDC) HDSS provides such an opportunity [13]. This paper reports on deaths attributed to injuries, and poisonings, identified through verbal autopsy, and examines risk factors associated with these deaths.
Materials and Methods
Study site and population
The population is described in detail elsewhere [13-15]. Briefly, the study site includes 385 villages spread over a 700km2 area along the shores of Lake Victoria, Nyanza Province, western Kenya. The area is rural and includes Asembo, Wagai, and parts of Yala Divisions and from 2008, Karemo Division. The population approximating 220,000 persons, is mostly of the Luo ethnic group, with families living in compounds comprised of a separate house for each wife and her children. The majority of adults are subsistence farmers.
Health and Demographic Surveillance System (HDSS)
The HDSS site is registered as an International Network for the Demographic Evaluation of Populations and Their Health in Developing Countries INDEPTH partner [13]. Households are geo-spatially located, and the population is registered with each person receiving a unique identification number allowing record linkage. A household census takes place three times a year to capture data on births, deaths, and in and out migration. These census data are used to provide mid-year denominators per five year age group, stratified by gender and area. Identified deaths are followed up by trained field staff to validate and record events around each death using the standard verbal autopsy (VA) methodology. Data are gathered from households on items that provide an indication of wealth status which are then used to calculate a weighted average through multiple correspondence analysis (MCA) [13]. This facilitates the calculation of a composite score ranking of households by quintiles from one (poorest) to five (least poor).
Verbal autopsy (VA)
VA is conducted at least one month after death using a standardised WHO questionnaire, endorsed by INDEPTH, to gather information on symptoms and care seeking prior to death [16]. Information on risk factors such as alcohol use is gathered in addition to socio-demographic, educational and occupational data. A narrative section of the questionnaire facilitates collection of additional information on events surrounding death. Adult members of the household, preferably the spouse of the deceased, are identified as the most appropriate informants and provide consent for participation. VA forms are reviewed independently by two clinical officers and a single, probable cause of death is assigned, as previously described [17]. In 2007, Sample Vital Registration with Verbal Autopsy (SAVVY) was adopted to strengthen monitoring and measurement [18]. More detailed description on use of VA to examine mortality profiles is published elsewhere [13,15].
Data preparation and analyses
Adult (15 years and above) data were extracted from the HDSS database for years 2003 to 2008; deaths were grouped into ‘trauma-related’ and ‘non-trauma-related’ using the main diagnosis group code, with underlying cause further examined. Causes of death were categorized under assault, RTI, poisoning, suicide, burns, animal bites/stings, sudden death and ‘other’ trauma-related death with a separate non-specific category for ‘other injuries/poisoning’. Each death was assigned to just one cause of death category. Suicides were recorded within the suicide category irrespective of how the person died (for example a person who drowned themselves would be included in the suicide category only). The category for poisonings refers to accidental only; intentional cases fall under either suicide or assault according to cause. Due to a large number of trauma-related deaths falling into the generic ‘other injury/poisoning’ category, the research team examined the underlying cause of death, enabling re-categorisation of 21 deaths. Three new categories were also created - ‘falls’, ‘drowning’ and ‘other injuries (specified cause)’. Adjustment was made to ensure intentional deaths were included within assault if inflicted on the victim, or suicide if self-inflicted. Deaths were then grouped into intentional (assault and suicide) and unintentional (all other groups) causes.
Free text was abstracted to provide contextual information on events surrounding trauma-related deaths. Social characteristics, generated through the HDSS, include marital status (ever married, married at death) and school (primary, secondary) attendance. MCA quintiles were aggregated into MCA1-2 (poorest) and MCA3-5 (less poor). Measures for alcohol consumption and for being drunk were dichotomised into regular drinkers (persons reported to have consumed alcohol at least weekly) and non-regular drinkers (occasional drinkers who consumed alcohol less than once a week, including non-drinkers). More detailed breakdown on the frequency of drinking was not possible as four of the six verbal autopsy surveillance years had limited data on patterns of alcohol consumption.
Analyses were performed using SPSS v17 and EpiInfo Stat Calc. Age at death was categorised and trauma-related mortality rates per 100,000 population were estimated by year, gender and age group using mid-year population estimates from the HDSS census, with 95% confidence intervals calculated. chi-square (χ2) tests were used for categorical comparisons. Differences between groups were determined using Pearson's χ2 test, with the level of significance set at 0.05 or less. Median age (with interquartile range; IQR) and Mann Whitney U was used to compare male and female ages for each specific type of trauma-related death. Multivariate analysis, using Poisson regression, with adjusted RR, 95% CI, and wald χ2, was conducted to identify factors associated with trauma-related deaths; all variables included in univariate analyses were entered into the model. Among duplicate variables presented in univariate analyses, we selected the variable showing strongest association for example, for education - attended primary school; for where died – categorical died at home or elsewhere; for marital status – married at death. Variables thus entered into the model were age, gender, socio-economic status, attended primary school, year of death, married at death, regular alcohol drinker, received care before death, and died at home.
Ethical considerations
The HDSS protocol and consent procedures, including surveillance and VA was approved by KEMRI (#1801) and CDC Institutional Review Boards (#3308), and is updated annually.
Written informed consent for all compound members to participate in the HDSS activities was provided by compound heads. Any individual could refuse to participate at any time. Named data were securely stored in a MS-SQL database and only authorized data personnel had access rights. Data sets used by scientists for analysis were stripped of names to protect confidentiality.
Results
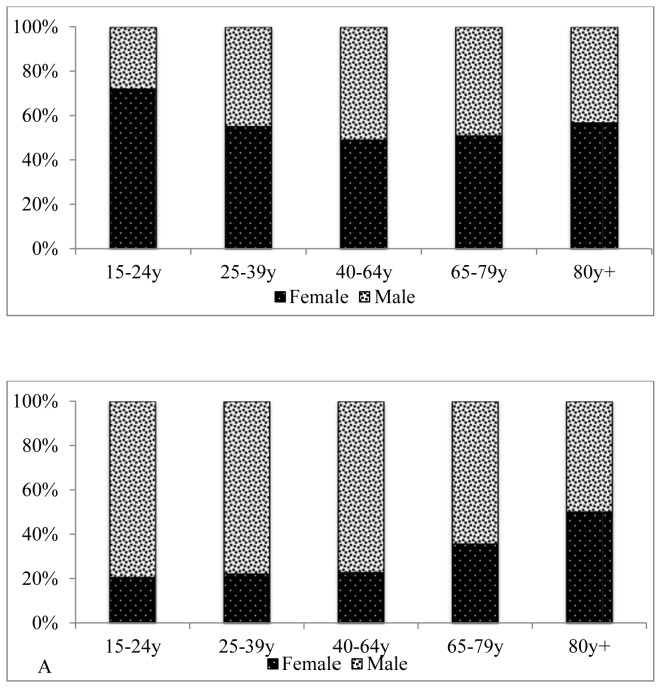
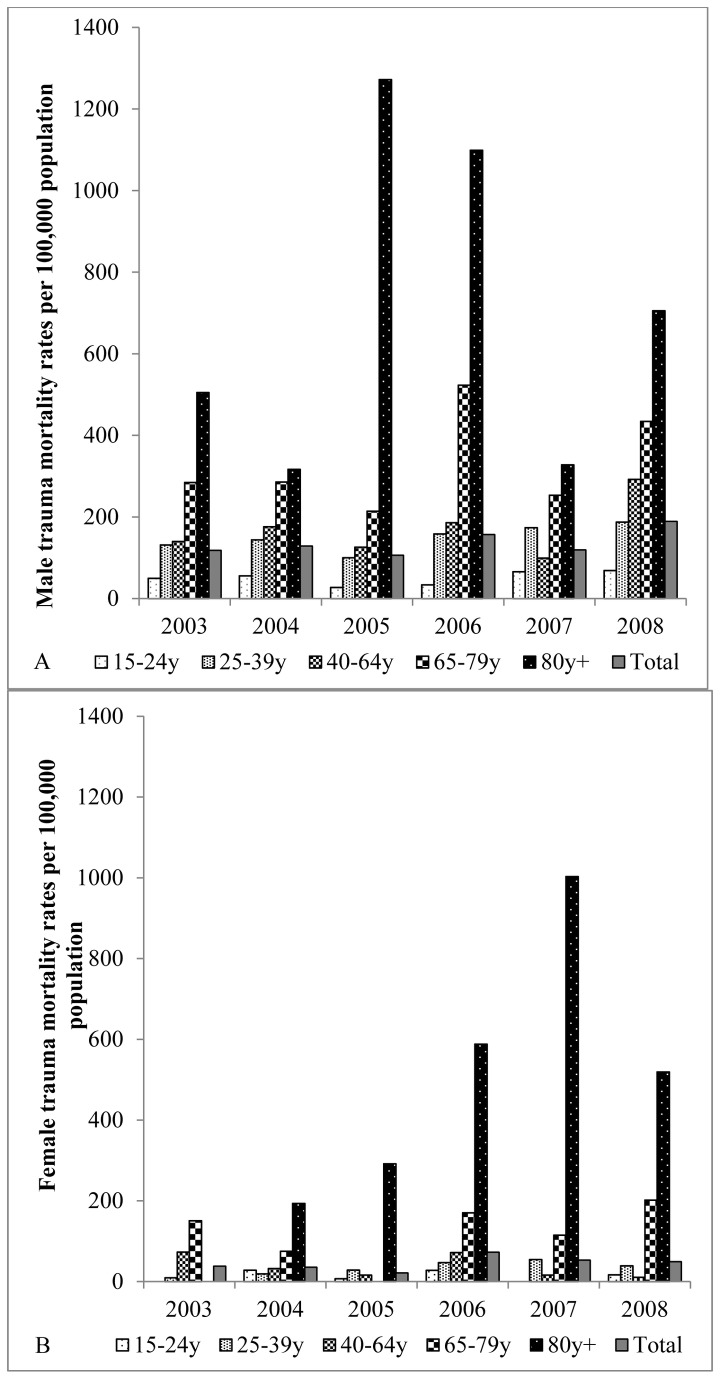
Of 11,147 adult deaths recorded between 2003 and 2008, 447 (4% overall, or 2% of female and 6% of male deaths) were attributed to trauma (Tables 1, 2). The proportion of trauma related deaths increased from 2.5% to 5.9% between 2003 and 2008 (test for linear trend 35.5; p < 0.001). Among males, trauma-related deaths were proportionately higher than other causes among adolescents and young adult deaths, with 16% of trauma deaths in persons aged 15-24 years, compared with 5% for all other causes of death (Table 1). In this age group 17% (50/292) of all deaths were trauma related. Among females, trauma-related deaths were proportionately higher than other causes among older aged adult deaths. Except among deaths occurring in the very elderly, trauma deaths were 2 to 4-fold higher among males with, for example, close to four out of every five trauma deaths in the 15 to 24 year old age group being male (Figure 1; Table 3). Overall, mortality rates illustrated a 2 to 5-fold higher burden of trauma-related deaths among males compared with females by age category across the years of study (Figure 2). On a population basis, rates of trauma-related deaths were highest in older persons aged 65 years and above, for both males and females, reflecting the relatively high contribution of trauma amongst the elderly (Figure 2).
Table 1. Comparison between characteristics of trauma-related and non-trauma-related deaths among adult males.
| Attributes | N | Category | Trauma (%) | Non-trauma (%) | Total (%) | RR (95% CI) | χ2 ; p value |
|---|---|---|---|---|---|---|---|
| Year1 | 5256 | 2003 | 39 (12.2) | 869 (17.6) | 908 (17.3) | Reference | 32.7;<0.001 |
| 2004 | 43 (13.5) | 819 (16.6) | 862 (16.4) | 1.08 (0.87-1.34) | |||
| 2005 | 36 (11.3) | 829 (16.8) | 865 (16.5) | 0.98 (0.77-1.25) | |||
| 2006 | 54 (16.9) | 781 (15.8) | 835 (15.9) | 1.23 (1.03-1.47) | |||
| 2007 | 42 (13.2) | 607 (12.3) | 649 (12.3) | 1.26 (1.01-1.57) | |||
| 2008 | 105 (32.9) | 1032 (20.9) | 1137 (21.6) | 1.34 (1.21-1.50) | |||
| Age | 5256 | 15 to 24 | 50 (15.7) | 242 (4.9) | 292 (5.6) | Reference | 67.4;<0.001 |
| 25 to 39 | 84 (26.3) | 1403(28.4) | 1487 (28.3) | 0.74 (0.64-0.84) | |||
| 40 to 64 | 95 (29.8) | 1796 (36.4) | 1891 (36.0) | 0.74 (0.66-0.84) | |||
| 65 to 79 | 61 (19.1) | 975 (19.7) | 1036 (19.7) | 0.69 (0.58-0.81) | |||
| 80+ | 29 (9.1) | 521 (10.6) | 550 (10.5) | 0.54 (0.40-0.72) | |||
| Area | 5256 | Gem | 159 (49.8) | 2726 (55.2) | 2885 (54.9) | Reference | 8.6; 0.013 |
| Asembo | 124 (38.9) | 1858 (37.6) | 1982 (37.7) | 1.08 (0.94-1.24) | |||
| Karemo | 36 (11.3) | 353 (7.2) | 389 (7.4) | 1.61 (1.18-2.20) | |||
| SES2 | 4977 | MCA1-2 | 114 (37.3) | 1994 (42.7) | 2108 (42.4) | Reference | 3.5; 0.062 |
| MCA3-5 | 192 (62.7) | 2677 (57.3) | 2869 (57.6) | 1.10 (1.00-1.20) | |||
| Ever | 4866 | No | 61 (19.2) | 367 (8.1) | 428 (8.8) | Reference | 45.8;<0.001 |
| married | Yes | 257 (80.8) | 4181 (91.9) | 4438 (91.2) | 0.88 (0.83-0.93) | ||
| Married at death | 4868 | No | 113 (35.5) | 1567 (34.4) | 1680 (34.5) | Reference | 0.16; 0.69 |
| Yes | 205 (64.5) | 2983 (65.6) | 3188 (65.5) | 0.98 (0.90-1.07) | |||
| Attend primary3 | 3336 | No | 42 (19.5) | 703 (22.5) | 745 (22.3) | Reference | 1.04; 0.31 |
| Yes | 173 (80.5) | 2418 (77.5) | 2591 (77.7) | 1.04 (0.97-1.11) | |||
| Attend secondary | 4687 | No | 241 (80.3) | 3644 (83.1) | 3885 (82.9) | Reference | 1.48; 0.22 |
| Yes | 59 (19.7) | 743 (16.9) | 802 (17.1) | 1.16 (0.92-1.47) | |||
| Any care pre-death | 4804 | No | 147 (52.7) | 204 (4.5) | 351 (7.3) | Reference | 901;<0.001 |
| Yes | 132 (47.3) | 4321 (95.5) | 4453 (92.7) | 0.50 (0.44-0.56) | |||
| Hospital pre-death | 4439 | No | 37 (28.0) | 1608 (37.3) | 1645 (37.1) | Reference | 4.75; 0.03 |
| Yes | 95 (72.0) | 2699 (62.7) | 2794 (62.9) | 1.15 (1.03-1.28) | |||
| Place died | 4873 | Home | 174 (54.9) | 3814 (83.7) | 3988 (81.8) | Reference | 750; <0.001 |
| HFtravel | 10 (3.2) | 53 (1.2) | 63 (1.3) | 3.97 (2.05-7.67) | |||
| HF | 24 (7.6) | 261 (5.7) | 285 (5.8) | 1.89 (1.28-2.80) | |||
| Hospital | 33 (10.4) | 394 (8.6) | 427 (8.8) | 1.70 (1.23-2.36) | |||
| Other | 76 (24.0) | 34 (0.7) | 110 (2.3) | 34.4 (23.4-50.5) | |||
| Regular4 alcohol | 4727 | No | 185 (62.5) | 3180 (71.8) | 3365 (71.2) | Reference | 11.6; 0.001 |
| Yes | 111 (37.5) | 1251 (28.2) | 1362 (28.8) | 1.33 (1.14-1.55) | |||
| Regularly4 drunk | 4236 | No | 185 (77.1) | 3247 (81.3) | 3432 (81.0) | Reference | 2.56; 0.11 |
| Yes | 55 (22.9) | 749 (18.7) | 804 (19.0) | 1.22 (0.96-1.56) |
1 Data collection in Karemo commenced in 2008 2.SES: socio-economic status measured using multiple correspondence analysis in order to calcuate wealth quintiles (1=poorest 5=least poor) 3.This question not consistently asked 4. Reportedly occurred at least weekly.
Table 2. Comparison between characteristics of trauma-related and non-trauma-related deaths among adult females.
| Attributes | N | Category | Trauma (%) | Non-trauma (%) | Total (%) | RR (95% CI) | χ2 ; p value |
|---|---|---|---|---|---|---|---|
| Year1 | 5891 | 2003 | 16 (12.5) | 965 (16.7) | 981 (16.7) | Reference | 18.9; 0.002 |
| 2004 | 15 (11.7) | 968 (16.8) | 983 (16.7) | 0.97 (0.67-1.39) | |||
| 2005 | 9 (7.0) | 936 (16.2) | 945 (16.0) | 0.73 (0.43-1.24) | |||
| 2006 | 31 (24.2) | 929 (16.1) | 960 (16.3) | 1.35 (1.09-1.66) | |||
| 2007 | 23 (18.0) | 792 (13.7) | 815 (13.8) | 1.31 (1.00-1.71) | |||
| 2008 | 34 (26.6) | 1173 (20.4) | 1207 (20.5) | 1.24 (1.02-1.51) | |||
| Age | 5891 | 15 to 24 | 13 (10.2) | 626 (10.9) | 639 (10.8) | Reference | 25.8;<0.001 |
| 25 to 39 | 24 (18.8) | 1721 (29.9) | 1745 (29.6) | 0.89 (0.70-1.12) | |||
| 40 to 64 | 28 (21.9) | 1722 (29.9) | 1750 (29.7) | 0.93 (0.76-1.15) | |||
| 65 to 79 | 34 (26.6) | 1010 (17.5) | 1044 (17.7) | 1.17 (0.98-1.40) | |||
| 80+ | 29 (22.7) | 684 (11.9) | 713 (12.1) | 1.32 (1.07-1.63) | |||
| Area | 5891 | Gem | 69 (53.9) | 3136 (54.4) | 3205 (54.4) | Reference | 0.19; 0.91 |
| Asembo | 49 (38.3) | 2234 (38.8) | 2283 (38.8) | 1.00 (0.80-1.24) | |||
| Karemo | 10 (7.8) | 393 (6.8) | 403 (6.8) | 1.14 (0.63-2.04) | |||
| SES2 | 5513 | MCA1-2 | 66 (55.9) | 2850 (52.8) | 2916 (52.9) | Reference | 0.45;0.50 |
| MCA3-5 | 52 (44.1) | 2545 (47.2) | 2597 (47.1) | 0.93 (0.76-1.15) | |||
| Ever | 5389 | No | 13 (10.2) | 296 (5.6) | 309 (5.7) | Reference | 4.74;0.03 |
| married | Yes | 115 (89.8) | 4965 (94.4) | 5080 (94.3) | 0.95 (0.90-1.01) | ||
| Married at death | 5391 | No | 93 (72.7) | 3382 (64.3) | 3475 (64.5) | Reference | 3.85; 0.05 |
| Yes | 35 (27.3) | 1881 (35.7) | 1916 (35.5) | 0.77 (0.58-1.02) | |||
| Attend primary3 | 3982 | No | 60 (59.4) | 1867 (48.1) | 1927 (48.4) | Reference | 5.03; 0.025 |
| Yes | 41 (40.6) | 2014 (51.9) | 2055 (51.6) | 0.78 (0.62-0.99) | |||
| Attend secondary | 5095 | No | 114 (92.7) | 4569 (91.9) | 4683 (91.9) | Reference | 0.10; 0.75 |
| Yes | 9 (7.3) | 403 (8.1) | 412 (8.1) | 0.90 (0.48-1.71) | |||
| Any care pre-death | 5368 | No | 44 (37.9) | 215 (4.1) | 351 (4.8) | Reference | 283; <0.001 |
| Yes | 72 (62.1) | 5037 (95.9) | 5109 (95.2) | 0.65 (0.56-0.75) | |||
| Hospital pre-death | 5080 | No | 33 (45.8) | 1993 (39.8) | 2026 (39.9) | Reference | 1.08;0.3 |
| Yes | 39 (54.2) | 3015 (60.2) | 3054 (60.1) | 0.90 (0.73-1.11) | |||
| Place died | 5398 | Home | 88 (68.8) | 4452 (84.5) | 4540 (84.1) | Reference | 243; <0.001 |
| HFtravel | 1 (0.8) | 75 (1.4) | 76 (1.4) | 0.68 (0.10-4.82) | |||
| HF | 11 (8.6) | 284 (5.4) | 295 (5.5) | 1.85 (1.05-3.27) | |||
| Hospital | 15 (11.7) | 444 (8.4) | 459 (8.5) | 1.61 (1.00-2.59) | |||
| Other | 13 (10.2) | 15 (0.3) | 28 (0.5) | 38.3 (18.7-78.4) | |||
| Regular4 alcohol | 5261 | No | 110 (90.9) | 4734 (92.1) | 4844 (92.1) | Reference | 0.23; 0.63 |
| Yes | 11 (9.1) | 406 (7.9) | 417 (7.9) | 1.15 (0.65-2.04) | |||
| Regularly4 drunk | 5055 | No | 108 (94.7) | 4710 (95.3) | 4818 (95.3) | Reference | 0.09; 0.77 |
| Yes | 6 (5.3) | 231 (4.7) | 237 (4.7) | 1.13 (0.51-2.48) |
1 Data collection in Karemo commenced in 2008 2.SES: socio-economic status measured using multiple correspondence analysis in order to calcuate wealth quintiles (1=poorest 5=least poor) 3.This question not consistently asked 4. Reportedly occurred at least weekly.
Figure 1. Trauma (panel A) and non-trauma (panel B) deaths among adults aged 15 years and above by age and gender, 2003 to 2008.
Table 3. Characteristics of trauma-related deaths in adults 15 years and above by gender.
| Attributes | N | Category | Female (%) | Male (%) | Total (%) | RRmale (95% CI) | χ2; p value |
|---|---|---|---|---|---|---|---|
| Year1 | 447 | 2003 | 16 (12.5) | 39 (12.2) | 55 (12.3) | Reference | 7.05; 0.22 |
| 2004 | 15 (11.7) | 43 (13.5) | 58 (13.0) | 1.08 (0.71-1.65) | |||
| 2005 | 9 (7.0) | 36 (11.3) | 45 (10.1) | 1.33 (0.75-2.37) | |||
| 2006 | 31 (24.2) | 54 (16.9) | 85 (19.0) | 0.88 (0.67-1.15) | |||
| 2007 | 23 (18.0) | 42 (13.2) | 65 (14.5) | 0.88 (0.63-1.23) | |||
| 2008 | 34 (26.6) | 105 (32.9) | 139 (31.1) | 1.07 (0.87-1.33) | |||
| Age | 447 | 15 to 24 | 13 (10.2) | 50 (15.7) | 63 (14.1) | Reference | 21.6;<0.001 |
| 25 to 39 | 24 (18.8) | 84 (26.3) | 108 (24.2) | 0.97 (0.74-1.27) | |||
| 40 to 64 | 28 (21.9) | 95 (29.8) | 123 (27.5) | 0.96 (0.76-1.22) | |||
| 65 to 79 | 34 (26.6) | 61 (19.1) | 95 (21.3) | 0.76 (0.60-0.97) | |||
| 80+ | 29 (22.7) | 29 (9.1) | 58 (13.0) | 0.53 (0.37-0.76) | |||
| Area | 447 | Gem | 69 (53.9) | 159 (49.8) | 228 (51.0) | Reference | 1.37; 0.50 |
| Asembo | 49 (38.3) | 124 (38.9) | 173 (38.7) | 1.06 (0.82-1.36) | |||
| Karemo | 10 (7.8) | 36 (11.3) | 46 (10.3) | 1.46 (0.76-2.79) | |||
| SES2 | 424 | MCA1-2 | 66 (55.9) | 114 (37.3) | 180 (42.5) | Reference | 12.2; <0.001 |
| MCA3-5 | 52 (44.1) | 192 (62.7) | 244 (57.5) | 1.42 (1.14-1.78) | |||
| Ever Married | 446 | No | 13 (10.2) | 61 (19.2) | 74 (16.6) | Reference | 5.37; 0.02 |
| Yes | 115 (89.8) | 257 (80.8) | 372 (83.4) | 0.90 (0.83-0.97) | |||
| Married at death | 372 | No | 80 (69.6) | 52 (20.2) | 132 (35.5) | Reference | 84.5; <0.001 |
| Yes | 35 (30.4) | 205 (79.8) | 240 (64.5) | 2.62 (1.98-3.48) | |||
| Attend primary 3 | 316 | No | 60 (59.4) | 42 (19.5) | 102 (32.3) | Reference | 50.0; <0.001 |
| Yes | 41 (40.6) | 173 (80.5) | 214 (67.7) | 1.98 (1.55-2.53) | |||
| Attend secondary | 423 | No | 114 (92.7) | 241 (80.3) | 355 (83.9) | Reference | 9.9; 0.002 |
| Yes | 9 (7.3) | 59 (19.7) | 68 (16.1) | 2.69 (1.38-5.25) | |||
| Care pre-death | 395 | No | 44 (37.9) | 147 (52.7) | 191 (48.4) | Reference | 7.2; 0.008 |
| Yes | 72 (62.1) | 132 (47.3) | 204 (51.6) | 0.76 (0.63-0.92) | |||
| Hospital pre-death | 204 | No | 33 (45.8) | 37 (28.0) | 70 (34.3) | Reference | 6.6; 0.01 |
| Yes | 39 (54.2) | 95 (72.0) | 134 (65.7) | 1.33 (1.05-1.69) | |||
| Died | 445 | No | 40 (31.3) | 143 (45.1) | 183 (41.1) | Reference | 7.24;0.007 |
| home | Yes | 88 (68.8) | 174 (54.9) | 262 (58.9) | 0.80 (0.69-0.93) | ||
| Regular4 alcohol | 417 | No | 110 (90.9) | 185 (62.5) | 295 (70.7) | Reference | 33.5; <0.001 |
| Yes | 11 (9.1) | 111 (37.5) | 122 (29.3) | 4.13 (2.30-7.39) | |||
| Regularly4 drunk | 354 | No | 108 (94.7) | 185 (77.1) | 293 (82.8) | Reference | |
| Yes | 6 (5.3) | 55 (22.9) | 61 (17.2) | 4.35 (1.93-9.81) | 16.9; <0.001 |
1 Data collection in Karemo commenced in 2008 2.SES: socio-economic status measured using multiple correspondence analysis in order to calcuate wealth quintiles (1=poorest 5=least poor) 3.This question not consistently asked 4. Reportedly occurred at least weekly.
Figure 2. Trauma mortality rates among adults aged 15 years and above by age group and gender, 2003 to 2008.
A: Male; B: Female.
Causes of trauma-related deaths
Thirty one percent (n=140) of trauma deaths were recorded as arising from intentional causes (assault and suicides), and the remainder were non-intentional. Intentional causes accounted for 37% (n=117) of male deaths and 18% (n=23) of female deaths (RR 2.04, 1.37-3.04, p<0.001). Intentional causes accounted for a similar proportion of deaths among the youngest three age groups (43%, 43% and 39% respectively). Compared to the reference age group of 15<25 years, people aged 65<80 years were less likely to die from intentional causes (RR 0.37, 0.21-0.64, p<0.001), as were people aged 80+ (RR 0.16, 0.06-0.43, p<0.001). When data were split by age group, males were significantly more likely than females to die from intentional causes for ages 15<25 (intentional = 50% of male deaths and 15% of female deaths, RR 3.25, 0.88-11.98, p=0.025) and ages 25<40 (intentional = 49% of male deaths and 21% of female deaths, RR 2.34, 1.04-5.27, p=0.015) but there was no significant difference between males and females in the proportion dying from intentional causes in the older three age groups.
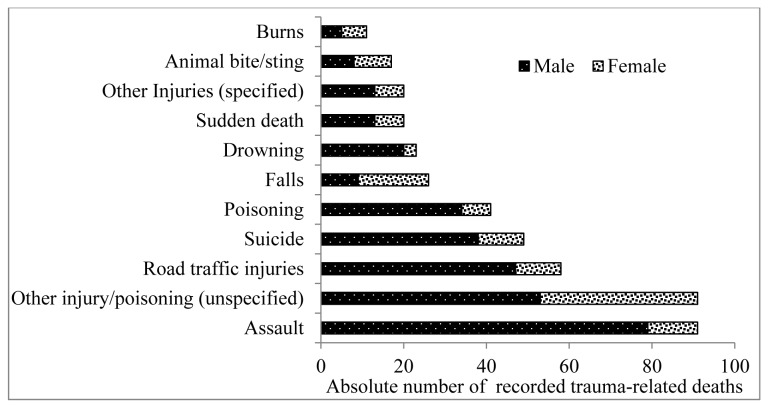
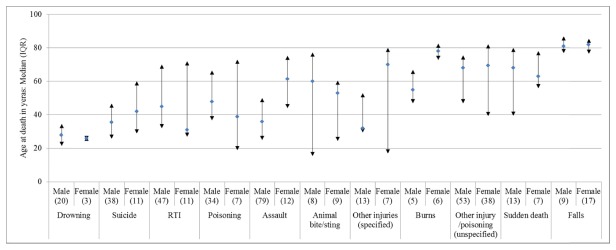
The leading causes of trauma death among adult females were ‘other injuries/poisoning’ (i.e. unspecified cause of trauma; n=38) and falls (n=17); for males the leading causes were assault (n=79) and RTIs (n=47, Figure 3). The contribution to all trauma-related deaths by cause differed by age and gender (Figure 4). The youngest median age at death for both males and females were among those who drowned, while the oldest median age at death was for males and females who had died from a fall.
Figure 3. Major causes of trauma deaths among adults aged 15 years and above by gender, 2003 to 2008.
Figure 4. Age at death by cause of trauma death and gender among adults aged 15 years and above, 2003 to 2008.
Intentional trauma-related deaths
Assault
Among 91 deaths from assault, 79 (87%) were male. Assault contributed 25% of all male trauma-related deaths, except in 2008, when this reached 34%. Deaths clustered in young and middle aged adults, with 54% below 40 years, and 89% below 65 years; deaths occurred among significantly younger males (median age of 36 years (IQR 25-50) compared with females (61.5 years, IQR 44-75; p=0.002). The majority of male assault deaths were from assaults or beatings by individuals or by mobs, with 7 reportedly by a relative, friend, neighbour or the police. Alcohol was documented as a contributory factor in five of the assault deaths; in four of the five deaths both the deceased and the people who attacked them had been drinking. Among those who drank alcohol at least weekly (regular users), 26% trauma-related deaths were caused by assault; for those who drank alcohol less than weekly, 15% of trauma-related deaths were caused by assault (RR 1.8, 1.2-2.6, p=0.006). Six deaths were reported by VA as associated with post-election violence in 2008. Assault-related deaths of females were rarer with 12 reported between 2003 and 2008.
Suicide
49 deaths were categorised as definite suicides, of which 38 (78%) were in males. Ninety percent of suicides were among people below 65 years of age, with a median age of 36 years (IQR 26-50.5); there was no difference by gender. Hanging was the main form of suicide, undertaken by 16 males and five females. Fourteen men and four women poisoned themselves. Other means of suicide were drowning (three men and one woman) and burning (one man); with the means of suicide unreported for the remaining five deaths. Forty-five percent of males who died from suicide were regular alcohol consumers, and 3% were reported to get drunk regularly.
Unintentional trauma-related deaths
Road traffic injuries
Of 58 RTI-related deaths, 47 (81%) were in males. Deaths occurred in all age groups, with a third occurring in 25 to 39 year olds; the median age was 43.5 years (IQR 30-70) with no significant difference by gender. Thirty (52%) RTI-related deaths were among pedestrians, 26 (45%) were in drivers or passengers, and the category of the remaining two deaths was unknown. Nineteen percent were regular drinkers, and 9% were reported to get drunk regularly.
Accidental Poisonings
Of 41 poisonings, 34 (83%) were in males. Deaths spanned all ages, with 37% below 40 years, and 71% below 65 years, with a median age of 47 years (IQR 34-68) and no difference by gender. Poisoning by alcohol was the main cause, reported in 19 male and two female deaths; it was not recorded whether this was from over-consumption or from tainted local brews. While fewer females died from alcohol poisoning, the circumstances were similar between genders. Sixty-five percent of persons who died from accidental poisoning were regular alcohol consumers, and 41% were reported to get drunk regularly. Among trauma-related deaths who were not regular alcohol consumers, 4% were due to poisonings, but among persons who drank regularly, poisoning accounted for 22% of all trauma-related deaths (RR 5.0; 2.7-9.4, p<0.001).
Falls
Of 26 deaths recorded as caused by falls, 17 (65%) were in females, in whom this was the leading specified cause of trauma-related death. Deaths were predominantly in older ages, with 23 (88%) in persons 65 years and above, and 17 (65%) over 80 years; the median age was 81.5 years (IQR 77-87). Falls resulted in broken limbs, back, neck or pelvis, with complications leading to death. Forty-two percent (66% of males, and 26% of females) were regular alcohol consumers, and 29% were reported to get drunk regularly.
Drowning
Of 23 deaths due to drowning, 20 (87%) were in males. Deaths were predominantly in young adults, with 83% less than 40 years of age, and a median age of 27 years (IQR 23-33). In three male and all three female deaths the drowning was thought to have occurred as a result of an epileptic convulsion while the person was in or near the water. Two drownings occurred while crossing a river and four were among males who were fishing. Other male deaths occurred in a dam, a well, a stream and the lake. Fourteen percent were regular alcohol consumers, and 5% were reported to get drunk regularly.
Burns
Of 11 deaths recorded from burns, six (55%) were in females. Just over half of all burns occurred in persons 65 years or older, with a median age of 72 years (IQR 55-78). Burns were mainly caused by house fires, including persons who caught fire from cooking stoves and lanterns. Fourteen percent were regular alcohol consumers, and 8% were reported to get drunk regularly.
Animal bites/stings
17 deaths from bites or stings were distributed equally between males (eight) and females (nine). The median age at death was 53 years (IQR 22-75) with no difference by gender. Of the 14 with a reported cause, eight (57%) were from snake bites, three from dogs, two from bees and one was caused by an unknown insect. All age groups were represented with six (35%) occurring in persons aged 65 and above. Eighteen percent were regular alcohol consumers, and a similar proportion was drunk regularly.
Other injuries (specified)
Other specific injuries caused 20 deaths, predominantly in males (n=13, 65%). These occurred in all age groups, with a median of 38.5 years (IQR 28-71); differences in age by gender were not significant. Specific causes of death in this category were varied and included, for example: being struck by lightning or hit by animals (ox, cow, and donkey), electrocution, walls and other structures collapsing onto them, and a gold mining incident.
Sudden death
Of 20 persons dying suddenly with no clear cause, two-thirds (65%) were among males. Sudden death was recorded in middle or older age, with 17 (85%) occurring in persons over 40 years, with a median age of 63.5 years (IQR 50-78). Information around the deaths was sparse; in six cases the informants could not say how the death had arisen as they were absent when the death occurred. Other records described sudden death as related to old-age.
Other injury/poisoning (unspecified)
This category, consisting of 91 deaths, 53 (58%) in males, was distributed across the age groups. The median age at death was 69 years (IQR 43-78), with no difference by gender. In the majority of these cases, information available did not allow a specific cause to be attributed. Over half (n=52, 57%) were among people aged over 65.
Other characteristics of trauma-related deaths
For both males and females, people dying from trauma were significantly less likely than those dying from other causes to be recorded by the VA as receiving medical care after the trauma and before death (both p<0.001, Table 1). Among trauma-related deaths more females had sought any form of care from both formal and informal health sectors including traditional sources prior to death compared with males (62% vs 47%; p=0.008). However, a significantly lower proportion of females received formal medical care from a hospital (54% compared with 72% among male deaths; p=0.01), while a significantly higher proportion of females (69%) compared with males (55%), died at home p=0.007, Table 3).
Males dying from trauma were significantly more likely to be regular alcohol consumers (38%) compared to those dying from other non-trauma-related causes (28%; p<0.001, Table 1). Of trauma-related deaths, males were significantly more likely than females to consume alcohol regularly (RR 4.1, 2.3-7.4) and to get drunk regularly (RR 4.4, 1.9-9.8, Table 3).
Multivariate analysis
Each key variable shown to be significant in univariate analysis contributed to the multivariate analysis (Table 4). Gender, age, alcohol consumption, receipt of any care prior to death, and place of death (home or health facility) remained significant within the model. Socio-economic status, education (primary school attendance), year of death, and marital status were not significant. The risk of death from trauma rose with age, with persons aged over 80 and persons 65-80 years, 7- and 4-fold more likely to be ascribed trauma as their cause of death, compared with young adults (Table 4). Males had a 4-fold higher risk of a trauma-related death (ARR 4.0, 1.7-9.4) than females. Regular alcohol consumption remained significantly associated with trauma-related deaths (Adjusted RR 1.5, 1.3-1.9). The strongest predictor of a trauma death was absence of any care prior to death (ARR 12.2, 9.4-15.8). Despite this, trauma cases were 3-fold more likely to die outside the home reflecting the frequency of RTI and other fatalities.
Table 4. Factors predicting trauma-related deaths, multivariate analysis (n=6076 deaths).
| Attribute | Category | Exp (B) | 95% Confidence interval | p value |
|---|---|---|---|---|
| Year1 | 2003 | Reference | ||
| 2004 | 0.93 | 0.59-1.49 | 0.78 | |
| 2005 | 0.71 | 0.42-1.21 | 0.21 | |
| 2006 | 1.35 | 0.88-2.10 | 0.17 | |
| 2007 | 1.15 | 0.74-1.80 | 0.53 | |
| 2008 | 1.30 | 0.83-2.02 | 0.25 | |
| Sex | Female | Reference | ||
| Male | 3.99 | 1.71-9.39 | 0.001 | |
| Age (years) | 15 to 24 | Reference | ||
| 25 to 39 | 1.41 | 0.55-3.67 | 0.48 | |
| 40 to 64 | 1.65 | 0.52-5.29 | 0.40 | |
| 65 to 79 | 4.23 | 0.84-21.24 | 0.08 | |
| 80+ | 7.33 | 1.09-49.19 | 0.04 | |
| SES2 | MCA1-2 | Reference | ||
| MCA3-5 | 1.25 | 0.96-1.64 | 0.10 | |
| Attend Primary | No | 0.97 | 0.65-1.43 | 0.86 |
| School | Yes | Reference | ||
| Married | No | 0.96 | 0.72-1.28 | 0.78 |
| at death | Yes | Reference | ||
| Any care | No | 12.21 | 9.43-15.80 | <0.001 |
| Yes | Reference | |||
| Died at home | No | 3.00 | 2.25-3.92 | <0.001 |
| Yes | Reference | |||
| Regular3 use of alcohol | No | Reference | ||
| Yes | 1.46 | 1.13-1.89 | 0.004 |
1 Karemo excluded as data collection commenced in 2008 2.SES: socio-economic status measured using multiple correspondence analysis in order to calcuate wealth quintiles (1=poorest 5=least poor). Interaction terms sexF*age groups 80y+ (expB 0.23); 65<80y (expB 0.37); 40<65y (expB 0.45); 25<40y (expB 0.53); 15<25y (reference) 3 Reportedly occurred at least weekly.
Discussion
The burden of trauma is growing globally and there has been a call for improving surveillance methodologies to capture information for public health interventions [6]. In this paper we present unique data identifying deaths associated with trauma in a rural community of Eastern Africa. While trauma contributes a relatively small percentage of deaths in rural areas of Eastern and Southern Africa (here 2% of female deaths and 6% of male deaths), where a high burden of HIV, TB and malaria dominate, case histories show considerable suffering and lack of access to care, in particular hospital-based care for women.
Global estimates suggest injuries account for half of all male mortality in the ages 10 to 24 [2,3]. Here, the contribution of trauma to all deaths in young adult males aged 15 to 24 years is lower (17% of all male deaths in this age group), but still considerable. Separate analysis found trauma equalled HIV as the main contributor to deaths among young males in this area [15], and confirms the need to document such health threats in adolescents and young adults in SSA [19]. We noted physical injuries leading to death among elderly members of the community; on a population basis, trauma-related mortality rates were highest among persons 65 years and older of both genders. While this belies the larger number of trauma deaths numerically occurring in younger age groups, it indicates a need for interventions to reduce injury risk in this age group, for example, home assessment and reducing safety risks.
Deaths from intentional causes accounted for one third of all deaths; of these there were 91 deaths from assault and 49 from suicide. Deaths from intentional causes accounted for a greater proportion of male than female deaths and a greater proportion of deaths of people in the youngest three age groups than the oldest two. Indeed assault was the main cause of death from trauma among males, comprising 25% of all male trauma deaths and 36% of deaths among young males aged 15 to 24. Interpersonal violence contributed 5.2% of all deaths among males aged 15-49 years globally in 2010 [2], with 12% of deaths among young males (ages 10 to 24 years) estimated to be due to violence [3]. In South Africa, interpersonal violence was the second leading cause of healthy years of life lost and Norman and colleagues recommended that violence be considered a priority health problem as well as a human rights and social issue [20]. In 2008, the number of male deaths from assault occurring in the HDSS accounted for 34% of male deaths, likely related to post election violence, raising the need for protective interventions during election periods when civil unrest might be predicted.
Global Burden of Disease data highlight injuries as an important cause of death in females, as well as males, worldwide [2-4]. Among females, injury from assault is mainly associated with intimate partner violence (IPV), with 1.6% of deaths among females 15-45 years due to this cause worldwide in 2010 [2]. However, prevalence studies show endemic levels of IPV in many countries [22]. In the nationally representative Kenyan Demographic Health Survey, 25% of women reported having been violently abused in the 12 months prior to survey [23]. Highest rates (of 36%) were reported in Nyanza Province, where the HDSS is located. Reasons women gave for “deserved beatings” included burning food, arguing, going out without telling, child ‘neglect’, and refusing sex [23]. However, despite the reported pervasive violence, only 1% of adult female deaths in the HDSS were classified as assault. Under-ascertainment of deaths from IPV is suspected since documentation through VA depends upon the spouse or partner, as next of kin, to report on the events surrounding death. Further consideration should be given to how IPV can better be captured using the VA tool.
The 49 deaths in the current study from suicide accounted for 11% of all injury deaths. By comparison, in South Africa, 9% of all injury deaths were due to suicide [20]. Globally, suicide (self-harm) was identified as a leading cause of death for both males and females in 2010, contributing 5.7% and 4.8% of all deaths in this age group, respectively [2]. These data underscore the need to strengthen health care services in LMIC for mental health disorders, including depression, which is the leading global cause of years lived with disability [21].
Between 1990 and 2010, one million more deaths from injuries worldwide has been calculated (a 24% increase), and accounting for close to one in ten (9.6%) of all deaths [2]. This was largely due to a rise in unintentional injuries, for example a 46% rise in deaths from road traffic injuries, and an increase in deaths from falls [2]. In our study area, RTIs accounted for 58 (13.0%) of trauma-related deaths; 81.0% were among males, a third occurred in persons aged 25 to 39, and half of the deaths were among pedestrians, who tend to walk on roads rather than footpaths. The contribution of RTIs to mortality in Kenya is significant in terms of human suffering and financial cost, and the number of fatalities is increasing [24,25]. Pedestrians and passengers are most affected [25,26], and in rural areas, passengers in buses and public service commuter vans (matatus) account for the majority of fatalities [24,25]. Road safety is determined by both individual behaviour and structural issues [25,26], and both should be considered by the National Road Safety Council of Kenya in terms of formulating road safety policy. Such policies could include the development of footpaths to protect pedestrians, education about where to walk and the need for reflective clothing if walking at night, street lighting, proper road maintenance, speed enforcement and regulations that ensure that drivers are capable of driving safely and vehicles are road worthy [26]. That trauma deaths significantly occur outside of care, and at home, also suggest road accident victims do not reach services in time to receive life-saving treatment, and support is needed to develop ambulance services to reach persons critically injured.
We identified a significantly higher proportion of male trauma-related deaths among regular alcohol drinkers compared with non-regular drinkers. Alcohol consumption is a well-established risk factor for injury [27]. Alcohol consumption in this population is characterised by persons drinking until they get drunk [28], placing them at risk of injury. Nearly half of all male assault deaths and a third of all female assault deaths recorded were regular consumers of alcohol. Four out of every five male deaths from poisoning were also reported to be regular drinkers. Poisoning may arise from excessive ethanol consumption or from tainted brews. Separate systematic chemical analyses of locally used traditional homebrews in Kenya found that an average changaa (a traditional spirit) drink equalled 3.5 standard drinks in the UK (2 in the USA), and busaa (a traditional beer) equalled 2.3 (1.3 in the USA) [29]. The ethanol content of changaa varied from less than 20% to just over 50% [29]. Toxicity from contaminants in the brewing process, by error or to enhance alcohol content, cause additional and potentially large scale morbidity and mortality [30]. The Kenyan Alcoholic Drinks Control Act, introduced in 2010 to control illicit brewing [31], has yet to be examined to determine its full impact on trauma-related morbidity and mortality.
Our multivariate analysis illustrated the risk of death among the elderly, persons who died without receiving any form of care, and who died in the home. Our data also show how unintentional injuries from falls disproportionately affected the elderly and women. Each year, about a third of people aged 65 years and over experience a fall, although this varies by country [32]. Unintentional falls among the elderly result from environmental hazards and an increased susceptibility due to sight loss, memory impairment, poorer posture control and muscle strength and tone [33]. Lower educational level and lack of resources place the elderly at risk of injury, and limit their ability to seek care following injury. Regular alcohol consumption was reportedly higher among these female deaths; a survey among this population noted the frequency of alcohol consumption increased with age among females, potentially placing the elderly at risk of accidental injuries [28]. This community, as in many SSA countries, has been disrupted by deaths from HIV/AIDs in prime aged adults, frequently leaving elderly female widows in poverty and unsupported [34]. The VA documented deaths following broken limbs, back, neck and pelvis as a consequence to falls, and found few of the injured received care from hospital after their fall and prior to death. Coupled with the deaths from house fires, especially among older women, these results suggest the need for home assessments to develop safety strategies through Kenya’s community health worker programme.
Study limitations
This study has a number of important limitations. First, the population has been part of a health and demographic surveillance system for over a decade and thus, has been exposed to numerous trials testing interventions. These have all been for communicable disease control, however; and impact on trauma-related deaths is likely to be relatively small. Second, the number of deaths attributed to trauma constitutes only a small proportion of all deaths in rural communities affected by HIV, TB, and malaria, minimising the scope of analysis possible. Third, while the sensitivity and specificity of both physician and computer algorithm based diagnoses are higher for injuries than any other cause of death [35], we acknowledge that trauma-related deaths may be misclassified. Questioning of the closest relative on events surrounding death has severe limitations, particularly for ascribing cause of death for trauma. Literature illustrates that a high proportion of deaths from intentional injury are perpetrated by an assailant known to the victim; yet in our data a very low proportion of female deaths were ascribed to IPV, despite a known high prevalence of domestic violence in this population. False reporting of cause of death requires additional research in order to adjust for this important public health concern. Moreover, one in five deaths lacked the details necessary to ascribe a specific trauma-related cause; because of the relatively small number of deaths attributed to trauma, lack of information among 20% of deaths severely hampered more sophisticated analyses. This may have also occurred among unintentional trauma deaths for more benign reasons, such as family migration, observer recall bias, and no living relative. This is particularly relevant for deaths among the elderly who may have no living relative close by, or whose spouse is infirm and unable to adequately respond. We suggest follow-up of deaths occur within a narrower time window to minimise migration loss and reduce recall bias. Approaches to generating information on vulnerable deaths, however, clearly require further exploration. Lack of data on cause of death extends also to minimal information being captured on a range of data characterising the individual. Alcohol consumption, socio-economic status, age and gender, and marital status have been available, but other information is only available through informal reporting, such as fighting or social pressures occurring before the fatal event. The VA questionnaires have hitherto included open text fields, allowing the recording of consequences such as “fell and broke neck”, “clothes caught fire from cigarette”, or “fall resulted in complications leading to death”. These have been useful in attribution, and we are reluctant to endorse attempts to remove textual information from VA questionnaires. Finally, underlying pathology in many of such deaths may not have been recognized by the next of kin, resulting in only the physical consequences being recorded; for example, falls among the elderly may be caused by hypotension, ischaemic heart disease, or stroke. While VA classifies ‘sudden death’ as a trauma death; cerebral vascular deaths or cardio-vascular disease resulting in sudden death may again be misclassified as trauma. Due to these limitations, we have chosen to limit the scope of our analysis to descriptive characterisations, and believe these data contribute towards an understanding of the causes of trauma, current pitfalls in knowledge, and inferences for research and preventive interventions to minimise such deaths.
Conclusions
Publications documenting deaths from trauma, especially in LMIC, are relatively scarce. However, an understanding of causes of largely preventable trauma deaths is needed to guide the design of public health interventions and policies [36]. We conclude that, while a small portion of deaths in rural areas with high HIV, TB and malaria prevalence, are ascribed to trauma they represent preventable mortality, and interventions to reduce these deaths are urgently needed. Trauma among young males is well documented, but surprisingly high in this rural population, matching the mortality from HIV [15]. Here we also show the vulnerability of older groups, especially older women, from trauma deaths such as falls. Data suggest the elderly subsequently die at home, without any resort to care. Policies and guidelines for targeting interventions to prevent trauma in different population groups are needed, as are improvements in systems and tools to record underlying causes of death associated with trauma. Methods are required to improve the quality of data, including the underlying causes of deaths; while targeted research could provide new insights, more logistical changes such as earlier follow-up, and a broader scoping of informants could contribute to strengthening systems. Potential under-reporting of deaths from intimate partner violence among women is a particular concern.
Acknowledgments
We are grateful to the communities living in the HDSS for their support and assistance. We thank the HDSS field and office staff for their hard work collecting and evaluating HDSS data. INDEPTH is acknowledged for its support in strengthening HDSS and VA methodologies. Dr John Vulule is thanked for his advice and support. The Director of KEMRI has approved this manuscript.
Funding Statement
The HDSS and field staff support has been funded through the KEMRI/CDC Cooperative Agreement grant, with supplemental support from project-specific grants. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Lopez AD, Mathers CD (2006) Measuring the global burden of disease and epidemiological transitions: 2002-2030. Ann Trop Med Parasitol 100: 481-499. doi: 10.1179/136485906X97417. PubMed: 16899150. [DOI] [PubMed] [Google Scholar]
- 2. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K et al. (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380: 2095-2128. doi: 10.1016/S0140-6736(12)61728-0. PubMed: 23245604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Patton GC, Coffey C, Sawyer SM, Viner RM, Haller DM et al. (2009) Global patterns of mortality in young people: a systematic analysis of population health data. Lancet 374: 881-892. doi: 10.1016/S0140-6736(09)60741-8. PubMed: 19748397. [DOI] [PubMed] [Google Scholar]
- 4. Ribeiro PS, Jacobsen KH, Mathers CD, Garcia-Moreno C (2008) Priorities for women's health from the Global Burden of Disease study. Int J Gynaecol Obstet 102: 82-90. doi: 10.1016/j.ijgo.2008.01.025. PubMed: 18387613. [DOI] [PubMed] [Google Scholar]
- 5. Garcia-Moreno C, Watts C (2011) Violence against women: an urgent public health priority. Bull World Health Organ 89: 2. doi: 10.2471/BLT.10.085217. PubMed: 21346880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mathers CD, Loncar D (2006) Projections of global mortality and burden of disease from 2002 to 2030. PLOS Med 3: e442. doi: 10.1371/journal.pmed.0030442. PubMed: 17132052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ranney ML, Odero W, Mello MJ, Waxman M, Fife RS (2009) Injuries from interpersonal violence presenting to a rural health center in Western Kenya: characteristics and correlates. Inj Prev 15: 36-40. doi: 10.1136/ip.2008.019547. PubMed: 19190274. [DOI] [PubMed] [Google Scholar]
- 8. Odero W, Polsky S, Urbane D, Carel R, Tierney WM (2007) Characteristics of injuries presenting to a rural health centre in western Kenya. East Afr Med J 84: 367-373. PubMed: 17970004. [DOI] [PubMed] [Google Scholar]
- 9. Bhalla K, Harrison JE, Shahraz S, Fingerhut LA, Burden Global of Disease Injury Expert Group (2010) Availability and quality of cause-of-death data for estimating the global burden of injuries. Bull World Health Organ 88: 831-838C [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Garrib A, Herbst AJ, Hosegood V, Newell ML (2011) Injury mortality in rural South Africa 2000-2007: rates and associated factors. Trop Med Int Health 16: 439-446. doi: 10.1111/j.1365-3156.2011.02730.x. PubMed: 21284789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. WHO (2011) World Health Statistics. Available: http://www.whoint/whosis/whostat/EN_WHS2011_Fullpdf. Accessed July 2012.
- 12. Otieno T, Woodfield JC, Bird P, Hill AG (2004) Trauma in rural Kenya. Injury 35: 1228-1233. doi: 10.1016/j.injury.2004.03.013. PubMed: 15561111. [DOI] [PubMed] [Google Scholar]
- 13. Odhiambo FO, Laserson KF, Sewe M, Hamel MJ, Feikin DR et al. (2012) Profile: the KEMRI/CDC Health and Demographic Surveillance System--Western Kenya. Int J Epidemiol 41: 977-987. doi: 10.1093/ije/dys108. PubMed: 22933646. [DOI] [PubMed] [Google Scholar]
- 14. Adazu K, Lindblade KA, Rosen DH, Odhiambo F, Ofware P et al. (2005) Health and demographic surveillance in rural western Kenya: a platform for evaluating interventions to reduce morbidity and mortality from infectious diseases. Am J Trop Med Hyg 73: 1151-1158. PubMed: 16354829. [PubMed] [Google Scholar]
- 15. Phillips-Howard PA, Odhiambo FO, Hamel M, Adazu K, Ackers M et al. (2012) Mortality trends from 2003 to 2009 among adolescents and young adults in rural Western Kenya using a health and demographic surveillance system. PLOS ONE 7: e47017. doi: 10.1371/journal.pone.0047017. PubMed: 23144796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.http://www.indepthnetwork.org/ INDEPTH Standardized verbal autopsy questionnaire. Available: Accessed 2012 September 12.
- 17. van Eijk AM, Adazu K, Ofware P, Vulule J, Hamel M et al. (2008) Causes of deaths using verbal autopsy among adolescents and adults in rural western Kenya. Trop Med Int Health 13: 1314-1324. PubMed: 18721187. [DOI] [PubMed] [Google Scholar]
- 18.http://www.cpc.unc.edu/measure/tools/monitoring-evaluation-systems/savvy Sample Savvy Vital Registration with Verbal Autopsy. Available: . Accessed 2012 September 12.
- 19. Patton GC, Coffey C, Cappa C, Currie D, Riley L et al. (2012) Health of the world's adolescents: a synthesis of internationally comparable data. Lancet 379: 1665-1675. doi: 10.1016/S0140-6736(12)60203-7. PubMed: 22538181. [DOI] [PubMed] [Google Scholar]
- 20. Norman R, Schneider M, Bradshaw D, Jewkes R, Abrahams N et al. (2010) Interpersonal violence: an important risk factor for disease and injury in South Africa. Popul Health Metr 8: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Beddington J, Cooper CL, Field J, Goswami U, Huppert FA et al. (2008) The mental wealth of nations. Nature 455: 1057-1060. doi: 10.1038/4551057a. PubMed: 18948946. [DOI] [PubMed] [Google Scholar]
- 22. Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH (2006) Prevalence of intimate partner violence: findings from the WHO multi-country study on women's health and domestic violence. Lancet 368: 1260-1269. doi: 10.1016/S0140-6736(06)69523-8. PubMed: 17027732. [DOI] [PubMed] [Google Scholar]
- 23. KNBS (2010) Kenya Demographic and Health Survey 2008-09. Nairobi: Kenya: National.Bureau of Statistics (KNBS) and ICF Macro; [Google Scholar]
- 24. Azetsop J (2010) Social Justice Approach to Road Safety in Kenya: Addressing the Uneven Distribution of Road Traffic Injuries and Deaths across Population Groups. Public Health Ethics 3: 115-127. doi: 10.1093/phe/phq013. PubMed: 20664752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Odero W, Khayesi M, Heda PM (2003) Road traffic injuries in Kenya: magnitude, causes and status of intervention. Inj Control Saf Promot 10: 53-61. doi: 10.1076/icsp.10.1.53.14103. PubMed: 12772486. [DOI] [PubMed] [Google Scholar]
- 26. Lagarde E (2007) Road traffic injury is an escalating burden in Africa and deserves proportionate research efforts. PLOS Med 4: e170. doi: 10.1371/journal.pmed.0040170. PubMed: 17593893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rehm J, Kanteres F, Lachenmeier DW (2010) Unrecorded consumption, quality of alcohol and health consequences. Drug Alcohol Rev 29: 426-436. doi: 10.1111/j.1465-3362.2009.00140.x. PubMed: 20636660. [DOI] [PubMed] [Google Scholar]
- 28. Lo TQ, Oeltmann JE, Odhiambo FO, Beynon C, Pevzner E et al. (2013) Alcohol use, drunkenness and tobacco smoking in rural western Kenya. Trop Med Int Health 18: 506-515. doi: 10.1111/tmi.12066. PubMed: 23489316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Papas RK, Sidle JE, Wamalwa ES, Okumu TO, Bryant KL et al. (2010) Estimating alcohol content of traditional brew in Western Kenya using culturally relevant methods: the case for cost over volume. AIDS Behav 14: 836-844. doi: 10.1007/s10461-008-9492-z. PubMed: 19015972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. WHO (2004) Global Status Report on Alcohol 2004. Geneva Switzerland: World Health Organization; [Google Scholar]
- 31. NACADA (2010) The Alcohol Drinks Control Act, 2010. Nairobi. [Google Scholar]
- 32. WHO (2007) WHO global report on falls prevention in older age. Geneva, Switzerland:World Health Organization. [Google Scholar]
- 33. Rubenstein LZ (2006) Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 35 Suppl 2: ii37-ii41. doi: 10.1093/ageing/afl084. PubMed: 16926202. [DOI] [PubMed] [Google Scholar]
- 34. Kautz T, Bendavid E, Bhattacharya J, Miller G (2010) AIDS and declining support for dependent elderly people in Africa: retrospective analysis using demographic and health surveys. BMJ 340: c2841. doi: 10.1136/bmj.c2841. PubMed: 20554660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chandramohan D, Maude GH, Rodrigues LC, Hayes RJ (1998) Verbal autopsies for adult deaths: their development and validation in a multicentre study. Trop Med Int Health 3: 436-446. doi: 10.1046/j.1365-3156.1998.00255.x. PubMed: 9657505. [DOI] [PubMed] [Google Scholar]
- 36. Borse NN, Hyder AA (2009) Call for more research on injury from the developing world: results of a bibliometric analysis. Indian J Med Res 129: 321-326. PubMed: 19491427. [PubMed] [Google Scholar]