Update
This article was updated on January 13, 2015, because one of the members of the MOON Group (Warren R. Dunn, MD, MPH) was not listed in the footnote. The footnote now reads: “*MOON contributing authors: Kurt P. Spindler, MD, and Laura J. Huston, MS (Vanderbilt University School of Medicine); Rick W. Wright, MD, Matthew J. Matava, MD, and Robert H. Brophy, MD (Washington University School of Medicine at Barnes-Jewish Hospital); Eric C. McCarty, MD (University of Colorado School of Medicine); Robert G. Marx, MD, MSc (Hospital for Special Surgery); Richard D. Parker, MD, Jack T. Andrish, MD, and Morgan H. Jones, MD, MPH (Cleveland Clinic); Annunziato Amendola, MD, and Brian R. Wolf, MD, MS (University of Iowa); James L. Carey, MD, MPH (University of Pennsylvania); and Warren R. Dunn, MD, MPH (University of Wisconsin).”
An erratum has been published: J Bone Joint Surg Am 2015; 97(4); e21.
Background:
Recent efforts to improve the results of anterior cruciate ligament (ACL) reconstruction have focused on placing the femoral tunnel anatomically. Medial portal femoral tunnel techniques facilitate drilling of femoral tunnels that are more anatomic than those made with transtibial techniques. Few studies have compared the clinical outcomes of these two femoral tunnel techniques. We hypothesized that the transtibial technique is associated with decreased Knee injury and Osteoarthritis Outcome Scores (KOOS) and an increased risk of repeat surgery in the ipsilateral knee when compared with the anteromedial portal technique.
Methods:
Four hundred and thirty-six patients who had undergone primary isolated autograft ACL reconstruction with a transtibial (229 patients) or anteromedial portal (207 patients) technique in 2002 or 2003 were identified in a prospective multicenter cohort. A multiple linear regression model was used to determine whether surgical technique (transtibial or anteromedial portal) was a significant predictor of KOOS at six years postoperatively, after controlling for preoperative KOOS, patient age, sex, activity level, body mass index (BMI), smoking status, graft type, and the presence of meniscal and chondral pathology at the time of reconstruction. A multiple logistic regression model was used to determine whether surgical technique was a significant predictor of repeat ipsilateral knee surgery, after controlling for patient age and activity level, graft type, and meniscal pathology at the time of reconstruction.
Results:
Postoperative KOOS were available for 387 patients (88.8%). Femoral tunnel drilling technique was not a predictor of the KOOS Quality of Life subscore (p = 0.72) or KOOS Function, Sports and Recreational Activities subscore (p = 0.36) at the six-year follow-up evaluation. Data regarding the prevalence of repeat surgery were available for 380 patients. Femoral tunnel technique was a significant predictor of subsequent ipsilateral knee surgery (odds ratio [OR] = 2.49, 95% confidence interval [CI] = 1.30 to 4.78, p = 0.006).
Conclusions:
Patients who underwent ACL reconstruction with a transtibial technique had significantly higher odds of undergoing repeat ipsilateral knee surgery relative to those who underwent reconstruction with an anteromedial portal technique.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
Anterior cruciate ligament (ACL) reconstruction is often successful in enabling athletes to return to the playing field; however, relatively high reinjury and reoperation rates and suboptimal functional outcome scores have been noted in some populations1-3. As surgeons’ understanding of the anatomy and function of the ACL and its role in knee kinematics continues to improve, reconstructive techniques continue to evolve. Recent efforts have focused on the restoration of native ligament anatomy, with a trend away from placement of the femoral tunnel in the traditionally defined over-the-top position4,5.
Two commonly employed techniques for drilling the femoral tunnel are transtibial drilling and drilling via an anteromedial portal. While the transtibial technique has been used for years with good clinical outcomes, some investigators have shown that it cannot reliably place the femoral tunnel in its anatomic footprint6-10. The tunnels produced with use of transtibial methods have been shown by numerous authors to be, on average, located in an anatomically more anterior position (commonly referred to as more vertical in the notch) relative to those placed with the anteromedial portal technique6-14. Biomechanical studies have demonstrated that grafts placed in this nonanatomic position are subjected to less load than those placed anatomically15 and result in poorer rotational control11,16-21. Decreased rotational control and increased loading of other intra-articular structures such as menisci and articular cartilage would be expected to result in decreased patient-reported outcome scores and increased risk of subsequent ipsilateral knee surgery.
While biomechanical data increasingly demonstrate differences between the results of reconstructions with transtibial techniques and those of procedures done with anteromedial portal techniques, clinical differences have not been clearly demonstrated. The few studies comparing the outcomes of different tunnel positions22-24 and different femoral tunnel preparation techniques25-31 demonstrated mixed results regarding clinical outcomes. A recently published study of prospectively collected data from the Danish ACL registry demonstrated increased risk of revision ACL reconstruction when the anteromedial portal technique was compared with the transtibial technique but did not address the odds of repeat surgery other than revision ACL reconstruction32. The purpose of the present study was to compare, with use of a prospectively collected database, the clinical outcomes of patients in whom the ACL femoral tunnel had been drilled via the transtibial technique with those of patients in whom the tunnel had been drilled via the anteromedial portal technique. We hypothesized that the transtibial technique was associated with decreased Knee injury and Osteoarthritis Outcome Scores (KOOS) and increased risk of repeat surgery in the ipsilateral knee in the first six years following the index surgery.
Materials and Methods
Patient Selection
The study was performed with use of the 2002 to 2003 Multicenter Orthopaedic Outcomes Network (MOON) data set, which is a prospective longitudinal cohort including preoperative and six-year follow-up data on 988 patients treated with ACL reconstruction by experienced surgeons. Available data include patient demographic information, surgical technique and graft choice, prevalence of associated chondral and meniscal injuries, patient-reported outcome scores (KOOS) and activity level, and prevalence of repeat surgery including revision ACL reconstruction. Patients eligible for inclusion in this study had undergone unilateral primary ACL reconstruction with autograft tissue, with the femoral tunnel created by either a transtibial or an anteromedial portal technique. Patients who had undergone primary ACL reconstruction with allograft, revision reconstruction, or a concurrent meniscal transplant and those who had an associated posterior cruciate or collateral ligament injury of grade II or higher were excluded. Additionally, patients were excluded if the femoral tunnel had been created with a method other than the transtibial or the anteromedial portal technique. The 436 patients who met all inclusion and exclusion criteria formed the study group (Fig. 1).
Fig. 1.
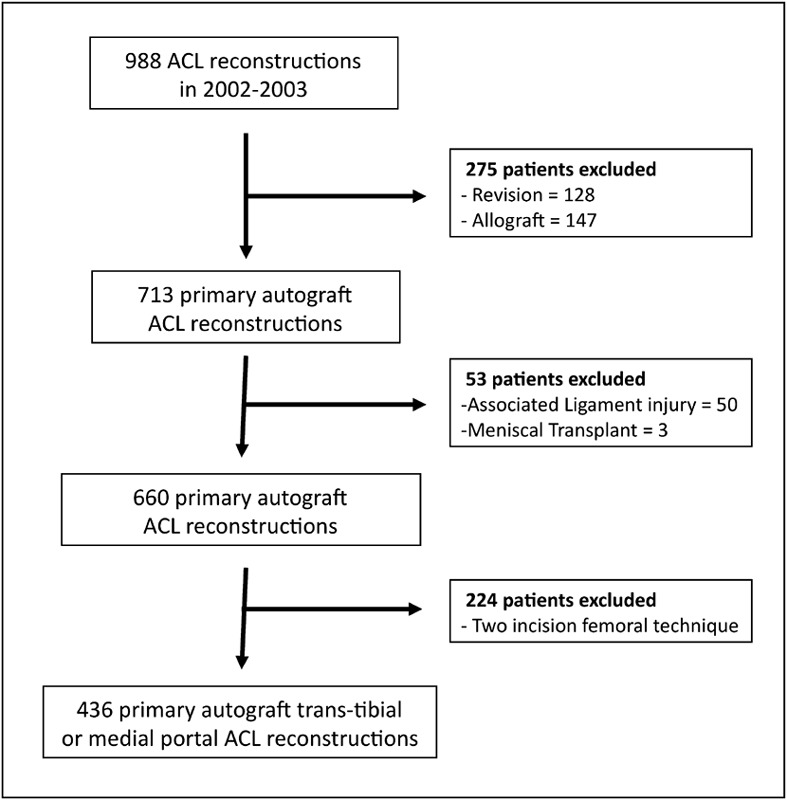
Flow diagram demonstrating the selection of eligible patients for the analysis. Exclusion criteria included revision reconstruction, reconstruction with allograft tissue, the presence of associated ligament injury of grade II or higher, the performance of a meniscal transplant, or the use of a two-incision technique for femoral tunnel ACL reconstruction.
Data Collection
Data extracted from the prospective database for analysis included patient sex; age at the time of the ACL reconstruction; graft type (hamstring or patellar tendon); body mass index (BMI) at the time of the reconstruction; smoking status; presence and treatment of meniscal and cartilage injuries; KOOS knee-related Quality of Life subscale (KOOS-QOL) and KOOS Function, Sports and Recreational Activities subscale (KOOS-Sports/Rec) preoperatively and at the six-year follow-up evaluation33; Marx activity score34 preoperatively and at the six-year follow-up evaluation; and the prevalence of subsequent ipsilateral knee surgery. The technique by which the femoral tunnel was drilled is not a variable initially recorded in the database. This variable was thus determined retrospectively by contacting the surgeons directly and querying them regarding their surgical technique during the data collection period. Three of six surgeons performed exclusively transtibial reconstructions, two performed exclusively anteromedial portal reconstructions, and one performed reconstructions utilizing both techniques. Chart review was utilized to identify the technique used for each patient by the surgeon who utilized both techniques. The surgical technique was unambiguously identified in all 436 cases.
Outcome Variables
The patient-reported outcome scores chosen for this analysis were the KOOS-QOL and KOOS-Sports/Rec subscales on the basis of prior evidence that questions from these subscales are the most responsive to patients’ symptoms and limitations following ACL reconstruction35. Subsequent surgery on the ipsilateral knee was utilized as the secondary outcome measure. Data regarding repeat surgery were obtained by telephone interviews with each patient and include surgical procedures performed at the index institution and elsewhere.
Statistical Methods
A multiple linear regression model was utilized to determine whether femoral tunnel technique (transtibial versus anteromedial portal) was a significant predictor of KOOS-QOL or KOOS-Sports/Rec subscale scores at six years postoperatively, after controlling for the respective preoperative KOOS, graft type, patient sex, patient age and BMI at the time of the reconstruction, smoking status, and the presence and treatment of associated intra-articular pathology. Cartilage injury was modeled with use of one variable for each compartment (medial, lateral, and patellofemoral) denoting the presence or absence of cartilage damage of at least grade II in that compartment. Meniscal injury and treatment were modeled separately for the medial and lateral menisci. Each compartment was coded as normal or no treatment rendered, partial meniscectomy performed, or meniscal repair performed. A power analysis based on the anticipated thirteen degrees of freedom in the model indicated that data from at least 101 patients were required to achieve a power of 80% with α set at 0.05.
A multiple logistic regression model was utilized to determine whether the femoral tunnel drilling technique was a significant predictor of repeat ipsilateral knee surgery. The a priori model used the occurrence of at least one subsequent ipsilateral knee surgery as the outcome variable and included the following predictors: femoral tunnel technique, graft type, patient age and activity level at the time of follow-up, and meniscal injury and treatment. Meniscal injury and treatment were modeled separately for the medial and lateral menisci. Each compartment was coded as normal or no treatment rendered, partial meniscectomy performed, or meniscal repair performed. Because of collinearity between the surgeon performing the surgery and the femoral tunnel technique utilized, the variable “surgeon” could not be included in the logistic regression model. To ensure that no one surgeon’s data had excessive influence on the result, a sensitivity analysis was performed. The logistic regression model was run six additional times, excluding one surgeon from the analysis each time, and the variability of the resulting odds ratio (OR) describing the relationship between femoral tunnel technique and revision was noted.
Source of Funding
This project was partially funded by Grant 5R01 AR053684-06 (K.P.S.) and 5K23 AR052392-05 from the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases and by Grant 5U18-HS016075 from the Centers for Education & Research on Therapeutics (Agency for Healthcare Research and Quality). The project was also supported by the Vanderbilt Sports Medicine Research Fund. Vanderbilt Sports Medicine received unrestricted educational gifts from Smith & Nephew Endoscopy and DonJoy Orthopedics.
Results
Of the 436 patients eligible for study inclusion, 229 (52.5%) underwent transtibial ACL reconstruction and 207 (47.5%) underwent anteromedial portal ACL reconstruction. The baseline characteristics of the patients in the two drilling-technique groups were similar except for an increased frequency of meniscal repair and patellar tendon grafts in the anteromedial portal group (Table I). One postoperative infection requiring debridement was reported in the transtibial group.
TABLE I.
Preoperative Characteristics of Patients According to Femoral Tunnel Technique
| Transtibial (N = 229) | Anteromedial Portal (N = 207) | P Value for Difference Between Groups | |
| Male (no. [%]) | 119 (52.0%) | 102 (49.3%) | 0.63 |
| Age*(yr) | 25.6 ± 10.3 | 27.0 ± 12.1 | 0.18 |
| Smokers (%) | 26 (11.4%) | 17 (8.2%) | 0.33 |
| BMI at surgery*(kg/m2) | 25.3 ± 4.3 | 25.2 ± 4.3 | 0.84 |
| Graft type (no. [%]) | 0.001 | ||
| Hamstring tendon | 172 (75.1%) | 112 (54.1%) | |
| Bone-tendon-bone | 57 (24.9%) | 95 (45.9%) | |
| Cartilage damage (no. [%]) | |||
| Lateral compartment | 27 (11.8%) | 29 (14.0%) | 0.57 |
| Medial compartment | 42 (18.3%) | 36 (17.4%) | 0.80 |
| Patellofemoral | 33 (14.4%) | 30 (14.5%) | 1.00 |
| Medial meniscus (no. [%]) | 0.001 | ||
| Normal | 145 (63.3%) | 129 (62.3%) | |
| Partial meniscectomy | 60 (26.2%) | 33 (15.9%) | |
| Meniscus repair | 19 (8.3%) | 29 (14.0%) | |
| Tear not addressed | 5 (2.2%) | 16 (7.7%) | |
| Lateral meniscus (no. [%]) | 0.004 | ||
| Normal | 143 (62.4%) | 109 (52.7%) | |
| Partial meniscectomy | 62 (27.1%) | 52 (25.1%) | |
| Meniscus repair | 12 (5.2%) | 15 (7.2%) | |
| Tear not addressed | 12 (5.2%) | 31 (15.0%) | |
| Preop. KOOS-QOL* | 35.9 ± 20.1 | 35.0 ± 19.9 | 0.65 |
| Preop. KOOS Sports/Rec* | 47.3 ± 29.5 | 48.5 ± 29.6 | 0.69 |
| Preinjury Marx score* | 11.0 ± 5.3 | 12.0 ± 4.9 | 0.048 |
The values are given as the mean and standard deviation.
Patient-reported outcome data were available preoperatively and at six years postoperatively for 387 (88.8%) of the 436 eligible patients. Multiple linear regression analysis revealed no significant association between femoral tunnel technique and the KOOS-QOL subscore (β = −0.83, 95% confidence interval [CI] = −5.43 to 3.77, p = 0.72) or KOOS-Sports/Rec subscore (β = 2.15, 95% CI = −2.43 to 6.71, p = 0.36) at six years postoperatively, after controlling for the respective preoperative KOOS subscale score, patient age, sex, BMI, smoking status, and meniscal and cartilage pathology. No significant changes in the findings were noted with the use of BMI and smoking status at the time of follow-up rather than BMI and smoking status at the time of reconstruction.
Data regarding repeat surgery, femoral tunnel technique, meniscal pathology, and activity level at six years postoperatively were available for 380 (87.2%) of the 436 eligible patients. Seventy-one subsequent ipsilateral knee operations were performed in forty-four of the 203 patients in the transtibial group and twenty-nine subsequent ipsilateral knee operations were performed in twenty-three of the 177 patients in the anteromedial portal group. The specific procedures performed in each group are described in Table II and stratified by surgeon in Table III. Multiple logistic regression analysis demonstrated a significantly higher odds of undergoing repeat surgery on the ipsilateral knee in the transtibial group relative to the anteromedial portal group (OR = 2.49, 95% CI = 1.30 to 4.78, p = 0.006), after controlling for graft type, patient age and activity level at the time of follow-up, and meniscal status at the time of the reconstruction. The results of the sensitivity analysis of the effect of surgeon demonstrated that the correlation of transtibial drilling with increased odds of repeat surgery was not dependent on any one surgeon’s data. The odds ratio describing this relationship ranged from 2.04 to 3.31 and in each case remained significant (p < 0.05). Because most of the anterior debridement procedures were performed by one surgeon, the multiple logistic regression analysis was repeated with repeat surgery other than anterior debridement as the end point. This analysis again demonstrated significantly higher odds of undergoing repeat surgery on the ipsilateral knee in the transtibial group relative to the anteromedial portal group (OR = 2.08, 95% CI = 1.05 to 4.10, p = 0.035).
TABLE II.
Subsequent Knee Surgery by Femoral Tunnel Technique
| Transtibial* (N = 203) | Anteromedial Portal* (N = 177) | |
| Total procedures† | 71 | 29 |
| Anterior debridement | 16 (7.9%) | 4 (2.3%) |
| Manipulation under anesthesia | 1 (0.5%) | 2 (1.0%) |
| Partial medial meniscectomy | 11 (5.4%) | 5 (2.8%) |
| Partial lateral meniscectomy | 9 (4.4%) | 5 (2.8%) |
| Articular cartilage procedures | 7 (3.4%) | 2 (1.0%) |
| Revision ACL reconstruction | 9 (4.4%) | 5 (2.8%) |
| Other procedures | 13 (6.4%) | 2 (1.0%) |
| No operative report | 5 (2.5%) | 5 (2.8%) |
The values are given as the number (percentage) of patients.
Some patients underwent multiple repeat operations.
TABLE III.
Subsequent Surgical Procedures Performed by Each Surgeon
| Surgeon | No. of Procedures | Anterior Debridement | Manipulation Under Anesthesia | Partial Medial Meniscectomy | Partial Lateral Meniscectomy | Articular Cartilage | Revision ACL | Other | No Report |
| Transtibial | |||||||||
| 1 | 51 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | |
| 2 | 111 | 12 | 1 | 8 | 5 | 4 | 5 | 5 | 3 |
| 3 | 42 | 1 | 1 | 2 | 2 | ||||
| 5 | 25 | 1 | 1 | 1 | 2 | 4 | |||
| Anteromedial portal | |||||||||
| 3 | 5 | ||||||||
| 4 | 56 | 1 | 3 | 1 | |||||
| 6 | 146 | 4 | 1 | 2 | 5 | 2 | 5 | 1 | 5 |
Discussion
The most important finding of this study is that patients who underwent ACL reconstruction with a transtibial technique to drill the femoral tunnel had significantly higher odds of undergoing repeat ipsilateral knee surgery relative to those in whom the femoral tunnel had been drilled with an anteromedial portal technique. Although we did not explore the reason for this association, it is possible that decreased loading of a nonanatomic graft and decreased rotational control in patients who underwent transtibial ACL reconstruction resulted in higher forces on the meniscus and altered pressure distribution on the articular cartilage15,16, increasing the risk of subsequent injury. Furthermore, the anatomically more anterior tunnel position (more vertical in the notch) that often results from a transtibial technique may predispose to graft impingement and an increased prevalence of anterior debridement surgery to address subsequent cyclops lesions36. Interestingly, no significant differences in patient-reported outcome scores were noted between the two groups. One might expect that, if decreased rotational control in the transtibial group is a contributor to the increased risk of repeat ipsilateral knee surgery, these patients would have poorer patient-reported outcome scores as well. Additional research is necessary to investigate the relationship between rotational control and patient-reported outcomes.
One must consider that tunnel position was not evaluated in this study and thus the more vertical tunnel position in the transtibial group cannot be confirmed; however, numerous studies have demonstrated that a transtibial technique generally results in femoral tunnels that are located anterior to the anatomic femoral footprint of the ACL6-14,37. While modifications of the transtibial technique have been reported to reproduce a normal femoral ACL footprint12,13, there is very little margin for error with use of such techniques.
Several authors have examined whether it is even possible to place a femoral tunnel within the anatomic femoral footprint via a traditional transtibial approach. In 2001, Arnold et al. investigated this question by performing arthroscopic transtibial ACL reconstruction on five cadaveric specimens7. Following open dissection, it was determined that it was not possible to place a transtibial femoral guide pin within the femoral ACL footprint. The closest position achievable was at the margin of the femoral attachment. Strauss et al. also investigated this topic in a cadaveric model37. They hypothesized that the constraint from an 8-mm tibial tunnel would preclude transtibial placement of the femoral tunnel in an anatomic position. The percent overlap with the native ACL femoral insertion averaged only 30%. Similarly, McConkey et al. demonstrated in cadavers that the transtibial technique is more likely to produce a more anterior femoral tunnel and less likely to be rated as anatomically placed by independent observers38. It is therefore highly likely that the femoral tunnels in the current study created with the transtibial approach were located in a more nonanatomic position than those created with an anteromedial portal technique.
Biomechanical evidence from both cadaveric and in vivo studies has demonstrated superior rotational control in anatomic single-bundle reconstructions relative to reconstructions with more anterior graft positions from transtibial techniques. Kondo et al., in a controlled laboratory study, tested tibiofemoral kinematics in eight cadaveric knees mounted in a six degrees of freedom setup18. Rotational laxity with internal tibial torque and anterior laxity in a simulated pivot shift were significantly less in anatomic single-bundle reconstructions compared with nonanatomic single-bundle reconstructions. Steiner et al. performed ACL reconstruction on ten pairs of cadaveric knees using either a transtibial drilling method or an independent drilling method14. The independent drilling method produced more horizontal grafts and a more central location of the femoral tunnel within the footprint. Biomechanically, the independent drilling was superior, with anterior translation and internal rotation restored under all loading conditions.
In vivo, Schairer et al. used magnetic resonance imaging (MRI) to evaluate knee kinematics following ACL reconstruction with either an anteromedial portal or a transtibial femoral tunnel technique39. MRIs were acquired with 125 N of simulated load at full extension and at 30° to 40° of flexion. ACL reconstructions performed with the anteromedial portal technique restored knee kinematics that were closer to normal than those resulting from the transtibial technique. In a similar study, Abebe et al. used MRI and biplanar fluoroscopy to evaluate in vivo knee kinematics following ACL reconstruction16. Patients were grouped on the basis of the location of their femoral tunnel as “anteroproximal” or central (anatomic) relative to the native ACL footprint. Patients were asked to perform a quasi-static lunge maneuver, and data were collected. Grafts placed more centrally in the ACL footprint restored normal knee kinematics more completely than those placed anteroproximally.
While the anatomic and biomechanical consequences of transtibial ACL reconstruction have been closely investigated, data are less consistent regarding the impact of surgical technique on clinical outcomes following ACL reconstruction. Alentorn-Geli et al. compared the results of transtibial and anteromedial portal techniques in a population of active soccer players25. Significantly larger improvements in International Knee Documentation Committee (IKDC) scores were noted in the anteromedial portal group compared with the transtibial group. Karlsson et al. compared single-incision and two-incision techniques for ACL reconstruction, with the two groups having similar age, sex distribution, and activity level28. They found significantly lower Lysholm scores in the single-incision group after a mean of forty-seven months of follow-up but the IKDC scores did not differ between the groups. Seon et al. compared patients with a more anatomic femoral tunnel with those with a more anterior (vertical) femoral tunnel24. Neither the Tegner nor the Lysholm scores differed between the groups. In a study in which recently published data from the Danish registry was used to compare revision risk and clinical outcomes (KOOS) between patients treated with the anteromedial technique and those treated with the transtibial technique32, an increased revision risk was noted in the anteromedial portal group. However, with findings similar to those of the current study, the authors noted no difference in KOOS between the groups. The current study did not demonstrate a difference in the risk of revision ACL reconstruction on the basis of femoral tunnel technique, but it was underpowered to detect such a difference.
The current study has several weaknesses. First, as a result of the design of the prospective database and follow-up, the exact three-dimensional position of each patient’s tunnel is not known. Unfortunately, we found no studies in the literature that included three-dimensional tunnel position and had sufficient power to perform multiple linear regression analysis to determine the impact of tunnel position along with other factors on outcome. Another weakness of our study is that we lacked physical examination data with which to detect any difference in rotational or anteroposterior laxity between the two groups. In addition, the relatively small number of revision ACL reconstructions performed in patients in this cohort limits the power to analyze the relationship between surgical technique and the odds of undergoing revision ACL reconstruction. Furthermore, the follow-up time of six years and lack of radiographs preclude detection and assessment of the influence of degenerative changes. Longer follow-up that includes radiographic evaluation may yield useful information in this cohort regarding the effect of femoral tunnel technique on outcome.
Another weakness is that the number of predictors that could be included in the multiple logistic regression model was limited by the number of patients who underwent repeat surgery on the ipsilateral knee (sixty-seven). The desired a priori model contained eight degrees of freedom, slightly in excess of those allowed by the traditional rule requiring n/10 predictors, where n is the number of events (in this case, repeat operations)40. However, recent work has demonstrated that this rule can be relaxed without compromising the model, particularly in cases (such as the current case) in which the predictor of interest is a binary variable41. The use of a composite outcome variable for repeat surgery (combining all procedures into a simple “yes/no”) is a simplification of the data that was necessary for analysis but does introduce possible bias if the prevalence of a single procedure drove the results. The finding that the results remained consistent even after removal of anterior debridement from the analysis (see above) demonstrates that this situation is unlikely.
A final, and perhaps the most important, limitation of this study is that nearly all of the surgeons performed only one surgical technique. Only one of the six surgeons performed two different techniques during the study. The resultant collinearity precluded the inclusion of “surgeon” as a potential predictor in the multiple logistic regression model. Although numerous potential confounders were controlled for in the analysis and we performed a sensitivity analysis to ensure that no one surgeon’s results unduly influenced the data, it is possible that additional, unidentified differences between the patient populations of the different surgeons contributed to the differences in repeat-surgery rates. Such differences could be explored only through evaluation of patients operated on by the same surgeon randomized to different techniques. Until such data are available, the current study represents the best available evidence regarding the effect of femoral tunnel drilling technique on the odds of repeat ipsilateral knee surgery.
In conclusion, patients undergoing ACL reconstruction with use of a transtibial technique to drill the femoral tunnel have increased odds of undergoing repeat ipsilateral knee surgery within the first six postoperative years compared with those who undergo reconstruction with an anteromedial portal technique. No differences in patient-reported outcome scores were noted.
Acknowledgments
Note: The authors thank the following research coordinators, analysts, and support staff from the MOON sites, whose efforts make this consortium possible: Julia Brasfield, Maxine Cox, Michelle Hines, Pam Koeth, and Leah Schmitz (Cleveland Clinic Foundation); Carla Britton and Catherine Fruehling-Wall (University of Iowa); Christine Bennett (University of Colorado); Linda Burnworth, Amanda Haas, and Robyn Gornati (Washington University in St Louis); Lana Verkuil (Hospital for Special Surgery); and Emily Reinke, John Shaw, Suzet Galindo-Martinez, Zhouwen Liu, Thomas Dupont, Erica Scaramuzza, and Lynn Cain (Vanderbilt University).
Investigation performed at The Ohio State University, Columbus, Ohio
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Magnussen RALawrence JTWest RLToth APTaylor DCGarrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012 Apr;28(4):526-31 Epub 2012 Feb 01. [DOI] [PubMed] [Google Scholar]
- 2.Shelbourne KDGray THaro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009 Feb;37(2):246-51 Epub 2008 Dec 24. [DOI] [PubMed] [Google Scholar]
- 3.Borchers JRPedroza AKaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case-control study. Am J Sports Med. 2009 Dec;37(12):2362-7 Epub 2009 Aug 14. [DOI] [PubMed] [Google Scholar]
- 4.Zantop TKubo SPetersen WMusahl VFu FH. Current techniques in anatomic anterior cruciate ligament reconstruction. Arthroscopy. 2007 Sep;23(9):938-47. [DOI] [PubMed] [Google Scholar]
- 5.Arnold MPFriederich NFMüller WHirschmann MT. From open to arthroscopic anatomical ACL-reconstructions: the long way round. A statement paper. Knee Surg Sports Traumatol Arthrosc. 2013 Jul;21(7):1478-81 Epub 2012 May 9. [DOI] [PubMed] [Google Scholar]
- 6.Abebe ESMoorman CT 3rdDziedzic TSSpritzer CECothran RLTaylor DCGarrett WE JrDeFrate LE. Femoral tunnel placement during anterior cruciate ligament reconstruction: an in vivo imaging analysis comparing transtibial and 2-incision tibial tunnel-independent techniques. Am J Sports Med. 2009 Oct;37(10):1904-11 Epub 2009 Aug 17. [DOI] [PubMed] [Google Scholar]
- 7.Arnold MPKooloos Jvan Kampen A. Single-incision technique misses the anatomical femoral anterior cruciate ligament insertion: a cadaver study. Knee Surg Sports Traumatol Arthrosc. 2001 Jul;9(4):194-9. [DOI] [PubMed] [Google Scholar]
- 8.Dargel JSchmidt-Wiethoff RFischer SMader KKoebke JSchneider T. Femoral bone tunnel placement using the transtibial tunnel or the anteromedial portal in ACL reconstruction: a radiographic evaluation. Knee Surg Sports Traumatol Arthrosc. 2009 Mar;17(3):220-7 Epub 2008 Oct 09. [DOI] [PubMed] [Google Scholar]
- 9.Gavriilidis IMotsis EKPakos EEGeorgoulis ADMitsionis GXenakis TA. Transtibial versus anteromedial portal of the femoral tunnel in ACL reconstruction: a cadaveric study. Knee. 2008 Oct;15(5):364-7 Epub 2008 Jun 25. [DOI] [PubMed] [Google Scholar]
- 10.Kaseta MKDeFrate LECharnock BLSullivan RTGarrett WE Jr. Reconstruction technique affects femoral tunnel placement in ACL reconstruction. Clin Orthop Relat Res. 2008 Jun;466(6):1467-74 Epub 2008 Apr 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bedi AMusahl VSteuber VKendoff DChoi DAllen AAPearle ADAltchek DW. Transtibial versus anteromedial portal reaming in anterior cruciate ligament reconstruction: an anatomic and biomechanical evaluation of surgical technique. Arthroscopy. 2011 Mar;27(3):380-90 Epub 2010 Oct 29. [DOI] [PubMed] [Google Scholar]
- 12.Heming JFRand JSteiner ME. Anatomical limitations of transtibial drilling in anterior cruciate ligament reconstruction. Am J Sports Med. 2007 Oct;35(10):1708-15 Epub 2007 Jul 30. [DOI] [PubMed] [Google Scholar]
- 13.Piasecki DPBach BR JrEspinoza Orias AAVerma NN. Anterior cruciate ligament reconstruction: can anatomic femoral placement be achieved with a transtibial technique? Am J Sports Med. 2011 Jun;39(6):1306-15 Epub 2011 Feb 18. [DOI] [PubMed] [Google Scholar]
- 14.Steiner MEBattaglia TCHeming JFRand JDFesta ABaria M. Independent drilling outperforms conventional transtibial drilling in anterior cruciate ligament reconstruction. Am J Sports Med. 2009 Oct;37(10):1912-9 Epub 2009 Sep 02. [DOI] [PubMed] [Google Scholar]
- 15.Xu YLiu JKramer SMartins CKato YLinde-Rosen MSmolinski PFu FH. Comparison of in situ forces and knee kinematics in anteromedial and high anteromedial bundle augmentation for partially ruptured anterior cruciate ligament. Am J Sports Med. 2011 Feb;39(2):272-8 Epub 2010 Dec 04. [DOI] [PubMed] [Google Scholar]
- 16.Abebe ESUtturkar GMTaylor DCSpritzer CEKim JPMoorman CT 3rdGarrett WEDeFrate LE. The effects of femoral graft placement on in vivo knee kinematics after anterior cruciate ligament reconstruction. J Biomech. 2011 Mar 15;44(5):924-9 Epub 2011 Jan 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brophy RHPearle AD. Single-bundle anterior cruciate ligament reconstruction: a comparison of conventional, central, and horizontal single-bundle virtual graft positions. Am J Sports Med. 2009 Jul;37(7):1317-23 Epub 2009 Mar 27. [DOI] [PubMed] [Google Scholar]
- 18.Kondo EMerican AMYasuda KAmis AA. Biomechanical comparison of anatomic double-bundle, anatomic single-bundle, and nonanatomic single-bundle anterior cruciate ligament reconstructions. Am J Sports Med. 2011 Feb;39(2):279-88 Epub 2011 Jan 14. [DOI] [PubMed] [Google Scholar]
- 19.Loh JCFukuda YTsuda ESteadman RJFu FHWoo SL. Knee stability and graft function following anterior cruciate ligament reconstruction: Comparison between 11 o’clock and 10 o’clock femoral tunnel placement. 2002 Richard O’Connor Award paper. Arthroscopy. 2003 Mar;19(3):297-304. [DOI] [PubMed] [Google Scholar]
- 20.Ristanis SStergiou NSiarava ENtoulia AMitsionis GGeorgoulis AD. Effect of femoral tunnel placement for reconstruction of the anterior cruciate ligament on tibial rotation. J Bone Joint Surg Am. 2009 Sep;91(9):2151-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scopp JMJasper LEBelkoff SMMoorman CT 3rd. The effect of oblique femoral tunnel placement on rotational constraint of the knee reconstructed using patellar tendon autografts. Arthroscopy. 2004 Mar;20(3):294-9. [DOI] [PubMed] [Google Scholar]
- 22.Jepsen CFLundberg-Jensen AKFaunoe P. Does the position of the femoral tunnel affect the laxity or clinical outcome of the anterior cruciate ligament-reconstructed knee? A clinical, prospective, randomized, double-blind study. Arthroscopy. 2007 Dec;23(12):1326-33. [DOI] [PubMed] [Google Scholar]
- 23.Sadoghi PKröpfl AJansson VMüller PEPietschmann MFFischmeister MF. Impact of tibial and femoral tunnel position on clinical results after anterior cruciate ligament reconstruction. Arthroscopy. 2011 Mar;27(3):355-64 Epub 2010 Dec 08. [DOI] [PubMed] [Google Scholar]
- 24.Seon JKPark SJLee KBSeo HYKim MSSong EK. In vivo stability and clinical comparison of anterior cruciate ligament reconstruction using low or high femoral tunnel positions. Am J Sports Med. 2011 Jan;39(1):127-33 Epub 2010 Sep 16. [DOI] [PubMed] [Google Scholar]
- 25.Alentorn-Geli ESamitier GAlvarez PSteinbacher GCugat R. Anteromedial portal versus transtibial drilling techniques in ACL reconstruction: a blinded cross-sectional study at two- to five-year follow-up. Int Orthop. 2010 Jun;34(5):747-54 Epub 2010 Apr 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brandsson SFaxén EEriksson BISwärd LLundin OKarlsson J. Reconstruction of the anterior cruciate ligament: comparison of outside-in and all-inside techniques. Br J Sports Med. 1999 Feb;33(1):42-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gerich TGLattermann CFremerey RWZeichen JLobenhoffer HP. One- versus two-incision technique for anterior cruciate ligament reconstruction with patellar tendon graft. Results on early rehabilitation and stability. Knee Surg Sports Traumatol Arthrosc. 1997;5(4):213-6. [DOI] [PubMed] [Google Scholar]
- 28.Karlsson JKartus JBrandsson SMagnusson LLundin OEriksson BI. Comparison of arthroscopic one-incision and two-incision techniques for reconstruction of the anterior cruciate ligament. Scand J Med Sci Sports. 1999 Aug;9(4):233-8. [DOI] [PubMed] [Google Scholar]
- 29.O’Neill DB. Arthroscopically assisted reconstruction of the anterior cruciate ligament. A prospective randomized analysis of three techniques. J Bone Joint Surg Am. 1996 Jun;78(6):803-13. [PubMed] [Google Scholar]
- 30.Reat JFLintner DM. One-versus two-incision ACL reconstruction. A prospective, randomized study. Am J Knee Surg. 1997 Fall;10(4):198-208. [PubMed] [Google Scholar]
- 31.Sgaglione NASchwartz RE. Arthroscopically assisted reconstruction of the anterior cruciate ligament: initial clinical experience and minimal 2-year follow-up comparing endoscopic transtibial and two-incision techniques. Arthroscopy. 1997 Apr;13(2):156-65. [DOI] [PubMed] [Google Scholar]
- 32.Rahr-Wagner LThillemann TMPedersen ABLind MC. Increased risk of revision after anteromedial compared with transtibial drilling of the femoral tunnel during primary anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Register. Arthroscopy. 2013 Jan;29(1):98-105. [DOI] [PubMed] [Google Scholar]
- 33.Roos EMRoos HPLohmander LSEkdahl CBeynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998 Aug;28(2):88-96. [DOI] [PubMed] [Google Scholar]
- 34.Marx RGStump TJJones ECWickiewicz TLWarren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001 Mar-Apr;29(2):213-8. [DOI] [PubMed] [Google Scholar]
- 35.Hambly KGriva K. IKDC or KOOS: which one captures symptoms and disabilities most important to patients who have undergone initial anterior cruciate ligament reconstruction? Am J Sports Med. 2010 Jul;38(7):1395-404 Epub 2010 Mar 29. [DOI] [PubMed] [Google Scholar]
- 36.van Dijck RASaris DBWillems JWFievez AW. Additional surgery after anterior cruciate ligament reconstruction: can we improve technical aspects of the initial procedure? Arthroscopy. 2008 Jan;24(1):88-95 Epub 2007 Nov 05. [DOI] [PubMed] [Google Scholar]
- 37.Strauss EJBarker JUMcGill KCole BJBach BR JrVerma NN. Can anatomic femoral tunnel placement be achieved using a transtibial technique for hamstring anterior cruciate ligament reconstruction? Am J Sports Med. 2011 Jun;39(6):1263-9 Epub 2011 Feb 18. [DOI] [PubMed] [Google Scholar]
- 38.McConkey MOAmendola ARamme AJDunn WRFlanigan DCBritton CLWolf BRSpindler KPCarey JLCox CLKaeding CCWright RWMatava MJBrophy RHSmith MVMcCarty ECVida AFWolcott MMarx RGParker RDAndrish JFJones MH; MOON Knee Group. Arthroscopic agreement among surgeons on anterior cruciate ligament tunnel placement. Am J Sports Med. 2012 Dec;40(12):2737-46 Epub 2012 Oct 17. [DOI] [PubMed] [Google Scholar]
- 39.Schairer WWHaughom BDMorse LJLi XMa CB. Magnetic resonance imaging evaluation of knee kinematics after anterior cruciate ligament reconstruction with anteromedial and transtibial femoral tunnel drilling techniques. Arthroscopy. 2011 Dec;27(12):1663-70 Epub 2011 Sep 29. [DOI] [PubMed] [Google Scholar]
- 40.Harrell FE. Regression modeling strategies. New York: Springer-Verlag; 2001. [Google Scholar]
- 41.Vittinghoff EMcCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2007 Mar 15;165(6):710-8 Epub 2006 Dec 20. [DOI] [PubMed] [Google Scholar]


