Abstract
Background:
Although rotator cuff disease is a common musculoskeletal problem in the United States, the impact of this condition on earnings, missed workdays, and disability payments is largely unknown. This study examines the value of surgical treatment for full-thickness rotator cuff tears from a societal perspective.
Methods:
A Markov decision model was constructed to estimate lifetime direct and indirect costs associated with surgical and continued nonoperative treatment for symptomatic full-thickness rotator cuff tears. All patients were assumed to have been unresponsive to one six-week trial of nonoperative treatment prior to entering the model. Model assumptions were obtained from the literature and data analysis. We obtained estimates of indirect costs using national survey data and patient-reported outcomes. Four indirect costs were modeled: probability of employment, household income, missed workdays, and disability payments. Direct cost estimates were based on average Medicare reimbursements with adjustments to an all-payer population. Effectiveness was expressed in quality-adjusted life years (QALYs).
Results:
The age-weighted mean total societal savings from rotator cuff repair compared with nonoperative treatment was $13,771 over a patient’s lifetime. Savings ranged from $77,662 for patients who are thirty to thirty-nine years old to a net cost to society of $11,997 for those who are seventy to seventy-nine years old. In addition, surgical treatment results in an average improvement of 0.62 QALY. Societal savings were highly sensitive to age, with savings being positive at the age of sixty-one years and younger. The estimated lifetime societal savings of the approximately 250,000 rotator cuff repairs performed in the U.S. each year was $3.44 billion.
Conclusions:
Rotator cuff repair for full-thickness tears produces net societal cost savings for patients under the age of sixty-one years and greater QALYs for all patients. Rotator cuff repair is cost-effective for all populations. The results of this study should not be interpreted as suggesting that all rotator cuff tears require surgery. Rather, the results show that rotator cuff repair has an important role in minimizing the societal burden of rotator cuff disease.
Approximately 4.5 million patient visits related to shoulder pain occur each year in the United States1. Disorders of the rotator cuff range from painful rotator cuff syndromes to full-thickness tears of varying sizes and functional limitations2. Outcomes for rotator cuff tears improve with both surgical and nonsurgical treatment3.
With the aging of the U.S. population and increased labor force participation of the elderly, the burden of rotator cuff tears in the U.S. is an important issue. Using outpatient data from Colorado, Florida, Maryland, New Jersey, New York, and Wisconsin in the State Ambulatory Surgery Databases, Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality, we find that more than two-thirds of patients treated with rotator cuff repair are of working age4. In addition, the prevalence of rotator cuff tears increases with age5. Despite these factors, few studies have examined the burden of rotator cuff tears and the economic impact of treatment is largely unknown.
Societal costs of a medical condition include direct and indirect costs. Direct costs are those associated with diagnosis and treatment, while indirect costs include lost income due to inability to work or lower wages, missed workdays, and disability payments.
The purpose of this study was to determine the value of operative treatment for rotator cuff tears, with value determined by reductions in costs to society from rotator cuff repair compared with nonoperative treatment. Markov models are commonly used in cost-effectiveness analysis. In assessing the value of rotator cuff repair, these models are useful because long-term clinical studies do not exist and the risk of an outcome is continuous over time. By taking a societal perspective, we estimated the costs and benefits of rotator cuff repair to patients, employers, and payers.
Materials and Methods
General Model Overview
We investigated the cost-effectiveness of rotator cuff repair compared with nonoperative treatment for symptomatic full-thickness rotator cuff tears using the Markov decision model presented in Figure 1. Cost-effectiveness is estimated from the societal perspective for the cohort in the U.S. undergoing rotator cuff repair. Outcome and state transition probabilities (i.e., treatment success rates, revision rates, and complications) were obtained from the literature or estimated on the basis of the expert opinion of five orthopaedic surgeons when data were not available. The cycle length was one year, and the model cycled until patient death. The primary effectiveness outcome was expressed in quality-adjusted life years (QALYs), and costs were estimated in 2013 U.S. dollars. Both costs and utilities were discounted at 3% to reflect their present value, as is standard practice in cost-effectiveness research6. The model and analysis were performed in accordance with the consensus-based recommendations for the conduct of cost-effectiveness analysis advocated by the Panel on Cost-Effectiveness in Health and Medicine of the U.S. Public Health Service and using a general decision analysis software package (TreeAge Pro Suite 2011; TreeAge Software, Williamstown, Massachusetts).
Fig. 1.
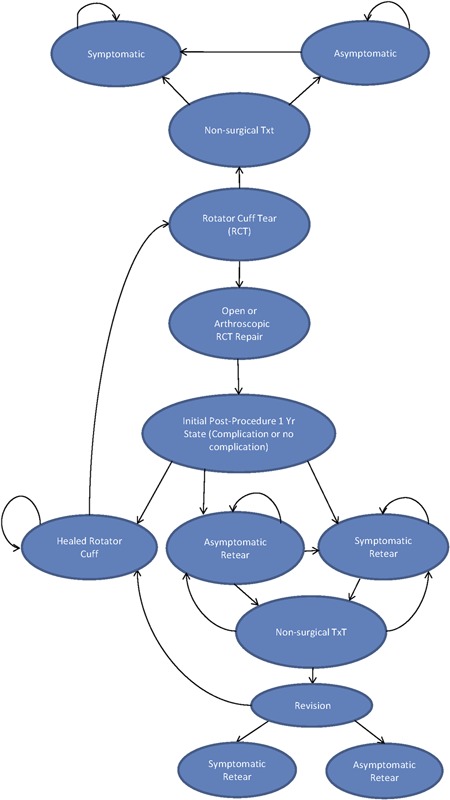
Model schematic diagram of rotator cuff repair treatment pathways. While not indicated directly in the diagram, patients are assumed to die on the basis of all-cause mortality, at which time they exit the model and enter a health state of death that is assigned no additional cost or utility. TxT = treatment.
Model Structure and Assumptions
Our decision tree consists of two primary treatment arms (Fig. 1). Patients with a symptomatic full-thickness rotator cuff tear underwent either open or arthroscopic rotator cuff repair or continued to receive nonoperative treatment. Patients in both treatment arms were assumed to have undergone an average of six weeks of nonoperative treatment prior to this initial decision point. After initial treatment, the model assumes that individuals remained in a postprocedure state for one year, which accounts for the costs and limitations of treatment and recovery as well as any complications. Postoperative complications after rotator cuff repair included infection, adhesive capsulitis, and retear or nonhealed rotator cuff repair.
After one year, the model transitions all rotator cuff repairs into one of four health states: (1) healed rotator cuff repair (symptomatic and asymptomatic), (2) asymptomatic retear, (3) symptomatic retear, or (4) death. Patients in the nonoperative treatment arm entered one of three health states: (1) symptomatic tear, (2) asymptomatic tear, or (3) death. Patients in the rotator cuff repair arm who had not healed in the first year, or who experienced a late retear, could choose to undergo revision surgery consisting of debridement only or reconstruction. Patients who experienced a healed rotator cuff repair could have a retear at rates consistent with the general population5. In the nonoperative treatment arm, patients who initially responded to treatment may have experienced a recurrence of symptoms and could undergo another six-week course of nonoperative treatment, succeeding with this treatment at the base rate outlined below. Patients who had failure of nonoperative treatment did not undergo repeat treatment and remained symptomatic for the remainder of the model. Because the focus of the study was on the value of receiving surgical treatment for rotator cuff tears, patients in the nonoperative treatment arm were not allowed to cross over to the surgical arm. Model assumptions are provided in Table I.
TABLE I.
Model Assumptions for Rotator Cuff Repair
| Base Case | |
| Health state utility* (QALY) | |
| Healed RCR | 0.74 (0.13) |
| Symptomatic RCT | 0.66 (0.12) |
| Asymptomatic RCT | 0.74 (0.13) |
| Transition probabilities | |
| Healing rate with RCR | 75% |
| Success of nonoperative treatment | 68% |
| Initial rate of symptom development after retear† | 5% |
| Long-term retear rate† | 2% |
| Rate of symptom development in RCT† | 8.8% |
| Rate of stiffness after RCR | 2.5% |
| Rate of infection | 0.1% |
| Rate of irreparable rotator cuff at revision | 10% |
| Death‡ | Life tables |
| Cost§ | |
| Nonoperative treatment | $1802 |
| RCR | $15,063 |
| Infection | $12,131 |
| Stiffness | $11,323 |
| Disutility* (QALY) | |
| RCR | 0.02 |
| Infection | 0.05 |
| Stiffness | 0.10 |
| Miscellaneous | |
| Discount rate | 3% |
| Age distribution (mean and stand. dev.) (yr) | 56 ± 13.5 |
The values are given as the mean quality-adjusted life years (QALYs), with the standard deviation in parentheses. RCR = rotator cuff repair, and RCT = rotator cuff tear.
Annual rate.
All-cause mortality was from the Centers for Disease Control and Prevention life tables.
The values are given as the cost per episode.
Population and Mortality Rates
The model was run with several populations, ranging from thirty to eighty years old. A population representative of the annual incidence of rotator cuff repair in the U.S. was used for the base case. All-cause mortality was from the Centers for Disease Control and Prevention life tables. No surgical mortality was modeled.
Utilities
Utilities, which represent an individual’s preferences for specific health outcomes, are derived from the Short Form-12 (SF-12) with the SF-6D (a preference-based six-dimensional health state classification)7. Preoperative SF-12 values were prospectively measured from a cohort of ninety-five patients (mean age, 55.4 years [range, thirty-one to seventy-eight years]; 61% male) who received a primary rotator cuff repair performed by an experienced, shoulder and elbow fellowship-trained orthopaedic surgeon at a major academic medical center. Minimum follow-up was one year, with the last value carried forward for patients whose last follow-up was at six months. The difference between the mean utility (and standard deviation) at the preoperative (0.66 ± 0.11 QALY) and postoperative evaluation (0.74 ± 0.13 QALY) was 0.08 QALY, which was above the minimum clinically important difference of 0.03 QALY8. Patients with a rotator cuff tear responding to nonoperative treatment were assumed to have the same utility as operatively treated patients; however, operatively treated patients experienced a disutility of surgery of 0.02 QALY because of postoperative pain and inconvenience of recovery. Asymptomatic retears were also assumed to have the utility of a healed rotator cuff. Utility was expressed as QALYs. More detail on utility can be found in the Appendix.
Rotator Cuff Healing Rates and Complications
For the spectrum of full-thickness rotator cuff tears, a systematic review of thirteen studies by Slabaugh et al. showed that healing rates ranged from 55% to 88%, with an average of 79%9. This average rate is similar to the 75% rate reported by Nho et al. on a prospective cohort of rotator repairs examined at two years with ultrasound10,11. Because the latter study allowed greater detail for subsequent analysis, 75% was chosen as the base case value, and rigorous sensitivity analyses were performed around this input.
Because no literature exists on the percentage of retorn rotator cuff repairs becoming symptomatic, it was estimated by expert opinion. Of the rotator cuff repairs that had a retear, 5% were assumed to become substantially symptomatic annually and were assigned a utility of 0.66 QALY (symptomatic rotator cuff tear). Long-term retear rates of healed rotator cuff repairs are not well established in the literature. Expert opinion suggested that they occur at rates consistent with rotator cuff tears in the general population. As such, long-term retear rates were based on age and were taken from the population study reported by Yamamoto et al.5.
For complications, we assumed rates for stiffness (2.5%) and infection (0.1%) following rotator cuff repair on the basis of the available literature12,13.
Outcomes with Nonoperative Treatment
There are few high-quality studies on outcomes of nonoperative treatment for rotator cuff tears. Most studies from the literature review had sample sizes of <100 and were prospective or retrospective cohort studies. These produced a range of satisfaction rates, from 15% to 90%14-16. A 2004 literature review by Gomoll et al.17 noted that pain relief and restoration of function had been observed in 62% to 74% of patients with symptomatic rotator cuff tears confirmed through magnetic resonance imaging (MRI) or other imaging studies14,17,18. Our study assumed 68%, the midpoint of the 62% to 74% range reported, as the rate of satisfactory outcome for nonoperative treatment.
Long-Term Outcomes
There are a limited number of studies on the long-term outcomes of rotator cuff disease. Yamaguchi et al. reported that 40% of patients with asymptomatic tears had progression of tear size at an average of 5.5 years19, whereas Maman et al. reported that 52% of previously symptomatic full-thickness tears increased in size and 24% developed atrophy of the rotator cuff musculature at a mean follow-up of twenty months20. In a separate study, Yamaguchi et al. found that 51% of previously asymptomatic patients with full-thickness rotator cuff tears developed symptoms over a mean of 2.8 years with follow-up at five years21. On the basis of this study, we annualized the rate of development of symptoms in asymptomatic rotator cuff tears to 8.8% (51% per 5.6 years).
Insufficient data exist to accurately model the progression to arthropathy, and this clinical outcome was not represented in the model.
Direct Medical Costs
Since this model is performed from the societal perspective, as is recommended by the Panel on Cost-Effectiveness in Health and Medicine22-24, the modeled costs are those that are accrued to society rather than to a hospital or orthopaedic practice. The costs for nonoperative treatment and surgery for both rotator cuff repair as well as revision procedures were based on the national average Medicare reimbursements for the procedures in 2013 U.S. dollars, adjusted to reflect reimbursement for various payers, including private insurance and Workers’ Compensation (see Appendix).
Indirect Costs
Four indirect costs were modeled: probability of employment, household income, missed workdays, and disability payments. We applied an approach to infer indirect costs associated with rotator cuff tears on the basis of the methods and data reported by Dall et al.25. They linked functional limitations and economic outcomes using data from the National Health Interview Survey (NHIS), a federally sponsored national survey26. To estimate the effects of rotator cuff tears and treatment, we applied patient outcome data to the findings from Dall et al. to predict indirect costs with and without surgery for patients undergoing rotator cuff surgery. Patient outcome data were obtained from a sample of seventy-three patients who underwent surgery for a rotator cuff tear (a separate cohort from the patients used to determine utility). The sample was derived from surgical patients at a large orthopaedic surgery group. Each patient reported his or her functional outcomes at the time of the survey (between one and two years after surgery) and, on the basis of patient recall, in the weeks prior to the rotator cuff repair. We assumed that functional outcomes for symptomatic patients after treatment (whether receiving surgery or not) would be the same as those reported at baseline prior to surgery. We assumed that workers lost an average of twenty-eight additional days as a result of rotator cuff repair compared with those undergoing nonoperative treatments27. Additional details can be found in the Appendix.
Cost-Effectiveness Analysis
The principal outcome calculated was the incremental cost-effectiveness ratio (ICER), which is the ratio between the difference in costs and QALY of each strategy. Incremental cost-effectiveness ratios of <$50,000 per QALY gained were considered to be cost-effective28. In this cost-effectiveness analysis, the preferred treatment strategy was the most effective strategy with an incremental cost-effectiveness ratio that was less than the willingness of the health-care system to pay. A strategy is termed dominant when it is both less costly and more effective.
One, two, and three-way sensitivity analyses were performed on all variables in the model.
Variables deemed sensitive are those that, when varied across a reasonable range, change the preferred strategy. If the preferred strategy does not change, then the variable is termed robust. Monte Carlo analysis was used to evaluate (1) the impact of uncertainty in the model assumptions using probabilistic sensitivity analysis and (2) the impact of individual patient variability using microsimulation. These two were combined to generate 95% confidence intervals for cost and QALYs.
Source of Funding
This study was funded by the American Academy of Orthopaedic Surgeons (AAOS), National Institutes of Health, and the National Cancer Institute through grant number KM1CA156687.
Results
Cost-Effectiveness Analysis
The lifetime age-weighted mean total societal savings per patient from rotator cuff repair compared with nonoperative treatment is $13,771. The mean difference in QALYs between rotator cuff repair and nonoperative treatment was 0.62. The mean savings ranged from a positive $77,662 for the youngest cohort of patients (thirty to thirty-nine years old) to a loss of $11,997 for the oldest (seventy to seventy-nine years old) (Table II). The lifetime QALYs were consistently higher for those who received surgical treatment in all age groups. The age-weighted average difference in QALYs between the surgical and nonsurgical groups ranged from 0.97 QALY gained in the youngest cohort to 0.33 QALY gained in the oldest. Detailed cost and effectiveness statistics for a cohort representative of the annual incidence of rotator cuff repair in the U.S. is found in Table III.
TABLE II.
Results of the Base Case: Mean Societal Impact of Rotator Cuff Repair*
| Age Group | Net Societal Savings (A) | QALY (B) | Incremental Cost-Effectiveness Ratio (A/B) |
| U.S. population | $13,771 | 0.62 | Dominant |
| 30-39 yr | $77,662 | 0.97 | Dominant |
| 40-49 yr | $49,285 | 0.81 | Dominant |
| 50-59 yr | $18,215 | 0.65 | Dominant |
| 60-69 yr | –$5712 | 0.48 | $12,024/QALY |
| 70-79 yr | –$11,997 | 0.33 | $36,576/QALY |
Net societal savings represent the difference in total lifetime costs (the direct costs of treatment and indirect costs, such as lost wages) between the rotator cuff repair and nonoperative treatment. Positive numbers represent economic savings, and negative numbers represent economic losses. A strategy is termed dominant when it is both less costly and more effective. All savings are expressed in 2013 U.S. dollars. QALY = quality-adjusted life year.
TABLE III.
Results of Probabilistic Sensitivity Analysis
| Treatment Strategy* | Mean | Stand. Dev. | 95% CI for the Mean† | Median | Min. | Max. |
| Cost (2012 US$) | ||||||
| RCR | 19,366 | 2730 | 19,312-19,419 | 20,266 | 12,231 | 22,275 |
| Nonoperative | 40,457 | 32,493 | 39,820-41,093 | 34,233 | 1807 | 151,451 |
| Effectiveness (QALY) | ||||||
| RCR | 12.61 | 4.04 | 12.5-12.72 | 12.47 | 1.21 | 26.94 |
| Nonoperative | 11.96 | 3.55 | 11.86-12.06 | 11.98 | 0.89 | 24.19 |
RCR = rotator cuff repair, and QALY = quality-adjusted life year.
CI = confidence interval.
Effect of Age
For patients under the age of sixty-one years, rotator cuff repair is a dominant treatment strategy compared with nonoperative treatment. The lifetime societal direct and indirect costs across the age range of thirty to eighty years is shown in Figure 2, with the area between nonoperative costs and operative costs representing societal savings for patients who are sixty-one years old or younger. For patients over the age of sixty-one years, societal costs for surgery exceed those for nonoperative treatment, indicating negative societal savings. The incremental cost-effectiveness ratio, however, remained well below the health-care system’s willingness-to-pay thresholds for those over sixty-one years old. Therefore, rotator cuff repair produces societal cost savings for patients under the age of sixty-one years and is cost-effective for all patients.
Fig. 2.
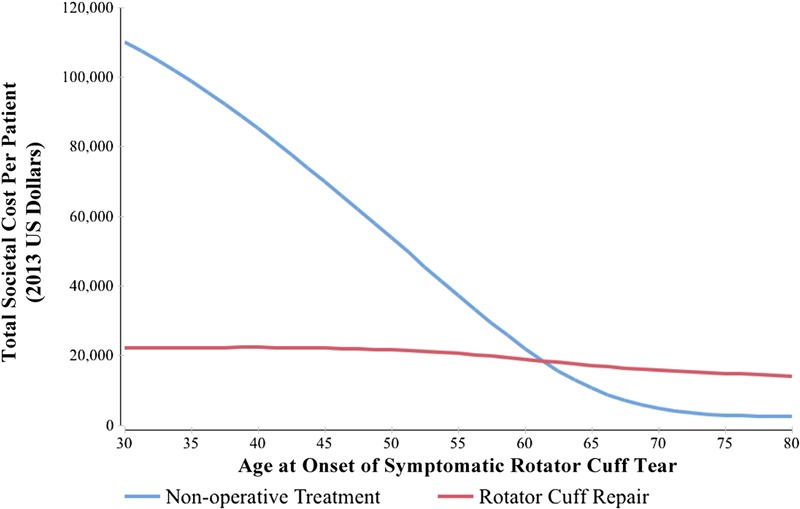
Sensitivity analysis on the age at nonoperative treatment of rotator cuff tear or rotator cuff repair and total societal savings.
Probabilistic Sensitivity Analysis
Rotator cuff repair was the preferred cost-effective strategy in 72.2% of the samples (70% with cost only as the outcome). Microsimulation, with a cohort representative of the annual U.S. incidence of rotator cuff repair, demonstrated that rotator cuff repair was the preferred cost-effective strategy in 48% of trials (44% with cost only as the outcome). This value suggests that, for 52% of patients, likely those who improve with nonoperative treatment or experience symptomatic retears, nonoperative treatment is preferred. However, the cost savings to society for patients for whom surgery is the preferred strategy far exceeds the savings from those patients when nonoperative treatment is the preferred strategy, which causes the mean cost of rotator cuff repair for everyone under the age of sixty-one years to be less than that of nonoperative treatment.
Threshold Analysis
Results from threshold analyses demonstrate that our estimates of the cost-effectiveness of rotator cuff repair are relatively robust to any one of the underlying model assumptions. The most influential variable on cost-effectiveness appears to be the response to nonoperative treatment. The break-even point for operative treatment of full-thickness rotator cuff tears in terms of societal savings is at 88% effectiveness of nonsurgical treatment, which is outside the range of values reported in the literature. Greater detail on the sensitivity analyses of specific variables appears in the Appendix.
Discussion
The model employed in this study estimated a lifetime societal savings (net present value in 2013 U.S. dollars) of approximately $3.44 billion from the approximately 250,000 rotator cuff repairs ($13,771 per patient) performed annually in the U.S. The reduced indirect costs resulting from the operative treatment of rotator cuff disease more than offset the additional direct costs of treatment in patients under the age of sixty-one years. Furthermore, for all ages, rotator cuff repair generates increased utility compared with nonoperative treatment and is cost-effective. The findings provide a rationale for payer coverage of rotator cuff repair after an initial trial of nonoperative treatment.
This study is the first, to our knowledge, to comprehensively examine the societal impact of rotator cuff disease and its treatments. Our cost-effectiveness results are lower than those reported previously in the literature. Vitale et al., for example, found that rotator cuff repair yielded cost-effectiveness ratios ranging from $13,093 to $3092 per QALY29. These values were based on the other two major indirect measures of utility, the Health Utilities Index (0.85 QALY for post-rotator cuff repair and 0.80 QALY for the preoperative state) and the EuroQoL index (0.75 QALY for post-rotator cuff repair and 0.55 QALY for the preoperative state). The difference between these numbers and those in our study is due to the lifetime perspective of our model and the inclusion of indirect costs.
The sensitivity analyses are revealing and must be considered with regard to societal cost and cost-effectiveness. First, our analysis demonstrates that the cost-effectiveness of rotator cuff repair is robust (Table IV). Second, even if indirect costs are completely excluded, rotator cuff repair is still cost-effective although not cost-saving. Only one variable is sensitive within a reasonable range: the success rate of nonoperative treatment. This rate must be >90% for the nonoperative treatment strategy to be preferred. The robustness of rotator cuff repair to cost-effectiveness was also supported using probabilistic sensitivity analysis.
TABLE IV.
Results of the Threshold Analyses*
| Base Case | RCR Cost Threshold† | RCR Cost-Effectiveness Threshold | |
| Transition probabilities | |||
| Healing rate with RCR | 75% | Robust | Robust |
| Recurrence of symptomatic RCT | 8.8% | Robust | Robust |
| Success of nonoperative treatment | 68% | 88% | Robust |
| Durability of the outcome of RCR | Lifetime‡ | 3.51 yr | Robust |
| Number of full workdays missed recovering from RCR | 28 | 153 | Robust |
| Rate of symptomatic nonhealed RCR | 5% | 97% | Robust |
| Cost§ | |||
| Nonoperative treatment | $1802 | Robust | Robust |
| RCR | $15,063 | $23,630 | $46,810 |
| Indirect costs of a symptomatic RCT | $6638 | $1250 | Robust |
| Utility (QALY) | |||
| Healed rotator cuff or asymptomatic tear | 0.74 | NA | 0.62 |
| Symptomatic RCT | 0.66 | NA | 0.77 |
| Age (yr) | 56 | 61.4 | Robust |
A variable is termed robust if the preferred strategy does not change across the range of values tested. RCR = rotator cuff repair, RCT = rotator cuff tear, and QALY = quality-adjusted life year.
NA = not applicable.
After a healed RCR, patients return to retear rates consistent with population rates for primary RCTs.
The values are given as the cost per episode.
When total societal cost is considered, several variables are highly sensitive, including success rates of nonoperative treatment and primary rotator cuff repair, initial costs of nonoperative treatment and primary rotator cuff repair, age, and durability of the benefit of rotator cuff repair. The rate of symptom recurrence with either strategy is robust (Table IV). These findings suggest that, when total societal cost only is considered, patient characteristics and treatment characteristics as well as the perspective of the particular stakeholders are highly influential in determining the preferred strategy.
There are a number of limitations of this study to consider. First, patients in the nonoperative treatment arm of the Markov model were not allowed to cross over to the rotator cuff repair arm, even if they responded poorly to nonoperative treatment. While this is an unlikely treatment pattern, the model assumption is appropriate, given that we were concerned with the costs and benefits of surgical care and examined what would have happened to surgical patients without access to operative treatment. Second, evidence to support some of the model assumptions is limited. Very few randomized controlled trials are designed to test the effectiveness of operative treatment of rotator cuff tears. The utility values used, while being generated by a validated outcome measure, were obtained from the experience of one surgeon at an academic medical center and may not represent the national mean, although sensitivity analysis on utility did not change the preferred treatment strategy. In addition, little is known about the longer-term outcomes regarding relapse, response to repeated rounds of nonoperative treatment, and progression to rotator cuff arthropathy. Further, while data exist on the rate of symptom development in rotator cuff disease, the mean duration of follow-up is less than five years, making extrapolation to an entire lifetime less certain. These weaknesses are important, but sensitivity analyses on these factors did not materially alter our findings.
Third, estimates of indirect costs associated with rotator cuff tears do not exist in the literature. We inferred these costs by linking estimates of the relationship between rotator cuff tears and functional limitations to estimates of the relationship between functional limitations and indirect cost factors. While the study contributes to our understanding of the full societal effects of rotator cuff tears, additional research is needed to confirm the study findings and caution should be taken in using the results to guide the treatment of individual patients.
Although rotator cuff repair is cost-saving across all patients, nonoperative treatment is the preferred strategy for a large number of patients. The challenge to maximize the value of treatment for rotator cuff disease overall is to better distinguish between the patients who would benefit more from nonoperative treatment and those who would benefit more from operative treatment. Furthermore, differences in the type and quality of both operative and nonoperative treatment could lead to further individual variation. Because the study focused on the cohort of patients receiving surgery, the results of this study should not be interpreted as suggesting that all rotator cuff tears require surgery. Rather, the results show that rotator cuff repair has an important role in minimizing the societal burden of rotator cuff disease.
In summary, the economic burden to society of rotator cuff tears is substantial and rotator cuff repair may play an important role in reducing that burden. We estimate that the surgical procedures for this condition performed each year in the U.S. will generate lifetime societal savings of approximately $3.44 billion. Rotator cuff repair is both cost-saving for society in younger patients and cost-effective for all patient age groups.
Appendix
A detailed description of the technical aspects of the analyses and tables showing annual disability payments as well as the Current Procedural Terminology (CPT) codes, rate of occurrence of concomitant procedures, and 2013 average Medicare reimbursements are available with the online version of this article as a data supplement at jbjs.org.
Supplementary Material
Disclosure of Potential Conflicts of Interest
A detailed description of the technical aspects of the analyses and tables showing annual disability payments as well as the Current Procedural Terminology (CPT) codes, rate of occurrence of concomitant procedures, and 2013 average Medicare reimbursements
Acknowledgments
Note: The authors thank the members of the AAOS Value Project Team for their valuable comments on earlier drafts of the paper. The authors also thank the Rothman Institute for providing patient outcome data, a panel of clinical experts who provided additional review and input, and Josh Saavoss and Sheila Sankaran for their editorial assistance.
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, one or more of the authors has had another relationship, or has engaged in another activity, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Oh LS, Wolf BR, Hall MP, Levy BA, Marx RG. Indications for rotator cuff repair: a systematic review. Clin Orthop Relat Res. 2007 Feb;455:52-63 [DOI] [PubMed] [Google Scholar]
- 2.Praemer A, Furner S, Rice DP. Musculoskeletal conditions in the United States. 2nd ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1999 [Google Scholar]
- 3.Seida JC, LeBlanc C, Schouten JR, Mousavi SS, Hartling L, Vandermeer B, Tjosvold L, Sheps DM. Systematic review: nonoperative and operative treatments for rotator cuff tears. Ann Intern Med. 2010 Aug 17;153(4):246-55 Epub 2010 Jul 05 [DOI] [PubMed] [Google Scholar]
- 4. HCUP State Ambulatory Surgery Databases. Healthcare Cost and Utilization Project (HCUP). 2007-2009. Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/sasdoverview.jsp.
- 5.Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H, Kobayashi T. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010 Jan;19(1):116-20 [DOI] [PubMed] [Google Scholar]
- 6.Smith DH, Gravelle H. The practice of discounting in economic evaluations of healthcare interventions. Int J Technol Assess Health Care. 2001 Spring;17(2):236-43 [DOI] [PubMed] [Google Scholar]
- 7.Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002 Mar;21(2):271-92 [DOI] [PubMed] [Google Scholar]
- 8.Walters SJ, Brazier JE. What is the relationship between the minimally important difference and health state utility values? The case of the SF-6D. Health Qual Life Outcomes. 2003;1:4 Epub 2003 Apr 11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Slabaugh MA, Nho SJ, Grumet RC, Wilson JB, Seroyer ST, Frank RM, Romeo AA, Provencher MT, Verma NN. Does the literature confirm superior clinical results in radiographically healed rotator cuffs after rotator cuff repair? Arthroscopy. 2010 Mar;26(3):393-403 [DOI] [PubMed] [Google Scholar]
- 10.Nho SJ, Brown BS, Lyman S, Adler RS, Altchek DW, MacGillivray JD. Prospective analysis of arthroscopic rotator cuff repair: prognostic factors affecting clinical and ultrasound outcome. J Shoulder Elbow Surg. 2009 Jan-Feb;18(1):13-20 [DOI] [PubMed] [Google Scholar]
- 11.Nho SJ, Shindle MK, Adler RS, Warren RF, Altchek DW, MacGillivray JD. Prospective analysis of arthroscopic rotator cuff repair: subgroup analysis. J Shoulder Elbow Surg. 2009 Sep-Oct;18(5):697-704 Epub 2009 Mar 09 [DOI] [PubMed] [Google Scholar]
- 12.Huberty DP, Schoolfield JD, Brady PC, Vadala AP, Arrigoni P, Burkhart SS. Incidence and treatment of postoperative stiffness following arthroscopic rotator cuff repair. Arthroscopy. 2009 Aug;25(8):880-90 [DOI] [PubMed] [Google Scholar]
- 13.Randelli P, Spennacchio P, Ragone V, Arrigoni P, Casella A, Cabitza P. Complications associated with arthroscopic rotator cuff repair: a literature review. Musculoskelet Surg. 2012 Jun;96(1):9-16 [DOI] [PubMed] [Google Scholar]
- 14.Bokor DJ, Hawkins RJ, Huckell GH, Angelo RL, Schickendantz MS. Results of nonoperative management of full-thickness tears of the rotator cuff. Clin Orthop Relat Res. 1993 Sep;(294):103-10 [PubMed] [Google Scholar]
- 15.Goldberg BA, Nowinski RJ, Matsen FA., 3rd Outcome of nonoperative management of full-thickness rotator cuff tears. Clin Orthop Relat Res. 2001 Jan;(382):99-107 [DOI] [PubMed] [Google Scholar]
- 16.Hawkins RH, Dunlop R. Nonoperative treatment of rotator cuff tears. Clin Orthop Relat Res. 1995 Dec;(321):178-88 [PubMed] [Google Scholar]
- 17.Gomoll AH, Katz JN, Warner JJ, Millett PJ. Rotator cuff disorders: recognition and management among patients with shoulder pain. Arthritis Rheum. 2004 Dec;50(12):3751-61 [DOI] [PubMed] [Google Scholar]
- 18.Wirth MA, Basamania C, Rockwood CA., Jr Nonoperative management of full-thickness tears of the rotator cuff. Orthop Clin North Am. 1997 Jan;28(1):59-67 [DOI] [PubMed] [Google Scholar]
- 19.Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006 Aug;88(8):1699-704 [DOI] [PubMed] [Google Scholar]
- 20.Maman E, Harris C, White L, Tomlinson G, Shashank M, Boynton E. Outcome of nonoperative treatment of symptomatic rotator cuff tears monitored by magnetic resonance imaging. J Bone Joint Surg Am. 2009 Aug;91(8):1898-906 [DOI] [PubMed] [Google Scholar]
- 21.Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001 May-Jun;10(3):199-203 [DOI] [PubMed] [Google Scholar]
- 22.Siegel JE, Weinstein MC, Russell LB, Gold MR; Panel on Cost-Effectiveness in Health and Medicine. Recommendations for reporting cost-effectiveness analyses. JAMA. 1996 Oct 23-30;276(16):1339-41 [DOI] [PubMed] [Google Scholar]
- 23.Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB. Recommendations of the Panel on Cost-effectiveness in Health and Medicine. JAMA. 1996 Oct 16;276(15):1253-8 [PubMed] [Google Scholar]
- 24.Russell LB, Gold MR, Siegel JE, Daniels N, Weinstein MC; Panel on Cost-Effectiveness in Health and Medicine. The role of cost-effectiveness analysis in health and medicine. JAMA. 1996 Oct 9;276(14):1172-7 [PubMed] [Google Scholar]
- 25.Dall TM, Gallo P, Koenig L, Gu Q, Ruiz D. Modeling the indirect economic implications of musculoskeletal disorders and treatment. Cost Eff Resour Alloc. 2013;11(1):5 Epub 2013 Mar 15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. 2010 national health interview survey. Hyattsville, MD: National Center for Health Statistics; June 2011. Accessed 2013 Aug 8.
- 27.Work Loss Data Institute Official disability guidelines: special edition top 200 conditions. 17th ed. Encinitas, CA: Work Loss Data Institute; 2012 [Google Scholar]
- 28.Grosse SD. Assessing cost-effectiveness in healthcare: history of the $50,000 per QALY threshold. Expert Rev Pharmacoecon Outcomes Res. 2008 Apr;8(2):165-78 [DOI] [PubMed] [Google Scholar]
- 29.Vitale MA, Vitale MG, Zivin JG, Braman JP, Bigliani LU, Flatow EL. Rotator cuff repair: an analysis of utility scores and cost-effectiveness. J Shoulder Elbow Surg. 2007 Mar-Apr;16(2):181-7 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest
A detailed description of the technical aspects of the analyses and tables showing annual disability payments as well as the Current Procedural Terminology (CPT) codes, rate of occurrence of concomitant procedures, and 2013 average Medicare reimbursements


