Abstract
Background:
Psychosexual problems are very common presentation, be it with psychiatric or physical illness but there are very few studies available on psychosexual disorders especially in the Indian context. Indian society is deeply ingrained in customs and several misconceptions, myths, prejudices, and social taboos are attached to sex which makes it further very difficult to tackle.
Objectives:
The aim of this current study was to descriptively analyze the nature of sexual disorders in a tertiary care center.
Materials and Methods:
The current retrospective chart review included 698 consecutive subjects seeking treatment for their psychosexual problems at the Sexual Clinic, Department of Psychiatry, Dr. Ram Manohar Hospital, New Delhi (between 2006 and 2010).
Results:
This study observed erectile dysfunction (ED) (29.5%), Premature ejaculation (PME) (24.6%), Dhat syndrome (DS) (18.1%), and ED with PME (17.5%) as the common sexual dysfunctions leading to treatment seeking. DS was the major complaint among younger and unmarried individuals. We observed more married individuals seeking treatment for sexual disorders.
Conclusions:
These findings provide important information on a relatively under-researched area.
Keywords: Dhat, ejaculation, erectile dysfunction, sexual
INTRODUCTION
Sexual disorders lay among the most prevalent psychological disorders in general population.[1] Overall, studies conducted worldwide have reported the prevalence of sexual disorders in the range of 10-25% among men and 25-64% among women.[2] Studies regarding prevalence of sexual problems have varied findings. Although few studies reported the most prevalent sexual problem to be premature ejaculation (PME) (30%),[3] other studies report that impotence or inhibited desire to be more common.[4,5] Studies have suggested a community prevalence rate ranging from of 4-10% for male orgasmic disorder, 4-9% for male erectile disorder, 5-10% for female orgasmic disorder, and 36-38% for PME.[2]
Multiple risk factors alone or in combination are associated with sexual dysfunction such as general health status of the individual, chronic illnesses particularly diabetes mellitus and cardiovascular disease, genitourinary disease, psychiatric/psychological disorders, and drugs (both prescribed and abused) and socio-demographic conditions.[6] Among the psychiatric population, sexual dysfunction is attributed to disorder-related factors as well as a side effect due to medications. While being medically managed, sexual problems have been reported in about 30-60% of patients with schizophrenia, up to 78% of patients with depression, and up to 80% in patients suffering from anxiety disorders.[7]
Partly as a consequence of the influence of cultural factors in their development, prevalence rates vary in different communities and due to the very nature of problems and psychological consequences, it is at times difficult to assess the exact prevalence of the sexual dysfunction. It is even more difficult in developing countries like India. In India, the pathway to care is hindered as large number of patients suffering from psychosexual problems tends to visit “quacks” and “sex clinics” rather than to the hospital setting. The problems are intensified by ill-advice from co-workers, friends, elders, and popular cheap literature on sex which heightens the fears, guilt, shame, and anxiety over the problem. Individuals then finally may turn up to hospitals for treatment seeking.
As literature lacks large-scale epidemiologic data on sexual disorders, smaller studies should be integrated to obtain population estimates regarding the prevalence of sexual disorders. We aimed to add to the existing data, the prevalence of sexual problems in patients coming to sexual clinic in a tertiary care center.
MATERIALS AND METHODS
This study included 698 subjects seeking treatment for their psychosexual problems at the Sexual Clinic, Department of Psychiatry, Dr. Ram Manohar Hospital, New Delhi. Data were collected retrospectively from case notes. The chart analysis of all consecutive subjects (between 2006 and 2010) was carried out.
Performa was prepared for the study which included demographic information including age, marital status, occupation, employment, socio-economic status, educational status, religion, catchment area, type of family, and their family background. Detailed family history of any substance use and psychiatric illness was elicited. Information was sought regarding the exact nature and duration of onset of the problem, associated problems in different phases of sexual response cycle, and presence of any performance anxiety. History regarding substance abuse was extracted along with detailed evaluation of any recent or ongoing stressor, past and presenting psychiatric illness including any personality traits or disorder, and co-morbid physical ailments. History of any indigenous medicines taken by these patients for the treatment of their psychosexual problem was assessed along with the prior types of consultations for the psychosexual problems. The diagnosis as assessed by the treating psychiatrist using standard definitions and criteria in accordance to international classification of diseases version 10 were evaluated.
The data were imputed and analyzed using SPSS, version 17.0. Descriptive analysis was done for the data and Pearson's correlation coefficient was calculated to find the association among the parameters. The level of statistical significance was kept at P < 0.05.
RESULTS
Socio-demographic parameters
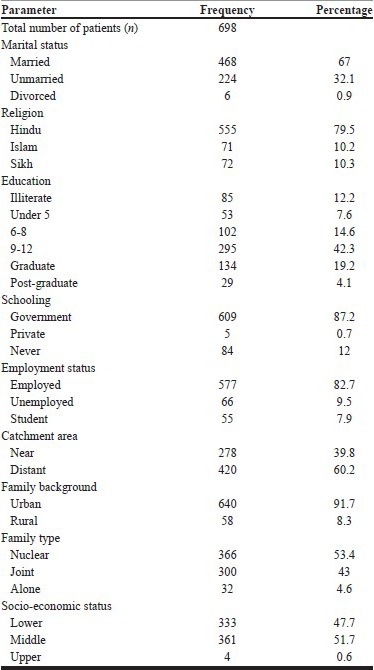
All the 698 subjects included in study were male with mean age of 30.3±8.6 years (range: 17-70). Table 1 represents the socio-demographic data obtained. More than two-thirds were married with the majority belonging to Hindu religion (79.5%). Most subjects were educated (88%), employed (82.7%), and belonged to urban community (91.7%). About 51% and 47% of subjects belonged to middle and lower socio-economic status, respectively. Only 4.6% of subjects were staying alone.
Table 1.
Socio-demographic parameters percentage
Clinical parameters
There was no family history of any substance abuse or dependence. A family history of psychiatric illness was present in only two subjects: Depression in one and psychosis in other.
Almost half of the patients had taken prior consultation with a physician. As shown in Table 2, about two-thirds of the subjects were having one or the other stressors in their life. None of the subjects are found to be suffering from any kind of personality disorder. Psychiatric illness apart from the sexual problems was observed in 21.6%. Most of the subjects were suffering from depression (15.1%), followed by anxiety disorder (4.4%) and psychosis (1.3%). Two subjects were suffering from epilepsy. The severity of psychiatric illness was not written. Very few subjects were suffering from psychiatric illness prior to their substance use. Most of the subjects were not having any co-morbid physical illness.
Table 2.
Clinical profile
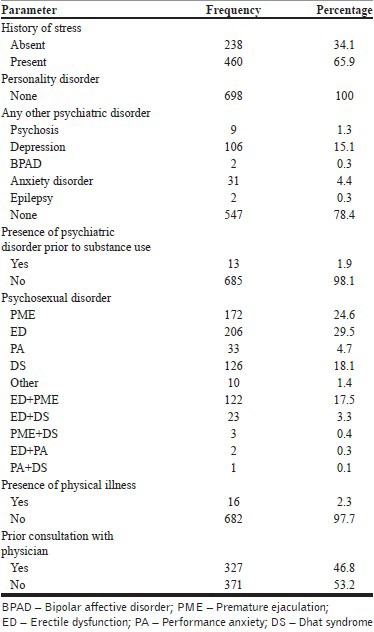
Of the various psychosexual disorders observed in our study, erectile dysfunction (ED) was most commonly reported (29.5%), followed by PME in 24.6% subjects and Dhat syndrome (DS) in 18.1% subjects. Among the subjects having more than one psychosexual disorder, ED with PME was most commonly reported (17.5%).
Sexual dysfunction and substance use
A history of current use of substance was reported in 26.5% of subjects. Current use of substance meant use of any substance within 1 month of presenting to the psychiatric Out Patient Clinic to denote active use of substance. The substance commonly reported was alcohol (19.2%). Nicotine use was reported by 6.3%, cannabis use by 1%, and opioid use by 0.1%. The details of substance use are provided in Tables 3 and 4 and Figures 1 and 2.
Table 3.
Substance use details
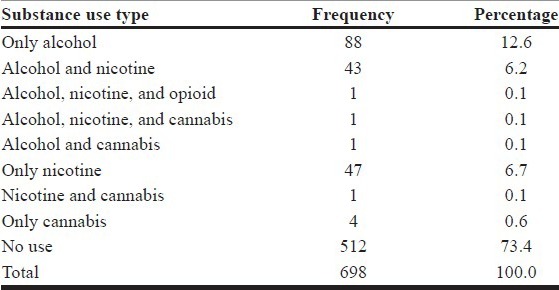
Table 4.
Psychosexual disorders relationship to substance use
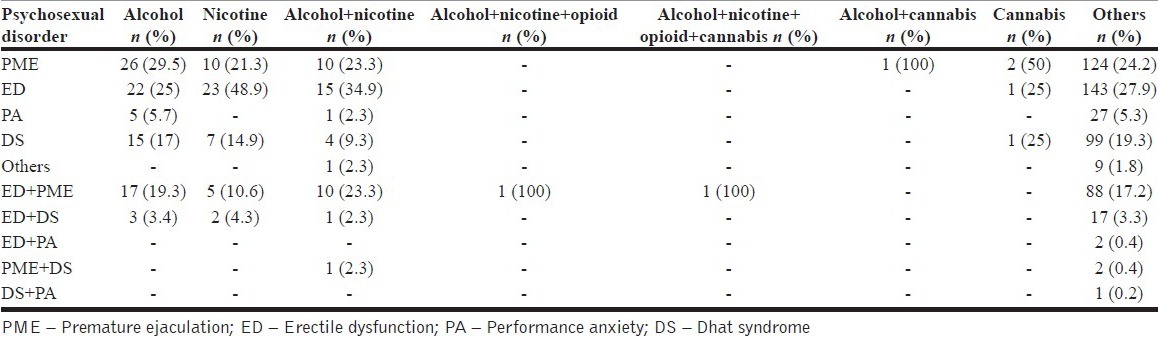
Figure 1.
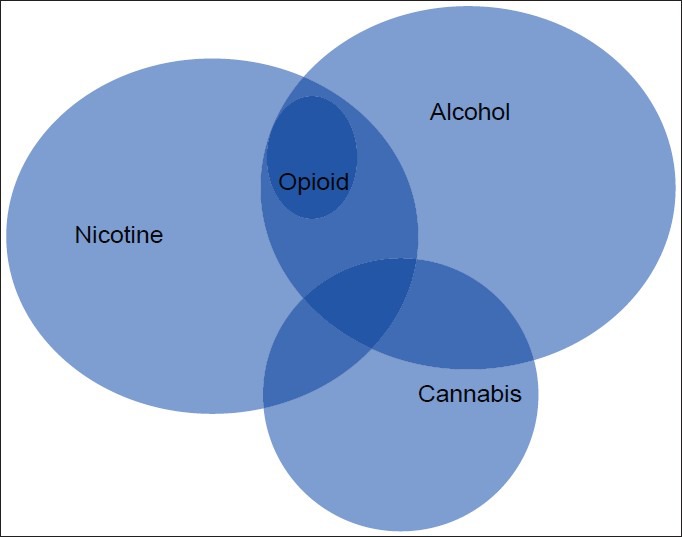
Inter-relationship among substance use in individuals with sexual disorders abusing substances
Figure 2.
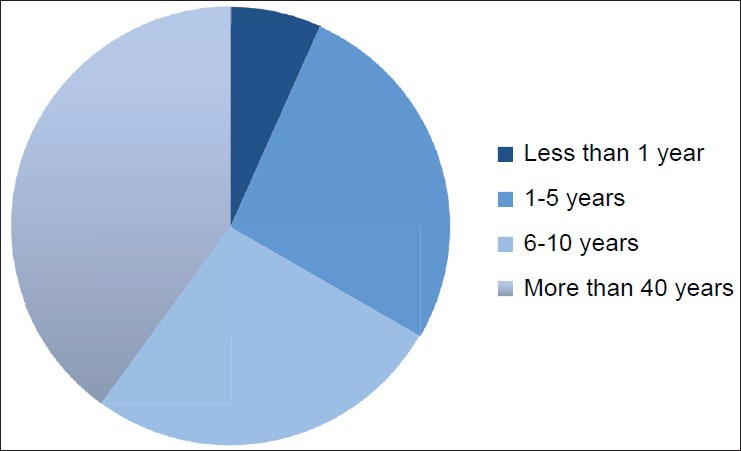
Duration of substance use details
Even after exclusion of substance use, ED was the most commonly reported sexual disorder (27.9%), followed by PME in 24.2% subjects and DS in 19.3% subjects. Among the subjects having more than one psychosexual disorder, ED with PME was most commonly reported (17.2%).
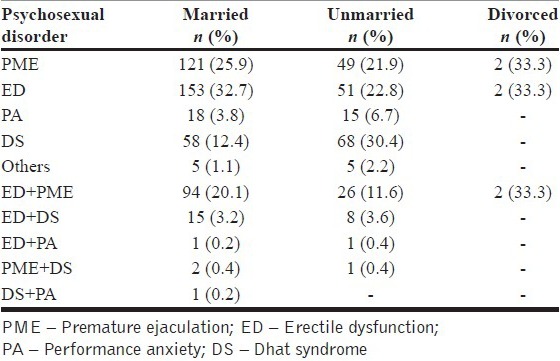
Sexual dysfunction and marital status
Among the married individuals, 32.7% had ED, 25.9% had PME, and about 20% of subjects had both, while DS comprised the majority (30.4%) among the unmarried population [Table 5]. Being married was significantly correlated (Pearson's correlation, r=0.08, P=0.03) to having any psychosexual disorder.
Table 5.
Sexual dysfunction in married versus unmarried
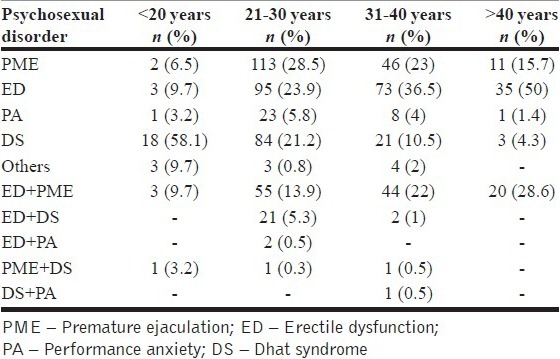
Sexual problems in different age groups
DS was reported by all age groups and dominated the nature of presenting complaints in the younger age group of below 20 years (58%) as shown in Table 6. The age group of 21-30 years was significantly correlated to have any psychosexual disorder among the total sample (r=0.07, P=0.02).
Table 6.
Sexual problems in different age groups
There was no correlation of sexual disorders to overall substance use, education, schooling, employment status, family background, family type, socio-economic status, family history of psychiatric illness, physical illness, and prior physician consultation.
DISCUSSION
This study observed that ED was the most commonly reported sexual disorder (29.5%), compared to PME (24.6%), DS (18.1%) and ED with PME (17.5%). Although some previous studies present similar pattern of data although with variable frequencies,[8,9,10] others have reported PME as a more common disorder.[11] A recent study, from north India, reported DS to be more common sexual disorder (35%), where 32% had DS with ED and 26% had DS with PME.[12] The difference could be due to the smaller sample size in above study compared to our study (100 vs. 698 subjects, respectively).
The major proportion of presenting complaints being ED or PME in our and other similar studies could be attributed to the reason that erectile impotence in males is considered to be very serious inadequacy in Indian society and poses higher degree of psychological stress on the patient due to which most of the patients having erectile impotence come for consultation and professional help to the hospital setting while other sexual complaints may go neglected.
Our study showed no female patient presenting with sexual complaints. This may be due to various reasons such as lack of knowledge regarding sexual disorders in this subgroup of population, females seeking help from gynecologists only, and embarrassment to come forth with sexual complaints in a male dominated society.
The mean age of the patients was 30 years in this study sample, which is within the range mentioned by other similar studies with most common age of presentation being 16-45 years.[13]
In study by Gupta et al.,[10] the younger age group (<20 years) had complaints of DS in 23.5%, ED in 14.7%, and PME in 11.7%, whereas our study reported prevalence rates of 58.1%, 9.7%, and 6.5%, respectively. In the same study,[10] in 20-30 years group, ED was found in 34.6%, PME in 28.7%, and DS in 18.8%, while we observed 23.9%, 28.5%, and 13.9% proportion of subjects, respectively, in this study. In 31-40 years group, the study reported ED in 66.6%, PME in 25%, and nil in DS, while we found in 36.5%, 23%, and 22%, respectively. In older adults (>40 years group), while the study reported 100% subjects complaining of ED, we observed ED in 50%, DS in 28.6%, and PME in 15.7%. Although both the studies infer that DS is commoner among younger age group (more proportion of subjects in our study, 58% vs. 23.5%) and ED among older age group (lesser proportion of subjects in our study, 50% vs. 100%), DS forms a significant proportion of complaint among older age group also.
We observed more married individuals seeking treatment for sexual disorders (67%), which is discrepant in previous literature from India.[13,14]
Similar to previous literature, DS was proportionately seen more in unmarried than married individuals, whereas PME and ED were more commonly observed vice-versa.[13,14] Bagadia et al. (1972) found anxiety over nocturnal emission (65%) and passing semen in urine (47%) are main problems in the unmarried group; whereas impotence (48%), PME (34%) and passing semen in urine (47%) were common in married group.[15] The reason for the above findings could be lack of sexual knowledge coupled with less sexual inexperience in unmarried males and shyness in discussing such issues with others (family, friends, or doctor) as, in Indian culture, pre-marital enrolment in sexual activity or self-stimulation is not very common and considered atrocious. The lack of education regarding sexual health may have been responsible for seeking help when the sexual situation arose after marriage.
Majority of patients were from urban area (91.7%). This may be due to the ignorance regarding the treatment facilities of such problems available in general hospital in rural area or due to more stigma/myths/lack of knowledge regarding the nature of the illness in rural area.
We found 21. 6% of subjects having more than one type of sexual dysfunctions, which was within the range of previous studies reporting a prevalence of 16-53% in Indian setting.[12,16] Performance anxiety, performance in haste, guilt about previous sexual experience such as masturbation, pre-marital and extramarital sexual contact, and misconcepts about sexuality are some factors which can lead to development of multiple psychosexual problems.
In our study, commonest psychiatric illness in patients presenting with sexual dysfunctions was depression (15%), which is in concordance with study by Kumar et al. reporting neurotic depression to be 15%.[13] But while that study found anxiety disorders in similar proportion (16%), we observed it only in 4.4% subjects. Although one study reported prevalence of anxiety and depressive disorders in 30% and 20% individuals with sexual disorders, respectively,[12] another study found anxiety state (57%), schizophrenia (16%), and reactive depression (16%) as common psychiatric conditions.[15]
In our study, we did not find any personality traits or disorders in the sample contrary to the previous study which found 37% of the male patients having anxious personality disorder.[15] The reason for the discrepancy could be more elaborate personality assessment in the previous study which was prospective while we did a retrospective chart review. There is a need for better assessment of personality in sexual clinics for enhanced patient care.
Although we observed only two subjects having positive family history of psychiatric illness, previous literature reports contrary findings with as high as 31% of individuals having positive family history of psychiatric illness.[15]
The sample represented mainly Hindu population (79.5%) belonging to middle and lower classes (99.4%) which is comparable to other studies done in Indian set up.[13]
The percentage distributions of substance use in our study sample were in accordance with the various epidemiological studies done on substance use in India in general population.[17] There was no significant difference in the prevalence rates of sexual disorders when presence of substance use was included or excluded.
Among substance users, PME was the most common sexual dysfunction except in nicotine users in whom ED was the most common presentation. It was also found that in individuals consuming more than one substance, either ED or more than one psychosexual disorder was present. Other studies have also reported slight preponderance (37.5%) of PME among alcohol users.[18] A recent study reported sexual problems to be in 1% individuals using nicotine.[19] Indian studies in substance users have reported co-morbid sexual dysfunctions in about 23%.[20] Reversible vagal neuropathy due to use of alcohol is the most common cause besides alteration of gonadal hormones being noted so far in various studies.[21,22] Raised nicotine levels in smokers may increase the sympathetic tone in the penis, interfering with the relaxation of intra-corporeal smooth muscle.[23] Opioids impact the neuro-endocrine system inhibiting gonadotropin-releasing hormone resulting in decreased sexual desire and decreased testosterone levels.[24] Cannabis may cause sexual dysfunction in the long term in high doses.[25]
We found majority of individuals reporting stress (65.9%) like previous literature.[15] Components of stress have been reported as interpersonal stress in 22%, financial stress in 52%, and occupational stress in 32% of patients.[15] Stress may cause neuro-endocrinal changes particularly mediating disturbances in Hypothalamic-Pituitary-Axis which may secondarily lead to sexual dysfunctions. There is a need to understand the relationship between them using large-scale epidemiological and biological-based studies.
Almost half of the patients had prior consultations with physician before consulting to psychiatric care which is in accordance with the basic trend of the Indian population with psychiatric illness, i.e., consulting non-psychiatrist first, be it a faith healer or local physician.[10,26] This could be due to the significant stigma still existing in our country to consult a psychiatrist and also a general tendency to keep the sexual problems secretive. A more elaborative sexual education which would lead to timely medical consultation with qualified practitioner to deal the problem effectively is the need of the hour.
In our study, only 2.3% of patients had co-morbid physical illness and there was no suggestive history of spinal surgery or trauma. Studies have reported almost 15% of patients having physical illness.[15] The possibility of very few organic conditions could be due to the study being conducted in tertiary hospital where mostly referred cases approach.
Although this study is limited in generalization due to being conducted as a retrospective chart review of a clinic-based population, it associates high prevalence of sexual disorders in the community. There is a need for sexual health education among general population. Although further studies need to focus on biological understanding of sexual dysfunctions, large-scale epidemiological-based studies are needed in the continent to assess the knowledge regarding sexual health and develop policies for enhancing knowledge.
CONCLUSION
This study observed ED (29.5%), PME (24.6%), DS (18.1%), and ED with PME (17.5%) as the common sexual dysfunctions leading to treatment seeking. DS is the major complaint among younger and unmarried individuals. We observed more married individuals seeking treatment for sexual disorders. The lack of education regarding sexual health may have been responsible for seeking help when the sexual situation arose after marriage. There seems to be a significant stigma still existing in India to consult a psychiatrist and also a general tendency to keep the sexual problems secretive.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Sadock VA. Normal human sexuality and sexual dysfunctions. In: Sadock BJ, Sadock VA, Kaplan HI, editors. Kaplan and Sadock's Comprehensive Textbook of Psychiatry. 8th ed. Philadelphia: Lippincott Williams and Wilkins; 2005. pp. 1903–36. [Google Scholar]
- 2.Spector IP, Carey MP. Incidence and prevalence of the sexual dysfunctions: A critical review of the empirical literature. Arch Sex Behav. 1990;19:389–408. doi: 10.1007/BF01541933. [DOI] [PubMed] [Google Scholar]
- 3.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: Prevalence and predictors. JAMA. 1999;281:537–44. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 4.Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: Results of the Massachusetts Male Aging Study. J Urol. 1994;151:54–61. doi: 10.1016/s0022-5347(17)34871-1. [DOI] [PubMed] [Google Scholar]
- 5.Líndal E, Stefànsson JG. The lifetime prevalence of psychosexual dysfunction among 55-57-year-olds in Iceland. Soc Psychiatry Psychiatr Epidemiol. 1993;28:91–5. doi: 10.1007/BF00802098. [DOI] [PubMed] [Google Scholar]
- 6.Weinhardt LS, Carey MP. Prevalence of erectile disorder among men with diabetes mellitus: Comprehensive review, methodological critique, and suggestions for future research. J Sex Res. 1996;33:205–13. [Google Scholar]
- 7.Balon R. Introduction: New developments in the area of sexual dysfunction(s) Adv Psychosom Med. 2008;29:1–6. doi: 10.1159/000126619. [DOI] [PubMed] [Google Scholar]
- 8.Nakara B, Wig NN, Verma VK. A study of male potency disorders. Indian J Psychiat. 1977;19:13. [Google Scholar]
- 9.Avasthi A, Basu D, Kulhara P, Banerjee ST. Psychosexual dysfunction in Indian male patients: Revisited after seven years. Arch Sex Behav. 1994;23:685–95. doi: 10.1007/BF01541819. [DOI] [PubMed] [Google Scholar]
- 10.Gupta SK, Dayal S, Jain VK, Kataria U, Relhan V. Profile of male patients with psychosexual disorders. Indian J Sex Trans Dis. 2004;25:33–7. [Google Scholar]
- 11.Kendurkar A, Kaur B, Agarwal AK, Singh H, Agarwal V. Profile of adult patients attending a marriage and sex clinic in India. Int J Soc Psychiatry. 2008;54:486–93. doi: 10.1177/0020764008090795. [DOI] [PubMed] [Google Scholar]
- 12.Bhatia MS, Jhanjee A, Srivastava S. Pattern of Psychosexual Disorders among males attending Psychiatry OPD of a Tertiary Care Hospital. Delhi Psychiatry J. 2011;14:266–9. [Google Scholar]
- 13.Kumar S, Agarwal AK, Trivedi JK. Neurosis and sexual behaviour in men. Indian J Psychiatry. 1983;25:190–7. [PMC free article] [PubMed] [Google Scholar]
- 14.Varma VK, Wig NN, Nakral BRS. Sexual behaviour in the adult north Indian male (a study of 150 patients of male potency disorders) Indian J Psychiatry. 1978;20:178–82. [Google Scholar]
- 15.Bagadia VN, Dave KP, Pradhan PV, Shah LP. Study of 258 male patients with sexual problems. Indian J Psychiatry. 1972;14:143–51. [Google Scholar]
- 16.Banerjee G, Dutta AK, Nandi DN, Banerjee G, Sen B. A study of psychiatric morbidity in married males with sexual dysfunction. Indian J Psychiatry. 1987;29:139–41. [PMC free article] [PubMed] [Google Scholar]
- 17.Basu D, Mattoo SK. Epidemiology of substance abuse in India: Methodological issues and future perspectives. Indian J Psychiatry. 1999;41:145–53. [PMC free article] [PubMed] [Google Scholar]
- 18.Arackal BS, Benegal V. Prevalence of sexual dysfunction in male subjects with alcohol dependence. Indian J Psychiatry. 2007;49:109–12. doi: 10.4103/0019-5545.33257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.D’Souza G, Rekha DP, Sreedaran P, Srinivasan K, Mony PK. Clinico-epidemiological profile of tobacco users attending a tobacco cessation clinic in a teaching hospital in Bangalore city. Lung India. 2012;29:137–42. doi: 10.4103/0970-2113.95314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kisore P, Lal N, Trivedi JK, Dalal PK, Aga VM. A study of comorbidity in psychoactive substance dependence patients. Indian J Psychiatry. 1994;36:133–7. [PMC free article] [PubMed] [Google Scholar]
- 21.Villalta J, Estruch R, Antúnez E, Valls J, Urbano-Márquez A. Vagal neuropathy in chronic alcoholics: Relation to ethanol consumption. Alcohol Alcohol. 1989;24:421–8. [PubMed] [Google Scholar]
- 22.Gümüş B, Yiğitoğlu MR, Lekili M, Uyanik BS, Müezzinoğlu T, Büyüksu C. Effect of long-term alcohol abuse on male sexual function and serum gonadal hormone levels. Int Urol Nephrol. 1998;30:755–9. doi: 10.1007/BF02564864. [DOI] [PubMed] [Google Scholar]
- 23.Sullivan ME, Keoghane SR, Miller MA. Vascular risk factors and erectile dysfunction. BJU Int. 2001;87:838–45. doi: 10.1046/j.1464-410x.2001.02211.x. [DOI] [PubMed] [Google Scholar]
- 24.Jaffe JH, Knapp CM, Ciraulo DA. Opiates: Clinical aspects. In: Lowinson JH, Ruiz P, Millman RB, Langrod JG, editors. Substance Abuse: A Comprehensive Textbook. 3rd ed. Baltimore Maryland: Williams & Willkins; 1997. pp. 158–165. [Google Scholar]
- 25.Smith S. Drugs that cause sexual dysfunction. Psychiatry J. 2007;6:111–4. [Google Scholar]
- 26.Trivedi JK, Jilani AQ. Pathway of psychiatric care. Indian J Psychiatry. 2011;53:97–8. doi: 10.4103/0019-5545.82530. [DOI] [PMC free article] [PubMed] [Google Scholar]


