Abstract
Background:
Diabetes mellitus is a significant cause of visual impairment, hence adequate knowledge on this condition and its ocular manifestations is of immense importance to diabetic patients.
Aim:
To assess the knowledge of diabetic patients on the disorder and its ocular manifestations, and their attitude towards ocular examinations.
Materials and Methods:
A cross-sectional survey involving the use of a structured interview was conducted among diabetic patients attending the Diabetic Clinic of the Korle-Bu Teaching Hospital. Using Fishers Exact Chi-square (χ2) and Odds Ratios (ORs), data obtained was analyzed.
Results:
Only 103 (26.4%) patients knew the type of diabetes mellitus they were suffering from. Knowledge on ocular effects of diabetes mellitus was low and only 15 (3.8%) knew that it could affect the ocular refraction with no patient mentioning that diabetes mellitus could cause cataract or diabetic retinopathy. Attitude to routine eye examination was poor. As much as 135 (34.6%) had never had an eye examination since being diagnosed of diabetes. Knowledge of the type of diabetes mellitus the individual had or any ocular complication of this disorder was significantly related (OR: 4.22; P < 0.001 and OR: 2.55; P < 0.001) respectively to their attitude to seeking eye care.
Conclusion:
Diabetic patients’ knowledge on diabetes mellitus and its ocular manifestations, and the attitude of diabetic patients towards eye examination were poor. Intensive health education by diabetes care givers and leaders of the Ghana Diabetic Association for diabetic patient is therefore required to improve attitude towards eye care to prevent visual impairment.
Keywords: Cataract, diabetes mellitus, diabetic retinopathy, ocular manifestations
INTRODUCTION
Diabetes mellitus (DM), a multi-systemic disease characterized by hyperglycemia, is on the increase worldwide. The prevalence of DM was estimated at 171 million in 2000 and future projections made to the next three decades indicate that this prevalence could reach 366 million with developing countries being the most affected.1 Report indicate that in the year 2000, there were 7.5 million cases of DM in Africa with more than 80% of these cases remaining undiagnosed.2 According to the International Diabetes Federation over 7.1 million people in sub-Saharan Africa are now estimated to suffer from DM and this will increase to 15.0 million by 2025.3
Diabetes used to be very uncommon some decades ago with estimates ranging from 0.2 to 0.4% in Ghana.4,5,6 This situation is steadily changing as diabetes now accounts for 6.8% adult admissions at the Korle-Bu Teaching Hospital in Accra, Ghana.7 This estimate is close to the finding of a population-based survey in Accra which recorded a prevalence of 6.3% among subjects aged 25 years and older.8 President of the National Diabetes Association gave a current estimate of the diabetic population in Ghana to be more than 4 million.9 This increase in prevalence could be attributed to several risk factors including ageing, diet, obesity and physical inactivity.10
Diabetic patients suffer systemic complications including ocular disorders. It is estimated that 4.51 million of the diabetic population in sub-Saharan Africa have one form of ocular complications due to diabetes.11 People living with diabetes are about 25 times more likely of becoming blind compared to the normal population.12 The incidence of vision loss or blindness due to ocular complications of diabetes raises sufficient public health concern, with diabetic retinopathy alone responsible for 12,000 to 24,000 new cases of blindness yearly in the United States.13 Some other known causes of blindness secondary to diabetes are cataracts, glaucoma, nerve palsies and macular degeneration.14
Diabetic patients are required (due to the disposition of their condition) to have sufficient knowledge regarding their illness so as to exhibit a positive attitude to health care. Despite the increased tendency of blindness, studies have shown that most diabetic patients do not seek the recommended ocular examinations (such as regular dilated fundus examination) aimed at preventing visual impairment and blindness.15 It is therefore very essential that patients’ knowledge on the ocular manifestations of diabetes be ascertained to determine if this is the barrier to seeking recommended eye examination among the diabetic population in Ghana. This study therefore evaluated the knowledge that diabetic patients had concerning ocular manifestations of diabetes mellitus and their attitude towards ocular examination. This will aid diabetes care givers and the Ghana Diabetic Association to provide counseling and conduct health educational programmes.
MATERIALS AND METHODS
Study area
This study was carried out in the Diabetes Clinic of the Korle-Bu Teaching Hospital (KBTH), Accra, Ghana. It serves as the center for National Diabetes Management and Research.
Study population
The study population comprised DM patients aged 16 years and above who attended the Diabetes Clinic and consented to participate in the study. A total of 390 diabetic patients were recruited for the study. The figure meets the minimum sample requirement for a study population greater than 10,000 based on the formula below.16
n = Z2 P(1–P)/d2
n = the desired sample size (when population is greater than 10,000)
z = the standard normal deviate, usually set at 1.96, which corresponds to the 95% confidence interval
P = proportion in the target population estimated to have a particular characteristic (50%)
d = degree of accuracy.
Ethical considerations
Institutional approval to conduct the study was sought and obtained from the Department of Optometry, University of Cape Coast, Cape Coast, Ghana, and the National Diabetes Management and Research Center (NDMRC), Korle-Bu Teaching Hospital, Accra, Ghana. Informed consent was administered and only those who gave consent were recruited to participate in the study. The study was conducted in accordance with the World Medical Association Declaration of Helsinki on the ethical principles for medical research involving human subjects.
Study conduct and design
A prospective cross-sectional survey was conducted over a three-month period, among the DM patients. Each patient was given an interview guide and assisted by an interviewer to respond to questions in the guide. The interviews were conducted by one of the authors (SA) and five trained research persons from NDMRC. Participants responded to questions in; basic demographic information of patient (age, sex, location, occupation, education, onset and duration of the disease), patients’ knowledge of their diabetic status, knowledge on the ocular manifestations of diabetes, and practices towards eye examination. The interview was conducted in the language that the participant understood and could communicate well with the interviewer.
Patients were categorized based on their knowledge on diabetes and/or ocular manifestations of diabetes: “Knowledge present” -comprised those who gave the right response and “Knowledge absent”- comprised those without the appropriate response. Also, patients that had undergone ocular examination were regarded as having “positive practice” while those without any eye examination since diagnosis of diabetes were labeled as having “negative practice”.
Data analysis
The Statistical Package for social sciences (SPSS) version 17 was used for the computation. Descriptive statistics including frequencies, percentages, means and standard deviations were computed. The Fisher's Exact Chi-square (χ2) test was used in determining statistically significant differences in demographic characteristics between male and female diabetic patients. Odds ratios were also computed to determine the relationship between patient's knowledge on diabetes and its ocular effects and their practices regarding eye examination. Binary logistic regression was also used to assess the effects of other demographic characteristics on patient's knowledge.
RESULTS
Demographics
Of the 390 diabetics that volunteered to participate in the study, 299 (76.7%) were females while 91 (23.3%) were males (M: F = 1:3.3). The mean age of the participants was 56.98 ± 12.93 years (95% CI = 55.70 - 58.26 years). The mean duration of diabetes mellitus was 8.69 ± 6.14 years (95% CI = 8.08 - 9.30 years); males had a significantly lower (P = 0.033) duration [Table 1].
Table 1.
Demographic characteristics of DM patients involved in the study
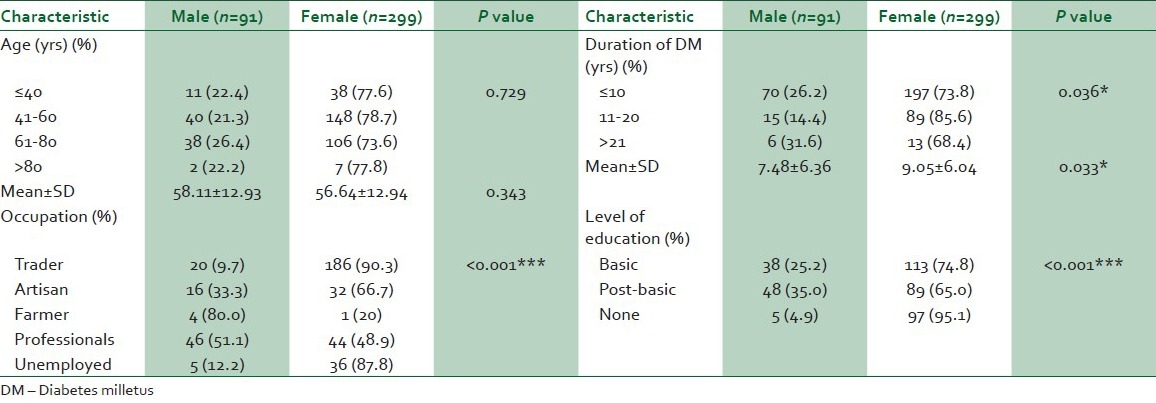
Most of the patients (n = 206) were traders (of whom 186 [90.3%] were women), while farmers (n = 5) and the “professionals (n = 90)” were mainly men. Gender was significantly (P < 0.001) associated with the diabetic patient's occupation. In relation to formal education, 288 (73.8%) had either basic education or above, while 102 (26.2%) did not have any formal education. Males were more educated with only five (4.9%) having no formal education. A strong association (P < 0.001) existed between gender and education [Table 1].
Knowledge of types of DM
Regarding diabetic patient's knowledge on the type of diabetes they had been diagnosed of, only 103 (26.4%) had knowledge of their DM status. Of these 18 (4.6%) had type I, 77 (19.7%) had type II and eight (2.1%) had gestational diabetes [Table 2]. Although females were less knowledgeable of their status, gender (P = 0.345) was not significantly related to patient's knowledge on the type of diabetes being suffered [Table 3].
Table 2.
Relationship between diabetic patient’s knowledge (regarding diabetes its ocular manifestations) and practice towards eye examination
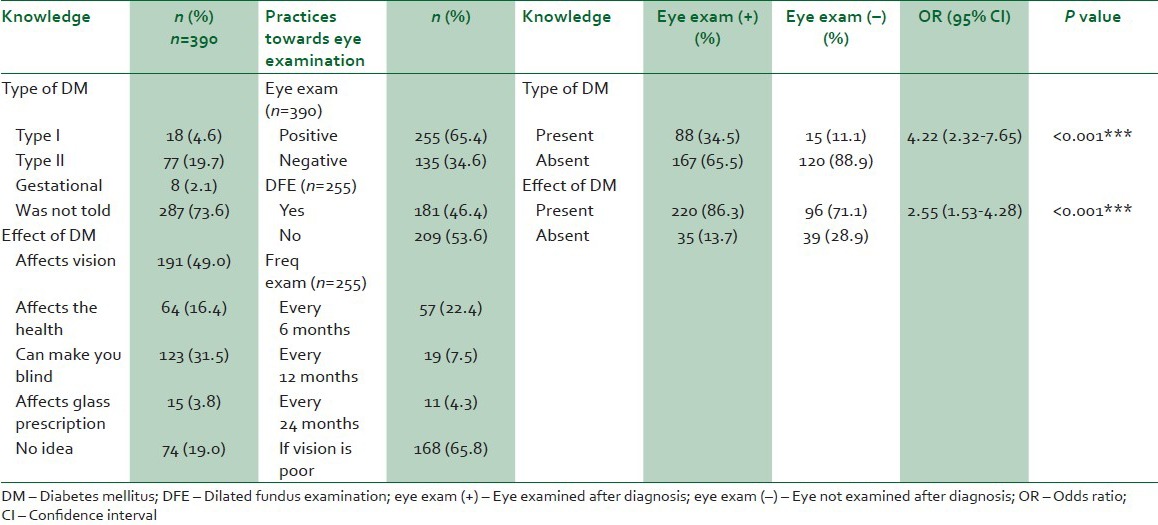
Table 3.
Multivariate analysis of diabetic patient’s knowledge and attitude regarding diabetes and the ocular manifestations
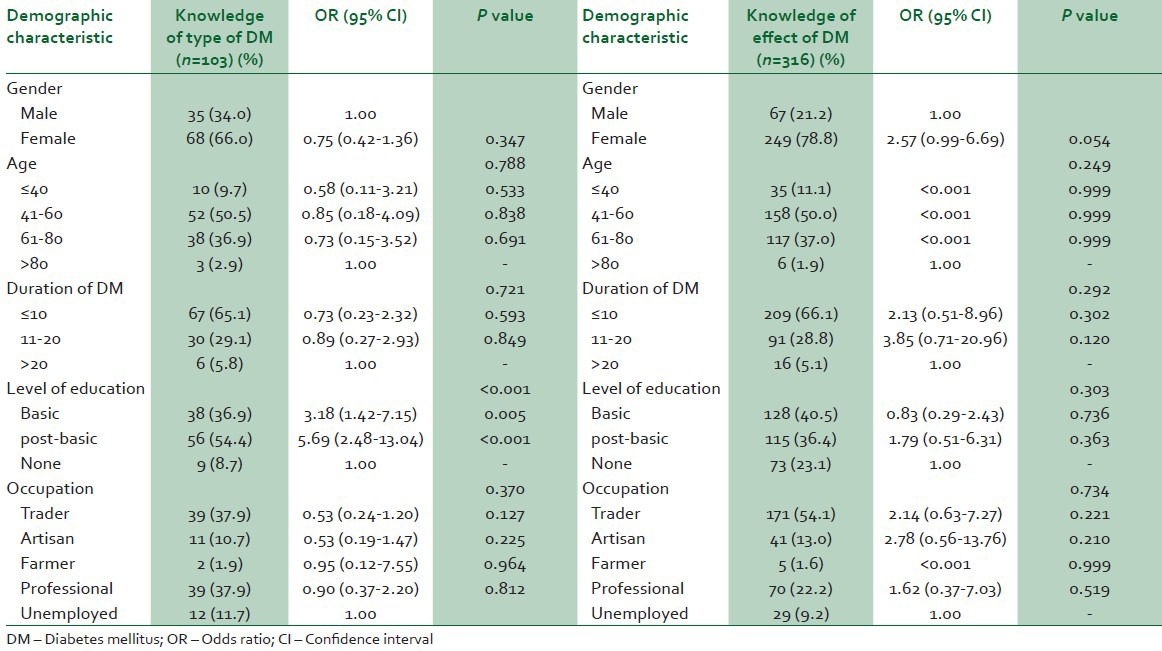
With regards to age, 93 (90.3%) of those with knowledge on type of DM (n = 103) were above 40 years, with those older than 80 years having more knowledge compared to all other age groups. The age of the patients was not significantly related (P = 0.788) to the individuals knowledge on type of DM [Table 3].
Of the 103 patients who had knowledge of the type of DM they had, 67 (65.1%) were diagnosed less than 10 years ago and were the least to know about the type of DM (OR: 0.73) though patient's duration of DM had no significant (P = 0.721) association with the individual's knowledge on the type of DM [Table 3].
The patient's level of formal education was significantly related (P < 0.001) to the individuals knowledge of the type of DM. Patients with post-basic education being most knowledgeable (OR: 5.69) of the type of DM suffered [Table 3]. Traders 39 (37.9%) and professionals 39 (37.9%) constituted the majority who were knowledgeable of the type of DM they had, but patient's occupation was not significantly related (P = 0.370) to the knowledge of the type of DM [Table 3].
Knowledge on ocular effects of DM
Regarding the knowledge on the ocular effects of DM, 74 (19.0%) had no idea of any specific ocular effect of DM but 191 (49%) reported it could affect vision. Only 15 (3.8%) knew that DM could affect the patient's ocular refractive state (i.e., their spectacle correction) [Table 2].
Of the 316 who had knowledge of some ocular effects of DM, 249 (78.8%) were females indicating that they were slightly more knowledgeable (P = 0.054) on some ocular effects of diabetes than males [Table 3].
Although patient's age was not significantly related (P = 0.249) to the knowledge on the ocular effects of diabetes, those older than 80 years were comparatively more knowledgeable [Table 3].
While majority of patients (209 (66.1%)) with knowledge of some ocular effects of DM had had diabetes for 10 years or less, patients with DM ranging from 11 to 20 years were most knowledgeable (OR: 3.85). Patient's duration of diabetes was, however, not significantly related (P = 0.292) to the knowledge on the ocular effects of diabetes [Table 3].
Most of the diabetic patients (243 (76.9%)) who were knowledgeable on some ocular effects of DM had had basic education or more. Although patient's level of formal education was not significantly (P = 0.303) associated with the individuals knowledge of the ocular effects of DM, patients with post-basic education were more knowledgeable (OR: 1.79; P = 0.363) compared to those without basic education [Table 3].
Even though traders constituted more than half of the individuals with knowledge on the ocular effects of diabetes, this was not statistically different (OR: 2.14; P = 0.221) from other occupations. Patient's occupation was not a statistically significant determinant (P = 0.734) of the individuals knowledge regarding the ocular effects of diabetes [Table 3].
Diabetic patient's practices towards eye examination
Among the 390 participants, 255 (65.4%) reported having had an eye examination after being diagnosed of diabetes, of which only 181 (46.4%) underwent dilated fundus examination. When these patients who had undergone eye examination were asked how frequently they examined their eyes, majority 168 (65.85%) indicated that they only examined their eyes if their vision got poor [Table 2].
Relationship between knowledge and practices of diabetic patients
Of the 255 patients that had their eyes examined, 88 (34.5%) were those who were knowledgeable on the type of DM diagnosed [Table 2]. A statistically significant association existed between knowledge of the type of diabetes diagnosed and ocular examination, with diabetic patients knowing the type of DM suffered being more likely (OR: 4.22; P < 0.001) to undertake an eye examination [Table 2].
Also, among the 255 patients that had eye examination after diagnosis, 220 (86.3%) were knowledgeable on the ocular effects of DM. Knowledge of ocular effect of DM was significantly related to eye examination with those having knowledge on the ocular effects of DM being more likely to undertake eye exam (OR: 2.55; P < 0.001) [Table 2].
Information on eye care providers consulted, source of eye education, relatives with DM, DM treatment and hypertensive status.
Concerning the sources of education on the ocular effects of DM, most patients (210 (66.4%)) obtained their knowledge from general practitioners and nurses with only 26 (8.2%) having obtained this knowledge from optometrists [Table 4].
Table 4.
Information on eye care providers consulted, source of eye education, relatives with DM, DM treatment and hypertensive status
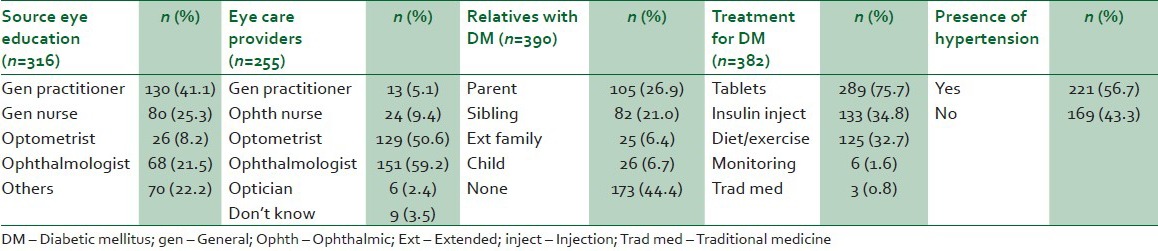
Of the 255 who have had their eyes examined at least once after diagnosis of DM, most of these patients reported having been examined by ophthalmologist (151 (59.2%))and optometrists (129 (50.6%)) with nine (3.5%) not knowing which practitioner did the examination.
Some diabetic patients 217 (55.6%) had one or more relatives also suffering from DM, with 115 (26.9%) having parents with DM and 82 (21.0%) having siblings with DM.
Management of diabetic patients usually involved a combination of treatment options with 289 (75.7%) being treated with oral medications, 133 (34.8%) on insulin injections and/or diet and exercise 125 (32.7%).
Regarding the association between diabetes and hypertension, 221 (56.7%) of the diabetic patients also had systemic hypertension.
DISCUSSION
Diabetes mellitus is a significant cause of visual impairment among its sufferers. Therefore, sufficient knowledge concerning diabetes and its ocular manifestations as well as good practices with regards to controlling their diabetes and taking the recommended eye examination are crucial. Our study showed that patients had little knowledge of the ocular complications of diabetes. The type of diabetes an individual suffers determines the period of onset of ocular complications. Literature estimates that about 25% of sufferers of non-insulin dependent (type II) diabetes develop some degree of diabetic retinopathy before diagnosis of diabetes is made.17,18 No patient mentioned cataract or diabetic retinopathy as ocular disorders that could be caused by DM. Contrary to our findings, a study by Khandekar et al.19 found that 72.9% diabetic patients in Oman were knowledgeable on the ocular complications of DM. Other studies20,21 have even found over 95% of their study population being knowledgeable on DM and its ocular effects.
Coincidentally, the patients in our study also exhibited poor practices with regards to eye examination with only 19.5% having undertaken last ocular examination within one year with 34.6% never having had an eye examination since being diagnosed of DM. This negative practice towards eye examination and poor knowledge of ocular complications of DM may be attributed to the work overload of the few diabetic practitioners thereby reducing the contact time spent on attending to the needs of each patient. Practitioners lack sufficient time to educate patients on the need to take eye examination as was observed with more than half of the patients reporting not having been advised on taking periodic eye examination. It is recommended that diabetic patients undergo a comprehensive eye examination at least annually to facilitate early diagnosis and management of ocular disorders associated with DM to avoid severe visual impairment.22 A study conducted in Durban, South Africa, found that about 48% of the diabetic patients had undergone an eye examination over one and half year ago.23 Their patients, therefore, had better attitude towards ocular examination than our study population. The reason for the low uptake of eye care among our study population compared to the participants in the Durban study could be due to the poor knowledge exhibited by our patients. A study of diabetic patient's compliance in assessing eye care at a Tanzanian referral hospital also observed that 28.8% of their patients had received ocular examination within the past year.15 This negative attitude to eye care in our participants could be due to the very low level of knowledge (on diabetes or its ocular effects) exhibited as we observed a very strong association (P < 0.001) between patient's knowledge and attitude to eye care. This supports a study conducted by Hartnett et al.24 to assess the barriers to uptake of eye examination among diabetic patients which cited lack of patient education and knowledge about DM as the most significant hindrance.
The association between diabetes and gender has been controversial, while some studies have found increased preponderance for one particular sex; others have found no gender predilection in the prevalence of diabetes. In our study, a huge proportion of patients were women. This might be due to the non-randomization of the study population. In hospital survey of this nature, only patients presenting at the time of the study and giving consent to participate were recruited. Thus we cannot on the basis of the preponderance of female in our study assert that sex is a risk factor for DM.
Also, Omar et al.25 observed in their study that the prevalence of DM was more than twice in women than men of Zulu descent in Durban. Obesity is a very important health issue as it has been identified as the underlying risk factor in most chronic non-communicable diseases, especially diabetes. Studies have shown that the prevalence of obesity in Ghanaian women is three times that in men.26,27 Therefore, obesity could be the confounding variable establishing the seeming relationship between gender and diabetes.
The mean age of onset of diabetes among the patients was after the fourth decade of life. The significantly lower duration of diabetes in males could be a reflection of the comparatively lower life expectancy among Ghanaian men compared to women.28
Among the diabetic patient's demographics, only the level of patient's formal education significantly influenced the individual's knowledge of the type of DM suffered. This may be due to the difficulty of expressing this information on the various types of DM to uneducated patients or that this information seems to be incomprehensible to patients without formal education. Conversely, knowledge on the ocular effect of DM was not related to the level of patient's formal education. This implies that no specific education-dependent strategy is required to be employed in the counseling and creating of patient awareness on the ocular manifestations of diabetes.
Diabetic patients are usually more conscious of their general health and therefore more frequently visits their primary diabetic physicians. This may be the reason why most of these patients cited general physicians as source of knowledge on ocular effects of DM. General Physicians due to their regular contact with diabetic patients could do more in educating patients on the ocular complications of DM and the need to adopt the right attitude to eye examination.
Due to the numerous risks of diabetics developing ocular complications, these patients usually require services of trained eye care professionals to attend to their needs. Ophthalmologists and optometrist are required to conduct comprehensive examination including dilated fundus examination (DFE) to aid in early detection and prevention of ocular complications. According to our study, the expertise of these two eye care providers is almost equally utilized in the management of ocular health disorders of diabetic patients.
The family history of diabetes has been a suggested screening tool for assessing the risk of diabetes as it signifies the genetic susceptibility of an individual, especially first degree relatives.29 Several studies indicate that persons with relatives suffering from DM were between 2 to 6 times more susceptible to develop DM.30 Our study supports this assertion as more than 20% of respondents reported having either parents or siblings suffering from DM.
Literature indicates an association between diabetes and hypertension.31 This may be because diabetes mellitus as well as cardiovascular diseases share common risk factors and also either one of these disease entities could precipitate the occurrence of the other.32 This study indicated that more than half of the diabetic population also suffered from hypertension. Blood pressure monitoring and control, therefore, should be a routine in the management of all diabetic patients.
CONCLUSIONS
Diabetic patient's knowledge on the type of diabetes suffered and its ocular complications were poor. Patient's knowledge was significantly related to their attitude towards receiving ocular examination. Intensive diabetic patient education from diabetic care givers is therefore required to improve their eye care attitude to prevent visual impairment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes; Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 2.Diabetes cases in Africa to double in next 25 years. [Last accessed on 2013 Jan 04];Bull World Health Organ. 2004 82:397–8. Available from: http://www.scielosp.org/pdf/bwho/v82n5/v82n5a26.pdf . [Google Scholar]
- 3.The Diabetes Atlas. Brussels: International Diabetes Federation; 2003. International Diabetes Federation; pp. 15–71. [Google Scholar]
- 4.Dodu SR, de Heer N. A diabetes case-finding survey in Ho, Ghana. Ghana Med J. 1964;3:75–80. [Google Scholar]
- 5.Dodu SR. The incidence of diabetes mellitus in Accra (Ghana).A study of 4000 patients. West Afr Med J. 1958;7:129–34. [PubMed] [Google Scholar]
- 6.Owusu SK. Epidemiology of diabetes mellitus in West Africa: Incidence and prevalence studies. Ghana Med J. 1988;22:2–6. [Google Scholar]
- 7.Adubofour KO, Ofei F, Mensah-Adubufour J, Owusu SK. Diabetes in Ghana. In: Gill G, Mbanya JC, Alberti G, editors. Diabetes in Africa. Reach, Cambridge, UK: FSG Communications Ltd; 1997. pp. 83–8. [Google Scholar]
- 8.Amoah AG, Owusu SK, Adjei S. Diabetes in Ghana: A community based prevalence study in Greater Accra. Diabetes Res Clin Pract. 2002;56:197–205. doi: 10.1016/s0168-8227(01)00374-6. [DOI] [PubMed] [Google Scholar]
- 9.Okertchiri JA. Ghana needs more Diabetic Educators. Daily Guide. 2012. Nov 16, [Last accessed on 2013 Jan 04]. Available from: http://www.dailyguideghana.com/?p=67402 .
- 10.Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–50. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 11.The Diabetes Atlas. Brussels: International Diabetes Federation; 2007. International Diabetes Federation; pp. 82–91. [Google Scholar]
- 12.Thomann KH, Marks ES, Adamczyk DT. New York: McGraw-Hill; 2001. Primary Eye care in Systemic Disease; pp. 189–204. [Google Scholar]
- 13.Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2007. [Last accessed on 2013 Jan 04]. Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States. Available from: http://www.cdc.gov/diabetes/pubs/estimates . [Google Scholar]
- 14.Jeganathan VS, Wang JJ, Wong TY. Ocular associations of diabetes other than diabetic retinopathy. Diabetes Care. 2008;31:1905–12. doi: 10.2337/dc08-0342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mumba M, Hall A, Lewallen S. Compliance with eye screening examinations among diabetic patients at a Tanzanian referral hospital. Ophthalmic Epidemiol. 2007;14:306–10. doi: 10.1080/09286580701272079. [DOI] [PubMed] [Google Scholar]
- 16.Kasiulevicius V, Sapoka V, Filipaviciute R. Sample size calculation in epidemiological studies. Gerontologija. 2006;7:225–31. [Google Scholar]
- 17.Cacallerano J. AOA reference guide for clinicians. St Louis: American Optometric Association; 2002. Optometric clinical guidelines. Care of the patient with diabetes mellitus; pp. 13–6. [Google Scholar]
- 18.Fowler MJ. Microvascular and macrovascular complications of diabetes. Clin Diabetes. 2008;26:77–82. [Google Scholar]
- 19.Khandekar R, Al Harby S, Al Harthy H, Al Lawatti J. Knowledge, attitude and practice regarding eye complications and care among Omani persons with diabetes – A cross sectional study. Oman J Ophthalmol. 2010;3:60–5. doi: 10.4103/0974-620X.64228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Funatsu H, Hori S, Shimizu E, Nakamura S. Questionnaire survey on periodic ocular examination in Japanese diabetic patients. Am J Ophthalmol. 2003;136:955–7. doi: 10.1016/s0002-9394(03)00542-7. [DOI] [PubMed] [Google Scholar]
- 21.Schmid KL, Schmid LM, Pedersen KC. Knowledge of the ocular effects of diabetes among the general population of Australia and the members of Diabetes Australia. Clin Exp Optom. 2003;86:91–103. doi: 10.1111/j.1444-0938.2003.tb03067.x. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization. Prevention of blindness from diabetes mellitus: Report of WHO consultation in Geneva, Switzerland, 9-11 November 2005. [Last accessed on 2013 Jan 04]. Available from: http://www.who.int/blindness/Prevention%20of%20Blindness%20from%20Diabetes%20Mellitus-with-cover-small.pdf .
- 23.Mashige KP, Notshweleka A, Moodley S, Rahmtoola FH, Sayed SB, Singh S, et al. An assessment of the level of diabetic patients’ knowledge of diabetes mellitus, its complications and management in Durban, South Africa. S Afr Optom. 2008;67:95–105. [Google Scholar]
- 24.Hartnett ME, Key IJ, Loyacano NM, Horswell RL, DeSalvo KB. Perceived barriers to diabetic eye care: Qualitative study of patients and physicians. Arch Ophthalmol. 2005;123:387–91. doi: 10.1001/archopht.123.3.387. [DOI] [PubMed] [Google Scholar]
- 25.Omar MA, Seedat MA, Motala AA, Dyer RB, Becker P. The prevalence of diabetes mellitus and impaired glucose tolerance in a group of urban South African Blacks. S Afr Med J. 1993;83:641–3. [PubMed] [Google Scholar]
- 26.Biritwum RB, Gyapong J, Mensah G. The Epidemiology of Obesity in Ghana. Ghana Med J. 2005;39:82–5. [PMC free article] [PubMed] [Google Scholar]
- 27.Amoah AG. Obesity in adult residents of Accra, Ghana. Ethn Dis. 2003;13(Suppl 2):S29–101. [PubMed] [Google Scholar]
- 28.Ghana: WHO Regional Office for Africa; 2009. [Last accessed on 2013 Jan 04]. Second Generation, World health Organization Country Coopertation Strategy 2008-2011. Available from: http://www.who.int/countryfocus/cooperation_strategy/ccs_gha_en.pdf . [Google Scholar]
- 29.Valdez R. Detecting undiagnosed type 2 diabetes: Family history as a risk factor and screening tool. J Diabetes Sci Technol. 2009;3:722–6. doi: 10.1177/193229680900300417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harrison TA, Hindorff LA, Kim H, Wines RC, Bowen DJ, McGrath BB, et al. Family history of diabetes as a potential public health tool. Am J Prev Med. 2003;24:152–9. doi: 10.1016/s0749-3797(02)00588-3. [DOI] [PubMed] [Google Scholar]
- 31.Tai TY, Chuang LM, Chen CJ, Lin BJ. Link between hypertension and diabetes mellitus. Epidemiological study of Chinese adults in Taiwan. Diabetes Care. 1991;14:1013–20. doi: 10.2337/diacare.14.11.1013. [DOI] [PubMed] [Google Scholar]
- 32.Cederholm J, Nilsson PM. A review of risk factors and cardiovascular disease in diabetes care-2011. Eur J Cardiovasc Med. 2011;1:21–5. [Google Scholar]


