Abstract
Background:
The burden of obstructive sleep apnea among commercial drivers in Nigeria is not known.
Aim:
To assess the prevalence of high risk of obstructive sleep apnea (OSA) and excessive daytime sleepiness (EDS) among intra-city commercial drivers.
Setting and Design:
A descriptive cross-sectional study in three major motor parks in Lagos metropolis.
Materials and Methods:
Demographic, anthropometric and historical data was obtained. The risk of OSA and EDS was assessed using the STOP BANG questionnaire and the Epworth Sleepiness Scale, respectively.
Statistical Analysis:
The relationship between the OSA risk, EDS risk and past road traffic accident (RTA) was explored using the Pearson's chi square. Independent determinants of OSA risk, EDS risk and past RTA, respectively, were assessed by multiple logistic regression models.
Result:
Five hundred male commercial drivers (mean age (years) ±SD = 42.36 ± 11.17 and mean BMI (kg/m2) ±SD = 25.68 ± 3.79) were recruited. OSA risk was high in 244 (48.8%) drivers and 72 (14.4%) had EDS. There was a positive relationship between OSA risk and the risk of EDS (Pearson's X2 = 28.2, P < 0.001). Sixty-one (12.2%) drivers had a past history of RTA but there was no significant relationship between a past RTA and either OSA risk (X2 = 2.05, P = 0.15) or EDS risk (X2 = 2.7, P = 0.1), respectively. Abdominal adiposity, regular alcohol use and EDS were independent determinants of OSA risk while the use of cannabis and OSA risk were independent determinants of EDS. No independent risk factor for past RTA was identified.
Conclusion:
A significant proportion of commercial drivers in Lagos metropolis are at high risk of OSA and EDS.
Keywords: Commercial drivers, excessive day time sleepiness, Lagos, obstructive sleep apnea
INTRODUCTION
Obstructive sleep apnea (OSA) is a form of sleep disordered breathing characterized by recurring episodes of partial or complete airway obstruction during sleep resulting in repeated arousals and lack of restful sleep.1 The adverse consequences of OSA include excessive daytime sleepiness (EDS), fatigue and impaired cognitive functioning which could increase the risk of road traffic accidents (RTA) as well as other accidents. In addition, there is increased cardiovascular risk and poor quality of life.2,3,4
The cognitive effects of OSA are particularly important in persons engaged in daytime activities that require intense concentration, simultaneous visuo-spatial computations, prompt reaction time and decision making, especially in the face of threats. Controlled experiments have demonstrated that sleep loss results in episodic lapses comprising of brief unresponsiveness with extreme drowsiness and electroencephalographic slowing, which are worsened with increased duration of sleep loss, and are strongly affected by stimulus monotony, as may be experienced during driving.5
Approximately 20% of driving accidents are attributable to inadequate sleep such as occurs in persons with OSA.6 In Nigeria, it is estimated that over 90% of RTA are due to driver error.7 Multiple factors contributing to the risk of RTA among long distance truck drivers in Nigeria include daytime sleepiness, fatigue and stimulant use.8 Studies have shown that commercial bus drivers with undiagnosed and untreated OSA are at increased risk of RTAs.9,10,11,12,13 Intra-city commercial drivers with OSA are also vulnerable because of the long driving hours and economic pressure to achieve financial commitment and targets. The burden of OSA in commercial drivers in Lagos, Nigeria, has not been evaluated, but such data are undoubtedly important as a baseline to guide counselling, driver certification and education, and ultimately improve road safety.
Polysomnography is the gold standard for diagnosing OSA, but its wide applicability is hampered by limited access and cost.13 Thus, OSA risk assessment typically comprises the use of validated screening instruments that evaluate multiple parameters to obtain a score that reflects the magnitude of risk of OSA.14,15,16 This can then guide selection of high-risk individuals for further evaluation and treatment.
The objectives of the study were to assess the prevalence of high risk of OSA and EDS among commercial drivers as well as to determine the relationship of high risk of OSA to the past history of RTA and use of psychoactive substances.
MATERIALS AND METHODS
This is a descriptive cross-sectional study, for which prior ethical approval was obtained from the Lagos University Teaching Hospital Health Research Ethics Committee (ADM/DCST/HREC/310). The study was conducted at the three major commercial motor parks in Lagos Mainland, situated at Ojuelegba, Idi Araba and Lawanson. These parks were selected based on information obtained from local government authorities and the National Union of Road Transport Workers (NURTW) as being among the top ranking parks in Mushin (8 parks) and Surulere (12 parks) zones in terms of membership of registered operators of commercial vehicles. A total of 610 commercial drivers were registered under the NURTW (mandatory membership required of all commercial drivers) at the three parks at the time of the study between September and December 2011. Verbal permission was obtained from the NURTW executive at each park, while individual written consent was obtained from each participating driver.
Data was collected from consecutively consenting drivers during the weekly NURTW meetings held at the park. Based on an initial pilot to test the study instrument, in which 8 out of 10 consented to participate, we estimated a total sample of 488 (80% of 610) with the intention to round this up to a final sample size of 500.
The study instrument was a questionnaire containing demographic information, anthropometric data, historical, social, occupational and medical data, the STOP-BANG questionnaire for assessment of OSA risk, and the Epworth Sleepiness Scale for assessing daytime sleepiness. The questionnaire was administered by trained interviewers.
Specific demographic information obtained were age and gender. Medical history of physician diagnosed diabetes mellitus, bronchial asthma or any lung disease was obtained. Self-declared smoking status, psychoactive substance (in local parlance), kolanut (caffeine containing nuts), caffeine and alcohol use were also obtained. Information related to driving occupation included duration and past history of RTA on the job.
The anthropometric measurements were obtained using standard procedures, and included weight (kilograms), height (metres), waist circumference (centimetres), and neck circumference (centimetres).17 Abdominal adiposity was defined as waist circumference >88 cm in females and >102 centimetres in males.18 Body mass index (kg/m2) was calculated using Quetlet's index and translated as underweight (<18.5), normal (18.5-24.9) overweight (25-29.9) or obese class 1 (30-34.9), obese class 2 (35-39.9) and extremely obese (≥40).19,20 Blood pressure (mmHg) was measured using an Omron; electronic sphygmomanometer and a reading of ≥140/90 considered as hypertension.21,22 The presence any of the following - diabetes mellitus, hypertension, current cigarette smoking, obesity and central adiposity, were documented, with patient's having any of these categorized as high cardiovascular risk.23
Current cigarette smoking was defined as smoking at least one puff of cigarette in the preceding 30 days. Current cannabis smoking was defined as smoking at least one puff of cannabis in the preceding 30 days. Regular alcohol use was defined as taking an alcoholic beverage at least once every 7 days. Alcohol use was quantified in terms of bottles of alcoholic beverage (beers typical volume 600 mls per bottle, alcohol contents approximately 5 - 6 g per 100 mls) taken per week and those who took more than 14 bottles per week were categorised as heavy drinkers.
The risk of OSA was measured using the STOP-BANG questionnaire.14 The STOP-BANG questionnaire is a simple validated 8 item instrument that asks about symptoms of Snoring, Tiredness, Observed apnea and a history of high blood Pressure.14,24 It includes a section to document the body mass index, age, neck circumference in centimeters, and gender. A systematic review of the various screening tools for OSA recommends the use of the STOP-BANG questionnaire due to its higher methodological quality and easy to use features.25 A total score of 3 and above is considered a high risk of OSA.14
The risk of excessive daytime sleepiness (EDS) was assessed using the Epworth Sleepiness Scale© ((ESS)© MW Johns 1990-1997 used with permission). This is a validated 8-item questionnaire that measures the ease of falling asleep in the daytime under various circumstances as a measure of daytime hypersomlonence.26 In the setting of OSA, the ESS has been shown to distinguish between patients with primary snoring (without airway obstruction) and OSA.27 The interpretation is as follows: 0 - 5: Good (likely getting restful sleep quality); 6 - 9: (sleep could be improved but may not be to sleep apnea); 10 and above: Bad (likely to have excessive sleepiness (suggestive of a sleep disorder possibly OSA).26
Data obtained was analyzed using the Statistical Software for Social Sciences (SPSS) version 20. Continuous variables with normal distribution (age, blood pressures, BMI, waist circumference, STOP-BANG and ESS scores) are expressed as means and standard deviation and compared using the Pearson's correlation. Group differences in discrete variables (e.g., BMI category, OSA risk category, ESS category (presented as frequencies)), are compared with the Pearson C2 test. Independent predictors of OSA risk were assessed in multivariate logistic regression analysis.
RESULTS
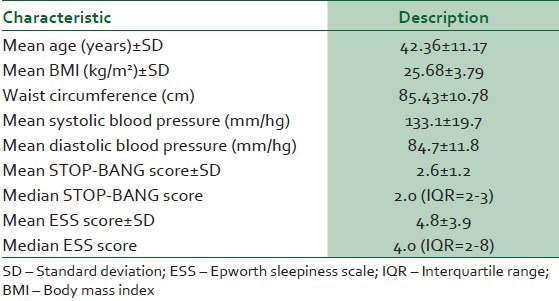
Five-hundred commercial drivers (all men) participated in the study. Table 1 shows baseline characteristics of the commercial drivers. The age range was 20-73 years. Two hundred and thirteen (42.6%) were aged 15-39 years, 285 (57%) were 40-65 years and 2 (0.4%) >65 years. Median duration of working as a commercial driver was 10 years (interquartile range 4-18); 272 (54.5%) had driven for 1-10 years, 155 (31%) for 11-20 years and 73 (14.6%) for >20 years. Based on the BMI, 4 (0.8%) of the drivers were underweight, 248 (49.6%) normal, 173 (34.6%) overweight, 61 (12.2%) obese (class 1), and 14 (2.8%) obese (class 2). There were 52 (10.8%) drivers with abdominal adiposity, 211 (42.2%) with hypertension and 3 (0.6%) with diabetes. A total of 341 (68.2%) drivers had at least one risk factor for adverse cardiovascular events. None of the participants had a prior diagnosis of asthma or COPD.
Table 1.
Baseline characteristics of study participants
Use of psychoactive substances among commercial drivers
One-hundred and sixty (32%) were current cigarette smokers, 108 (21.6%) smoked cannabis regularly and 72 (14.4%) smoked cannabis daily. There were 362 (72.4%) who took alcohol regularly and 79 (15.8%) were heavy alcohol drinkers. Fourteen (2.8%) ate kolanuts daily and 5 (1%) took sedatives at least once weekly. No driver reported the use of cocaine, heroin, amphetamines or other psychoactive substances.
Risk of OSA in commercial drivers
Two-hundred and forty-four (48.8%) of the drivers had a high risk of OSA based on a total STOP-BANG score of ≥3. On the individual domains, regarding symptoms (STOP), 202 (40.4%) snored loudly, 176 (35.2%) felt tired or sleepy during the day and 211 (42.4%) had hypertension. One-hundred and forty-five (29%) had a combination of two of these symptoms present and 26 (5.2%) has a combination of three symptoms present. With regards to the domains on demography and anthropometry (BANG), 10 (2%) had BMI greater than 35, 147 (29.4%) were aged ≥50 years, and 63 (12.6%) had neck circumference greater than 40 cm (all were male). No driver admitted to having been observed to have stopped breathing during sleep.
Risk of excessive daytime sleepiness and relationship to the OSA risk
Based on the ESS score, 351 (70.2%) of the drivers were getting restful sleep (ESS score 0-5), 77, (15.4%) could have their sleep improved (ESS score 6-9) and 72 (14.4%) had EDS, possibly due to OSA (ESS score ≥10). In correlation analysis, OSA score correlated positively and significantly with the ESS score (Pearson's correlation 0.29, P < 0.001). In intra-group comparison based on risk category, 56 (23%) of those at high risk of OSA also had excessive day time sleepiness compared to 16 (6.2%) of those with low risk of OSA (Pearson's X2 = 28.2, P < 0.001). Figure 1 shows a comparison of measures of central tendency of the ESS scores across the STOP-BANG risk category.
Figure 1.

Comparison of measures of central tendency of the ESS scores across the STOP BANG risk category. The median ESS score is higher for those with high risk of OSA than for those with low risk of OSA. There is greater variation in the ESS score in those at high risk of OSA but most are within the 95% confidence interval with very few outliers
Determinants of high risk of OSA and excessive daytime sleepiness
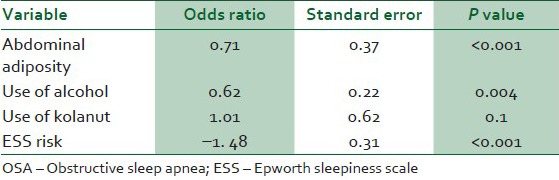
Multiple logistic regression analysis was done to identify the independent determinants of OSA risk [Table 2]. After univariate regression, abdominal adiposity, alcohol intake, use of kolanut and risk of excessive day time sleepiness were included in the model. Potential determinants represented in the STOP-BANG questionnaire (snoring, tired or sleepy during the day, hypertension, obesity, age, neck circumference and male gender) were excluded from the model. Abdominal adiposity (P < 0.001) use of alcohol (P = 0.004) and excessive daytime sleepiness (P < 0.001) were significant associated with OSA risk and are thus independent determinants of OSA.
Table 2.
Multiple logistic regression analysis for the determinants of OSA risk
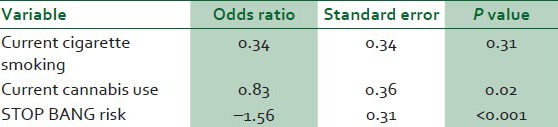
To assess the independent determinants of excessive daytime sleepiness, a multiple logistic regression analysis was also conducted [Table 3]. The model included, current smoking, current cannabis use, and the OSA risk after univariate analysis. The independent determinants of excessive day time sleepiness were the OSA risk (P < 0.001) and the use of cannabis (P = 0.02).
Table 3.
Multiple logistic regression analysis for the determinants of risk of excessive day time sleepiness
Factors associated with past-RTA
Sixty-one (12.2%) of the drivers admitted to a past history of at least one RTA. Twenty-one (34.4%) of them believed that excess alcohol intake contributed to the accident and none reported that feeling sleepy contributed to the accident. There was no difference in the prevalence of high risk of OSA in drivers with and without a past history of RTA (X2 = 2.1, P = 0.2). Similarly there was no statistical difference in the risk of EDS (ESS ≥10) in those with past history of RTA compared to those without (X2 = 2.7, P = 0.1). The BMI category (obese or not obese) was also not associated with a past history of RTA (X2 = 1.7, P = 0.4).
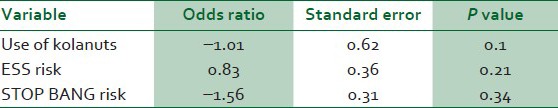
Use of kolanuts was a statistically significant determinant of past RTA on univariate analysis (P = 0.07) but when imputed in a multiple logistic regression model with other potential risk factors (ESS risk, STOP-BANG risk) [Table 4], none was independently associated with risk of RTA in the past.
Table 4.
Multiple logistic regression analysis for determinants of history of past road traffic accident
DISCUSSION
The potential impact of OSA on the performance of commercial drivers in relation to driving safety is of major public health importance. According to reports from the Federal Road Safety Commission in Nigeria, Nigeria ranks second to Eritrea in RTA rates in sub-Saharan Africa.28 Current medical requirements for commercial drivers’ certification in Nigeria include tests of vision and general medical examination, blood pressure, and history of epilepsy. However the risk of excessive daytime sleepiness or OSA is not addressed.29 The Federal Highway Administration in the United States of America has published standards for medical examination of commercial drivers regarding OSA.30
In this study, approximately half of the drivers were found to have a high risk of OSA, and this in turn was associated with excessive daytime sleepiness in about one-quarter. The prevalence of OSA in our study affirms the figures reported from other populations. In a study conducted in Australia by Howard et al., about 50% of over 3000 drivers assessed using a questionnaire had a high risk of OSA, while 45% of drivers in a Malaysian study had OSA based on an apnea/hypopnea index (AHI) greater than 5 on polysomnography.9,31 The AHI index is the number of episodes of apnea or hypopnea occurring per hour of sleep during a polysomnography test. Apnea is the complete cessation of airflow or greater than 50% reduction in airflow lasting at least 10 seconds, while hypopnea is <50% reduction in airflow lasting longer than 10 seconds that is accompanied by ≥4% oxygen desaturation or by arousal from sleep. The prevalence of excessive daytime sleepiness in our study overall (14%) was also similar to that in Edinburgh where 20% of the drivers had excessive daytime sleepiness using the ESS.12
The occupational hazards attributable to OSA and EDS in commercial drivers are particularly significant because the risk extends, not just to the individuals themselves, but also to third parties including passengers and other road users. Pack et al. demonstrated that commercial drivers with OSA had marked sleepiness and impaired driving performance.10 Simulated driving experiments have also demonstrated impaired steering ability in those with OSA compared to controls, with patients with OSA wandering more often from the road and having delayed response to distractions.32,33 Two meta-analyses have clearly shown that there is an increased risk of RTA among patients with OSA and this risk is actually more profound in those patients with very severe OSA (AHI ≥30).34,35 Although we did not demonstrate any direct relationship between OSA and ESS risk with past history of RTA, the potential impact of these conditions on the high rate of RTAs in our population may have been masked by the use of self-reported RTA (which is retrospective, subject to bias, under-reported and not verifiable in the absence of official records). Drivers can deliberately under-report the symptoms of excessive daytime sleepiness or sleepiness while driving to appear competent and many episodes of micro sleep may go unnoticed when they occur.36 Additionally, intra-city drivers often drive shorter distances per trip compared to long distance drivers and may have the opportunity to catch short naps while waiting for passengers in the parks. Micro-sleep tends to occur on long stretches of road without traffic where the driving is monotonous in contrast to intra-city driving. The effects of OSA goes beyond increasing the risk of RTA, as the impaired neuro-cognitive functioning due to OSA also results in reduced productivity, mood disorders including depression, irritability, poor libido and overall negative impact on the quality of life.2,3 There is a strong association of OSA in the etiology and adverse outcomes in several cardiovascular conditions such as hypertension, stroke, coronary artery disease, diabetes mellitus and cardiac arrhythmias.4,37,38
In evaluating risk factors for OSA in this study, the independent determinants considered included snoring, daytime sleepiness, witnessed apnea during sleep, hypertension, obesity (class 2), age, neck circumference and male gender. Documented risk factors for OSA include snoring, increasing age, male gender, obesity (both central and nuchal), altered craniofacial anatomy, decreased posterior airspace from various causes and cigarette smoking.39,40,41 Use of alcohol and sedatives worsens symptoms in those with OSA.39 The STOP-BANG questionnaire used in our study incorporates class 2 obesity (BMI 35-39.9) in the risk assessment; however, we demonstrated that abdominal adiposity independent of BMI was also a significant determinant of OSA risk. The high rate of psychoactive substances use among commercial drivers in this study and the demonstrated interaction with OSA risk and EDS has the potential of further impairing driving safety. This makes it imperative for the regulatory authorities to make education and enforcement of laws relating to abstinence from alcohol and cannabis during work hours a priority in improving road safety.
The implications of the finding in our study are that a significant proportion of commercial drivers in the Lagos metropolis are at increased risk of adverse cardiovascular outcome due to the high OSA risk and use of psychoactive substances and are also potentially at increased risk of RTA. This thus serves as the rationale for recommending that commercial drivers in Nigeria should be screened for OSA using validated questionnaires as part of medical assessment for initial issue and subsequent renewal of commercial vehicle licences. Further formal assessment using polysomnography can then be offered to those at high risk to make a definite diagnosis of OSA. Those confirmed to have OSA should be treated appropriately using several modalities including weight loss (improves overall cardiovascular outcome), oral appliances (that keep the airway open during sleep) and continuous positive airway pressure (CPAP). The role of CPAP treatment in improving driving skills and reducing RTA in compliant patients has been clearly demonstrated.42,43,44
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.White DP. Sleep related breathing disorder: Pathophysiology of obstructive sleep apnoea. Thorax. 1995;50:797–804. doi: 10.1136/thx.50.7.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al Lawati NM, Patel SR, Ayas NT. Epidemiology, risk factors, and consequences of obstructive sleep apnoea and short sleep duration. Prog Cardiovasc Dis. 2009;51:285–93. doi: 10.1016/j.pcad.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 3.Rakel RE. Clinical and societal consequences of obstructive sleep apnoea and excessive daytime sleepiness. Postgrad Med. 2009;121:86–95. doi: 10.3810/pgm.2009.01.1957. [DOI] [PubMed] [Google Scholar]
- 4.Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A. Sleep apnoea and cardiovascular disease. Circulation. 2008;118:1080–111. doi: 10.1161/CIRCULATIONAHA.107.189375. [DOI] [PubMed] [Google Scholar]
- 5.Williams HL, Lubin A, Goodnow JJ. Impaired performance with acute sleep loss. Psychol Monogr. 1959;73:1–26. [Google Scholar]
- 6.Home JA, Reyner LA. Sleep related vehicle accidents. BMJ. 1959;310:565–7. doi: 10.1136/bmj.310.6979.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Atubi AO. Determinants of road traffic accident occurrences in Lagos state: Some lessons for Nigeria. [Last accessed on 19 Jun 2012]. Available from: http://www.ijhssnet.com/journals/Vol 2 No 6 Special../23.pdf .
- 8.Adekoya BJ, Adekoya AO, Adepoju FG, Owoeye JF. Driving under influence among long distance commercial drivers in Ilorin, Nigeria. Int J Biol Med Res. 2011;2:870–3. [Google Scholar]
- 9.Howard ME, Desai AV, Grunstein RR, Hukins C, Armstrong JG, Joffe D, et al. Sleepiness, sleep disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med. 2004;170:1014–21. doi: 10.1164/rccm.200312-1782OC. [DOI] [PubMed] [Google Scholar]
- 10.Pack AI, Maislin G, Staley B, Pack FM, Rogers WC, George CF, et al. Impaired performance in commercial drivers: Role of sleep apnea and short sleep duration. Am J Respir Crit Care Med. 2006;174:446–54. doi: 10.1164/rccm.200408-1146OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shiomi T, Arita AT, Sasanabe R, Banno K, Yamakawa H, Hasegawa R, et al. Falling asleep while driving and automobile accidents among patients with obstructive sleep apnea-hypopnea syndrome. Psychiatry Clin Neurosci. 2002;56:333–4. doi: 10.1046/j.1440-1819.2002.01004.x. [DOI] [PubMed] [Google Scholar]
- 12.Vennelle M, Engleman HM, Douglas NJ. Sleepiness and sleep-related accidents in commercial bus drivers. Sleep Breath. 2010;14:39–42. doi: 10.1007/s11325-009-0277-z. [DOI] [PubMed] [Google Scholar]
- 13.Practice parameters for the indications for polysomnography and related procedures. Polysomnography Task Force, American Sleep Disorders Association Standards of Practice Committee. Sleep. 1997;20:406–22. [PubMed] [Google Scholar]
- 14.Chung F, Yegneswaran B, Liao P, Chung SA, Viaravanathan S, Islam S, et al. STOP questionnaire; A tool to screen patients with obstructive sleep apnea. Anesthesiology. 2008;108:812–21. doi: 10.1097/ALN.0b013e31816d83e4. [DOI] [PubMed] [Google Scholar]
- 15.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnoea syndrome. Ann Intern Med. 1999;131:485–91. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- 16.Gross JB, Bachenberg KL, Benumof JL, Caplan RA, Connis RT, Cote CJ, et al. Practiceguidelines for the perioperative management of patients with obstructive sleepapnoea: A report by the American Society of Anaesthesiologists task force on perioperative management of patients with obstructive sleep apnoea. Anaesthesiology. 2006;104:1081–93. doi: 10.1097/00000542-200605000-00026. [DOI] [PubMed] [Google Scholar]
- 17.National Health and Nutrition Examination Survey (NHANES) Anthropometry procedures manual. 2007. Jan, [Last accessed on 1 Sep 2012]. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf .
- 18.Han TS, van Leer EM, Seidell JC, Lean ME. Waist circumference action levels in theidentification of cardiovascular risk factors: Prevalence study in a random sample. BMJ. 1995;311:1401–5. doi: 10.1136/bmj.311.7017.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eknoyan G. AdolpheQuetlet: The average man and the indices of obesity. Nephrol Dial Transplant. 2001;23:47–51. doi: 10.1093/ndt/gfm517. [DOI] [PubMed] [Google Scholar]
- 20.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults; The Evidence Report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51–209S. [PubMed] [Google Scholar]
- 21.O’Brien E, Waeber B, Parati G, Staessen J, Myers MG. Blood pressure measuring devices: Recommendations of the European Society of Hypertension. BMJ. 2001;322:531–6. doi: 10.1136/bmj.322.7285.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.The Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation and Treatment of High Blood Pressure. NIH publication. 2004 No. 04-5230. [Google Scholar]
- 23.Grundy SM, Pasternak R, Greenland P. Assessment of cardiovascular risk by use of multiple-risk-factor assessment equations; A Statement for Healthcare Professionals From the American Heart Association and the American College of Cardiology. Circulation. 1999;100:1481–92. doi: 10.1161/01.cir.100.13.1481. [DOI] [PubMed] [Google Scholar]
- 24.Chung F, Yegneswaran B, Liao P, Chung SA, Viaravanathan S, Islam S, et al. Validation of the Berlin questionnaire, the American Society of Anaesthesiologist checklist as screening tools for obstructive sleep apnoea in surgical patients. Anaesthesiology. 2008;108:822–30. doi: 10.1097/ALN.0b013e31816d91b5. [DOI] [PubMed] [Google Scholar]
- 25.Abrishami A, Khajehdehi A, Chung F. A systematic review of screening questionnaires for obstructive sleep apnoea. Can J Anaesth. 2010;57:423–38. doi: 10.1007/s12630-010-9280-x. [DOI] [PubMed] [Google Scholar]
- 26.John MW. A new method to measure daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1999;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 27.Johns MW. Daytime sleepiness, snoring, and obstructive sleep apnea. The Epworth sleepiness scale. Chest. 1993;103:30–6. doi: 10.1378/chest.103.1.30. [DOI] [PubMed] [Google Scholar]
- 28. [Last accessed on 12 June 2012]. Accessed from http://www.punchng.com/news/ nigeria-ranks-second-to-eritrea-in-road-accidents-frsc/
- 29. [Last accessed on 12 June 2012]. Accessed from: http://www.viodvla.com/sl/page.php?pg=Driverlicence and subpg=Driver licence process .
- 30.Publication No. FHWA- MC-91-004. Washington: USDOT; 1991. [Last accessed on 12 June 2012]. U.S. Department of Transportation, Federal Highway Administration, Office of Motor Carriers. Conference on Respiratory/PulmonaryDisorders and Commercial Drivers. http://www.fmcsa.dot.gov/documents/pulmonary1.pdf . [Google Scholar]
- 31.Yusoff MF, Baki MM, Mohamed N, Mohamed AS, Yunus RM, Ami M, et al. Obstructive sleep apnea among express bus drivers in Malaysia: Important Indicators for Screening. Traffic Inj Prev. 2010;11:594–9. doi: 10.1080/15389588.2010.505255. [DOI] [PubMed] [Google Scholar]
- 32.George CF, Boudreau AC, Smiley A. Simulated driving performance in patients with obstructive sleepapnea. Am J Respir Crit Care Med. 1996;154:175–81. doi: 10.1164/ajrccm.154.1.8680676. [DOI] [PubMed] [Google Scholar]
- 33.Juniper M, Hack MA, George CF, Davies RJ, Stradling JR. Steering simulation performance in patients with obstructivesleep apnoea (OSA) and matched control subjects. Eur Respir J. 2000;15:590–5. doi: 10.1034/j.1399-3003.2000.15.27.x. [DOI] [PubMed] [Google Scholar]
- 34.Tregear S, Reston J, Schoelles K, Phillips B. Obstructive sleep apnea and risk of motor vehicle crash: Systematic review and meta-analysis. J Clin Sleep Med. 2009;5:573–81. [PMC free article] [PubMed] [Google Scholar]
- 35.Ellen RL, Marshall SC, Palayew M, Molnar FJ, Wilson KG, Man-Son-Hing M. Systematic review of motor vehicle crash risk in persons with sleep apnea. J Clin Sleep Med. 2006;2:193–200. [PubMed] [Google Scholar]
- 36.Bunn TL, Slavova S, Struttmann TW, Browning SR. Sleepiness/fatigue and distraction/inattention as factors for fatal versus nonfatal commercial motor vehicle driver injuries. Accid Anal Prev. 2005;37:862–9. doi: 10.1016/j.aap.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 37.Yaggi H, Concato J, Kernan WN, Lithchman JH, Brass LM, Mohsenein V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034–41. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- 38.Punjabi NM, Sorkin JD, Katzel LI, Goldberg AP, Schwartz AR, Smith PL. Sleep-disordered breathing and insulin resistance in middle-aged and overweight men. Am J Respir Crit Care Med. 2002;165:677–82. doi: 10.1164/ajrccm.165.5.2104087. [DOI] [PubMed] [Google Scholar]
- 39.Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:136–43. doi: 10.1513/pats.200709-155MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cistulli PA. Craniofacial abnormalities in obstructive sleep apnoea: Implications for treatment. Respirology. 1996;1:167–74. doi: 10.1111/j.1440-1843.1996.tb00028.x. [DOI] [PubMed] [Google Scholar]
- 41.Franklin KA, Gislason T, Omenaas E, Jogi R, Jensen EJ, Lindberg E. The influence of active and passive smoking on habitual snoring. Am J Respir Crit Care Med. 2004;170:799–803. doi: 10.1164/rccm.200404-474OC. [DOI] [PubMed] [Google Scholar]
- 42.Findley L, Smith C, Hooper J, Dineen M, Suratt PM. Treatment withnasal CPAP decreases automobile accidents in patients with sleep apnea. Am J Respir Crit Care Med. 2000;161:857–9. doi: 10.1164/ajrccm.161.3.9812154. [DOI] [PubMed] [Google Scholar]
- 43.George CF. Reduction in motor vehicle collisions following treatment of sleep apnoea with nasal CPAP. Thorax. 2001;56:7–12. doi: 10.1136/thorax.56.7.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hack M, Davies RJ, Mullins R, Choi SJ, Ramdassingh-Dow S, Jenkinson C, et al. Randomised prospective parallel trial of therapeutic versussub-therapeutic nasal continuous positive airway pressure on simulated steering performance in patients with obstructive sleep apnoea. Thorax. 2000;55:224–31. doi: 10.1136/thorax.55.3.224. [DOI] [PMC free article] [PubMed] [Google Scholar]


