Abstract
A 40-year-old male presented with mid-thoracic backache and progressive, ascending, spastic, paraparesis for one year. Magnetic resonance imaging demonstrated an extraosseous, extradural mass, without any bone invasion at the T2-T4 vertebral levels, located dorsal to the thecal sac. The spinal cord was compressed ventrally. The lesion was totally excised after a T2-T4 laminectomy. Histopathological examination revealed a cavernous hemangioma. The authors reported this case and reviewed the literature, to explain why extraosseous, extradural, cavernous hemangiomas should be considered in the differential diagnosis of extradural thoracic compressive myelopathy.
Keywords: Cavernous hemangioma, epidural, magnetic resonance imaging, myelopathy, thoracic spine
Introduction
Cavernous hemangiomas (CH) in the spine are uncommon hamartomatous malformations, which occur per se in vertebral bodies, but may have an associated extradural component. Previously described nomenclatures include cavernous angiomas, hemangiomas, varicosities, venous angiomas, and angiolipomas, with cavernous vessels.[1,2,3,4,5] This may be better understood in the context that histological classification can be affected by the predominant type of vascular channels. Extraosseous, extradural cavernous hemangiomas (EECH) are relatively uncommon, differ radiologically from their cranial counterparts, and may be difficult to diagnose preoperatively.[6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22] Purely extradural causes of compressive myelopathy are by themselves rare entities. The authors discuss EECH as a part of this differential diagnosis.
Case Report
A 40-year-old male presented with a band-like feeling of constriction at the nipple level for eight months, followed by numbness to all modalities of sensation below this level. During the last month, progressive ascending spastic paraparesis had rendered him wheelchair-bound. There was no history of trauma, fever, deformity, tenderness over the spine, weight loss, or bowel or bladder dysfunction. He had no neurocutaneous markers. He had grade 3/5 medical Research Council (MRC) spastic paraparesis, exaggerated bilateral knee and ankle reflexes, and sustained ankle clonus on the left side. There was a graded sensory impairment to all modalities below the fourth thoracic dermatome. His hematological and biochemical investigations were within normal limits. The chest skiagram was normal.
Radiology
Magnetic resonance imaging (MRI) of the thoracic spine revealed an extradural lesion, opposite the T2-T4 vertebral bodies, which was homogenously isointense on T1- and hyperintense on T2-weighted images. The lesion was located dorsally and had compressed the thoracic cords ventrally. The axial sections revealed that the mass was located eccentrically; more on the patient's left side, with a small projection into the intervertebral foramen. The spinal cord at that level could be seen displaced ventrally and to the right. A central hyperintensity on T2-weighted imaging, within the cord substance, was also observed. Of note was the presence of a remote intraosseous T8 vertebral hemangioma. The lesion enhanced avidly and homogenously with contrast [Figure 1]. Computerized tomography (CT) of the upper dorsal spine did not reveal any bony destruction or widening of the intervertebral foramen. A radiological differential of an extradural schwannoma or meningioma was considered.
Figure 1.

a: T2-weighted, mid-sagittal magnetic resonance image revealing a thoracic, hyperintense, solitary, extradural mass (black arrows) opposite the D2-4 vertebral bodies. The signal intensity differs from that of the cerebrospinal fluid, but is similar to that of a remote intraosseous hemangioma within the D8 vertebral body. Axial magnetic resonance images reveal an eccentrically placed dorsal extradural mass (asterisk), which is isointense on T1- (b) and hyperintense on T2- (c) weighted images, with left foraminal extension (black dashed arrow)
Surgery
The patient underwent a T2-T4 laminectomy. Intraoperatively, the mass was encountered within the epidural fat and immediately beneath the laminae. It was reddish in color, firm, friable, and highly vascular. It was located epidurally, mostly dorsal to the thecal sac, but also extended laterally to the left, along the left T2 nerve root sheath. Its blood supply was derived from the intervertebral foramina on both sides. Initially, the tumor's dorsal surface was devascularized, with bipolar cautery, under the operating microscope. Its arterial feeders were then sequentially cauterized and interrupted, just medial to the intervertebral foramina, taking care not to injure the dorsal nerve roots. The lesion was then peeled off the surface of the dura and the adjacent nerve sheaths. The lesion was excised en bloc. The underlying dura was then opened, taking care to preserve the arachnoid, to ensure total microsurgical excision.
The patient was discharged 48 hours after surgery. His postoperative course was significant for a subjective improvement in spasticity and numbness. The histopathological examination indicated a CH [Figure 2]. On the last follow-up, 12 months after surgery, a check craniospinal MRI confirmed complete excision, with no recurrence at the operative site and no other new lesions. His power and sensations were nearly normal and he had returned to work.
Figure 2.
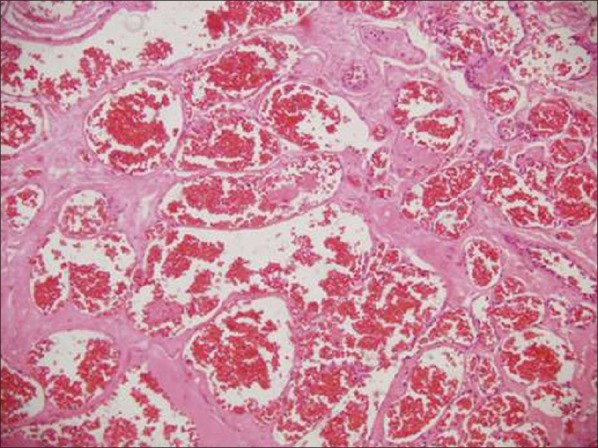
Photomicrograph showing numerous dilated vascular channels filled with blood and separated from each other by fibrous septae. These vascular channels do not communicate with each other (H and E ×200)
Discussion
Epidemiology
Cavernous hemangiomas are ubiquitous. Within the central nervous system, they tend to occur predominantly within the cranial cavity's supratentorial compartment.[7] Within the spine, CH are rare. Hillman and Bynke (1991) reported an incidence of 0.22 cases/million/year.[21] Although EECH are supposedly rarer, slightly less than a 100 cases have been reported in the literature to date, since Globus and Doshay first described this entity in 1929.[1,22] In this specific subgroup, a female preponderance is noted (70%). The average age at diagnosis has been reported to be around 40 years, which is the exact age of our patient. EECH are generally seen in the thoracic spine (60%), and are typically located posterolaterally and may extend into the neural foramina (19%). An extraspinal component may be evident in about 13% of all cases. The most common presentation is that of slowly progressive paraparesis (71%) and radiculopathy (10%).[8,10,18,19] Taking all these features into account, our patient had a fairly classical presentation. Rarely, acute paraparesis has also been reported and been ascribed to intralesional thrombosis and/or hemorrhage, with subsequent compression from an epidural hematoma.[7,8,10,11,18]
Investigations
An MRI is the investigation of choice and demonstrates a well-circumscribed, lobulated lesion, iso- to-hypointense to the spinal cord on T1- and hyperintense on T2-weighted images, with avid homogenous post-contrast enhancement.[6,7,8,9,10,14,22] The peripheral rim of hypointensity, resulting from hemosiderin deposition, is usually seen in the intramedullary CH and not in EECH. EECH also differs from their intracranial counterparts in that they are homogenously hyperintense on T2-weighted images, and enhance avidly with contrast. In this, they may resemble the CH arising from the cavernous sinus more. The absence of popcorn-like peripheral blood products may be explained by the fact that these may be washed away as EECH lie outside the blood-brain barrier.[14] It may be impossible to differentiate between extradural CH and extradural schwannomas or neurofibromas.[5,6,7,8,10,14] We were certainly unable to differentiate between the two preoperatively. During surgery too, our first thought was that of a vascular metastasis, as the lesion lacked a classical multilobulated purplish mulberry/blueberry appearance and was instead reddish. This was described by other surgeons too.[12,14,18,22] Feng et al.[9] had described the visual effect of contrast enhancement within these tumors as that of ‘wafting silk’, with lobules bulging into the interlaminar space on the sagittal images, especially so in the thoracic spine. They also described widening intervertebral foramina and bone erosion. Elegant as it sounds, we have seen this appearance before in schwannomas, meningiomas, and round cell tumors, and still believe that to make a preoperative diagnosis reliably, in a classical case such as ours, it is not possible by using MRI alone. However, the addition of angiography may make a difference. EECH are angiographically occult, but enhance brilliantly with contrast. Osseous CH show up on angiograms as would vascular schwannomas and meningiomas.[23]
Round cell tumors and even tubercular granulation tissue may be differentiated from classical EECH by a hypointense signal on T2-weighted images.[23] Similarly meningiomas too would be hypo- to-isointense to the spinal cord on T2-weighted images in a majority of the cases. Theoretically, extradural, extraosseous CH are homogeneously hyperintense on T2-weighted images, unlike schwannomas, which are likely to be heterogenous and may display a ‘target sign’.[24] Practically, differentiation may not be reliable, especially when reports in the literature describe juxtapositioned intradural schwannomas and EECH.[25] Lesions that are hyperintense/heterogeneous on both T1- and T2-weighted images should raise a greater doubt about the preoperative diagnosis of EECH.[5,18]
Our case, in hindsight, did deliver one additional pearl of instruction. The remote vertebral hemangioma at T8 shared nearly the exact MRI signal characteristics as the EECH at T2-T4. This was especially so on the T2-weighted images. The EECH [Figure 1] has a signal different from the epidural fat and CSF, but similar to the vertebral hemangioma.
Management
The majority of patients with EECH present with thoracic compressive myelopathy, secondary to lesions that are dorsally located, and pose a diagnostic conundrum on MRI. For these very reasons they are excellent surgical candidates. In expert hands, total excision via a posterior approach is the norm, with excellent results.[8,12,14,15,16,17,18,21,22] Postoperative radiotherapy has been described, but is perhaps, reserved only for patients with incomplete resection where the risks of redo surgery are deemed unacceptable.[26] More recently, spinal image-guided Stereotactic Radiosurgery (SRS) has been reported for the adjuvant therapy of residual biopsy-proven extraforaminal EECH.[13]
Once a histopathological diagnosis has been established, it may be worthwhile to scan the craniospinal axis, as 40% of the patients with spinal CH may have cranial lesions.[27]
Conclusions
Extraosseous, extradural cavernous hemangiomas are relatively rare lesions within the vertebral canal. They occur most commonly in middle-aged women, in the thoracic spine, dorsal to the spinal cord, but are eccentrically placed. Intervertebral and extraforaminal extensions can occur. EECH frequently mimic the more common schwannomas clinically and radiologically. On an MRI, classical EECH signal properties differ significantly from their intracranial and intramedullary counterparts and more closely resemble the cavernomas of the cavernous sinus. Although preoperative differentiation may not be reliable using the current imaging techniques, EECH must form an important differential diagnosis of a purely extradural thoracic compressive lesion. Surgical excision in expert hands results in an excellent outcome. Adjuvant SRS may be effective in residual lesions after subtotal removal.
Footnotes
Source of Support: Nil.
Conflict of Interest: The authors declare no potential conflict of interest.
References
- 1.Decker RE, San Augustin W, Epstein JA. Spinal epidural venous angioma causing foraminal enlargement and erosion of vertebral body: Case report. J Neurosurg. 1978;49:605–6. doi: 10.3171/jns.1978.49.4.0605. [DOI] [PubMed] [Google Scholar]
- 2.Globus JH, Doshay LJ. Venous dilatations and other intraspinal vessel alterations, including true angiomata, with signs and symptoms of cord compression. Surg Gynecol Obstet. 1929;48:345–66. [Google Scholar]
- 3.Haddad FS, Abla A, Allam CK. Extradural spinal angiolipoma. Surg Neurol. 1978;26:473–86. doi: 10.1016/0090-3019(86)90261-2. [DOI] [PubMed] [Google Scholar]
- 4.Johnston LM. Epidural hemangioma with compression of spinal cord. JAMA. 1938;110:119–22. [Google Scholar]
- 5.Graziani N, Bouillot P, Figarella-Branger D, Dufour H, Peragut JC, Grisoli F. Cavernous angiomas and arteriovenous malformations of the spinal epidural space: Report of 11 cases. Neurosurgery. 1994;35:863–4. doi: 10.1227/00006123-199411000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Lee JW, Cho EY, Hong SH, Chung HW, Kim JH, Chang KH, et al. Spinal epidural hemangiomas: Various types of MR imaging features with histopathologic correlation. AJNR Am J Neuroradiol. 2007;28:1242–8. doi: 10.3174/ajnr.A0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leu NH, Chen SC, Chou JM. MR features of posterior spinal epidural cavernous hemangioma: A case report. Chin J Radiol. 2006;31:127–31. [Google Scholar]
- 8.Hatiboglu MA, Iplikcioglu AC, Ozcan D. Epidural spinal cavernous hemangioma. Neurol Med Chir (Tokyo) 2006;46:455–8. doi: 10.2176/nmc.46.455. [DOI] [PubMed] [Google Scholar]
- 9.Feng J, Xu YK, Li L, Yang RM, Ye XH, Zhang N, et al. MRI diagnosis and preoperative evaluation for pure epidural cavernous hemangiomas. Neuroradiology. 2009;51:741–7. doi: 10.1007/s00234-009-0555-2. [DOI] [PubMed] [Google Scholar]
- 10.Aoyagi N, Kojima K, Kasai H. Review of spinal epidural cavernous hemangioma. Neurol Med Chir (Tokyo) 2003;43:471–5. doi: 10.2176/nmc.43.471. [DOI] [PubMed] [Google Scholar]
- 11.Floeth F, Riemenschneider M, Herdmann J. Intralesional hemorrhage and thrombosis without rupture in a pure spinal epidural cavernous angioma: A rare cause of acute lumbal radiculopathy. Eur Spine J. 2010;19(Suppl 2):S193–6. doi: 10.1007/s00586-010-1345-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Satpathy DK, Das S, Das BS. Spinal epidural cavernous hemangioma with myelopathy: A rare lesion. Neurol India. 2009;57:88–90. doi: 10.4103/0028-3886.48805. [DOI] [PubMed] [Google Scholar]
- 13.Sohn MJ, Lee DJ, Jeon SR, Khang SK. Spinal radiosurgical treatment for thoracic epidural cavernous hemangioma presenting as radiculomyelopathy: Technical case report. Neurosurgery. 2009;64:E1202–3. doi: 10.1227/01.NEU.0000345940.21674.AE. [DOI] [PubMed] [Google Scholar]
- 14.Sanghvi D, Munshi M, Kulkarni B, Kumar A. Dorsal spinal epidural cavernous hemangioma. J Craniovertebr Junction Spine. 2010;1:122–5. doi: 10.4103/0974-8237.77677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kivelev J, Niemelä M, Hernesniemi J. Outcome after microsurgery in 14 patients with spinal cavernomas and review of the literature. J Neurosurg Spine. 2010;13:524–34. doi: 10.3171/2010.4.SPINE09986. [DOI] [PubMed] [Google Scholar]
- 16.Doyle PM, Abou-Zeid A, Du Plessis D, Herwadkar A, Gnanalingham KK. Dumbbell-shaped intrathoracic-extradural hemangioma of the thoracic spine. Br J Neurosurg. 2008;22:299–300. doi: 10.1080/02688690701678610. [DOI] [PubMed] [Google Scholar]
- 17.Tekkök IH, Akpinar G, Güngen Y. Extradural lumbosacral cavernous hemangioma. Eur Spine J. 2004;13:469–73. doi: 10.1007/s00586-003-0658-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.D›Andrea G, Ramundo OE, Trillò G, Roperto R, Isidori A, Ferrante L. Dorsal foramenal extraosseous epidural cavernous hemangioma. Neurosurg Rev. 2003;26:292–6. doi: 10.1007/s10143-003-0275-8. [DOI] [PubMed] [Google Scholar]
- 19.Antunes A, Beck MF, Strapasson AC, Franciscatto AC, Franzoi M. Extradural cavernous hemangioma of thoracic spine. Arq Neuropsiquiatr. 2011;69:720–1. doi: 10.1590/s0004-282x2011000500029. [DOI] [PubMed] [Google Scholar]
- 20.Saringer W, Nöbauer I, Haberler C, Ungersböck K. Extraforaminal, thoracic, epidural cavernous hemangioma: Case report with analysis of magnetic resonance imaging characteristics and review of the literature. Acta Neurochir (Wien) 2001;143:1293–7. doi: 10.1007/s007010100028. [DOI] [PubMed] [Google Scholar]
- 21.Hillman J, Bynke O. Solitary extradural cavernous hemangiomas in the spinal canal. Report of five cases. Surg Neurol. 1991;36:19–34. doi: 10.1016/0090-3019(91)90127-u. [DOI] [PubMed] [Google Scholar]
- 22.Santoro A, Piccirilli M, Bristot R, di Norcia V, Salvati M, Delfini R. Extradural spinal cavernous angiomas: Report of seven cases. Neurosurg Rev. 2005;28:313–9. doi: 10.1007/s10143-005-0390-9. [DOI] [PubMed] [Google Scholar]
- 23.Shin JH, Lee HK, Rhim SC, Park SH, Choi CG, Suh DC. Spinal epidural cavernous hemangioma: MR findings. J Comput Assist Tomogr. 2001;25:257–61. doi: 10.1097/00004728-200103000-00019. [DOI] [PubMed] [Google Scholar]
- 24.Bhargava R, Parham DM, Lasater OE, Chari RS, Chen G, Fletcher BD, et al. MR imaging differentiation of benign and malignant peripheral nerve sheath tumors: Use of the target sign. Pediatr Radiol. 1997;27:124–9. doi: 10.1007/s002470050082. [DOI] [PubMed] [Google Scholar]
- 25.Thomé C, Zevgaridis D, Matejic D, Sommer C, Krauss JK. Juxtaposition of an epidural intraforaminal cavernous hemangioma and an intradural schwannoma. Spine (Phila Pa 1976) 2004;29:E524–7. doi: 10.1097/01.brs.0000144835.83018.1d. [DOI] [PubMed] [Google Scholar]
- 26.Padovani R, Tognetti F, Proietti D, Pozzati E, Servadei F. Extrathecal cavernous hemangioma. Surg Neurol. 1982;18:463–5. doi: 10.1016/0090-3019(82)90191-4. [DOI] [PubMed] [Google Scholar]
- 27.Jallo GI, Freed D, Zareck M, Epstein F, Kothbauer KF. Clinical presentation and optimal management for intramedullary cavernous malformations. Neurosurg Focus. 2006;21:e10. doi: 10.3171/foc.2006.21.1.11. [DOI] [PubMed] [Google Scholar]


