Abstract
Fear of negative evaluation, a core feature of social anxiety disorder, has been prospectively related to eating pathology over and above other established risk factors, suggesting that it may be an important cognitive risk factor for eating disorders. The present study examined reciprocal longitudinal relations among fear of negative evaluation and eating disorder risk factors using a female undergraduate sample (N=82) enrolled in an eating disorder prevention program. Cross-lagged panel analysis revealed that fear of negative evaluation was a determinant of subsequent body dissatisfaction and eating disorder symptoms. Fear of negative evaluation also predicted subsequent thin-ideal internalization among participants with high BMI, but not among those with low BMI. Fear of negative evaluation did not predict future dietary restraint or negative affect but was itself predicted by prior levels of thin ideal internalization, body dissatisfaction, dietary restraint, and negative affect. Findings suggest that fear of negative evaluation may be a useful target for reducing body image concerns and maladaptive eating behavior.
Keywords: Fear of negative evaluation, eating disorders, prevention, social anxiety, risk factors
Eating disorders (EDs) are one of the most prevalent classes of psychological disorders among adolescent and young adult women (Lewinsohn, Striegel-Moore, & Seeley, 2000; Zivin, Eisenberg, Gollust, & Golberstein, 2009). Up to 50% of college women reportedly engage in binge eating during their first year of college (Striegel-Moore, Silberstein, Grundberg, & Rodin, 1990), and about 12% either meet full diagnostic criteria for an ED or reported clinically significant subthreshold symptoms (Keel, Heatherton, Dorer, Joiner, & Zalta, 2006). A recent longitudinal study found that 18–19% of college students had clinically significant eating pathology, and 59% of those with a probable ED at baseline also reported clinically significant ED symptoms 2 years later (Zivin et al., 2009). In addition to being characterized by a chronic course, EDs are often accompanied by comorbid psychiatric conditions and contribute to significant functional impairment (Fairburn & Beglin, 1990; Heatherton, Nichols, Mahamedi, & Keel, 1995; Lewinsohn et al., 2000). Furthermore, disordered eating behavior can cause significant medical conditions including loss of bone density or osteoporosis, cardiac problems, and even death (Fairburn & Harrison, 2003; Sullivan, 1995; Treasure & Szmukler, 1995).
Given that only half of women treated with the current gold standard for ED intervention, cognitive-behavioral therapy, experience long-term symptom reduction (Fairburn et al., 2008; Wilson, Becker, & Heffernan, 2002), researchers have increasingly focused on prevention efforts (Stice, South, & Shaw, 2012). A recent meta-analysis found that 29% of prevention programs decreased eating pathology, and 51% resulted in significant decreases in one or more established ED risk factors (Stice, Shaw, & Marti, 2007). Programs that specifically promote body acceptance and use cognitive dissonance-based techniques (e.g., having participants voluntarily argue against the thin ideal of feminine beauty) were particularly efficacious (Stice et al., 2007). Some of the most efficacious prevention programs have been informed by the dual-pathway model of bulimic pathology, which posits five risk factors for the development of bulimia nervosa: social pressure to be thin, thin ideal internalization, body dissatisfaction, dieting, and negative affect (Stice, 2001; Stice & Agras, 1998). Dissonance-based programs primarily target internalization of the thin ideal and have demonstrated both efficacy and effectiveness (Becker, Bull, Schaumberg, Cauble, & Franco, 2008; Becker, Smith & Ciao, 2006; Stice, Chase, Stormer, & Appel, 2001; Stice, Mazotti, Weibel, & Agras, 2000; Stice, Shaw, Burton, & Wade, 2006; Stice, Marti, Spoor, Presnell, & Shaw, 2008; Stice, Trost, & Chase, 2003). However, there is room for improvement. Stice and colleagues (2012) have emphasized the need for establishing the causal influence of the putative risk factors that are commonly targeted in prevention programs. Indeed, although the five risk factors each significantly predict subsequent eating pathology, the full model accounts for only 33% of the variance in bulimic symptomology (Stice, 2001; Stice & Agras, 1998; Shepherd & Ricciardelli, 1998; Stice, Shaw, & Nemeroff, 1998). Improving prevention programs will require uncovering and targeting additional factors that lead to the development of EDs.
Recent research points to social anxiety-related cognitive vulnerabilities, and particularly those related to social anxiety disorder, as candidate factors. Social anxiety disorder and EDs are highly comorbid, with social anxiety disorder diagnosed in 41% of those with bulimia nervosa, 32% of those with binge eating disorder, and 25% of those with anorexia nervosa (Hudson, Hiripi, Pope, & Kessler, 2007). Furthermore, onset of social anxiety disorder appears to pre-date the onset of EDs, suggesting that social anxiety psychopathology may serve as a predisposing risk factors for the later development of EDs (Brewerton et al., 1995; Bulik, Sullivan, Fear, & Joyce, 1997; Swinbourne, Hunt, Abbott, Russell, St. Clare, & Touyz, 2012). It is possible that the disorders are linked as a result of an overlapping risk factor such as fear of negative evaluation (FNE). FNE is considered both a vulnerability factor for and a core feature of social anxiety disorder (Heimberg, Brozovich, & Rapee, 2010; Rapee & Heimberg, 1997). Because individuals high in FNE are intensely concerned with others’ evaluations and about the loss of social approval, they may be more likely to ascribe to and strive to embody social ideals such as the ‘thin ideal,’ if they believe it will protect them from negative social outcomes (Utschig, Presnell, Madeley, & Smits, 2010). Fang and Hofmann (2010) have further suggested that FNE may account for the large overlap in diagnostic features, clinical correlates, and treatment response in social anxiety disorder and body dysmorphic disorder, which is characterized by a marked concern about physical appearance and social appearance comparison and is highly comorbid with eating disorders.
FNE has been cross-sectionally related to drive for thinness (Gilbert & Meyer, 2003) and ED symptoms (Wonderlich-Tierney & Vander Wal, 2010) and prospectively related to bulimic attitudes (Gilbert & Meyer, 2003). Furthermore, Utschig and colleagues (2010) found that fear of negative evaluation (FNE) added significantly to the predictive ability of the dual-pathway etiological model (Stice & Agras, 1998) and was uniquely associated with bulimic symptoms over and above the other risk factors in the model. FNE was also correlated with three established ED risk factors: pressure to be thin, thin ideal internalization, and negative affect (Utschig et al., 2010). Levinson and Rodebaugh (2011) recently investigated the association of eating pathology with several social anxiety fears (i.e., FNE, fear of positive evaluation, fear of scrutiny, social interaction anxiety, and social appearance anxiety) and found that FNE and social appearance anxiety were the only two vulnerability factors to emerge as unique predictors of both social anxiety and ED symptoms. FNE uniquely predicted drive for thinness and restraint, over and above the other social anxiety variables, and social appearance anxiety uniquely predicted body dissatisfaction, bulimic symptoms, and shape, weight, and eating concerns.
Together, these studies provide preliminary evidence that FNE may have a place in a comprehensive etiological model of EDs. However, the extant work on FNE and eating pathology is limited by cross-sectional designs. As recommended by Stice and colleagues (2012), prevention work must investigate the causal role of purported vulnerability factors in the development of eating pathology. The present study sought to extend this line of work by examining the reciprocal relations between FNE and ED risk factors over time in context of an ED prevention program. Although this type of longitudinal design cannot clearly establish a causal role of FNE in the development of disordered eating, it effectively tests whether changes in FNE over time are associated with later changes in eating disorder psychopathology. Demonstrating that decreases in FNE precede decreases in ED symptoms in an intervention context would provide preliminary evidence for a causal role of FNE-reduction in the amelioration of ED symptoms.
The aim of this study was to investigate the interplay between FNE and ED risk factors and symptoms. Given previous work demonstrating the temporal precedence of anxiety among those with comorbid anxiety and eating disorders, we hypothesized that FNE would predict subsequent ED symptoms and risk factors (i.e., thin ideal internalization, body dissatisfaction, restrained eating, negative affect, and an ED symptom composite) during an ED prevention intervention and 12-month follow-up period.
Method
Participants
Study participants (N=82) were undergraduate women recruited from a sorority at a large Southwestern university. Recruitment methods included announcements made in sorority chapter meetings and to the psychology department’s undergraduate subject pool. Participants were reimbursed with sorority service points and extra credit points if they were enrolled in a psychology course. Ages ranged from 18 to 20 years (M = 18.7, SD = 0.7). The ethnic/racial breakdown of the sample was: 90.2% White, 10% Hispanic/Latina, 2.4% Asian, 1.2% American Indian or Alaska Native, and 6.1% other races. Body mass index (BMI) was in the healthy range, ranging from 17.5 to 28.3 (M = 21.7, SD = 2.2).
We targeted college-age women because previous work has demonstrated a high incidence of eating disorders among women of this age, with peak onset for bulimia nervosa at 19-years-old (Hudson et al., 2007). Furthermore, given high-FNE individuals’ tendency to perceive interpersonal experiences as threatening (Stopa & Clark, 1993; Vassilopoulos, 2006), they may experience particularly high levels of stress and elevated symptomology during college years, a stage characterized by increased interpersonal distress (Ross, Neibling, & Heckert, 1999).
Participation in the intervention and this study was open to all sorority members, and participants were not required to meet a predetermined cut-off score for any ED risk factors. Baseline scores on measures of ED risk factors and symptoms were comparable to community norms (Stice, Fisher, & Martinez, 2004) for adolescent and young adult women, suggesting that this sample as a whole was not at increased risk for eating pathology relative to other college women. Baseline scores for FNE were also similar to undergraduate norms (M = 32.8, SD = 10.04; Carleton, McCreary, Norton, & Asmundson, 2006).
Eating Disorders Diagnostic Scale (EDDS; Stice et al., 2000) scores indicated that 14 (17.3%) participants were experiencing clinically significant eating pathology at baseline. Two (2.5%) participants met full diagnostic criteria for bulimia nervosa and four (4.9%) met criteria for binge eating disorder. Three (3.7%) participants met criteria for subthreshold anorexia nervosa, four (4.9%) for subthreshold bulimia nervosa, and one (1.2%) for subthreshold binge eating disorder.
Procedure
The primary aim of the study was to examine outcome differences between a two-session version and a four-session version of the dissonance intervention, both of which effectively reduce ED risk factors (Becker et al., 2008; 2006; 2005; Stice et al., 2001; 2006; 2000; 2008 Stice et al., 2002). This study was guided by evidence that distributing prevention content across a greater number of sessions facilitates learning, consolidation, skills practice, and behavior change (Bouton, 2000, 2002) and by important clinical considerations such as increasing retention and enhancing group cohesion, which may be achieved by consolidating intervention content which reduces logistical scheduling difficulties. Because the two versions were identical in content and total time (i.e., two 2-hour sessions versus four 1-hour sessions) and there were no group differences in ED risk factors and symptoms at follow-up (Kilpela, DeBoer, West, Presnell, & Becker, in preparation), we collapsed across intervention conditions and examined mediation effects for the sample as a whole in the present study.
Participants provided written informed consent prior to completing the baseline questionnaire packet and beginning the first intervention session. Subsequent questionnaires were completed at post-intervention, 2-month follow-up, 6-month follow-up, and 12-month follow-up. Intervention groups were comprised of 3–11 participants (M=5.95; SD=3.54) and were led by trained peer facilitators within the sorority. Peer facilitators first participated in the intervention themselves, attended two 4-hour training sessions, and were supervised throughout the intervention by the first and fourth authors.
Session activities were manualized (see Becker, Smith, & Ciao, 2005) and included defining, critiquing, and listing the costs of pursuing the thin-ideal of feminine beauty; discussing pressures to be thin; discussing varying definitions of beauty across time and culture; developing strategies to improve the body image of sorority members; and role playing dissuading others from pursuing the thin-ideal. Participants were also asked to complete counter-attitudinal home exercises (e.g., listing positive physical and emotional/mental qualities while looking in a mirror) between sessions, which were discussed at the following session.
Measures
Thin-ideal internalization
We assessed thin-ideal internalization with the 10-item Ideal-Body Stereotype Scale—Revised (IBSS–R; Stice, Ziemba, Margolis, & Flick, 1996). Participants responded to statements (e.g., “Thin women are more attractive”) on a Likert scale from 1 = strongly disagree to 5 = strongly agree. The IBSS–R has acceptable retest reliability (r = .63; Stice, 2001), internal consistency (α= .89), as well as convergent, discriminative, and predictive validity (Stice & Agras, 1998). Internal consistency was adequate (α= .73) in the current sample at baseline.
Body dissatisfaction
Nine items assessing satisfaction with body parts, shape, and weight from the Satisfaction and Dissatisfaction with Body Parts Scale (SDBPS; Berscheid, Walster, & Bohrnstedt, 1973) were used to measure body dissatisfaction. Participants indicated their degree of satisfaction with each item on a Likert scale from 1 = extremely satisfied to 5 = extremely dissatisfied. This version of the scale has demonstrated internal consistency (α= .94), temporal reliability (r = .90), and predictive validity (Stice & Agras, 1998). This scale had good internal consistency (α= .91) in this sample at baseline.
Restrained eating
The Dutch Restrained Eating Scale (DRES; van Strien et al., 1986) was used to assess the frequency of dieting behaviors. The DRES contains 10 items (e.g., “Do you deliberately try to eat foods that are slimming?”) and asks participants to respond on a Likert scale from 1 = never to 5 = always. The scale is internally consistent (α= .95; van Strien, Frijters, Bergers, & Defares, 1986) and has demonstrated good predictive validity (r = .38–.46; Laessle, Tuschl, Kotthaus, & Pirke, 1989; van Strien, Frijters, Van Staveren, et al., 1986; Wardle, 1987; Wardle & Beales, 1987). Internal consistency in the current sample was at baseline was good (α= .91).
Negative affect
We assessed negative affect with the Positive and Negative Affect Schedule – Expanded Form (Watson & Clark, 1992). The 23 items that forms the fear, hostility, guilt, and sadness subscales were used. Participants reported the extent to which they have experienced the emotional states in the past two weeks using a Likert scale ranging from 1 = very slightly or not at all to 5 = extremely. This scale has shown adequate internal consistency (α= .82–.87), retest reliability (r = .57–.68), convergent validity (r = .92–.95), and discriminant validity (r = −.16–.00; Watson & Clark, 1999). Internal consistency for this sample at baseline was good (α= .94).
Eating disorder symptoms
The Eating Disorder Diagnostic Scale (EDDS; Stice, Telch, & Rizvi, 2000) was used to assess DSM-IV ED symptoms. The EDDS has shown good internal consistency (α= .89), 1-week retest reliability (r = .87), criterion validity (K = .78), and sensitivity to detecting intervention effects (Stice et al., 2004; Stice, Presnell, et al., 2007). We used the EDDS Symptom Composite as a measure of overall ED symptoms for this study.
Fear of negative evaluation
The Brief Fear of Negative Evaluation Scale—Revised (BFNE-R; Carleton et al., 2006) is an 12-item questionnaire that measures fear and distress related to negative evaluation from others on a 5-point scale, ranging from 1 = not at all characteristic of me to 5 = extremely characteristic of me. The psychometric properties of the BFNE-R, which has only straightforwardly worded items, are superior to the original BFNE (Carleton et al., 2006; Leary, 1983). The BFNE-R has demonstrated high internal consistency (α= .95), inter-item correlation (r = .72), predictive validity (AUC = .79; Carleton, Collimore, McCabe, & Antony, 2011; Carleton et al., 2006). Internal consistency in the present sample was good (α= .94).
Data Analytic Strategy
In order to investigate the interplay between the reduction in FNE and the five dependent variables, we used a within-person, cross-lagged panel analysis. Analyses were conducted using multilevel linear modeling (MLM) in SPSS® Version 20, with repeated measures (level 1) nested within participants (level 2). The covariance of the errors of repeated measures was modeled as autoregressive [AR(1)].
MLM is one of the recommended techniques for longitudinal data analysis and has the benefits of incorporating all data and reducing bias due to participant dropout (Hamer & Simpson, 2009). Rather than completely omitting subjects with missing data or imputing missing data by carrying previous values forward, MLM imputes missing data using an estimated regression line for each participant based on their existing data, and, in cases of dropout, the participant’s curve is projected to the end of the study.
Cross-lagged panel analyses allow for examination of the temporal and reciprocal relations between the hypothesized mediating variable (of assessment time point in this study; i.e., lower-level mediation), FNE, and each outcome variable (thin ideal internalization, body dissatisfaction, dietary restraint, negative affect, and ED symptoms). Cross-lagged panel designs are among the most effective methods for determining the direct effects and reciprocal relations of variables on each other over time (Kessler & Greenberg, 1981; Menard, 1991; Tschacher & Ramseyer, 2009). We selected this analytic strategy instead of a latent trajectory approach because, although a latent trajectory approach calculates all relationships at each time point, it models between-subjects relations as opposed to within-subject relationships (Curran & Bauer, 2011; Curran et al., 2012). The purpose of this study is to examine the relation of FNE with risk factors within individuals over time, and methods for examining within-subject changes using a latent trajectory approach have not yet been well established in the literature.
In order to account for unequal time intervals between assessments and potential differences in the prospective relationships across phases ranging from no treatment (i.e., baseline), post-treatment (i.e., acute intervention effects), and follow-up (which could represent maintenance, deterioration, or continued growth of intervention effects), we used dummy codes for assessment points (e.g., DPost-Tx, D2Month, D6Month, D12Month) in place of a time variable (e.g., Week0, Week3, Week12, etc.). This approach imposes no specific functional form (e.g., linear, quadratic, etc.) on the means over time, and freely estimates the means at each time point. Thus, we were able to test if the relation between FNE and EDRF at any given time point differed significantly from the reference time point (we used the 6-mo fu as the reference). We included the dummy codes and each of their interactions with FNEt−1 and EDRFt−1 as moderators of all Level 1 relationships. When none of the three dummy variables significantly interacted with EDNFt−1 or FNEt−1, the interaction and main effect for that dummy variable were dropped from the model. Given its association with both ED risk factors and social anxiety (Petry, Barry, Pietrzak, & Wagner, 2008; Westerberg-Jacobson, Edlund, & Ghaderi, 2010), BMI was initially entered in all analyses both a predictor and as a moderator of FNE; these terms were dropped from models when they were not significant. We ran the following two models (with j representing the assessment time point and i representing the individual) for each outcome variable, separately:
At Level 1 each outcome variable at each time point (t) was predicted by each assessment point; two time-varying predictors: FNE at the previous assessment (t − 1); the outcome at the previous assessment (t − 1); the interactions of each assessment point with FNE t−1; and BMI and its interaction with FNEt−1. By modeling the outcome at time t − 1 as an additional predictor of the outcome at time t, we were able to control for prior levels of the outcome and for the possibility of “reverse” causation (i.e., the possibility that the relation between FNE at time t − 1 and the outcome at time t was a result of the outcome at time t − 1 causing both FNE at time t − 1 and the outcome at time t; see Smits et al., 2006; Smits et al., 2012).
In addition, we computed the models with FNE as the dependent variable predicted by its value at the previous assessment (t − 1) and by each outcome variable at the previous assessment in order to explicitly test the reciprocal relations (t − 1; see Figure 1). The MLM level 1 models testing whether the outcome caused the mediator were:
Figure 1.
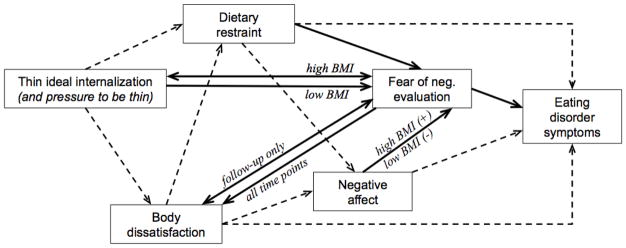
Hypothesized temporal order of symptom reduction in the context of a dissonance prevention intervention, with pathways supported by the current study bolded.
Results
Preliminary Analyses
Means, standard deviations, and baseline correlations for the main study variables are presented in Tables 1 and 2. FNE (b = −2.24, t(79) = −8.36, p < .001) and four of the five outcome variables decreased from baseline to 12-month follow-up (thin ideal internalization, b = −.07, t(121) = −4.55, p < .001; body dissatisfaction, b = −.09, t(85) = −4.27, p < .001; dietary restraint, b = −.38, t(112) = −3.07, p =. 003; ED symptoms, b = −1.22, t(71) = −5.31, p < .001). The decrease in negative affect over time was not significant (b = −.03, t(81) = −1.76, p = .083).
Table 1.
Sample characteristics
| Variable | n | M | SD |
|---|---|---|---|
| Age | 82 | 18.70 | 0.70 |
|
| |||
| Body mass index (BMI) | 85 | 21.72 | 2.17 |
| Fear of negative evaluation (BFNE) | 80 | 34.63 | 9.92 |
| Thin ideal internalization (IBSS–R) | 81 | 3.39 | 0.47 |
| Body dissatisfaction (SDBPS) | 80 | 1.85 | 0.69 |
| Dietary restraint (DRES) | 79 | 2.62 | 0.78 |
| Negative affect (PANAS) | 80 | 1.52 | 0.57 |
| Eating disorder symptoms (EDDS) | 79 | 16.77 | 10.67 |
| Race/Ethnicity | n | % |
|---|---|---|
| Caucasian | 74 | 90.24 |
| Hispanic/Latina | 8 | 10.00 |
| Asian/Asian American | 2 | 2.44 |
| American Indian/Alaska Native | 1 | 1.21 |
| Other | 5 | 6.10 |
Table 2.
Correlations of study variables at baseline.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Fear of negative evaluation | -- | |||||
| 2. Thin ideal internalization | 0.42** | -- | ||||
| 3. Body dissatisfaction | 0.18 | 0.09† | -- | |||
| 4. Dietary restraint | 0.45** | 0.56** | 0.30** | -- | ||
| 5. Negative affect | 0.33** | 0.19 | 0.22† | 0.21† | -- | |
| 6. Eating disorder symptoms | 0.44** | 0.59** | 0.42** | 0.63** | 0.38** | -- |
As detailed below, BMI interacted with FNE in the prediction of thin ideal internalization, and BMI interacted with negative affect in the prediction of FNE. We also found main effects for BMI for both body dissatisfaction and dietary restraint when controlling for prior levels of those variables and prior levels of FNE. BMI and its interactions were removed from analyses in which there were no significant BMI interactions or main effects.
Cross-Lag Panel Analyses
Thin ideal internalization
FNE interacted with BMI (b = −0.003, t = 2.214, p = .030) in predicting subsequent thin ideal internalization. When probing the interactions, we found that the relation between FNE and thin ideal internalization was not significant for women with a low BMI (i.e., 1 standard deviation (SD) below the mean, BMI = 19.55; b = 0.001, t = 0.352, p = .725), but it was significant for those with elevated BMI (i.e., 1 SD above the mean, BMI = 23.89; b = −0.015, t = −4.000, p < .001). Among those with a low BMI, prior FNE did not predict thin ideal internalization at any assessment point (DPT: b = 0.001, t = 0.352; p = .725; D2MFU: b = 0.005, t = 1.325; p = .186; D6MF: b = 0.005, t = 1.333; p = .184; D12MF: b = 0.006, t = 1.732; p = .085). For women with elevated BMIs, on the other hand, the association was significant and negative at all time points (DPT: b = −0.015, t = −4.000; p < .001; D2MFU: b = −0.009, t = −2.504; p = .013; D6MF: b = −0.010, t = −2.535; p = .012; D12MF: b = −0.010, t = −2.463; p = .014).
There was also a significant interaction with between FNE and assessment point, such that the link between thin ideal internalization and prior FNE was weaker at the 2-month follow-up than at other assessment points (DPT: b = 0.012, t = 2.670; p =.009; D6MF: b = 0.010, t = 2.214; p = .030; D12MF: b = 0.009, t = 2.177; p = .032). There was not a significant three-way FNE by BMI by 2-month assessment interaction (b = 0.001, t = 0.336, p = .737), indicating that the FNE-thin ideal internalization link was relatively weaker at the 2-month follow-up regardless of participants’ BMI.
Finally, FNE was predicted by prior levels of thin ideal internalization (b = 2.301, t = 2.775, p = .006). There were no differences in the strength of this relation over time (DPT: b = −1.030, t = −0.576; p = .565; D2MF: b = −1.813, t = −1.287; p = .199; D12MF: b = 0.112, t = 0.059; p = .953) or by BMI (b = 0.071, t = 0.196; p = .845). There was also not a main effect of BMI in this model (b = −0.028, t = −0.063, p = .950).
In sum, we found that higher levels of FNE were related to lower levels of subsequent thin ideal internalization among women with elevated BMIs. For women with low BMIs, there was a positive but nonsignificant relation between FNE and subsequent thin ideal internalization. In addition, elevations in thin ideal internalization predicted greater future FNE, thus indicating a reciprocal relation for those with elevated BMIs and a unidirectional relation for women with low BMIs.
Body dissatisfaction
FNE predicted subsequent body dissatisfaction (b = 0.012, t = 3.161, p = .002), and there were no significant FNE by assessment period interactions (DPT: b = 0.014, t = 1.635, p = .103; D2MF: b = 0.016, t = 1.957, p = .052; D12MF: b = 0.011, t = 1.351, p = .178), indicating no differences in the strength of this relation over time. There were also no differences in the strength of the relation between FNE and body dissatisfaction by BMI (b = 0.0004, t = 0.223, p = .816), but there was a main effect of baseline BMI in the prediction of body dissatisfaction throughout the intervention and follow-up periods (b = 0.103, t = 2.112, p = .036).
The relation between FNE and prior body dissatisfaction was significantly different at post-intervention relative to the 6-month and 12-month follow-ups (D6MF: b = 3.178, t = 3.228, p = .001; D12MF: b = 2.857, t = 2.302, p = .002), as well as at 2-month follow-up relative to all other assessment points (DPT: b = 2.421, t = 2.297, p = .023; D6MF: b = 3.568, t = 3.465, p = .001; D12MF: b = 3.217, t = 2.480, p = .014). The strength of the relation was stronger at the 6- and 12-month follow-up assessments than at the post-intervention and 2-month assessment. Body dissatisfaction significantly predicted later FNE at the 6- and 12-month follow-ups (D6MF: b = 1.440, t = 2.563, p = .011; D12MF: b = 1.583, t = 2.828, p = .005) but not at post-intervention and 2-month follow up (DPT: b = 0.179, t = 0.306, p = .760; D2MF: b = −0.338, t = 0.495, p = .621). There was not a significant BMI by body dissatisfaction interaction (b = −0.104, t = −0.057, p = .955) nor a significant main effect of BMI (b = −0.086, t = −0.195, p = .846).
In sum, FNE and body dissatisfaction were reciprocally and positivity related throughout the long-term maintenance period, but the association was unidirectional (i.e., FNE predicted subsequent body dissatisfaction) during the acute intervention phase and 2-month follow-up.
Dietary Restraint
FNE did not predict subsequent levels of dietary restraint (b = −0.002, t = −0.515, p = .607), and the strength of this relation did not vary over time (DPT: b = 0.012, t = 1.854, p = .065; D2MF: b = 0.007, t = 1.013, p = .3125; D12MF: b = 0.005, t = 0.635, p = .526). There was not a BMI by FNE interaction (b = −0.001, t = −0.890, p = .375), but baseline BMI significantly predicted dietary restraint throughout intervention and follow-up (b = 0.072, t = 2.014, p = .048).
Dietary restraint significantly predicted later FNE (b = 1.980, t = 2.994, p = .003). Dietary restraint did not interact with any assessment time periods (DPT: b = 0.200, t = 0.177, p = .860; D2MF: b = −1.199, t = −1.227, p = .860; D12MF: b = −0.457, t = −0.401, p = .689) or BMI (b = −0.171, t = −0.562, p = .575), and there was no main effect of BMI (b = 0.103, t = 0.029, p = .977).
In sum, there was a unidirectional and positive association between dietary restraint and FNE, such that frequent dieters, who also tended to have higher BMIs, were more likely to report higher subsequent FNE.
Negative affect
FNE did not predict subsequent negative affect (b = −0.005, t = −1.754, p = .080), and there were no significant FNE by time interactions (DPT: b = 0.112, t = 1.945, p = .053; D2MF: b = 0.011, t = 1.786, p = .076; D12MF: b = 0.004, t = 0.578, p = .564) nor an FNE by BMI interaction (b = −0.001, t = −0.440, p = .660). There was also not a main effect of BMI (b = 0.007, t = 0.369, p = .714).
We found a significant BMI by negative affect interaction in the prediction of future FNE (b = 1.186, t = 3.137, p = .002), and there were no differences in the strength of the relations over the assessment periods (DPT: b = 0.301, t = 0.203, p = .839; D2MF: b = −2.081, t = −1.243, p = .215; D12MF: b = −2.929, t = −1.587, p = .114). Greater levels of negative affect were associated with greater future FNE for women with elevated BMIs (b = 1.988, t = 2.086, p = .038), but greater levels of negative affect were associated with less FNE for women with low BMIs (b = −3.159, t = −2.291, p = .023).
In sum, we found a unidirectional relation between negative affect and subsequent FNE that varied by BMI.
Eating disorder symptoms
FNE predicted subsequent ED symptoms (b = 0.115, t = 2.553, p = .011). The strength of this relation did not vary over time (DPT: b = −0.066, t = −0.779, p = .437; D2MF: b = 0.023, t = 0.273, p = .785; D12MF: b = −0.012, t = −0.132, p = .895) or by BMI (b = 0.004, t = 0.213, p = .832). There was no BMI main effect (b = 0.419, t = 0.870, p = .388).
Neither ED symptoms (b = 0.082, t = 1.638, p = .102) nor BMI (b = −0.086, t = −0.195, p = .846) predicted later FNE. FNE did not interact with any of the assessment points (DPT: b = −0.024, t = −0.263, p = .793; D2MF: b = −0.125, t = −1.491, p = .138; D12MF: b = −0.097, t = −0.917, p = .360) or BMI (b = −0.103, t = −0.535, p = .593).
Discussion
Expanding on prior cross-sectional research, our results indicated that, when controlling for prior levels of each outcome, FNE was a determinant of future body dissatisfaction and ED symptoms among college women, as well as future thin ideal internalization, although this latter relation was only evident among those with elevated BMIs. We also found that FNE was predicted by earlier levels of thin ideal internalization, body dissatisfaction (only at the 6- and 12-month follow-up assessments), dietary restraint, and negative affect. Interestingly, women high in negative affect were more likely to have greater future FNE if they had high BMIs but more likely to have lower future FNE if they had low BMIs. Thus, FNE was reciprocally related to thin ideal internalization for women with relatively high BMIs and to body dissatisfaction at the more distal follow-up assessments. FNE, however, did not predict subsequent dietary restraint or negative affect in this sample, suggesting unidirectional relations with changes in dietary restraint and negative affect contributing to later changes in FNE. Overall, these results confirm that FNE is related to the majority of risk factors in the dual-pathway model. FNE served as a predictor of subsequent thin ideal internalization, body dissatisfaction, and ED symptoms while itself being predicted by thin ideal internalization, body dissatisfaction, dietary restraint, and negative affect.
Our examination of the longitudinal relations between FNE and negative affect yielded two surprising findings. First, we found no significant main effect over time in either direction, nor did we find improvement in negative affect over the course of intervention and follow-up. This finding is inconsistent with studies demonstrating positive associations between FNE and negative affect (e.g., Weeks & Howell, 2012; Utschig et al., 2010) and reductions in negative affect across dissonance-based ED prevention programs (Becker, McDaniel, Bull, Powell, & McIntyre, 2012; Stice et al., 2001; 2000; 2006; 2008; 2002). A floor effect for negative affect may have accounted for these discrepant findings. Scores on the PANAS-X typically range from about 2.10 to 2.22 (SD = 0.69 to 0.98) in trials of dissonance prevention programs (e.g., McMillan, Stice, & Rohde, 2011; Stice, Mazotti, Weibel, & Agras, 2000; Stice, Presnell, Gau, & Shaw, 2007; Stice et al., 2008), whereas the mean score at baseline for the current sample was 1.52 (SD = 0.57). The relatively low level of negative affect experienced by the participants at baseline may have left little room for improvement across the intervention, and the restricted range may have precluded significant associations with other variables.
Second, we observed that a significant interaction with BMI accounted for the lack of a main effect of negative affect on subsequent FNE. Interestingly, the relation was significantly positive for women with BMIs elevated for this sample (i.e., 23.85; 1 SD above the mean) and significantly negative for women with relatively low BMIs (i.e., 19.55; 1 SD above the mean). This interaction is particularly interesting, given that an opposite association between affect and FNE appeared among women within such a small and healthy BMI range. Prior work has shown that currently or previously depressed individuals and those with poorer self esteem and body image are more likely to engage in and have greater negative affective responses to upward social appearance comparison (Bäzner, Brömer, Hammelstein, & Meyer, 2006; Patrick, Neighbors, & Knee, 2004). It seems plausible that body image and social appearance comparison may mediate the link between negative affect and FNE (and more specifically fear of negative appearance evaluation) among women with an elevated BMI relative to their close peer group. On the other hand, women high in negative affect but who are relatively thin may be less likely to fear others’ evaluations, particularly as they relate to physical appearance. This discrepancy may be especially likely in the context of social groups that value thinness, such as some sororities (Cashel, Cunningham, Landeros, Cokley, & Muhammad, 2003).
We found that thin ideal internalization was associated with elevated FNE at subsequent assessments. This finding seems logical given that a strong adoption of group norms would likely lead to concern or preoccupation with being evaluated based on those norms. More surprising was that, for women with elevated BMIs only, greater FNE predicted lower levels of future thin ideal internalization. Social psychology theories of ego-defensiveness and the human drive to maintain cognitive consistency may help to explain this finding. Prior work has shown that individuals often discount information, attitudes, and values that threaten their self-concept (Gawronski, 2012; Lapinski & Boster, 2003). In order for a societal value, such as the thin ideal of feminine beauty, to be threatening, the value must be both counter-attitudinal and central to one’s self-concept (Gawronski, 2012; Lapinski & Boster, 2003). This could explain the current finding if: (1) participants with elevated BMIs held overall positive beliefs about themselves (i.e., valuing the thin ideal would be counter-attitudinal), and (2) their body weight or shape was central to their self-concept, which is highly typical among college-age women (Fitzsimmons-Craft, 2011) and may be more likely among those who are particularly concerned about “fitting in” and others’ evaluations (i.e., those high in FNE). Based on these theories, however, one would expect the opposite relation, that is, that elevated FNE would be associated with greater internalization of the thin ideal, for women with elevated BMIs and poor overall self-esteem. Future work should seek to determine whether global self-esteem moderates the relation between FNE and subsequent thin ideal internalization among college women with elevated BMIs.
Utschig and colleagues (2010) concluded that the significant direct paths between FNE and pressure to be thin and thin ideal internalization, respectively, suggested that FNE influences eating pathology early in the causal chain. However, they did not examine these relations longitudinally, and the results of the present study suggest a more robust effect in the opposite direction, namely, the degree of thin ideal internalization at a given time point may influence future FNE for participants regardless of their BMI. However, the directionality of associations between variables may be different in the context of symptom development versus symptom amelioration. Specifically, whereas FNE may put women at risk for succumbing to sociocultural pressures by internalizing the thin ideal and, in turn, becoming dissatisfied with their bodies (Utschig et al., 2010), directly intervening with thin ideal internalization in the context of a prevention program may decrease fears of being negatively evaluated based on body shape or weight, either directly or indirectly through decreases in body dissatisfaction, as our findings may suggest. Indeed, thin ideal internalization is the primary point of intervention in dissonance programs, and it is therefore likely to be among the first risk factors to change. Interpreted in the context of the dual-pathway model and the theoretical basis of dissonance interventions, our results are consistent with an initial shift in thin ideal internalization, which promoted subsequent decreases in dietary restraint, body dissatisfaction, and FNE.
Decreases in body dissatisfaction and dietary restraint also contributed to decreases in FNE in our study. In addition to a likely direct influence of body dissatisfaction and dietary restraint on ED symptoms (which was not tested in this study but is supported by theory and prior empirical work), decreases in FNE also directly contributed to future decreases in ED symptoms, as well as subsequent body dissatisfaction. Figure 1 illustrates a hypothesized model of changes occurring in the context of a dissonance-based prevention program for women regardless of their BMI, with pathways supported by the current finding bolded and pathways supported by theory and empirical data on the dual-pathway model and dissonance-based interventions dashed.
Our findings provide evidence that changes in FNE may impact subsequent changes in thin ideal internalization, body dissatisfaction, and ED symptoms. These findings, along with evidence that social anxiety develops prior eating pathology (Brewerton, Lydiard, Herzog, & Brotman, 1995; Bulik et al., 1997), provide support for directly targeting FNE in prevention programs. Incorporating cognitive restructuring and exposure exercises, commonly used in cognitive behavioral interventions for social anxiety, is one way to do this. Furthermore, given its associations with numerous ED risk factors as well as its independent association with bulimia nervosa (Utschig et al., 2010), it may be prudent to screen individuals with social anxiety or high FNE for eating pathology.
Another interesting finding is that, depending on the outcome variable, the relation between FNE and ED risk factors or symptoms may vary over time. Specifically, we found that prior FNE predicted body dissatisfaction only at the 6-month and 12-month follow-up assessments and that the relation between FNE and thin ideal internalization from post-intervention to 2-month follow-up was weaker, although still significant, than at the other time intervals. These findings may suggest that the relation between FNE and ED risk factors are different during the course of treatment (i.e., reflecting intervention effects) than during the naturalistic follow-up period (i.e., reflecting maintenance effects or continued improvement). Alternatively, the moderator effect of assessment phase observed in this study may be best explained by the unequal time intervals between assessments, with longer intervals during the naturalistic follow-up relative to the intervention phase. Indeed, longer lags are typically associated with weaker relations (Olatunji et al., 2013).
Although this study has several strengths, including a longitudinal design and the use of cross-lagged panel analyses, several limitations deserve mention. First, given that six (7.4%) participants met full diagnostic criteria for an ED and another eight (9.8%) met criteria for a subthreshold ED, our study did not examine the interplay of FNE and ED variables in a purely prevention context (i.e., among those at risk for, but not currently experiencing, an eating disorder). It is possible that FNE and ED outcomes are associated in different ways or respond differently to intervention for college women with and without EDs. The generalizability of our findings is therefore less clear, and it is possible that the strength of relations among variables may have been either underestimated or inflated due to the inclusion of women with actual EDs.
Another limitation is the use of a predominantly Caucasian college sorority sample, which further limits generalizability. Given the social nature of college sororities, sorority women may seem likely to have lower levels of FNE and other social anxiety-related concerns. However, baseline BFNE-R scores (M = 34.63, SD = 9.92) were comparable to other undergraduate samples (M = 32.8, SD = 10.04; Carleton et al., 2006) and there is currently no evidence that rates of social anxiety differ between sorority and non-sorority members. Still, sorority women may differ from non-sorority college women in other ways that confer greater risk for eating pathology. For example, those with high evaluative concerns may be at increased risk for succumbing to sociocultural pressures to be thin, possibly due to pressure to conform to a certain sorority identity and more frequent opportunities for physical appearance comparison. Extant work suggests that, relative to other college women, sorority members may be more likely to conform to social norms related to subscription to the thin ideal of feminine beauty (Basow, Foran, & Bookwala, 2007; Cashel et al., 2003), eating behavior (Basow et al., 2007; Crandall, 1988), alcohol consumption (Larimer, Turner, Mallet, & Geisner, 2004; Neighbors, Lee, Lewis, Fossos, & Larimer, 2007), and other health risk behaviors (Scott-Sheldon, Carey, & Carey, 2008). These potential differences would suggest that this group is even more at risk than college women in general.
Despite these limitations, the present study is the first to provide evidence for causal relations between FNE and various ED risk factors. Specifically, FNE served as a predictor of subsequent thin ideal internalization among women with elevated BMI for the sample, body dissatisfaction during the follow-up phase, and ED symptoms regardless of assessment interval. FNE was itself predicted by thin ideal internalization, body dissatisfaction, dietary restraint, and negative affect (positively for high-BMI and negatively for low-BMI participants). By demonstrating directionality, our findings suggest that FNE may play a significant role in the amelioration (and potentially prevention) of eating pathology. Future longitudinal research should (1) examine the impact of FNE on the development and maintenance of ED risk factors and symptoms, (2) compare the interplay of these symptoms for women who do and do not go on to develop full threshold EDs, and (3) examine differences in the role of FNE in the trajectories for different ED diagnoses, as FNE may operate differently in anorexia nervosa, bulimia nervosa, and binge eating disorder. In addition, other features and correlates of social anxiety such as sociotropy (Duemm et al., 2003), social appearance anxiety (Levinson & Rodebaugh, 2012), social appearance comparison (Bazner et al., 2006; Patrick et al., 2004), and body dysmorphic concerns (Fang & Hofmann, 2010; Schneider, Blanco, Antia, & Leibowitz, 2002) have been independently related to ED risk factors, and future work should examine the impact of FNE alongside these variables. Such research will further our understanding of anxiety-eating disorder comorbidity and facilitate the development of a more comprehensive model of ED development, prevention, and intervention.
References
- Basow SA, Foran KA, Bookwala J. Body objectification, social pressure, and disordered eating behavior in college women: The role of sorority membership. Psychology of Women Quarterly. 2007;31(4):394–400. [Google Scholar]
- Bäzner E, Brömer P, Hammelstein P, Meyer TD. Current and former depression and their relationship to the effects of social comparison processes: Results of an internet based study. Journal of Affective Disorders. 2006;93:97–103. doi: 10.1016/j.jad.2006.02.017. [DOI] [PubMed] [Google Scholar]
- Becker CB, Bull S, Schaumberg K, Cauble A, Franco A. Effectiveness of peer-facilitated eating disorders prevention: A randomized replication trial. Journal of Consulting and Clinical Psychology. 2008;76:437–454. doi: 10.1037/0022-006X.76.2.347. [DOI] [PubMed] [Google Scholar]
- Becker CB, McDaniel L, Bull S, Powell M, McIntyre K. Can we reduce eating disorder risk factors in female college athletes? A randomized exploratory investigation of two peer-led interventions. Body Image. 2012;9:31–42. doi: 10.1016/j.bodyim.2011.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker CB, Smith LM, Ciao AC. Peer-facilitated eating disorder prevention: A randomized effectiveness trial of cognitive disonance and media advocacy. Journal of Counseling Psychology. 2006;53:550–555. [Google Scholar]
- Becker CB, Smith LM, Ciao AC. Reducing eating disorder risk factors in sorority members: A randomized trial. Behavior Therapy. 2005;36:245–254. [Google Scholar]
- Berscheid E, Walster E, Bohrnstedt G. The happy American body: A survey report. Psychology Today. 1973;7:119–131. [Google Scholar]
- Brewerton TD, Lydiard RB, Herzog DB, Brotman AW. Comorbidity of Axis I psychiatric disorders in bulimia nervosa. Journal of Clinical Psychiatry. 1995;56:77–80. [PubMed] [Google Scholar]
- Brewerton TD, Stellefson EJ, Hibbs N, Hodges EL, Cochrane CE. Comparison of eating disorder patients with and without compulsive exercising. International Journal of Eating Disorders. 1995;17:413–416. doi: 10.1002/1098-108x(199505)17:4<413::aid-eat2260170414>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Sullivan PF, Fear JL, Joyce PR. Eating disorders and antecedent anxiety disorders: A controlled study. Acta Psychiatrica Scandinavica. 1997;96:101–107. doi: 10.1111/j.1600-0447.1997.tb09913.x. [DOI] [PubMed] [Google Scholar]
- Carleton RN, Collimore KC, McCabe RE, Antony MM. Addressing revisions to the Brief Fear of Negative Evaluation scale: Measuring fear of negative evaluation across anxiety and mood disorders. Journal of Anxiety Disorders. 2011;25:822–828. doi: 10.1016/j.janxdis.2011.04.002. [DOI] [PubMed] [Google Scholar]
- Carleton RN, McCreary DR, Norton PJ, Asmundson GJG. Brief Fear of Negative Evaluation scale--revised. Depression & Anxiety. 2006;23:1091–4269. doi: 10.1002/da.20142. [DOI] [PubMed] [Google Scholar]
- Cashel ML, Cunningham D, Landeros C, Cokley KO, Muhammad G. Sociocultural attitudes and symptoms of bulimia: Evaluating the SATAQ with diverse college groups. Journal of Counseling Psychology. 2003;50:287–296. [Google Scholar]
- Crandall CS. Social contagion of binge eating. Journal of Personality and Social Psychology. 1988;55:588–598. doi: 10.1037//0022-3514.55.4.588. [DOI] [PubMed] [Google Scholar]
- Duemm I, Adams GR, Keating L. The addition of sociotropy to the dual pathway model of bulimia. Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement. 2003;35:281–291. [Google Scholar]
- Fairburn CG, Beglin SJ. Studies of the epidemiology of bulimia nervosa. American Journal of Psychiatry. 1990;147:401–408. doi: 10.1176/ajp.147.4.401. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Harrison PJ. Eating disorders. Lancet. 2003;361:407–416. doi: 10.1016/S0140-6736(03)12378-1. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, Sharfran R, Wilson GT. Clinical handbook of psychological disorders: A step-by-step treatment manual. 4. New York: Guilford Press; 2008. Eating disorders: A transdiagnostic protocol. [Google Scholar]
- Fang A, Hofmann SG. Relationship between social anxiety disorder and body dysmorphic disorder. Clinical Psychology Review. 2010;30:1040–1048. doi: 10.1016/j.cpr.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzsimmons-Craft EE. Social psychological theories of disordered eating in college women: Review and integration. Clinical Psychology Review. 2011;31:1224–1237. doi: 10.1016/j.cpr.2011.07.011. [DOI] [PubMed] [Google Scholar]
- Gawronski B. Back to the future of dissonance theory: Cognitive consistency as a core motive. Social Cognition. 2012;30:652–668. [Google Scholar]
- Gilbert N, Meyer C. Social anxiety and social comparison: Differential links with restrictive and bulimic attitudes among nonclinical women. Eating Behaviors. 2003;4:257–264. doi: 10.1016/S1471-0153(03)00026-6. [DOI] [PubMed] [Google Scholar]
- Hamer RM, Simpson PM. Last observation carried forward versus mixed models in the analysis of longitudinal psychiatric clinical trials. American Journal of Psychiatry. 2009;166:639–641. doi: 10.1176/appi.ajp.2009.09040458. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Nichols P, Mahmedi F, Keel P. Body weight, dieting, and eating disorder symptoms among college students, 1982 to 1992. The American Journal of Psychiatry. 1995;152:1623–1629. doi: 10.1176/ajp.152.11.1623. [DOI] [PubMed] [Google Scholar]
- Heimberg RC, Brozovich FA, Rapee RM. A cognitive behavioral model of social anxiety disorder: Update and extension. In: Hofmann SG, DiBartolo PM, editors. Social anxiety: Clinical, developmental, and social perspectives. 2. San Diego, CA US: Elsevier Academic Press; 2010. pp. 395–422. [DOI] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the national comorbidity survey replication. Biological Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keel PK, Heatherton TF, Dorer DJ, Joiner TE, Zalta AK. Point prevalence of bulimia nervosa in 1982, 1992, and 2002. Psychological Medicine. 2006;36:119–127. doi: 10.1017/S0033291705006148. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Greenberg DF. Linear panel analysis: Models of quantitative change. New York: Academic Press; 1981. [Google Scholar]
- Kilpela LS, DeBoer LB, West J, Alley MC, Presnell KE, Becker CB. Distributed and condensed versions of an eating disorder prevention program: Effects on eating disorder symptoms and risk factors. (in preparation) [Google Scholar]
- Laessle RG, Tuschl RJ, Kotthaus BC, Pirke KM. Behavioral and biological correlates of dietary restraint in normal life. Appetite. 1989;12:83–94. doi: 10.1016/0195-6663(89)90098-6. [DOI] [PubMed] [Google Scholar]
- Lapinkski MK, Boster FJ. Modeling the ego-defensive function of attitudes. Communication Monographs. 2001;68:314–324. [Google Scholar]
- Larimer ME, Turner AP, Mallet KA, Geisner IM. Predicting drinking behavior and alcohol-related problems among fraternity and sorority members: Examining the role of descriptive and injunctive norms. Psychology of Addictive Behaviors. 2004;18:203–214. doi: 10.1037/0893-164X.18.3.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leary MR. A brief version of the Fear of Negative Evaluation Scale. Personality and Social Psychology Bulletin. 1983;9:371–375. [Google Scholar]
- Levinson CA, Rodebaugh TL. Validation of the Social Appearance Anxiety Scale: Factor, convergent, and diverent validity. Assessment. 2011;18:350–356. doi: 10.1177/1073191111404808. [DOI] [PubMed] [Google Scholar]
- Levinson CA, Rodebaugh TL. Social anxiety and eating disorder comorbidity: The role of negative social evaluation fears. Eating Behaviors. 2012;13:27–35. doi: 10.1016/j.eatbeh.2011.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Streigel-Moore RH, Seeley JR. Epidemiology and natural course of eating disorders in young women from adolescence to young adulthood. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:1284–1292. doi: 10.1097/00004583-200010000-00016. [DOI] [PubMed] [Google Scholar]
- McMillan W, Stice E, Rohde P. High- and low-level dissonance-based eating disorder prevention programs with young women with body image concerns: An experimental trial. Journal of Consulting and Clinical Psychology. 2011;79:129–134. doi: 10.1037/a0022143. [DOI] [PubMed] [Google Scholar]
- Menard S. Longitudinal research. Thousand Oaks, CA US: Sage Publications, Inc; 1991. [Google Scholar]
- Miller RS. On the nature of embarrassability: Shyness, social evaluation, and social skill. Journal of Personality. 1995;63:315–339. doi: 10.1111/j.1467-6494.1995.tb00812.x. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Lee CM, Lewis MA, Fossos N, Larimer ME. Are social norms the best predictor of outcomes among heavy-drinking college students? Journal of Studies on Alcohol and Drugs. 2007;68:556–565. doi: 10.15288/jsad.2007.68.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olatunji BO, Rosenfield D, Tart CD, Cottraux J, Powers MB, Smits JAJ. Behavioral versus cognitive treatment of obsessive-compulsive disorder: An examination of outcome and mediators of change. Journal of Consulting & Clinical Psychology. doi: 10.1037/a0031865. (in press) [DOI] [PubMed] [Google Scholar]
- Patrick H, Neighbors C, Knee CR. Appearance-related social comparisons: The role of contingent self-esteem and self-perceptions of attractiveness. Personality and Social Psychology Bulletin. 2004;30:501–514. doi: 10.1177/0146167203261891. [DOI] [PubMed] [Google Scholar]
- Petry NM, Barry D, Pietrzak RH, Wagner JA. Overweight and obesity are associated with psychiatric disorders: Results from the National Epidemiological Survey on Alcohol and Related Conditions. Psychosomatic Medicine. 2008;70:288–297. doi: 10.1097/PSY.0b013e3181651651. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Heimberg RG. A cognitive-behavioral model of anxiety in social phobia. Behaviour Research and Therapy. 1997;35:741–756. doi: 10.1016/s0005-7967(97)00022-3. [DOI] [PubMed] [Google Scholar]
- Ross SE, Neibling BC, Heckert TM. Sources of stress among college students. College Student Journal. 1999;33:312–317. [Google Scholar]
- Schneider FR, Blanco C, Antia SX, Liebowitz MR. The social anxiety spectrum. Psychiatric Clinics of North America. 2002;25:757–774. doi: 10.1016/s0193-953x(02)00018-7. [DOI] [PubMed] [Google Scholar]
- Scott-Sheldon LAJ, Carey KB, Carey MP. Health behavior and college students: Does Greek affiliation matter? Journal of Behavioral Medicine. 2008;31:61–70. doi: 10.1007/s10865-007-9136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepherd H, Ricciardelli LA. Test of Stice’s dual pathway model: Dietary restraint and negative affect as mediators of bulimic behavior. Behaviour Research and Therapy. 1998;36:345–352. doi: 10.1016/s0005-7967(98)00033-3. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Julian K, Rosenfield D, Powers MB. Threat reappraisal as a mediator of symptom change in cognitive-behavioral treatment of anxiety disorders: a systematic review. Journal of Consulting and Clinical Psychology. 2012;80:624–635. doi: 10.1037/a0028957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smits JAJ, Rosenfield D, McDonald R, Telch MJ. Cognitive mechanisms of social anxiety reduction: An examination of specificity and temporality. Journal of Consulting and Clinical Psychology. 2006;74:1203–1212. doi: 10.1037/0022-006X.74.6.1203. [DOI] [PubMed] [Google Scholar]
- Stice E, Agras WS. Predicting onset and cessation of bulimic behaviors during adolescence: A longitudinal grouping analysis. Behavior Therapy. 1998;29:257–276. [Google Scholar]
- Stice E. A prospective test of the dual pathway model of bulimic pathology: Mediating effects of dieting and negative affect. Journal of Abnormal Psychology. 2001;110:124–135. doi: 10.1037//0021-843x.110.1.124. [DOI] [PubMed] [Google Scholar]
- Stice E, Chase A, Stormer S, Appel A. A randomized trial of a dissonance-based eating disorder prevention program. International Journal of Eating Disorders. 2001;29:247–262. doi: 10.1002/eat.1016. [DOI] [PubMed] [Google Scholar]
- Stice E, Fisher M, Martinex E. Eating Disorder Diagnostic Scale: Additional evidence of reliability and validity. Psychological Assessment. 2004;16:60–71. doi: 10.1037/1040-3590.16.1.60. [DOI] [PubMed] [Google Scholar]
- Stice E, Marti CN, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: Long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008;76:329–340. doi: 10.1037/0022-006X.76.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Mazotti L, Weibel D, Agras WS. Dissonance prevention program deceases thin-ideal internalization, body dissatisfaction, dieting, negative affect, and bulimic symptoms: A preliminary experiment. International Journal of Eating Disorders. 2000;27:206–217. doi: 10.1002/(sici)1098-108x(200003)27:2<206::aid-eat9>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Stice E, Presnell K, Gau J, Shaw H. Testing mediators of intervention effects in randomized controlled trials: An evaluation of two eating disorder prevention programs. Journal of Consulting and Clinical Psychology. 2007;75:20–32. doi: 10.1037/0022-006X.75.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Marti CN. A meta-analytic review of eating disorder prevention programs: Encouraging findings. Annual Review of Clinical Psychology. 2007;3:207–231. doi: 10.1146/annurev.clinpsy.3.022806.091447.OR Stice E, Shaw H, Marti CN. A meta-analytic review of eating disorder prevention programs: Progress at last. Annual Review of Clinical Psychology. 2007;3:233–257. doi: 10.1146/annurev.clinpsy.3.022806.091447.
- Stice E, Shaw H, Nemeroff C. Dual pathway model of bulimia nervosa: Longitudinal support for dietary restraint and affect-regulation mechanisms. Journal of Social and Clinical Psychology. 1998;17:129–149. [Google Scholar]
- Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: A randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2006;74:263–275. doi: 10.1037/0022-006X.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, South K, Shaw H. Future directions in etiologic, prevention, and treatment research for eating disorders. Journal of Clinical Child and Adolescent Psychology. 2012;41:845–855. doi: 10.1080/15374416.2012.728156. [DOI] [PubMed] [Google Scholar]
- Stice E, Telch CF, Rizvi SL. Development and validation of the Eating Disorder Diagnostic Scale: A brief self-report measure for anorexia, bulimia, and binge eating disorder. Psychological Assessment. 2000;12:123–131. doi: 10.1037//1040-3590.12.2.123. [DOI] [PubMed] [Google Scholar]
- Stice E, Trost A, Chase A. Healthy weight control and dissonance-based eating disorder prevention programs: results form a controlled trial. International Journal of Eating Disorders. 2003;33:10–21. doi: 10.1002/eat.10109. [DOI] [PubMed] [Google Scholar]
- Stice E, Ziemba C, Margolis J, Flick P. The dual pathway model differentiates bulimics, subclinical bulimics, and controls: Testing the continuity hypothesis. Behavior Therapy. 1996;27:531–549. [Google Scholar]
- Stopa L, Clark DM. Cognitive processes in social phobia. Behaviour Research and Therapy. 1993;31:255–267. doi: 10.1016/0005-7967(93)90024-o. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Silberstein LR, Grunberg NE, Rodin J. Competing on all fronts: Achievement orientation and disordered eating. Sex Roles. 1990;23(11–12):697–702. [Google Scholar]
- Sullivan PF. Mortality in anorexia nervosa. The American Journal of Psychiatry. 1995;152:1073–1074. doi: 10.1176/ajp.152.7.1073. [DOI] [PubMed] [Google Scholar]
- Swinbourne J, Hunt C, Abbott M, Russell J, St Clare T, Touyz S. The comorbidity between eating disorders and anxiety disorders: Prevalence in an eating disorder sample and anxiety disorder sample. Australian and New Zealand Journal of Psychiatry. 2012;46:118–131. doi: 10.1177/0004867411432071. [DOI] [PubMed] [Google Scholar]
- Tschacher W, Ramseyer F. Modeling psychotherapy process by time-series panel analysis (TSPA) Psychotherapy Research Methods. 2009;19:469–481. doi: 10.1080/10503300802654496. [DOI] [PubMed] [Google Scholar]
- Treasure J, Szmukler GI. Medical complications of chronic anorexia nervosa. In: Szmukler GI, Dare C, Treasure J, editors. Handbook of eating disorders: Theory, treatment and research. Oxford England: John Wiley & Sons; 1995. pp. 197–220. [Google Scholar]
- Utschig AC, Presnell K, Madeley MC, Smits JAJ. An investigation of the relationship between fear of negative evaluation and bulimic psychopathology. Eating Behaviors. 2010;11:231–238. doi: 10.1016/j.eatbeh.2010.05.003. [DOI] [PubMed] [Google Scholar]
- van Strien T, Frijters JER, Bergers GPA, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. International Journal of Eating Disorders. 1986;5:295–315. [Google Scholar]
- van Strien T, Frijters JE, Van Staveren WA, Defares PB, Deurenberg P. The predictive validity of the Dutch Restrained Eating Scale. International Journal of Eating Disorders. 1986;5:747–755. [Google Scholar]
- Vassilopoulos S. Interpretation and judgment biases in socially anxious and nonanxious individuals. Behavioural and Cognitive Psychotherapy. 2006;34:243–254. doi: 10.1017/S1352465809005189. [DOI] [PubMed] [Google Scholar]
- Wardle J, Beales S. Restraint and food intake: An experimental study of eating patterns in the laboratory and in normal life. Behavior Research and Therapy. 1987;25:179–185. doi: 10.1016/0005-7967(87)90044-1. [DOI] [PubMed] [Google Scholar]
- Wardle J. Eating style: A validation study of the Dutch eating behavioral questionnaire in normal subjects and women with eating disorders. Journal of Psychosomatic Research. 1987;31:161–169. doi: 10.1016/0022-3999(87)90072-9. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Affects separable and inseparable: On the hierarchical arrangment of the negative affects. Journal of Personality and Social Psychology. 1992;62:489–505. [Google Scholar]
- Watson D, Clark LA. The PANAS-X. Manual for the positive and negative affect schedule – expanded form. 1999 Retrieved from University of Iowa, Department of Psychology Web site: www.psychology.uiowa.edu/faculty/Clark/PANAS-X.pdf.
- Weeks JW, Howell AN. The bivalent fear of evaluation model of social anxiety: Further integrating finding on fears of positive and negative evaluation. Cognitive Behaviour Therapy. 2012;41:83–95. doi: 10.1080/16506073.2012.661452. [DOI] [PubMed] [Google Scholar]
- Westerberg-Jacobson J, Edlund B, Ghaderi A. Risk and protective factors for disturbed eating: A 7-year longitudinal study of eating attitudes and psychological factors in adolescent girls and their parents. Eating and Weight Disorders. 2010;15:208–218. doi: 10.1007/BF03325302. [DOI] [PubMed] [Google Scholar]
- Wilson GT, Becker CB, Heffernan K. Eating disorders. In: Mash EJ, Barkley RA, editors. Child psychopathology. 2. New York: Guilford Press; 2003. pp. 687–715. [Google Scholar]
- Wonderlich-Tierney AL, Vander Wal JS. The effects of social support and coping on the relationship between social anxiety and eating disorders. Eating Behaviors. 2010;11:85–91. doi: 10.1016/j.eatbeh.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Zivin K, Eisenberg D, Gollust SE, Golberstein E. Persistence of mental health problems and needs in a college student population. Journal of Affective Disorders. 2009;117:180–185. doi: 10.1016/j.jad.2009.01.001. [DOI] [PubMed] [Google Scholar]


