Abstract
Background:
Tako-Tsubo syndrome (TS) is a still rarely diagnosed clinical syndrome, which is characterized by acute onset of chest pain, transient cardiac dysfunction with (frequently) reversible wall motion abnormalities (WMAs), but with no relevant obstructive coronary artery disease.
Methods and results:
Among 179 consecutive patients with proven diagnosis of TS that were retrospectively analysed in this multicentre registry, women represented the majority of patients (94%) while only 11 men (6%) developed TS. Mean age was 69.1±11.5 years (range 35–88 years). Cardinal symptoms of TS, which led to admission, were acute chest pain (82%) and dyspnoea (32%), respectively. All patients demonstrated typical WMAs, whereby four different types of WMAs could be defined: (1) a more common apical type of TS (n=89; 50%); (2) a combined apical and midventricular form of TS (n=23; 13%); (3) the midventricular TS (n=6; 3%); and (4) an unusual type of basal WMAs of the left ventricle (n=3). Only in 101 patients (57%), a clear causative trigger for onset of symptoms could be identified. In-hospital cardiovascular complications occurred in 25 patients (14%) and consisted of cardiac arrhythmias in 10 patients (40%), cardiogenic shock in six patients (24%), cardiac decompensation in eight patients (32%) and cardiovascular death in one patient, respectively. Echocardiographic control of left ventricular function after the initial measurement was available in almost 70% of the patients: complete recovery of WMAs was found in 73 patients (58.87%); 49 patients (39.52%) showed persistent WMAs. Recurrences of TS were only seen in four patients. During the follow-up period, 13 patients died: three of cardiovascular causes and 10 of non-cardiac causes. In-hospital mortality was 0.6%, 30-day mortality was 1.3% and 2-year mortality was 6.7%.
Conclusions:
This study represents to date the largest series of patients suffering from TS in Austria and worldwide. Similar to others, in our series the prevalence of TS was significantly higher in women than in men, while in contrast to other studies, the apical type of TS was detected most frequently. The similar clinical presentation of TS patients to the clinical picture of acute myocardial infarction demonstrates the importance of immediate coronary angiography for adequate differential diagnosis of TS. TS is not necessarily a benign disease due to cardiovascular complications as well as persistent WMAs with delayed recovery.
Keywords: Acute coronary syndrome, complications, Tako-Tsubo syndrome, triggering factors, wall motion abnormalities
Introduction
Tako-Tsubo syndrome (TS), also known as stress-induced cardiomyopathy, apical ballooning syndrome, or ‘broken-heart’ syndrome, is defined by acute onset of chest pain or dyspnoea, transient mainly left ventricular wall motion abnormalities (WMAs) not attributable to a single coronary artery territory with cardiac dysfunction, as well as electrocardiographic (ECG) changes and elevation of myocardial enzymes mimicking acute myocardial infarction (MI), in the absence of obstructive epicardial artery disease. Due to the fact that TS has a similar pattern of clinical presentation as acute MI, it is often misdiagnosed as acute coronary syndrome (ACS). Studies report prevalence from 0.9 to 2.0%1 of patients with TS among a population of patients with ACS, in whom the TS affects mostly elderly post-menopausal women after an acute emotional or physical stress event. The overall frequency of TS in the USA is reported as 0.02%% of all hospitalizations. In addition, a seasonal variation in admission can be seen.2,3–6
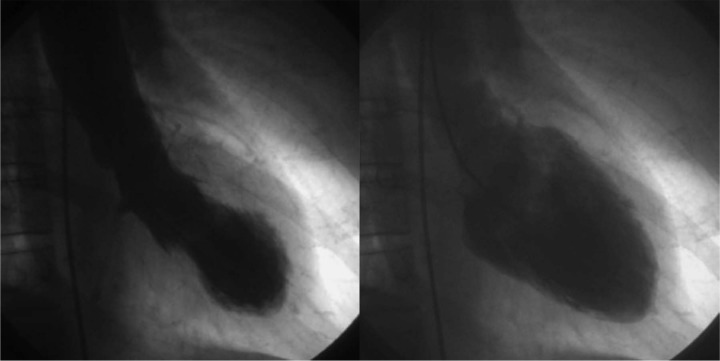
TS was first described by Satoh et al.7 and Dote et al.8 and named after the ‘takotsubo’, a bottle with a round bottom and narrow neck used for trapping octopus, due to a similar-looking typical wall motion abnormality (Figure 1). Beside the apical type of TS showing apical ballooning with a hypercontractile base of the left ventricle, there are furthermore three different types of TS recognized: a midventricular type of the TS, a type of TS affecting the apical as well as the midventricular segments of the left ventricle, and a recently described form of an inverted type of the TS involving the basal left-ventricular structures.1,3,9–12
Figure 1.
Evaluation of typical WMAs in levocardiography showing the typical type of an apical TS.
There is still a lack of data from large, multicentre studies, therefore, we collected data from patients from centres with interventional facilities to define more completely the clinical presentation, underlying stress events and different types of WMAs, as well as long-term prognosis of this syndrome.
Materials and methods
The local ethic committee of the Medical University of Vienna approved the study protocol. The study was conducted according to the principles expressed in the Declaration of Helsinki.
Inclusion criteria
A total of 179 patients with TS were retrospectively defined by the participating 11 centres and enrolled in the registry. Patients were diagnosed having TS by the participating centres and selected for analysis based on the following inclusion criteria: hospital admission with symptoms characteristic for acute MI accompanied by new electrocardiography (ECG) changes consistent with acute myocardial ischaemia, transient left ventricular WMAs in a multivessel distribution, and exclusion of a ≥50% stenosis of epicardial coronary arteries.
Patients who were suspected to have another disease as TS, such as acute MI with occluded or significantly narrowed epicardial arteries, myocarditis, pheochromocytoma, obstructive epicardial coronary artery disease, hypertrophic cardiomyopathy, as well as recent significant brain trauma or intracranial bleeding, were excluded from this study.
Patient population
Demographic and clinical parameters
Clinical characteristics such as gender, age, clinical presentation, coronary risk factors, and potential triggering factors were evaluated. Comorbidities and current medications were analysed.
12-lead ECG
12-lead ECG findings were examined in each centre; the first available ECG findings after symptom onset were analysed. Changes in ST-segment, T-wave, and Q-wave were evaluated and reported.
Cardiac angiography and levocardiography
All patients underwent coronary angiography or coronary computed tomography for evaluation of epicardial coronary arteries. Significant coronary artery disease was defined as ≥50% stenosis of a major epicardial coronary artery or major branch vessel. Levocardiography was performed in all patients in whom an echocardiographic determination of WMAs was not performed with excellent quality (25.14%).
Transthoracic echocardiography
Transthoracic echocardiography was performed in 135 patients (75%) in the acute phase of TS or within 4 days during hospitalization. Left ventricular ejection fraction (EF) was analysed either numerical or as definition of reduction (normal, mildly, moderately, severely reduced). WMAs were described as akinesia, hypokinesia, and dyskinesia, and the wall motion score index was reported. For determination of the WMAs as a key factor for diagnosis of TS, the left ventricle was divided into 16 segments according to the recommendation of the American Society of Echocardiography.13 Forty-four patients (25%) underwent a levocardiography or cardiovascular magnetic resonance imaging (cMRI) for examination of wall motion abnormalities due to low quality of the echocardiogram.
In-hospital complications and clinical outcome
Data on complications and mortality were collected by reviewing the patient’s individual medical records and by contacting the Austrian registry of deaths.
Clinical follow up
Data were collected through detailed review of all available medical records. Echocardiographic control of left ventricular function after the initial measurement was available in almost 70% (n=124) of the patients: 46 patients (26%) underwent repeat echocardiography prior to discharge within 7.24±4.83 days and 78 patients (44%) had an examination of regional WMAs within 186.36±316.67 days after the initial diagnosis. Data of survival was available of 150 patients (84%) after discharge within 6 and 88 months; data of the remaining 29 patients (16%) were lost to follow up (Figure 2).
Figure 2.
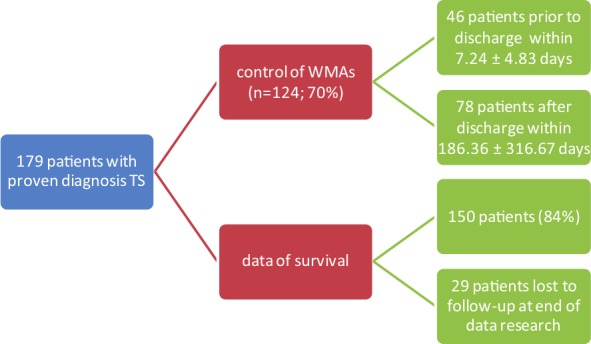
Overview of patients with proven diagnosis of TS: data concerning control of WMAs and data of survival.
Statistical analysis
Continuous variables are presented as mean±SD and ranges, unless otherwise specified. Categorical data are presented as absolute values and percentages. We analysed the data using Microsoft Office Excel 2007.
Results
Clinical characteristics and presentation
A total of 179 patients were diagnosed as having TS (Table 1). At initial hospitalization, 168 patients (94%) were women and 11 (6%) were men. Female patients were 38–88 years of age (69.6±11.3 years); male patients were 35–80 years of age (62.4±13.1 years). Of all 179 patients with TS, 44 (25%) had no coronary risk factor. As coronary risk factors, seven major coronary risk factors were detected: arterial hypertension was seen in 77% (n=104), 10% (n=13) were ex-smokers, 12% (n=16) had a family history of coronary heart disease, 13% (n=18) were suffering of hypercholesterolaemia and 24% (n=32) of hyperlipidaemia, 18% (n=24) were active smokers, 20% (n=20) were suffering from diabetes mellitus type II and one patient from diabetes mellitus type I. Most common clinical symptoms at the time of presentation in hospital were chest pain in 135 patients (82%), dyspnoea in 53 patients (32%), alone or in combination, vomitus, and nausea in 27 patients (16%), and vertigo as well as syncope in seven patients (4%). Four patients (2%) showed symptoms of transient global amnesia (Table 1.)
Table 1.
Patient characteristics at time of hospital admission.
| Characteristic | Patient population |
|---|---|
| Women | 94 (168) |
| Age (years) | 69.6±11.3 (35–88)a |
| Men | 6 (11) |
| Age (years) | 62.4±13.1 (38–88) |
| Cardiovascular risk factors | 75 (135) |
| Arterial hypertension | 77 (104) |
| Hyperlipidaemia | 24 (32) |
| Active smokers | 18 (24) |
| Hypercholesterinaemia | 13 (18) |
| Family history of coronary artery disease | 12 (16) |
| Former smoker | 10 (13) |
| DM II | 20 (20) |
| Other diseases | 55 (99) |
| Tumour disease | 28 (27) |
| Chronic obstructive pulmonary disease | 18 (17) |
| Atrial fibrillation | 16 (16) |
| Depression | 15 (15) |
| Symptoms at time of QE | 92 (165) |
| Chest pain | 82 (135) |
| Dyspnoea | 32 (53) |
| Nausea and vomiting | 16 (27) |
| Vertigo and syncope | 4 (7) |
| Transitory global amnesia | 2 (4) |
| Duration of hospitalization time (days) | 7.8±7.1 (1–63) |
| ECG at time of QE | 98 (173) |
| Normal ECG | 7 (12) |
| T-wave inversion | 49 (84) |
| ST-elevation | 43 (74) |
| Left bundle branch block | 6 (11) |
| ST-depression | 5 (9) |
Values are % (n) or mean±SD (range).
QE, qualifying event.
Various possible triggering factors were identified in 101 patients (57%) (Table 2). Forty-one patients (41%) had emotional problems at the onset, 52 patients (51%) had some type of physical stress, and eight patients (8%) showed emotional as well as physical stress factors (Table 2).
Table 2.
Examples of emotional and/or physical stressors triggering heart failure in TS patients.
| Triggering Factors | ||
|---|---|---|
| emotional (n=41) | physical (n=52) | emotional and physical (n=8) |
| visit of relatives (n=1) emotional load situation (n=4) death/funeral of family member/relative/ near person (n=15) alzheimer’s disease of relative (n=1) dispute with partner (n=1) concern about relative (n=2) job problems (n=1) family conflict (n=1) dispute with relative (n=1) prolonged sorrow (n=1) loss of money (n=2) increased family stress (n=1) insult of relative (n=1) pronounced stress (n=1) car fire at the previous day (n=1) private burden (n=1) total loss of green houses (n=1) scheduled operation (n=2) acute stress reaction (n=1) depression (n=1) panic attack (n=1) |
nausea and vomiting (n=2) car accident (n=2) fall (n=5) postoperative (n=4) acute psychosis with raptus (n=1) fit of coughing (n=1) exacerbation of infection (n=4) dental treatment (n=2) operation (n=5) walk (n=3) climbing of stairs (n=2) dialysis (n=1) unusual exercise (n=1) skiing (n=1) luging (n=1) anaphylactic shock (n=1) diarrhoe (n=2) insult (n=2) hypothermia (n=1) anesthetization (n=1) intestinal obstruction (n=1) alcohol withdrawal symptom (n=1) enterocolitis with clostridium difficile (n=1) dance (n=1) hematemesis (n=1) cough (n=1) computer tomography (n=1) common cold (n=1) hypertensive crisis (n=1) medical treatment (n=1) |
erradication of helicobacter pylori (n=1) medical treatment in combination with wearing conversation (n=1) dispute and strike against chest (n=1) urinary retention and death of relative (n=1) accident and operation (n=1) fall after syncope and aperture of apartment by the police (n=1) exacerbation of COPD and death of relative (n=1) performance of a rescucitation (n=1) |
Medication
Of all patients, 37% had no medication regularly taken at admission (Table 3). Among the remaining 112 patients (63%), 99 patients were taking drugs regularly at the time of their event either alone or in combination, including angiotensin-converting enzyme inhibitors (ACEIs) (41%), aspirin (37%), proton pump inhibitors (PPIs) (30%), beta-blockers (27%), diuretics (25%), statins (21%), oral anticoagulation (13%), calcium channel blockers (10%), clopidogrel (9%), angiotensin II receptor blockers (10%), nitrates (4%), heparins (4%), and antiarrhythmic agents (3%), respectively.
Table 3.
Medications of patients prior to TS onset, treatment of TS, discharge medication, and medication at time of follow up.
| Medication | Prior to qualifying event (n=112) | Treatment of TS (n=137) | Discharge medication (n=172) | Follow-up medication (n=52) |
|---|---|---|---|---|
| ACEI | 41 (46) | 28 (38) | 58 (100) | 42 (22) |
| Antidepressant drug | 21 (23) | 15 (20) | 24 (41) | 27 (14) |
| Aspirin | 37 (41) | 90 (123) | 74 (128) | 60 (31) |
| AT II inhibitor | 10 (11) | 6 (8) | 11 (19) | 15 (8) |
| Beta-blocker | 27 (30) | 49 (67) | 70 (121) | 60 (31) |
| Ca-channel blocker | 10 (11) | 4 (6) | 8 (14) | 12 (6) |
| Clopidogrel | 9 (10) | 75 (102) | 21 (36) | 14 (7) |
| Diuretic | 25 (28) | 30 (41) | 33 (56) | 33 (17) |
| Heparin | 4 (4) | 66 (90) | 17 (29) | 2 (1) |
| Oral anticoagulation | 13 (14) | 5 (7) | 8 (13) | 8 (4) |
| PPI | 30 (33) | 61 (84) | 61 (105) | 53 (28) |
| Statin | 20 (23) | 33 (45) | 42 (72) | 37 (19) |
| Catecholamines | None | 13 (18) | None | None |
Values are % (n).
ACEI, angiotensin-converting enzyme inhibitor; AT, angiotensin; PPI, proton pump inhibitor.
Discharge medications were beta-blockers (70%), aspirin (74%), PPIs (61%), ACEIs 58%) statins (42%) diuretics (33%) nitrates (4%) heparin (17%) clopidogrel (21%) angiotensin II inhibitors (11%) calcium channel blockers (8%), and oral anticoagulation (8%). In addition, 24% of the patients were taking antidepressant drugs (Table 3).
ECG
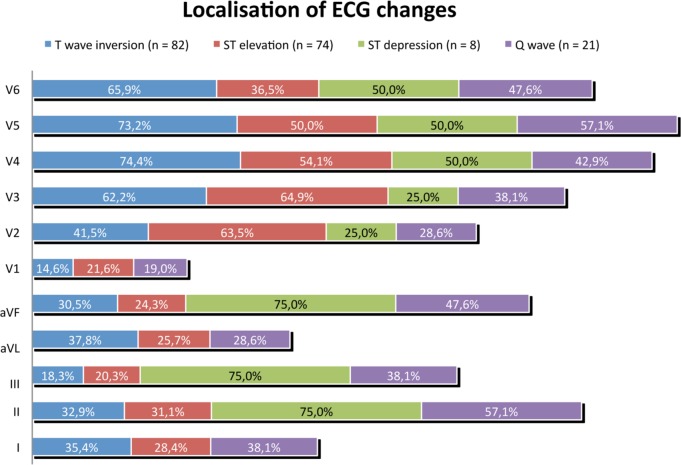
In the first diagnostic ECG at admission, diffuse T-wave inversion was the most common ECG findings, occurring in 86 patients (49%). ST-elevation mimicking acute ST-elevation MI (STEMI) was demonstrated in 74 patients (42%). Other ECG findings included initially pathological Q-waves (n=22; 13%), new left bundle branch block (n=11; 6%), new right bundle branch block (n=4; 2%), left axis deviation (n=22; 13%), or normal ECG (n=12; 7%) (Figure 3). The respective ECG changes showed various localizations: T-wave inversion was mainly seen in the lateral and anterior leads of the ECG, ST-elevation mostly in the lateral leads, ST-depression and Q-waves developed mainly in the inferior leads (Figure 4).
Figure 3.
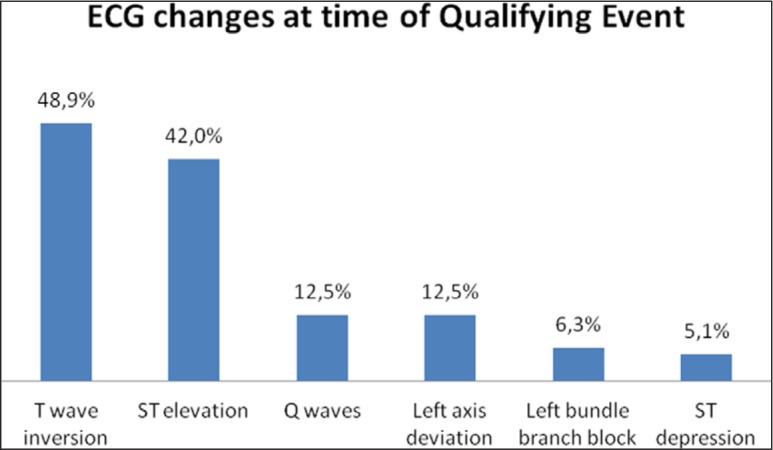
ECG changes at time of onset.
Figure 4.
Localization of ECG changes at time of onset.
Coronary angiography
Coronary angiography was performed in 177 patients (99%), and two patients (1%) had cardiac multislice computed tomography evaluation of coronary arteries. None of them showed significant coronary artery stenosis (defined as ≥50% stenosis), 21 patients (12%) showed non-significant stenosis of the left descending artery, 14 patients (8%) showed non-significant stenosis of the right coronary artery, six patients (3%) showed non-significant stenosis of the left circumflex artery, and 148 (83%) patients showed normal epicardial coronary arteries with no obstructive changes.
Echocardiography and levocardiography
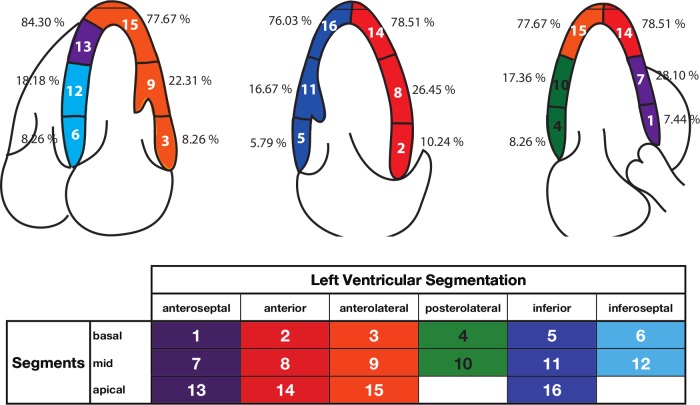
Left ventricular function and regional WMAs detected in echocardiography (n=134; 75%) and levocardiography (n=126; 70%) showed substantial variability with respect to the patterns of akinesia, hypokinesia, and dyskinesia and type of ventricular ballooning including: (1) an apical type of TS (n=89; 50%); (2) a combined apical and midventricular form of TS (n=23; 13%); (3) a midventricular form of TS (n=6; 3%); and (4) three patients showed an unusual type of basal WMAs of the left ventricle. WMAs detected by echocardiography demonstrated akinesia of apical segments in 55 patients, combined apical and midventricular akinesia in 13 patients as well as isolated midventricular akinesia in two patients. Hypokinesia was detected in apical segments in 13 patients and in the apical and midventricular left ventricular wall in three patients. An unusual pattern of basal hypokinesia or akinesia could be seen in two patients. Dyskinesia of the apical region was reported in 4 patients as well as midventricular dyskinesia in one patient. WMAs that do not correlate exactly to one of the mentioned classical types of TS above were seen in 53 patients (Figure 5). Wall motion score index was 1.56±0.31 (1.0625 to 2.5). WMAs seen in the levocardiography were apical dysfunction in 17 patients, midventricular dysfunction in three patients, the combined form of apical and midventricular dysfunction in eight patients. One patient showed atypical WMAs in the basal segments of the left ventricle.
Figure 5.
Distribution of WMAs at time of TS onset.
Ejection fraction and left ventricular function
Echocardiographically determined left ventricular function (LVF) was moderately reduced (EF 30–40%) in 49 patients (37%), mildly reduced LVF (EF 45–54%) in 30 patients (22%), normal LVF (EF ≥55%) in 25 patients (19%), and highly reduced LVF (EF ≤30%) in 19 patients (14%). In the acute period of the TS, 56 of 179 patients had a calculated EF determination measured by echocardiography: mean EF was 45.2±13.3% (range 15–82.9%). EF was calculated in 85 patients by levocardiography: mean EF was 49.6±13.3% (range 16–87%).
Acute management and complications
In the acute phase, patients received aspirin (90%), clopidogrel (75%), and heparin (66%) as recommended in established guidelines for treatment of ACS. In addition, patients were treated with PPIs (61%), beta-blockers (49%), statins (33%), diuretics (30%), nitrates (29%), and ACEIs (28%). Eighteen patients (13%) needed intravenous inotropic agents because of hypertension and cardiogenic shock (Table 3). Cardiovascular complications were observed in 25 patients (14%) during hospitalization and consisted of cardiac arrhythmias (n=10; 40%) including cardiac arrest in three patients, ventricular fibrillation in three patients, atrial fibrillation in two patients, cardiac decompensation in eight patients (32%), cardiogenic shock in six patients (24%), and death of cardiovascular cause in one patient. Mean time of hospital admission to discharge was 7.7±7.1 days (range 1–63 days).
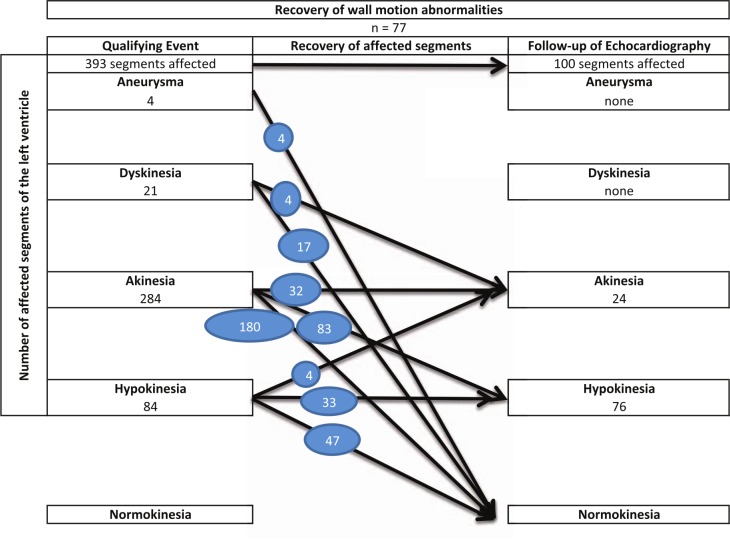
Follow-up determination of WMAs
Control of LVEF was available in 124 patients (70%): 46 patients (26%) underwent a control of echocardiography prior to discharge within 7.24±4.83 days and 78 patients (44%) had an examination of regional WMAs within 186.36±316.67 days after initial diagnosis of TS. Control of regional wall motion showed complete recovery of WMAs in 59% of patients (n=73) (Figures 6 and 7), 11% (n=14) of patients showed persistent akinesia, 34 patients (28%) demonstrated hypokinesia, and in one patient dyskinesia was detected (Figure 6). LVEF was reported in 72 patients and demonstrated normal LVEF (EF ≥55%) in 67 patients (93%), mildly reduced LVEF (EF 54 -45%) in four patients (6%) and severely reduced LVEF (EF ≤30%) in one patient. Follow up in patients that had a control of regional wall motion after discharge (n=78; within 186.36±316.67 days after initial event) showed beginning improvement of WMAs in most patients. No regional WMAs could be seen in 62 patients at time of follow up. Four patients showed improvement of regional WMAs due to reduced number of affected segments, 10 patients showed improvement contractility (from akinesia to hypokinesia), and two patients showed persistent apical hypokinesia.
Figure 6.
Recovery of WMAs detected in 77 patients with primary examination of WMAs by transthoracic echocardiography and follow-up echocardiography.
Figure 7.
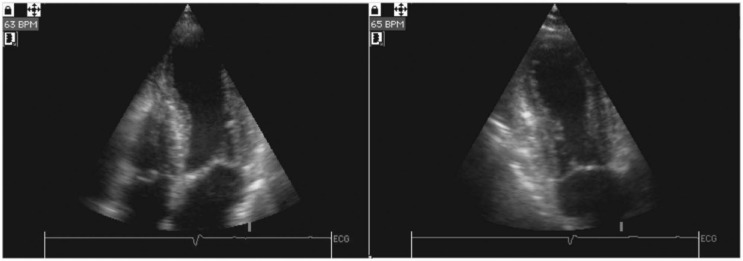
Four-chamber views in systole showing (a) TS in acute phase and (b) full recovery of WMAs 2 months after initial event.
A control of coronary angiography was reported in only two patients (3%): both of them showed normal coronary arteries without significant stenosis of coronary arteries and normalization of wall WMAs with normal systolic function. Medication at time of follow up was reported in 65% of the patients with follow up (Table 3).
Survival and mortality
In 150 of 179 patients (84%), data of survival was available over a follow-up period between 6 months and 88 months (36.5±18.9 months); 29 patients (16%) were lost to follow up (Figure 1). Thirteen patients died after hospital discharge, three of of cardiovascular causes, the others (n=10) of noncardiac causes. In-hospital mortality was 0.6%, 30-day mortality 1.3%, and mortality after 2 years 6.7%.
Recurrences
An additional non-fatal TS episode was experienced in four patients (2%) with typical symptoms and no significant stenosis of epicardial coronary arteries shown in the coronary angiogram. Medication on the occasion of the recurrent TS event was aspirin, ACEIs, statins, beta-blockers, angiotensin II inhibitors, diuretics, PPIs, and one patient had oral anticoagulation. Three patients with additional TS episodes exhibited apical akinesia either in echocardiography or levocardiography, no regional wall motion abnormalities was described in one patient. One patient had echocardiography follow up half a year after the recurrent event and the akinesia resolved in hypokinesia of the apex.
Discussion
The present series of patients with TS is one of the largest worldwide and confirms in general the data provided by other studies but presents also slight differences to what is known.4,7,8,14–21
In line with others, our series reports that most patients with TS were elderly women. Mean age of the patients in our study was 69.59±11.33 years which was similar in most other publications.14–17 While in our hands a minority of patients were ≤55 years of age (n=25; 14%) others found 35% of their patients significantly younger (≤50 years of age).17 Percentage of males developing TS was comparable with most other studies as were cardinal symptoms of TS including acute chest pain and dyspnoea.4,12,14–19
In our study only almost half of the patients (46%) showed emotional or physical stress immediately prior to hospitalization although others reported a higher incidence of those triggers in their patient cohort.17 These findings demonstrate the importance of further studies to detect causative trigger events with regard to psychosomatic analysis of patients suffering from cardiovascular disease.
In our hands the most common ECG changes were T-wave inversions and ST-elevation according also to the results from other studies.3,5,14,17,18
We were able to describe four different classes of TS based on the type of WMAs. In contrast to other studies, which described the combined biventricular and apical type as the most common,16 the most common type of TS in our series was the apical type. We detected also three patients with an unusual type of basal TS, which has been described only in previous studies1,9,20 and which has not been described in Austria. Complete recovery of initial WMAs was seen in about two-thirds of patients, which was lower as expected and described elsewhere.17
It is general believe that TS usually is a benign disease, but infrequent but severe complications of TS, mainly cardiac arrhythmias, cardiogenic shock, and cardiac decompensation, have been described12,16,17 and have also been seen in our patients. In line with a relatively benign course of disease is the relatively low mortality in our patient cohort: we found an in-hospital mortality of 0.6% and a 30-day mortality of 1.3%, as well as mortality after 2 years of 6.7%. This is markedly lower as expected from patients with STEMI based on severe coronary artery disease.22,23 These data also differ from another study in TS patients that showed higher mortality rates comparable to the mortality in patients with acute MI.3
Interestingly, patients with proven diagnosis of TS received not the optimal pharmacological therapy as recommended for patients with STEMI neither in-hospital nor at discharge. One explanation for this is that recommendations for optimal treatment of TS patients are still lacking and that cardio-protective drugs such as beta-blockers, ACEIs, aspirin, or oral anticoagulants could not prevent recurrence of TS, as shown previously.17
Study limitations
The retrospective analysis of this multicentre registry of patients with TS bears some problems and is potentially biased to some extent: Long-term follow up of patients was only available in roughly 84% of the patient cohort. Furthermore, the interval between the initial event and the follow-up echocardiography to prove changes in WMAs over time varied for months. Both limitations are based on the fact that no uniform strategy for control investigations was followed by the different participating centres. As a consequence of relatively early performed echocardiography controls (in many instances already at the end of the hospital stay following the index event), the numbers for improvement of WMAs after the initial event described in our series might be too low and delayed improvement was not investigated in all patients. However, hard clinical endpoints (e.g. mortality or relapses of TS) have been investigated in the long term in most patients.
In conclusion, our registry study in Austrian patients with TS is one of the biggest worldwide and gives detailed information about clinical characteristics, in-hospital complications as well as long-term follow up with respect to recurrence of disease and mortality. As demonstrated by others the prevalence of TS is higher in women than in men. Patients aged ≤55 years developed TS in our study cohort less frequently than described in the literature. Clinical presentation and ECG changes mimicking acute MI were found in the majority of patients, and acute coronary angiography is still the optimal diagnostic method to disclose severe coronary artery sclerosis. Trigger factors of TS were identified and showed a wide spread of emotional as well as physical stress events prior to qualifying event of TS. In contrast to other studies, there was a lack of preceding stress events in about half of our patients. While all patients demonstrated regional WMAs at presentation and four types of TS could be distinguished as also demonstrated in the international literature, the most common type of TS in our hands was not the combined apical and midventricular type as expected from other trials but the isolated apical type. Less frequent were the isolated midventricular type and the very rare basal type of TS. As also seen in our study, recovery of regional WMAs is frequently delayed, which underscores the importance of long-term echocardiographic follow up as a routine strategy. With respect to mortality and recurrences of disease, TS is, in general, benign. However, in-hospital cardiovascular complications like cardiac arrhythmias, cardiogenic shock, and/or heart failure have been shown to impact the clinical course of individual patients. Accordingly, adequate management of cardiac arrhythmias, hypertension and acute heart failure is needed in treatment of patients with complicated course of TS. As this retrospective analysis of an Austrian registry in patients with TS lacks important information, a prospective Austrian registry in patients with TS is in a concrete planning stage.
Footnotes
Conflict of interest: The authors declare that there is no conflict of interests.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1. Song BG, Chun WJ, Park YH, et al. The clinical characteristics, laboratory parameters, electrocardiographic, and echocardiographic findings of reverse or inverted takotsubo cardiomyopathy:comparison with mid or apical variant. Clin Cardiol 2011; 34: 693–699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Deshmukh A, Kumar G, Pant S, et al. Prevalence of Takotsubo cardiomyopathy in the United States. Am Heart J 2012; 164: 66–67 [DOI] [PubMed] [Google Scholar]
- 3. Kurowski V, Kaiser A, von Hof K, et al. Apical and midventricular transient left ventricular dysfunction syndrome (Tako-Tsubo cardiomyopathy). Frequency, mechanism, and prognosis. Chest 2007; 132: 809–816 [DOI] [PubMed] [Google Scholar]
- 4. Akashi YJ, Nakazawa K, Sakakibara M, et al. The clinical features of takotsubo cardiomyopathy. Q J Med 2003; 96: 563–573 [DOI] [PubMed] [Google Scholar]
- 5. Akashi YJ, Musha H, Kida K, et al. Reversible ventricular dysfunction takotsubo cardiomyopathy. Eur J Heart Fail 2005; 7: 1171–1176 [DOI] [PubMed] [Google Scholar]
- 6. Eitel I, Berhendt F, Schindler K, et al. Differential diagnosis of suspected apical ballooning syndrome using contrast-enhanced magnetic resonance imaging. Eur Heart J 2008; 29: 2651–2659 [DOI] [PubMed] [Google Scholar]
- 7. Satoh H, Tateishi H, Uchida T. Takotsubo-type cardiomyopathy due to multivessel spasm. In: Kodama K, Haze K, Hon M. (eds) Clinical aspects of myocardial injury: from ischemia to heart failure (in Japanese). Tokyo: Kagakuhyouronsya: 1990. pp 56–64 [Google Scholar]
- 8. Dote K, Sato H, Tateishi H, et al. Myocardial stunning due to simultaneous multivessel spasms: a review of five cases (in Japanese with English abstract). J Cardiol 1991; 21: 203–214 [PubMed] [Google Scholar]
- 9. Brenner R, Weilenmann D, Maeder MT, et al. Swish postmenopausal women with takotsubo cardiomyopathy. Clin Cardiol 2012; 35: 340–347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hurst RT, Askew JW, Reuss CS, et al. Transient midventricular ballooning syndrome. A new variant. J Am Coll Cardiol 2006; 48: 579–583 [DOI] [PubMed] [Google Scholar]
- 11. Sharkey SW, Lesser JR, Zenovich AG, et al. Acute and reversible cardiomyopathy provoked by stress in women from the United States. Circulation 2005;111;472–479 [DOI] [PubMed] [Google Scholar]
- 12. Haghi D, Athanasiadis A, Papavassiliu T, et al. Right ventricular involvement in Takotsubo cardiomyopathy. Eur Heart J 2006; 7: 2433–2439 [DOI] [PubMed] [Google Scholar]
- 13. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005; 18: 1440–1463 [DOI] [PubMed] [Google Scholar]
- 14. Tsuchihashi K, Ueshima K, Uchida T, et al. ; Angina pectoris-myocardial infarction investigations in Japan Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. J Am Coll Cardiol 2001; 38: 11–18 [DOI] [PubMed] [Google Scholar]
- 15. Bybee KA, Kara T, Prasad A, et al. Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med 2004; 141: 858–865 [DOI] [PubMed] [Google Scholar]
- 16. Elesber AA, Prasad A, Lennon RJ, et al. Four-year recurrence rate and prognosis of the apical ballooning syndrome. J Am Coll Cardiol 2007; 50: 448–452 [DOI] [PubMed] [Google Scholar]
- 17. Sharkey SW, Windenburg DC, Lesser JR, et al. Natural history and expansive clinical profile of stress (Tako-Tsubo) cardiomyopathy. J Am Coll Cardiol 2010; 55: 333–341 [DOI] [PubMed] [Google Scholar]
- 18. Park SM, Prasad A, Rihal C, et al. Left ventricular systolic and diastolic function in patients with apical ballooning syndrome compared with patients with acute anterior ST-segment elevation myocardial infarction: a functional paradox. Mayo Clin Proc 2009; 84: 514–521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wittstein IS, Thiemann DR, Lima JAC, et al. Neurohumoral features of myocardial stunning due to sudden stress. N Engl J Med 2005; 352: 539–548 [DOI] [PubMed] [Google Scholar]
- 20. Mahmoud RE, Mansencal N, Pilliére R, et al. Prevalence and characteristics of left ventricular outflow tract obstruction in Tako-Tsubo syndrome. AM Heart J 2008; 156: 543–548 [DOI] [PubMed] [Google Scholar]
- 21. Klug G, Wolf C, Trieb T, et al. Evaluation of transient apical ballooning with cardiac magnetic resonance imaging and 31-phosphorous magnetic resonance spectroscopy. Int J Cardiol 2007; 118: 249–252 [DOI] [PubMed] [Google Scholar]
- 22. Huber K, Goldstein P, Danchin N, et al. Network models for large cities: the European experience. Heart 2010; 96: 164–169 [DOI] [PubMed] [Google Scholar]
- 23. Wijns W, Kolh P, Danchin N, et al. Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2010; 31: 2501–2555 [DOI] [PubMed] [Google Scholar]