Abstract
Aims:
Hyperglycemia is associated with increased mortality in cardiac patients. However, the predictive value of admission- and average glucose levels in patients admitted to an intensive cardiac care unit (ICCU) has not been described.
Methods:
Observational study of patients admitted to the ICCU of a tertiary medical center in whom glucose levels were measured at and during admission. Over a 19-month period, 1713 patients were included. Mean age was 63±14 years, 1228 (72%) were male, 228 (17%) had known diabetes. Median (interquartile) glucose levels at admission were 7.9 (6.5–10.1) mmol/l; median glucose levels during ICCU admission (873 patients with three or more measurements) were 7.3 (6.7–8.3) mmol/l. Cox regression analysis was performed including the variables age, gender, admission diagnosis, length of stay, prior (cardio)vascular disease and diabetes.
Results:
A 1 mmol/l increase in admission glucose level (above 9 mmol/l) was associated with a 10% (95% confidence interval (CI): 7 –13%) increased risk for all-cause mortality. A 1 mmol/l higher average glucose level (above 8 mmol/l) was an additional independent predictor of mortality (HR 1.11, 95% CI: 1.03 – 1.20). At 30 days, 16.8% (97/579) of the patients with an admission glucose level in the highest tertile (>9.8 mmol/L) had died vs 5.2% (59/1134) of those with a lower admission glucose level.
Conclusion:
In a high risk ICCU population, both high admission glucose levels as well as high average glucose levels during hospitalization were independently associated with increased mortality, even when accounting for other risk factors and parameters of disease severity.
Keywords: Glucose levels, prognosis, acute coronary syndrome, intensive cardiac care
Introduction
Hyperglycemia in patients with acute medical conditions has been associated with increased mortality compared to normoglycemia in patients with the same condition.1 Indeed, outcome is improved with insulin treatment in hyperglycemic patients presenting with acute myocardial infarction.2 However, the prognostic implications of initial (admission) versus sustained hyperglycemia in high risk patients admitted to an intensive cardiac care unit (ICCU) have been less well studied. Therefore, the aim of this study was to evaluate the predictive value of both admission and average glucose levels in a high risk population of patients admitted to an ICCU with respect to all-cause mortality.
Methods
Study population
The Thoraxcenter of the Erasmus University Medical Center is a tertiary care facility in Rotterdam, The Netherlands. The ICCU consists of eight beds with a 1:1–1:2 nurse to patient ratio and 1400–1700 admissions per year. The present study cohort included patients admitted to the ICCU of the Thoraxcenter between 1 January 2007 and 28 July 2008. During that period, 2396 patients were admitted to the ICCU. Glucose measurements were available in 1796 patients (75%) who were included in the analysis of the relation between admission glucose level and survival (Figure 1).
Figure 1.
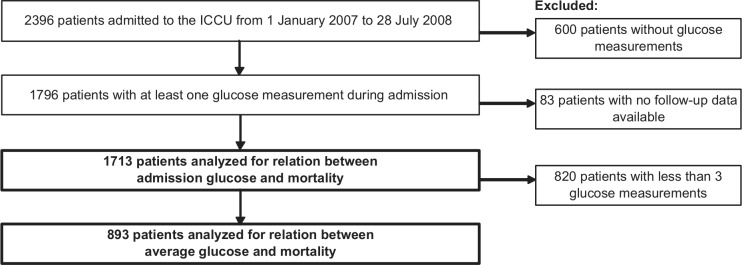
Patient inclusion.
ICCU: intensive cardiac care unit.
In the 893 patients with three or more measurements, the average glucose level during admission was calculated using the area under the curve with linear interpolation.3 This method takes into account differences in time intervals between the glucose measurements. Patients with less than three glucose measurements during admission were omitted from this analysis to provide a more reliable estimate of average glucose levels.
During the study period, a simple sliding scale insulin protocol with a target glucose range of 4.5–7.0 mmol/l was used. The protocol has been described previously.4 Briefly, after each glucose measurement some advice was given with regard to dosage of insulin infusion and when to repeat the glucose measurement. The advised interval between measurements was shorter for high and low glucose values than for measurements in the target range. The protocol was nurse-driven, and initiated for all patients with an acute myocardial infarction or with a history of diabetes. The initial glucose measurement was taken at admission, regardless of nutritional state. For all other patients with elevated glucose levels, a physician was consulted first. Copies of the protocol were available at the bedside of each patient and at the main ICCU desk. Plasma glucose concentration was measured in the hospital laboratory using the hexokinase method (Modular analytics EVO-P 800, Roche, Switzerland) in venous and arterial blood samples which were collected in Fluoride Ethylenediaminetetraacetic acid (F/EDTA) tubes to stabilize glucose.
Data collection and follow-up
Patient demographics, admission diagnosis and medical history were registered in the patient data management system. Additional medical data was retrieved from hospital discharge letters and charts. Laboratory values (including glucose and troponin-T) were registered in the hospital information system. Follow-up data were obtained in 2010. The median (interquartile range (IQR)) follow-up was 27 (23–34) months. All-cause mortality was determined from the hospital records and the municipal civil registries.
Analyses
Statistical analysis was performed with SPSS 15.0 (Chicago, USA). Continuous data were expressed as mean with standard deviation (SD) or median with IQR, as appropriate. Differences in continuous variables were evaluated using the Student t-test and analysis of variance. Differences in proportions were compared using the χ2 test. Cox-regression analysis was used to determine the predictive value of admission and average glucose levels for all-cause mortality.
The admission glucose and average glucose levels, as well as age, body mass index, duration of stay, troponin-T and Acute Physiology and Chronic Health Evaluation (APACHE)-2 score were entered as continuous variables. Diabetes, hypertension, prior hypertension, prior renal disease and prior heart failure were entered as dichotomous variables. Dichotomous variables were also defined for combined prior atherothrombotic events (myocardial infarction or (transient) cerebrovascular event) and atherosclerotic disease (prior percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG), prior angina or peripheral atherosclerotic disease). Admission diagnosis was categorized into three groups: acute coronary syndrome (myocardial infarction or unstable angina), other severe cardiac disease (cardiac arrest, heart failure or arrhythmia), and others (including valvular heart disease and periprocedural care).
First, univariate analysis was performed. Subsequently, multivariate analysis was performed adjusting for age and gender, and for all variables that were associated (p<0.05) with mortality in the univariate analysis. The risk was expressed as a hazard ratio (HR) with a corresponding 95% confidence interval (CI). A p-value<0.05 was considered statistically significant.
Results
During the study period, data were collected in the 1796 patients who had at least one glucose measurement (75% of all admissions). Follow-up data were available for 1713 patients (96%). Mean age was 63.2±14 years, 1227 (72%) were male and 228 (17%) were known diabetics (Table 1). A total of 1075 (70%) patients were admitted with an acute coronary syndrome. Median length of stay in the ICCU was 0.7 (0.2–1.5) days during which a median number of three (1–8) glucose measurements were done. Altogether 893 patients had three or more glucose measurements during their stay in the ICCU.
Table 1.
Patient characteristics.
| Parameter | All patients |
Tertile of admission glucose |
p-valuea | ||||
|---|---|---|---|---|---|---|---|
| (n=1713) |
Highest (n=579) |
Lower two (n=1134) |
|||||
| Value | n | Value | n | Value | n | ||
| Male gender | 72% | 1227 | 69% | 398 | 73% | 829 | 0.06 |
| Age (years) | 63.2±14 | 1713 | 65.0±13 | 579 | 62.2±14 | 1134 | <0.001 |
| BMI (kg /m2) | 26.4±4 | 899 | 26.9±5 | 182 | 26.2±4 | 606 | 0.03 |
| History | |||||||
| Diabetes | 17% | 288 | 31% | 177 | 10% | 111 | <0.001 |
| Hypertension | 30% | 519 | 33% | 188 | 29% | 331 | 0.2 |
| Chronic pulmonary disease | 8% | 143 | 9% | 49 | 8% | 94 | 0.2 |
| Renal disease | 7% | 123 | 6% | 37 | 8% | 86 | 0.03 |
| Prior AMI | 21% | 366 | 24% | 137 | 20% | 229 | 0.3 |
| Prior cerebrovascular event | 9% | 161 | 9% | 54 | 9% | 107 | 0.1 |
| Prior angina | 10% | 175 | 7% | 43 | 12% | 132 | <0.001 |
| Prior PCI | 17% | 289 | 16% | 92 | 17% | 197 | 0.4 |
| Prior CABG | 9% | 156 | 9% | 54 | 9% | 102 | 0.2 |
| Peripheral vascular disease | 5% | 80 | 5% | 30 | 4% | 50 | 0.7 |
| Prior heart failure | 8% | 130 | 6% | 33 | 9% | 97 | 0.001 |
| ICCU stay (days) | 0.7 (0.2–1.5) | 1713 | 0.8 (0.2–2.7) | 579 | 1.6 (0.2–1.1) | 1134 | <0.001 |
| APACHE-2 score | 14 (10–21) | 1222 | 16 (12–30) | 440 | 13 (10–18) | 782 | <0.001 |
| Suspected ACS | 69.7% | 1075 | 65.3% | 358 | 72.1% | 717 | 0.005 |
| Final diagnosis | <0.001 | ||||||
| Myocardial infarction | 44% | 761 | 52% | 303 | 40% | 458 | |
| Unstable angina | 16% | 267 | 8% | 45 | 20% | 222 | |
| Angina, stable | 3% | 47 | 2% | 10 | 3% | 37 | |
| Cardiac arrest | 6% | 98 | 13% | 73 | 2% | 25 | |
| Heart failure | 7% | 121 | 10% | 60 | 5% | 61 | |
| Arrhythmia | 7% | 114 | 5% | 29 | 8% | 85 | |
| Valvular disease | 5% | 80 | 2% | 10 | 6% | 70 | |
| Procedure | 5% | 90 | 4% | 21 | 6% | 69 | |
| Other | 8% | 135 | 5% | 28 | 9% | 107 | |
| Glucose measurements (n) | 3 (1–8) | 1713 | 5 (1–15) | 579 | 2 (1–6) | 1134 | <0.001 |
| Admission glucose (mmol/l) | 7.9 (6.5–10.1) | 1713 | 11.7 (10.0–14.8) | 579 | 6.9 (6.1–7.9) | 1134 | <0.001 |
| Average glucose (mmol/l) | 7.3 (6.7–8.3) | 893 | 7.9 (7.2–9.3) | 355 | 7.1 (6.5–7.4) | 538 | <0.001 |
Values are displayed as %, mean±standard deviation (SD) or median (25th–75th percentile).
ACS: acute coronary syndrome; AMI: acute myocardial infarction; APACHE: Acute Physiology and Chronic Health Evaluation; BMI: body mass index; CABG: coronary artery bypass grafting; ICCU: Intensive Cardiac Care Unit; PCI: percutaneous coronary intervention.
p value for comparison of highest vs lower two tertiles.
Median admission glucose level was 7.9 (6.5–10.1) mmol/l and, in patients with three or more measurements, the median glucose level during admission was 7.3 (6.7–8.3) mmol/l. Patients with an admission glucose level in the highest tertile were older, more often had known diabetes and were less likely to have prior angina, heart failure or PCI. These patients also had a longer duration of admission and had a higher disease burden, as reflected by a higher APACHE-2 score (Table 1).
Overall mortality at 30 days was 9.1% (n=156). At 12 months, 272 patients (15.9%) had died, reflecting the high risk population admitted to the ICCU (Table 2). In patients with acute myocardial infarction, mortality was 7.3% at 30 days, including patients with myocardial infarction in cardiogenic shock.
Table 2.
Mortality.
| Parameter | All patients |
Tertile of admission glucose |
p-value | ||||
|---|---|---|---|---|---|---|---|
| Value | n | Highest Value | n | Lower two Value | n | ||
| All patients (n=1713) | |||||||
| 30-day mortality | 9.1% | 156 | 16.8% | 97 | 5.2% | 59 | <0.001 |
| 12-month mortality | 15.9% | 272 | 23.7% | 137 | 11.9% | 135 | <0.001 |
| Patients with acute coronary syndrome (n=1075) | |||||||
| 30-day mortality | 5.6% | 60 | 12.3% | 44 | 2.2% | 16 | <0.001 |
| 12-month mortality | 9.7% | 104 | 16.6% | 59 | 6.3% | 45 | <0.001 |
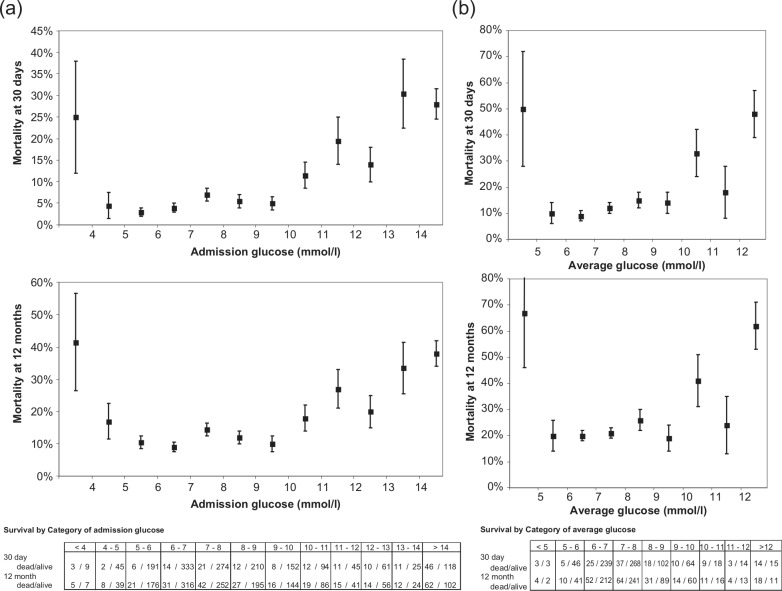
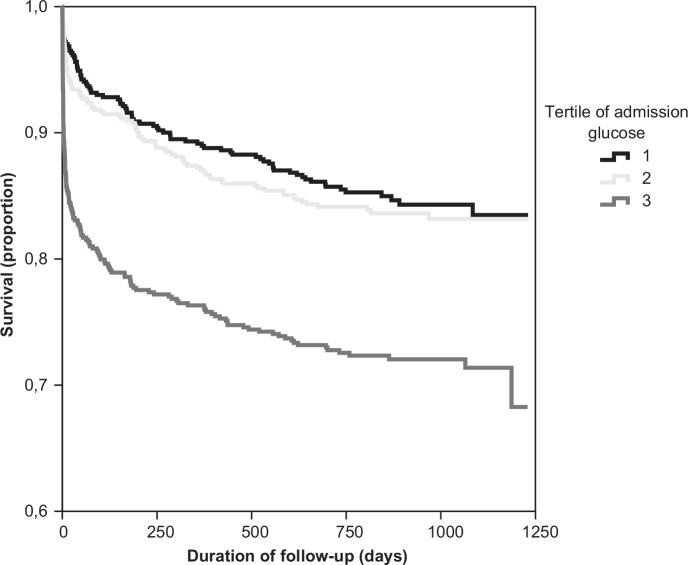
Mortality was relatively low in patients with normal or slightly elevated admission glucose levels but increased steeply in those with admission glucose levels higher than 9.0 mmol/l (Figure 2(a)), corresponding to the approximate cut-off for the upper tertile of admission glucose, which was 9.2 mmol/l. Indeed, survival was similar for patients in the lower two tertiles of the admission glucose level, as well as for average glucose levels, while mortality was significantly higher in the highest tertile (16.8% vs 5.2% at 30-days (p<0.001), Figure 3).
Figure 2.
(a) Mortality at 30 days (top) and 12 months (bottom) by admission glucose. Patients with a glucose <4 mmol/l and >14 mmol/l were grouped into the lowest and highest categories respectively. Error bars represent standard error of the mean. (b) Mortality at 30 days (top) and 12 months (bottom) by average glucose. Patients with a glucose <5 mmol/l and >12 mmol/l were grouped into the lowest and highest categories respectively. Error bars represent standard error of the mean.
Figure 3.
Survival curve by tertile of admission glucose. Tertile 1 (1.5–6.9 mmol/l); tertile 2 (7.0–9.1 mmol/l); tertile 3 (9.2–34.0 mmol/l).
Hypoglycemia (<4 mmol/l) on admission was observed in 12 patients (0.7%). We observed a high mortality in these patients of whom three had died at 30 days and five died at 12 months. However, due to the limited numbers, this did not reach statistical significance.
Each increase of 1 mmol/l in admission glucose level (above 9 mmol/l) was associated with an increased risk of death (HR 1.10, 95% CI 1.07–1.13) both in univariate and multivariate analysis (Table 3), after adjustment for risk factors, admission diagnosis, APACHE-2 score and troponin-T levels, although the latter two were not available for all patients. Separate analyses were performed for the 1075 patients admitted with an acute coronary syndrome and for 333 patients with other severe cardiac diseases, with similar results.
Table 3.
Cox-regression analysis for relation between admission and average glucose levels and all cause mortality.
| Univariate |
Multivariate |
Combined analysisa |
||||
|---|---|---|---|---|---|---|
| 1 mmol/l increase in | HR | 95% CI | HR | 95% CI | HR | 95% CI |
| Admission glucose | 1.10 | 1.08–1.13 | 1.10 | 1.07–1.13 | 1.07 | 1.04–1.10 |
| Average glucose | 1.17 | 1.10–1.23 | 1.22 | 1.14–1.30 | 1.11 | 1.03–1.20 |
HR: hazard ratio; CI: confidence interval.
Variables used for multivariate analysis: age, gender, admission diagnosis (acute coronary syndrome (ACS), cardiac arrest/heart failure/arrhythmia, others), diabetes, prior renal disease, prior heart failure, prior thrombotic event (cerebrovascular accident (CVA); transient ischemic attack (TIA);/ acute myocardial infarction (AMI)), atherosclerotic disease (peripheral, percutaneous coronary intervention (PCI)/ coronary artery bypass grafting (CABG), angina), duration of stay.
Analysis including both the admission and average glucose into the regression model, thus the HR here represents the value of admission and average glucose independent of each other.
For the 893 patients with three or more glucose measurements, the predictive value of the average glucose level, as an indicator of sustained hyperglycemia, was determined, using the same model as for admission glucose (Figure 2(b)). Again, a 1 mmol/l increase in the average glucose level above 8 mmol/l was associated with an increased risk of mortality (HR 1.22, 95% CI 1.14–1.30). In multivariate analysis, both the admission glucose level and the average glucose level were independently associated with mortality. Furthermore, the average glucose level provided prognostic information additional to that of the admission glucose level. Again, results were similar among patients with acute coronary syndromes and other cardiac diseases.
Discussion
In this high risk ICCU population, both hyperglycemia at admission (glucose>9 mmol/l) and sustained hyperglycemia during hospitalization (average glucose levels>8 mmol/l) were independent predictors of all-cause mortality. Furthermore, in patients with hypoglycemia at admission (<4 mmol/l) we also observed a trend towards an increased mortality, though the latter was not statistically significant. Other studies have reported similar relations between admission glucose levels and hospital mortality.5,6 However, in this analysis, we extend these findings to a high-risk population admitted to an ICCU and demonstrate also that sustained hyperglycemia is an independent risk factor for mortality that provides prognostic information additional to the admission glucose levels. Furthermore, we demonstrate that this relation is not linear, since patients in the two lower glucose tertiles had similar mortality rates, but that the increased risk for mortality starts at levels above 9 mmol/l for the admission glucose level and approximately 8 mmol/l for the average glucose levels.
High admission glucose levels occur in patients with known and in those with so far unrecognized diabetes mellitus,7 but may also reflect the severity of disease as a result of elevated catecholamine and cortisol levels. Additional conditions such as infection or sepsis may further disturb carbohydrate metabolism and glucose levels. These and several other factors are included in the APACHE-2 score.8 However, when this score was added to the regression model, this did not alter the findings of the current analysis, which suggests that the hyperglycemia per se is associated with impaired outcome.9–11 In patients with acute myocardial infarction, hyperglycemia has been associated with higher free fatty acid concentrations,12 insulin resistance and impaired myocardial glucose metabolism, which may result in an increased oxygen consumption and, consequently, a more severe ischemic state and larger infarct size.13
Previous studies have demonstrated that an increased initial,14 as well as an increase in fasting, glucose levels during admission15 are predictors of increased mortality in patients admitted with an acute myocardial infarction. The results of our study add to these previous studies by demonstrating that glucose values taken earlier (at admission) and randomly thereafter, without knowledge of nutritional status, in an ICCU population of higher risk, provide similar prognostic information without the need to measure fasting glucose levels.
Our observations that both admission glucose levels >9 mmol/l and sustained glucose levels >8 mmol/l are independently associated with impaired outcome. On the other hand, the higher mortality in the patients with an admission glucose level <4 mmol/l emphasize the need to prevent hypoglycemia. In an intensive care setting, Van den Berghe et al.16 demonstrated reduced mortality and morbidity during hospital admission among patients treated with glucose-lowering insulin therapy. Similarly, the diabetes and insulin-glucose infusion in acute myocardial infarction (DIGAMI) study achieved better outcome with intensive insulin therapy.17 This benefit was, however, not confirmed in DIGAMI-2,18 probably because of the small differences in glucose levels among the different treatment regimens. Furthermore, in the more recent NICE sugar trial,19 an increase in hypoglycemic episodes and mortality was seen in the patients allocated to more intensive insulin therapy. Indeed, careful regulation of glucose levels in the ICCU is difficult to achieve,4,20 so targets should not be set tighter than necessary. Further studies are needed to investigate the optimal insulin treatment regimen to improve outcome in patients with acute cardiac disease.
Previously, high admission glucose levels in patients with acute myocardial infarction receiving thrombolytic21 or percutaneous reperfusion therapy22 were associated with increased mortality and morbidity. However, these studies were restricted to patients with an acute myocardial infarction and did not investigate the predictive value of sustained hyperglycemia.
The current study was performed in a high-risk, mixed cardiac patient population. It is important to note the high 30-day mortality rate for myocardial infarction: in the overall population of patients with acute myocardial infarction admitted to the ICCU (including those without glucose measurements) the 30-day mortality rate was 7.3%. However, this included patients in cardiogenic shock (9.2% of the population) with a much higher mortality rate. The mortality rate for the patients admitted with acute myocardial infarction without cardiogenic shock was 3.8% during the study period, representative for a tertiary center. The Erasmus Medical Center treats approximately 650 patients per year with primary PCI. In addition to the patients with an uncomplicated acute myocardial infarction, who are directly transferred after reperfusion treatment to surrounding hospitals, the center also treats complex patients from other hospitals.
In this high-risk population, multivariate analysis demonstrated an independent and incremental prognostic value for the glucose value at admission and the average glucose level during hospitalization. Similarly, in the DIGAMI study17 of 620 diabetic patients with acute myocardial infarction, admission glucose was independently associated with mortality during 3.4 years follow-up. The admission glucose levels in DIGAMI (15.5 mmol/l) were higher than in the current study (7.9 mmol/l), as was the 30-day mortality rate (14% vs 9.1%). The lower mortality rate in the current analysis can be explained by the inclusion of non-diabetic patients. Similar high mortality rates were reported in other studies of patients with acute coronary syndromes and high admission glucose levels, and in elderly patients (>65 years) hospitalized for acute myocardial infarction.2,6
Study limitations
Glucose values were not collected in all patients. Therefore, patients without measurements were not included. These excluded patients represent the uncomplicated patients that were directly transferred back to the referring hospital or to a step-down unit. Also, in patients with more severe disease, glucose levels may have been measured more often: thus hyperglycemic episodes in less sick patients might have gone undetected resulting in an underestimation of average glucose in patients with less severe disease. However, the frequency of measurements was taken into account when calculating the average glucose level during admission.
Seventy-two percent of the patients were male, however this percentage was consistent over the different groups: furthermore, the effect was consistent for both genders.
Conclusions
Both higher admission glucose levels and higher average glucose levels are independently associated with increased mortality in a high risk population of patients with cardiac diseases admitted to the ICCU. Furthermore, average glucose levels provided prognostic information additional to that of the admission glucose levels.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest: None declared.
References
- 1. Penfold S, Gouni R, Hamilton P, et al. Immediate in-patient management of hyperglycaemia–confusion rather than consensus? QJM 2008; 101: 87–90 [DOI] [PubMed] [Google Scholar]
- 2. Weston C, Walker L, Birkhead J. Early impact of insulin treatment on mortality for hyperglycaemic patients without known diabetes who present with an acute coronary syndrome. Heart 2007; 93: 1542–1546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Le Floch JP, Escuyer P, Baudin E, et al. Blood glucose area under the curve. Methodological aspects. Diabetes Care 1990; 13: 172–175 [DOI] [PubMed] [Google Scholar]
- 4. Lipton JA, Barendse RJ, Akkerhuis KM, et al. Evaluation of a clinical decision support system for glucose control: Impact of protocol modifications on compliance and achievement of glycemic targets. Crit Pathw Cardiol 2010; 9: 140–175 [DOI] [PubMed] [Google Scholar]
- 5. Asadollahi K, Beeching N, Gill G. Hyperglycaemia and mortality. J R Soc Med 2007; 100: 503–507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kosiborod M, Rathore SS, Inzucchi SE, et al. Admission glucose and mortality in elderly patients hospitalized with acute myocardial infarction: Implications for patients with and without recognized diabetes. Circulation 2005; 111: 3078–3086 [DOI] [PubMed] [Google Scholar]
- 7. Rydén L, Standl E, Bartnik M, et al. Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: Executive summary. The Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD). Eur Heart J 2007; 28: 88–136 [DOI] [PubMed] [Google Scholar]
- 8. Junger A, Böttger S, Engel J, et al. Automatic calculation of a modified APACHE II score using a patient data management system (PDMS). Int J Med Inform 2002; 65: 145–157 [DOI] [PubMed] [Google Scholar]
- 9. Norhammar A, Tenerz A, Nilsson G, et al. Glucose metabolism in patients with acute myocardial infarction and no previous diagnosis of diabetes mellitus: A prospective study. Lancet 2002; 359: 2140–2144 [DOI] [PubMed] [Google Scholar]
- 10. Beck JA, Meisinger C, Heier M, et al. Effect of blood glucose concentrations on admission in non-diabetic versus diabetic patients with first acute myocardial infarction on short- and long-term mortality (from the MONICA/KORA Augsburg Myocardial Infarction Registry). Am J Cardiol 2009; 104: 1607–1612 [DOI] [PubMed] [Google Scholar]
- 11. Capes SE, Hunt D, Malmberg K, et al. Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: A systematic overview. Lancet 2000; 355: 773–778 [DOI] [PubMed] [Google Scholar]
- 12. Tansey MJ, Opie LH. Relation between plasma free fatty acids and arrhythmias within the first twelve hours of acute myocardial infarction. Lancet 1983; 2: 419–422 [DOI] [PubMed] [Google Scholar]
- 13. Oliver MF. Metabolic causes and prevention of ventricular fibrillation during acute coronary syndromes. Am J Med 2002; 112: 305–311 [DOI] [PubMed] [Google Scholar]
- 14. Suleiman M, Hammerman H, Boulos M, et al. Fasting glucose is an important independent risk factor for 30-day mortality in patients with acute myocardial infarction: A prospective study. Circulation 2005; 111: 754–760 [DOI] [PubMed] [Google Scholar]
- 15. Aronson D, Hammerman H, Suleiman M, et al. Usefulness of changes in fasting glucose during hospitalization to predict long-term mortality in patients with acute myocardial infarction. Am J Cardiol 2009; 104: 1013–1017 [DOI] [PubMed] [Google Scholar]
- 16. Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med 2001; 345: 1359–1367 [DOI] [PubMed] [Google Scholar]
- 17. Malmberg K, Norhammar A, Wedel H, et al. Glycometabolic state at admission: Important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction. Long-term results from the diabetes and insulin-glucose infusion in acute myocardial infarction (DIGAMI) study. Circulation 1999; 99: 2626–2632 [DOI] [PubMed] [Google Scholar]
- 18. Malmberg K, Rydén L, Wedel H, et al. Intense metabolic control by means of insulin in patients with diabetes mellitus and acute myocardial infarction (DIGAMI 2): Effects on mortality and morbidity. Eur Heart J 2005; 26: 650–661 [DOI] [PubMed] [Google Scholar]
- 19. NICE-SUGAR study investigators, Finfer S, Chittock DR, et al. Intensive versus conventional glucose control in critically ill patients. N Engl J Med 2009; 360: 1283–1297 [DOI] [PubMed] [Google Scholar]
- 20. Lipton JA, Barendse RJ, Schinkel AFL, et al. Impact of an alerting clinical decision support system for glucose control on protocol compliance and glycemic control in the intensive cardiac care unit. Diabetes Technol Ther 2011; 13: 343–349 [DOI] [PubMed] [Google Scholar]
- 21. Wahab NN, Cowden EA, Pearce NJ, et al. ; ICONS Investigators Is blood glucose an independent predictor of mortality in acute myocardial infarction in the thrombolytic era? J Am Coll Cardiol 2002; 40: 1748–1754 [DOI] [PubMed] [Google Scholar]
- 22. De Mulder M, Cornel JH, van der Ploeg T, et al. Elevated admission glucose is associated with increased long-term mortality in myocardial infarction patients, irrespective of the initially applied reperfusion strategy. Am Heart J 2010; 160: 412–419 [DOI] [PubMed] [Google Scholar]