Abstract
Background:
Data on temporal trends in outcomes, gender differences, and adherence to evidence-based therapy (EBT) of diabetic patients with ST-segment elevation myocardial infarction (STEMI) are sparse.
Methods:
We performed a retrospective analysis of prospectively acquired data on 3565 diabetic (2412 males and 1153 females) STEMI patients enrolled in the Swiss AMIS Plus registry between 1997 and 2010 and compared in-hospital outcomes and adherence to EBT with the nondiabetic population (n=15,531).
Results:
In-hospital mortality dramatically decreased in diabetic patients, from 19.9% in 1997 to 9.0% in 2010 (ptrend<0.001) with an age-adjusted decrease of 6% per year of admission. Similar trends were observed for age-adjusted reinfarction (OR 0.86, p<0.001), cardiogenic shock (OR 0.88, p<0.001), as well as death, reinfarction, or stroke (OR 0.92, p<0.001). However, the mortality benefit over time was observed in diabetic males (ptrend=0.006) but not females (ptrend=0.082). In addition, mortality remained twice as high in diabetic patients compared with nondiabetic ones (12.1 vs. 6.1%, p<0.001) and diabetes was identified as independent predictor of mortality (OR 1.23, p=0.022). Within the diabetic cohort, females had higher mortality than males (16.1 vs. 10.2%, p<0.001) and female gender independently predicted in-hospital mortality (OR 1.45, p=0.015). Adherence to EBT significantly improved over time in diabetic patients (ptrend<0.001) but remained inferior – especially in women – to the one of nondiabetic individuals.
Conclusions:
In-hospital mortality and morbidity of diabetic STEMI patients in Switzerland improved dramatically over time but, compared with nondiabetic counterparts, gaps in outcomes as well as EBT use persisted, especially in women.
Keywords: Diabetes mellitus, evidence-based therapy, gender, primary percutaneous coronary intervention, reperfusion therapy, ST-elevation myocardial infarction
Introduction
The prevalence of diabetes mellitus has markedly increased worldwide in the last three decades.1 Registry data have shown that in acute coronary syndromes (ACS) up to a third of patients may have known diabetes while an additional third may have undiagnosed abnormal glucose metabolism.2–4 Diabetic ACS patients have worse outcomes than nondiabetic individuals, both in the short and the long term.5,6 The unfavourable outcomes may be in part explained by the higher prevalence of comorbidities and the fact that diabetic patients may be less frequently exposed to evidence-based therapy (EBT) than nondiabetic individuals.7 While the Framingham Heart Study documented a major reduction in cardiovascular mortality over time in diabetic individuals,8 little is known about temporal trends as well as gender-related outcomes of diabetic patients presenting with ST-segment elevation myocardial infarction (STEMI). In a cohort of diabetic patients with STEMI enrolled in a nationwide registry over 14 years, we described gender-related temporal trends of in-hospital outcomes.
Methods
The AMIS (Acute Myocardial Infarction in Switzerland) Plus registry
The AMIS (Acute Myocardial Infarction in Switzerland) Plus project is a nationwide prospective registry of patients admitted with ACS to 77 Swiss hospitals. The details of the registry have been previously published.9 In brief, a wide variety of institutions – ranging from community hospitals to tertiary centers – have enrolled patients in the registry since 1997. Blinded patient data are collected using a standardised web-based questionnaire and are checked for plausibility and consistency by the Institute of Social and Preventive Medicine at the University of Zurich. The registry was approved by the Above-Regional Ethics Committee for Clinical Studies and the Swiss Board for Data Security.
For each patient a total of 200 items are filled in by the study coordinator of each institution, including medical history, comorbidities, cardiovascular risk factors, clinical presentation, out-of-hospital management, early (i.e., within 24 hours following admission) in-hospital management, reperfusion therapy, hospital course, diagnostic work up, length of stay, and discharge medication. Patients are enrolled in the registry on the basis of their final diagnosis. STEMI diagnosis is based on characteristic symptoms, ST-segment elevation and/or new left bundle branch block on the initial ECG, and total creatine kinase or creatine kinase MB fraction at least twice the upper limit of normal or troponin levels according to hospital-specific assay cut-off point for myocardial infarction. The primary outcome measure was in-hospital mortality. Secondary outcome measures were in-hospital major adverse cardiac or cerebrovascular events (MACCE, defined as death, reinfarction, or stroke). Temporal trends in outcomes as well as in adherence to EBT were analysed according to diabetic status and gender. The authors are solely responsible for all study analyses, the drafting and editing of the paper and its final contents.
Statistical analysis
The present analysis included all STEMI patients enrolled in AMIS Plus between 1 January 1997 and 31 December 2010. STEMI patients were stratified as diabetic or nondiabetic based on past medical history and medications. The results are presented as percentages for categorical variables and analysed using Pearson χ2 test or Fisher’s Exact test, as appropriate. Continuous normally distributed variables are expressed as mean ± one standard deviation (SD) and compared with Student’s two-tailed unpaired t-test. Continuous non-normally distributed variables are expressed as median and interquartile range and analysed by Mann–Whitney U test. A probability value of p<0.05 was considered significant. To assess the independent predictors of in-hospital mortality, the following variables were considered for multivariate logistic regression analyses: admission year; age; sex; systolic blood pressure; heart rate; history of arterial hypertension; history of hyperlipidaemia; current smoking status; Killip class >II; thrombolysis (‘no reperfusion’ as reference category); and primary percutaneous coronary intervention (PCI) (‘no reperfusion’ as reference category). The multivariate logistic regression models were computed using backwards elimination with a significance level of 0.05. For temporal trend analyses, percentages of 1997 were compared with those from 2010 using univariate logistic regression models. IBM SPSS version 20 (SPSS, Chicago, IL, USA) was used for all statistical analyses.
Adherence to EBT was assessed by means of a score (with values ranging from 1 to 8) based on whether or not eight therapies (each being assigned 1 point) were administered at any time point during hospital stay: aspirin, clopidogrel in patients undergoing PCI, glycoprotein IIb/IIIa receptor (GP IIb/IIIa) antagonists in patients undergoing PCI, beta-blockers, angiotensin-converting enzyme inhibitors or angiotensin II antagonists, statins, heparin or low-molecular-weight heparin, and reperfusion therapy with either thrombolysis or primary PCI.
Results
Impact of diabetes mellitus on outcomes
During the analysed period, a total of 34,772 patients with ACS were enrolled in the registry and 19,977 of them presented with STEMI. Among the STEMI population, 15,531 patients were classified as nondiabetic and 3565 patients as diabetic. There were 881 patients (4.4%) excluded from the analysis because diabetic status was missing. Baseline characteristics of the nondiabetic and diabetic cohorts are reported in Table 1. In essence, diabetic patients were older, had a higher prevalence of additional cardiovascular risk factors other than smoking, exhibited a longer delay between symptom onset and hospital admission, presented less frequently with chest pain but more often with dyspnoea, were in higher Killip class at presentation, and had more frequently atrial fibrillation. In addition, diabetic patients had more frequently known coronary artery disease and comorbidities such as cerebrovascular disease, peripheral arterial disease, and renal disease. With respect to early drug therapy (i.e. within 24 hours of admission), diabetic patients received less frequently aspirin, clopidogrel, glycoprotein IIb/IIIa receptor inhibitors, beta-blockers, and lipid-lowering agents (all p<0.001). Conversely, angiotensin-converting-enzyme inhibitors/angiotensin II receptor blockers and calcium channel blockers were more frequently administered in diabetic patients (p<0.001). In addition, diabetic patients received less frequently than nondiabetic individuals thrombolytic therapy (14.5 vs. 18.6%, p<0.001) and primary PCI (46.6 vs. 55.5%, p<0.001). Finally, diabetic patients had longer hospital stay (median 8.0 vs. 6.5 days, p<0.001).
Table 1.
Baseline characteristics according to diabetic status.
| Non-diabetics (n=15,531) | Diabetics (n=3565) | p-value | |
|---|---|---|---|
| Gender (n) | |||
| Male | 74.6 | 67.7 | <0.001 |
| Female | 25.4 | 32.3 | |
| Age (years) | |||
| Mean±SD | 63.8±13.6 | 68.1±12.1 | <0.001 |
| Median | 64 | 69 | |
| Pre-hospital events | |||
| Delay (min) (median, interquartile range)b | 195 (105–495) | 255 (121–720) | <0.001 |
| Cardiopulmonary resuscitation | 622/15,172 (4.1) | 146/3470 (4.2) | 0.780 |
| Cardioversion/defibrillation | 685/15,083 (4.5) | 113/3446 (3.3) | 0.001 |
| Signs and symptoms on admission | |||
| Pain | 13,336/15,136 (88.1) | 2844/3438 (82.7) | <0.001 |
| Dyspnoea | 3403/14,041 (24.2) | 1115/3210 (34.7) | <0.001 |
| Atrial fibrillation | 480/12,710 (3.8) | 186/2849 (6.5) | <0.001 |
| Killip classc | <0.001 | ||
| I | 12,280 (80.0) | 2301 (65.5) | |
| II | 2174 (14.2) | 738 (21.0) | |
| III | 489 (3.2) | 297 (8.5) | |
| IV | 414 (2.7) | 171 (4.9) | |
| Risk factors | |||
| Hypertension | 7398/15,037 (49.2) | 2532/3442 (73.6) | <0.001 |
| Dyslipidaemia | 7175/14,202 (50.5) | 1950/3121 (62.5) | <0.001 |
| Smoking (current) | 6441/14,664 (43.9) | 998/3225 (30.9) | <0.001 |
| Adiposis (BMI ≥30 kg/m2) | 1993/12,532 (15.9) | 840/2762 (30.4) | <0.001 |
| Comorbidities | |||
| Coronary artery disease | 4066/13,930 (29.2) | 1358/3226 (42.1) | <0.001 |
| Cerebrovascular diseasea | 457/10,882 (4.2) | 207/2434 (8.5) | <0.001 |
| Peripheral arterial diseasea | 341/10,882 (3.1) | 209/2434 (8.6) | <0.001 |
| Renal diseasea | 471/10,882 (4.3) | 274/2434 (11.3) | <0.001 |
Values are n/total (%) unless otherwise stated.
Data available since 2005. BMI = body mass index.
data on the delay between symptom onset and hospital admission available for 13,389 nondiabetics and 2870 diabetics.
Information on Killip class available for 15,357 nondiabetics and 3507 diabetics.
With respect to in-hospital outcomes, diabetic patients had almost double in-hospital mortality as well as cardiogenic shock rates than nondiabetic individuals. The difference in reinfarction, stroke, and MACCE rates were also statistically significant (Table 2). In multivariate analysis, diabetes was identified as predictor of mortality (OR 1.23, 95% CI 1.03–1.46, p=0.022) and of MACCE (OR 1.22, 95% CI 1.05–1.42, p=0.009).
Table 2.
In-hospital outcomes according to diabetes status.
| Non-diabetics (n=15,531) | Diabetics (n=3565) | p-value | |
|---|---|---|---|
| Cardiogenic shock | 1043/15,385 (6.8) | 431/3526 (12.2) | <0.001 |
| Reinfarction | 322/15,347 (2.1) | 114/3517 (3.2) | <0.001 |
| Stroke | 131/15,267 (0.9) | 53/3499 (1.5) | 0.001 |
| Death | 944/15,531 (6.1) | 431/3565 (12.1) | <0.001 |
| Death, reinfarction, or stroke | 1229/15,281 (8.0) | 514/3507 (14.7) | <0.001 |
Values are n/total (%).
With respect to temporal trends, both diabetic and nondiabetic individuals exhibited a significant reduction with respect to mortality, reinfarction, cardiogenic shock, and MACCE over time (Figure 1). Specifically, in-hospital mortality dramatically decreased in diabetic patients, from 19.9% in 1997 and 9.0% in 2010 (ptrend<0.001) with an age-adjusted annual mortality decrease of 6% (OR 0.94, 95% CI 0.91–0.96, p<0.001). Per additional admission year, a reduction in age-adjusted rate of reinfarction (OR 0.86, 95% CI 0.82–0.90, p<0.001), cardiogenic shock (OR 0.88, 95% 0.86–0.90, p<0.001), as well as MACCE (OR 0.92, 95% CI 0.90–0.94, p<0.001) was observed in diabetic patients.
Figure 1.
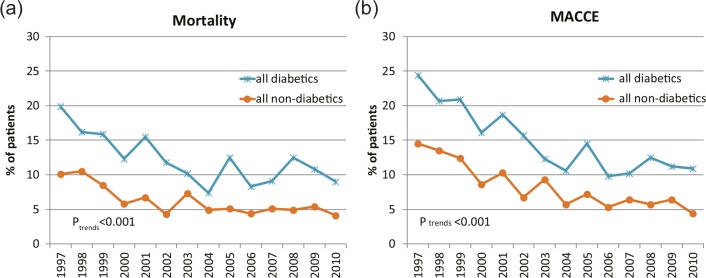
Trends in in-hospital mortality (a) and major adverse cardiac or cardiovascular events: death, reinfarction, or stroke (b) stratified for diabetes status.
Gender-related temporal trends in the outcomes of diabetic patients
Compared with diabetic males, diabetic females were older (mean age 73.0 years vs. 66.4 years), presented more frequently with dyspnoea, had more often atrial fibrillation, presented in more advanced Killip class, had more hypertension, and more frequently had a body mass index ≥30 kg/m2 but were less frequently current smokers (Table 3). With respect to comorbidities, women had less frequently pre-existing coronary artery disease than men while cerebrovascular, peripheral, and renal disease were equally distributed among genders. With respect to pharmacological treatment, diabetic females were significantly less frequently treated with clopidogrel, GP IIb/IIIa antagonists, beta-blockers, and lipid-lowering agents (all p<0.001). In addition, women with diabetes benefited less frequently from primary PCI than diabetic males (38.5 vs. 50.5%, p<0.001). Finally, diabetic women had longer hospital stay than men (median 9 vs. 7 days, p<0.001).
Table 3.
Baseline characteristics of the diabetic population stratified for gender.
| Male (n=2412) | Female (n=1153) | p-value | |
|---|---|---|---|
| Age (years) | |||
| Mean±SD | 66.4±11.7 | 73.0±11.6 | <0.001 |
| Median | 67 | 75 | |
| Pre-hospital events | |||
| Delay (min, median, interquartile range) (median, interquartilerange)b | 240 (120–650) | 300 (140–840) | |
| Cardiopulmonary resuscitation | 102/2351 (4.3) | 44/1119 (3.9) | 0.65 |
| Cardioversion/defibrillation | 88/2330 (3.8) | 25/1116 (2.2) | 0.018 |
| Signs and symptoms on admission | |||
| Pain | 1943/2335 (83.2) | 901/1103 (81.7) | 0.29 |
| Dyspnoea | 697/2162 (32.2) | 418/1048 (39.9) | <0.001 |
| Atrial fibrillation | 111/1943 (5.7) | 75/906 (8.3) | 0.011 |
| Killip class | |||
| I | 1632 (68.8) | 669 (58.9) | |
| II | 448 (18.9) | 290 (25.6) | |
| III | 177 (7.5) | 120 (10.6) | |
| IV | 115 (4.8) | 56 (4.9) | |
| Risk factors | |||
| Hypertension | 1640/2319 (70.7) | 892/1123 (79.4) | <0.001 |
| Dyslipidaemia | 1343/2137 (62.8) | 607/984 (61.7) | 0.55 |
| Smoking (current) | 793/2185 (36.3) | 205/1040 (19.7) | <0.001 |
| Adiposis (BMI ≥30 kg/m2) | 564/1923 (29.3) | 276/839 (32.9) | 0.065 |
| Comorbidities | |||
| Coronary artery disease | 954/2190 (43.6) | 404/1036 (39.0) | 0.015 |
| Cerebrovascular diseasea | 131/1651 (7.9) | 76/783 (9.7) | 0.16 |
| Peripheral arterial diseasea | 145/1651 (8.8) | 64/783 (8.2) | 0.64 |
| Renal diseasea | 175/1651 (10.6) | 99/783 (12.6) | 0.15 |
Values are n/total (%) unless otherwise stated.
Data available since 2005. BMI = body mass index.
data on the delay between symptom onset and hôpital admission available for 2001 diabetic males and 869 diabetic females.
Information on killip class available for 2372 diabetic males and 1135 diabetic females.
The delay between symptom onset and admission to hospital were significantly higher among diabetic patients than among nondiabetic individuals (median time 255 min vs. 195 min, p<0.001). Furthermore, diabetic females had longer delay between symptom onset and admission than males (median 300 min, interquartile range 140–840, vs. 240 min, 120–650). Over the years, the delays diminished among both diabetic and nondiabetic individuals (ptrend=0.035 and <0.001, respectively).
With respect to gender-related outcomes in the diabetic population, female patients had a significantly higher mortality (16.1 vs. 10.2%, p<0.001) as well as reinfarction, cardiogenic shock, and MACCE rates than nondiabetic individuals (Table 4). While among nondiabetic patients, both genders showed a significant mortality reduction over the study period (ptrend<0.001), a benefit was observed among diabetic males (ptrend=0.006) but not females (ptrend=0.082).
Table 4.
In-hospital outcomes of diabetic patients according to gender.
| Male (n=2412) | Female (n=1153) | p-value | |
|---|---|---|---|
| Cardiogenic shock | 259/2384 (10.9) | 172/1142 (15.1) | 0.001 |
| Reinfarction | 63/2378 (2.6) | 51/1139 (4.5) | 0.006 |
| Stroke | 30/2363 (1.3) | 23/1136 (2.0) | 0.103 |
| Death | 245/2412 (10.2) | 186/1153 (16.1) | <0.001 |
| Death, reinfarction, or stroke | 297/2368 (12.5) | 217/1139 (19.1) | <0.001 |
Values are n/total (%).
The gender-stratified analysis of temporal trends showed a benefit in diabetic men (ptrend<0.001 for reinfarction, cardiogenic shock, and MACCE), in diabetic women the benefit over time reached statistic significance for cardiogenic shock (ptrend<0.001) and MACCE (ptrend<0.04) but not for reinfarction (ptrend<0.055) (Figure 2).
Figure 2.
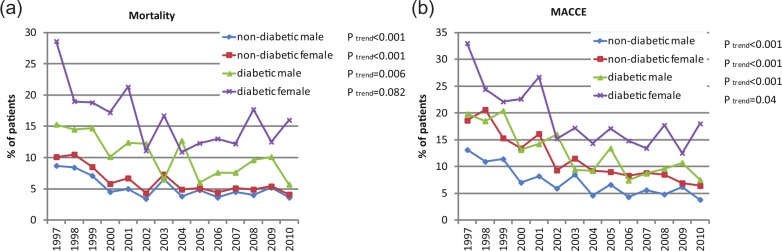
Trends in in-hospital mortality (a) and major adverse cardiac or cardiovascular events: death, reinfarction or stroke (b) stratified for diabetes status and gender.
Diabetic women had higher mortality (16.1 vs. 10.2%, p<0.001) and MACCE (19.1 vs. 12.5%, p<0.001) rates than diabetic men and within the diabetic population female gender was identified as independent predictor of mortality (OR 1.45, 95% CI 1.07–1.96, p=0.015) and MACCE (OR 1.44, 95% CI 1.10–1.88, p=0.007) (Table 5).
Table 5.
Multivariate analysis for predictors of in-hospital mortality and major cardiac and cerebrovascular events (death, reinfarction or stroke) in diabetic patients.
| Odds ratio (95% CI) | p-value | |
|---|---|---|
| Mortality | ||
| Age (per additional year) | 1.05 (1.04–1.07) | <0.001 |
| Gender | 1.45 (1.07–1.96) | 0.015 |
| Killip class >II | 3.35 (2.41–4.68) | <0.001 |
| Systolic blood pressure (per mmHg increase) | 0.98 (0.97–0.98) | <0.001 |
| Heart rate (per beat/min increase) | 1.01 (1.00–1.01) | 0.009 |
| Primary reperfusion | 0.54 (0.39–0.75) | <0.001 |
| MACCE | ||
| Age (per additional year) | 1.04 (1.03–1.06) | <0.001 |
| Gender | 1.44 (1.10–1.88) | 0.007 |
| Killip class >II | 3.09 (2.28–4.20) | <0.001 |
| Systolic blood pressure (per mmHg increase) | 0.98 (0.98–0.99) | <0.001 |
| Heart rate (per beat/min increase) | 1.01 (1.00–1.01) | 0.002 |
| Primary reperfusion | 0.71 (0.39–0.75) | 0.014 |
Use of evidence-based therapy
Diabetic patients had an overall lower EBT-adherence score than nondiabetic individuals (5.5±1.9 vs. 5.8±1.7, p<0.001), despite a significant improvement over time (from 2.9±1.3 in 1997 to 5.8±1.6 in 2010, ptrend<0.001). Despite an improvement over time for both males (from 3.1±1.2 in 1997 to 6.0±1.4 in 2010, ptrend<0.001) and females (from 2.6±1.3 in 1997 to 5.4±1.9 in 2010) (ptrend<0.001), diabetic females had an lower EBT-adherence score than diabetic males (5.1±1.9 vs. 5.6±1.8, p<0.001). Although the use of reperfusion therapy (thrombolysis or primary PCI) in diabetic patients increased from 42.3% in 1997 to 74.4% in 2010 (ptrend<0.001), it still remained significantly lower compared with nondiabetic individuals even after adjusting for age (OR 0.93, 95% CI 0.92–0.94, p<0.001). Within the diabetic population, independent predictors of both in-hospital mortality and MACCE included age, gender, advanced Killip class, hypotension, and tachycardia, while primary reperfusion was the only independent protective factor (Table 5). With respect to gender, the increase in reperfusion therapy over the years was observed in both male and females (ptrend<0.001 for both). Nevertheless, even after adjusting for age, the overall use of primary reperfusion was significantly lower among diabetic women than males (OR 0.83, CI 0.71–0.96, p =0.015).
Discussion
The present study analysed gender related in-hospital outcomes and trends over a 14-year period extending up to the year 2010 in a large diabetic STEMI population of Switzerland. The first major finding is that the in-hospital mortality dramatically decreased over time in diabetic patients, as demonstrated by a 6% age-adjusted mortality decrease per each additional admission year. Despite the encouraging observation, a nearly 2-fold mortality as well as MACCE rates persisted among diabetic patients compared with nondiabetic individuals. In addition, diabetes status independently predicted both mortality and MACCE in the overall STEMI population. Finally, although the administration of EBT improved over time for both diabetic and nondiabetic individuals, diabetic patients received less frequently EBT than nondiabetic counterparts. In particular, the rate of reperfusion in diabetic patients remained lower than in nondiabetic individuals.
The second main finding is that diabetic women had worse outcomes than male counterparts in terms of both in-hospital mortality and MACCE. In addition, while the decrease in mortality over time reached statistical significance in diabetic males, it did not in diabetic females. Moreover, female gender was identified as independent predictor of both mortality and MACCE within the diabetic cohort. Finally, diabetic women received less frequently EBT – notably reperfusion therapy – than man. Overall, the analysis shows that, in the setting of STEMI, female gender adds to the mortality and morbidity risk conferred by diabetes and that, among diabetic women, the risk is barely decreasing over time while EBT remain markedly underused.
The unfavourable outcomes we observed among diabetic patients compared with nondiabetic individuals in the setting of STEMI parallel previous findings in both the ACS clinical trial and registry settings.6,7 However, data on trends in mortality of diabetic patients presenting with STEMI were so far limited. A report from the USA using the Nationwide Inpatient Sample described an increase in age-adjusted in-hospital mortality between 1988 and 1996 followed by a decrease between 1996 and 2004.10 Other reports showing a decrease in mortality for diabetic patients in the STEMI setting were limited by the small numbers of patients included.11 Even sparser were the observations on gender-related trends in outcomes within the diabetic population. A gap in outcomes between diabetic women and men suffering myocardial infarction has been described in the Worcester Heart Attack Study which identified female gender, as in our analysis, to be an independent predictor of in-hospital mortality.12 Those findings could not be replicated in recent European reports limited by the small populations studied.13,14
We documented that diabetic patients received less frequently EBT, namely antiplatelet agents, beta-blockers, lipid-lowering agents (data not shown) as well as reperfusion therapy than nondiabetic counterparts. The reasons for those findings remain speculative. With respect to antiplatelet agents, the observed underuse may possibly reflect the perceived but unproven unfavourable risk/benefit ratio in this patient population. Accordingly, although diabetic patients with ACS are at increased risk of bleeding compared to nondiabetic counterparts,15 at the same time they derive greater benefit from potent antiplatelet agents such as GP IIb/IIIa inhibitors or prasugrel.5,16
The underuse of EBT in the diabetic population has been documented also in the Swedish Heart Intensive care Admissions (RIKS-HIA) registry.7 In a multivariate analysis including all patients admitted to coronary care units at 58 hospitals during 3 years for myocardial infarction, patients with diabetes (n=5193) were significantly less likely to be treated with reperfusion therapy, heparins, and statins. Similarly, the Can Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines (CRUSADE) quality improvement initiative, including 46,410 ACS patients in the USA, found that insulin-treated diabetic patients with ACS were less likely than nondiabetic counterparts to receive antithrombotic agents, beta-blockers, and cardiac catheterization.17 In addition, the Euro Heart Survey on Diabetes and the Heart including 3488 patients showed that, after correcting for imbalances in baseline characteristics with multivariate analysis, diabetic patients received less frequently evidence-based pharmacotherapy and reperfusion therapy than nondiabetic ones.18 Finally, a pooled analysis of mainly US-based ACS trials including a total of 10,163 diabetic patients showed, compared with nondiabetic individuals, lower prescription rates for aspirin, beta-blockers, and fibrinolytic therapy but not for thienopyridines, GP IIb/IIIa antagonists, or lipid-lowering agents.6
Limitations
The weaknesses of the AMIS Plus registry are limitations common to all registries. Participation in the AMIS Plus registry is voluntary; the number of hospitals varied and might therefore not be entirely representative of all hospitals in Switzerland despite the fact that more than 60% of the hospitals admitting ACS patients participated. In addition, although the registry requires enrolment of all consecutive patients at participating, selection biases cannot be excluded. The possibility of inaccuracies in data entry cannot be totally ruled out and may thus create unrecognized biases. Although individual on-site auditing at the participating centers was performed only sporadically, data questionnaires were continuously and carefully checked by the data management centre. The limited resources of the AMIS Plus registry do not allow for systematic site visits and audits or very large questionnaires. Important variables potentially influencing in-hospital mortality such as time from symptom onset to reperfusion, bleedings, extent of coronary artery disease, and patency of infarct-related artery were not available for a sizable proportion of patients because they were collected only at a later phase of the AMIS Plus experience. Therefore, those variables were not included in the analysis. In addition, there were no assessments of clinical eligibility for each drug class and thus failure to administer a certain drug may reflect a contraindication for the use. Moreover, the time point of drug administration was not recorded. In addition, important parameters like blood glucose on admission, fasting blood glucose, or haemoglobin A1c were not systematically collected. Finally, the components of the EBT were chosen according to current standards and were weighted equally, although the evidence for the individual components may be different and have changed over time. Despite all the mentioned limitations, the AMIS Plus database is sizable for a small country like Switzerland, represents hospitals of various size and settings and offers recent data.
Conclusion
In conclusion, in-hospital mortality of diabetic STEMI patients in Switzerland improved dramatically over time. However, it remained twice as high as in nondiabetic individuals and no significant improvement over time could be detected among diabetic females. While diabetes was found to be an independent predictor of in-hospital mortality in the overall population, the same was true for female gender within the diabetic cohort. The delay from symptom onset to hospital admission as well as the use of EBT – and specifically of reperfusion therapy – improved over time in the diabetic population but remained lower than in nondiabetic patients, particularly in females. This might have contributed to the less favourable outcomes observed in female diabetic patients.
Acknowledgments
Dr Marco Roffi and Dr Dragana Radovanovic had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. The authors gratefully thank Professor Burkhardt Seifert from the Institute of Social and Preventive Medicine, Zurich, for his assistance with the statistical analysis.
The AMIS Plus registry is supported by the Swiss societies of cardiology, internal medicine, and intensive care medicine
The AMIS Plus registry is funded by unrestricted grants from the Swiss Heart Foundation and from Abbot AG, Astra-Zeneca AG, Bayer Shering, Biotronik AG, Bristol-Myers Squibb AG, Daiichi-Sankyo/Lilly AG, Johnson & Johnson – Cordis Division, A Menarini, Merck Sharp & Dohme-Chibret, Medtronic, Pfizer, St. Jude Medical, Takeda Pharma, all in Switzerland. This support is gratefully acknowledged
The authors would like to express their gratitude to the teams of following hospitals (listed in alphabetical order and with mention of the local principal investigator): Aarau, Kantonsspital (P Lessing), Affoltern am Albis, Bezirkspital (F Hess), Altdorf, Kantonsspital (R Simon), Altstätten, Kantonales Spital (PJ Hangartner), Baden, Kantonsspital (U Hufschmid), Basel, Kantonsspital (P Hunziker), Basel, St. Claraspital (C Grädel), Bern, Beau-Site Klinik (A Schönfelder), Bern, Inselspital (S Windecker), Biel, Spitalzentrum (H Schläpfer), Brig-Glis, Oberwalliser Kreisspital (D Evéquoz), Bülach, Spital (G Mang), Burgdorf, Regionalspital Emmental (D Ryser), Chur, Rätisches Kantons- und Regionalspital (P Müller), Chur, Kreuzspital (R Jecker), Davos, Spital (W Kistler), Dornach, Spital (A Droll/T Hongler), Einsiedeln, Regionalspital (S Stäuble), Flawil, Spital (G. Freiwald), Frauenfeld, Kantonsspital (HP Schmid), Fribourg, Hôpital cantonal (JC Stauffer), Frutigen, Spital (K Bietenhard), Genève, Hôpitaux universitaires (JM Gaspoz / PF Keller), Glarus, Kantonsspital (W. Wojtyna), Grenchen, Spital (B Oertli/R Schönenberger), Grosshöchstetten, Bezirksspital (C Simonin), Heiden, Kantonales Spital (R Waldburger), Herisau, Kantonales Spital (M Schmidli), Interlaken, Spital (EM Weiss), Jegenstorf, Spital (H Marty), Kreuzlingen, Herzzentrum Bodensee (K Weber), La Chaux-de-Fonds, Hôpital (H Zender), Lachen, Regionalsspital (C Steffen), Langnau im Emmental, Regionalspital (A Hugi), Laufenburg, Gesundheitszentrum Fricktal (J Frei/E Koltai), Lugano, Cardiocentro Ticino (G Pedrazzini), Luzern, Kantonsspital (P Erne), Männedorf, Kreisspital (T Heimes), Martigny, Hôpital régional (B Jordan), Mendrisio, Ospedale regionale (A Pagnamenta), Meyrin, Hôpital de la Tour (P Urban), Monthey, Hôpital du Chablais (P Feraud), Montreux, Hôpital de Zone (E Beretta), Moutier, Hôpital du Jura bernois (C Stettler), Münsingen, Regionales Spital Zentrum (F Repond), Münsterlingen, Kantonsspital (F Widmer), Muri, Kreisspital für das Freiamt (C. Heimgartner), Nyon, Group. Hosp. Ouest lémanique (R Polikar), Olten, Kantonsspital (S Bassetti), Rheinfelden, Gesundheitszentrum Fricktal (HU Iselin), Rorschach, Kantonales Spital (M Giger), Samedan, Spital Oberengadin (P Egger), Sarnen, Kantonsspital Obwalden (T Kaeslin), Schaffhausen, Kantonsspital (R Frey), Schlieren, Spital Limmattal (T Herren/B Caduff), Schwyz, Spital (P Eichhorn), Scuol, Ospidal d’Engiadina Bassa (C Neumeier/G Flury), Solothurn, Bürgerspital Solothurn (A Grêt/R Schönenberger), St. Gallen, Kantonsspital (H Rickli), Sursee, Spital (S Yoon), Tiefenau, Tiefenauspital (P Loretan), Thun, Spital (U Stoller), Thusis, Krankenhaus (UP Veragut), Uster, Spital (E Bächli), Uznach, Kantonales Spital (A Weber), Wädenswil, Schwerpunktspital Zimmerberg-Horgen (B Federspiel), Walenstadt, Kantonales Spital (D Schmidt/J Hellermann), Wetzikon, GZO Spital (M Graber), Winterthur, Kantonsspital (A Fischer), Wolhusen, Kantonales Spital (M Peter), Zofingen, Spital (S Gasser), Zollikerberg, Spital (R Fatio), Zug, Kantonsspital (M Vogt/D Ramsay), Zürich, Klinik im Park (O Bertel), Zürich, Universitätsspital Zürich (M Maggiorini), Zürich, Stadtspital Triemli (F Eberli), Zürich, Stadtspital Waid (M Fischler/S Christen).
References
- 1. Danaei G, Finucane MM, Lu Y, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 2011; 378: 31–40 [DOI] [PubMed] [Google Scholar]
- 2. Bhatt DL, Roe MT, Peterson ED, et al. Utilization of early invasive management strategies for high-risk patients with non-ST-segment elevation acute coronary syndromes: results from the CRUSADE Quality Improvement Initiative. JAMA 2004; 292: 2096–2104 [DOI] [PubMed] [Google Scholar]
- 3. Roe MT, Parsons LS, Pollack CV, et al. Quality of care by classification of myocardial infarction: treatment patterns for ST-segment elevation vs non-ST-segment elevation myocardial infarction. Arch Intern Med 2005; 165: 1630–1636 [DOI] [PubMed] [Google Scholar]
- 4. Bartnik M, Ryden L, Ferrari R, et al. The prevalence of abnormal glucose regulation in patients with coronary artery disease across Europe. The Euro Heart Survey on diabetes and the heart. Eur Heart J 2004; 25: 1880–1890 [DOI] [PubMed] [Google Scholar]
- 5. Roffi M, Chew DP, Mukherjee D, et al. Platelet glycoprotein IIb/IIIa inhibitors reduce mortality in diabetic patients with non-ST-segment-elevation acute coronary syndromes. Circulation 2001; 104: 2767–2771 [DOI] [PubMed] [Google Scholar]
- 6. Donahoe SM, Stewart GC, McCabe CH, et al. Diabetes and mortality following acute coronary syndromes. JAMA 2007; 298: 765–775 [DOI] [PubMed] [Google Scholar]
- 7. Norhammar A, Malmberg K, Ryden L, et al. Under utilisation of evidence-based treatment partially explains for the unfavourable prognosis in diabetic patients with acute myocardial infarction. Eur Heart J 2003; 24: 838–844 [DOI] [PubMed] [Google Scholar]
- 8. Preis SR, Hwang SJ, Coady S, et al. Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the Framingham Heart Study, 1950 to 2005. Circulation 2009; 119: 1728–1735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Radovanovic D, Erne P. AMIS Plus: Swiss registry of acute coronary syndrome. Heart 2010; 96: 917–921 [DOI] [PubMed] [Google Scholar]
- 10. Movahed MR, John J, Hashemzadeh M, et al. Trends in the age adjusted mortality from acute ST segment elevation myocardial infarction in the United States (1988–2004) based on race, gender, infarct location and comorbidities. Am J Cardiol 2009; 104: 1030–1034 [DOI] [PubMed] [Google Scholar]
- 11. Cubbon RM, Wheatcroft SB, Grant PJ, et al. Temporal trends in mortality of patients with diabetes mellitus suffering acute myocardial infarction: a comparison of over 3000 patients between 1995 and 2003. Eur Heart J 2007; 28: 540–545 [DOI] [PubMed] [Google Scholar]
- 12. Crowley A, Menon V, Lessard D, et al. Sex differences in survival after acute myocardial infarction in patients with diabetes mellitus (Worcester Heart Attack Study). Am Heart J 2003; 146: 824–831 [DOI] [PubMed] [Google Scholar]
- 13. Meisinger C, Heier M, von Scheidt W, et al. Gender-Specific short and long-term mortality in diabetic versus nondiabetic patients with incident acute myocardial infarction in the reperfusion era (the MONICA/KORA Myocardial Infarction Registry). Am J Cardiol 2010; 106: 1680–1684 [DOI] [PubMed] [Google Scholar]
- 14. Venskutonyte L, Malmberg K, Norhammar A, et al. Effect of gender on prognosis in patients with myocardial infarction and type 2 diabetes. J Intern Med 2010; 268: 75–82 [DOI] [PubMed] [Google Scholar]
- 15. Subherwal S, Bach RG, Chen AY, et al. Baseline risk of major bleeding in non-ST-segment-elevation myocardial infarction: the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA Guidelines) Bleeding Score. Circulation 2009; 119: 1873–1782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wiviott SD, Braunwald E, Angiolillo DJ, et al. Greater clinical benefit of more intensive oral antiplatelet therapy with prasugrel in patients with diabetes mellitus in the trial to assess improvement in therapeutic outcomes by optimizing platelet inhibition with prasugrel – Thrombolysis in Myocardial Infarction 38. Circulation 2008; 118: 1626–1636 [DOI] [PubMed] [Google Scholar]
- 17. Brogan GX, Peterson ED, Mulgund J, et al. Treatment disparities in the care of patients with and without diabetes presenting with non-ST-segment elevation acute coronary syndromes. Diabetes Care 2006; 29: 9–14 [PubMed] [Google Scholar]
- 18. Anselmino M, Malmberg K, Ohrvik J, et al. Evidence-based medication and revascularization: powerful tools in the management of patients with diabetes and coronary artery disease: a report from the Euro Heart Survey on diabetes and the heart. Eur J Cardiovasc Prev Rehabil 2008; 15: 216–223 [DOI] [PubMed] [Google Scholar]


