OVERVIEW
PI3K/AKT/mTOR pathway is an established oncogenic driver in humans. Targeted biologic agents against components of this pathway have shown promising activity leading to the approval of the allosteric inhibitors of mTOR, everolimus, and temsirolimus for the treatment of advanced cancers of the kidney, breast, and pancreas. Despite the established and promising activity of this therapeutic strategy, the duration and quality of benefit remains suboptimal in unselected patients. Improved understanding of the biologic consequence of altered PI3K/AKT/mTOR signaling is informing the development of protein (phosphorylated forms of S6, AKT, eIF4e) and genetic (PIK3CA mutation, PTEN loss of function, TSC1 and TSC2 mutation, PIK3CA-GS genetic profile) biomarkers to identify patients most likely to benefit from this therapeutic strategy. This review provides an overview of the biologic rational and promising results of protein and genetic biomarkers for selecting patients appropriate for therapy with inhibitors of this pathway.
PHOSPHOINOSITIDE 3-KINASE, AKT, AND MAMMALIAN TARGET OF RAPAMYCIN SIGNALING PATHWAY
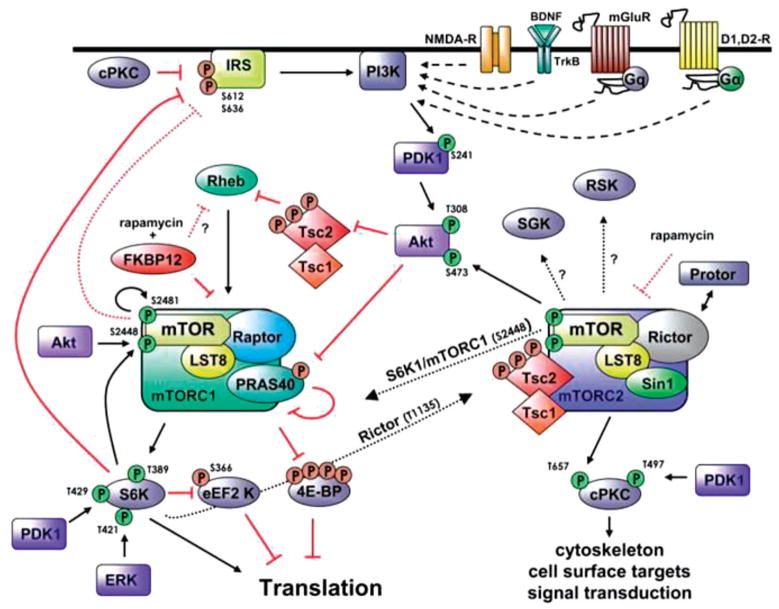
The PI3K/AKT/mTOR signaling pathway has been well characterized and recognized to play essential roles in normal cellular functions including nutrition and energy balance, protein synthesis, and growth control in mammalian cells. Eight classes of PI3K kinases have been described in mammalian cells, but only the class I product that can function as second-messenger in intracellular signaling has been implicated in oncogenesis. The class I PI3K protein consists of two main subunits of different sizes, p85 and p110, which, respectively, mediate regulatory and catalytic activity of the enzymes. There are three different isoforms of the p110 catalytic subunit: p110α, β, and δ, encoded by their specifıc genes, PIK3CA, PIK3CB, and PIK3CD. The p85 regulatory subunit is encoded by three genes: PIK3R1, PIK3R2, and PIK3R3. The PI3K family of lipid and protein kinases is activated by receptor-associated tyrosine kinases and phosphorylate the 3′-hydroxyl group of phosphoinositides to generate phoshatidylinositol-3,4,5-trisphosphate (PIP3).1–3 PIP3 is an important second messenger that signals through AKT to downstream activators of cellular growth and survival, whereas PTEN acts as a negative regulator of PIP3 activity by catalyzing its dephosphorylation. Figure 1 provides a schematic illustration of the interaction and regulation of the PI3K/AKT/mTOR pathway protein members.
FIG 1.
PI3K/AKT/mTOR signaling pathway showing interacting activation and regulatory feedback loops. Adapted from Hoeffer and Klann.35
Mammalian target of rapamycin (mTOR) is a serinethreonine kinase that is amaster regulator of protein synthesis, along with its important roles in other biologic processes such as cell growth and survival. mTOR activity in the cell is carried out by two distinct complexes. mTORC1 complex is made up of mTOR, raptor, mLST8, and PRAS40. It is very sensitive to rapamycin and activates S6K and inactivates 4E-BP1, leading to protein translation and cell growth. mTORC2 complex is composed of mTOR, rictor, Sin1, and mLST8. It is less sensitive to rapamycin, and its role in normal cell function and oncogenesis has not been well elucidated. However, it is known to activate AKT, thereby promoting cell proliferation and survival. The canonical pathway of mTOR activation depends on mitogen-driven signaling through PI3K/AKT, although alternative non-AKT dependent activation through the Ras/MEK/ERK pathway is now recognized.4
ESTABLISHED AND EMERGING THERAPEUTIC ANTICANCER AGENTS TARGETING THE PI3K/AKT/MTOR PATHWAY
Randomized phase III studies have confırmed the effıcacy of agents targeting the PI3K/AKT/mTOR axis, leading to the approval of mTOR inhibitors, everolimus, and temsirolimus, for an increasing array of solid malignancies including renal cell carcinoma, hormone refractory breast cancer, pancreatic neuroendocrine cancer, and subependymal giant cell astrocytoma (Table 1). Temsirolimus binds to an intracellular protein, FKBP-12, to form an inhibitory complex that abrogates mTOR signaling. In a phase III study in poor-risk advanced kidney cancer, 626 patients were randomized to receive interferon-alpha alone, temsirolimus alone, or the combination of both agents.5 Temsirolimus showed superior overall survival (OS) over interferon alone (HR: 0.73; 95% CI: 0.58–0.92; p = 0.008), whereas the 2-drug combination failed to show any additional benefıt to patients treated with IFN-α (HR: 0.96; 95% CI: 0.76–1.20; p = 0.70). The median OS for interferon alone, temsirolimus alone, and the 2-drug combination were 7.3, 10.9, and 8.4 months, respectively. The outcome of this study was the basis for the FDA approval of temsirolimus for advanced poor-risk kidney cancer.
TABLE 1.
Pivotal Clinical Trials Leading to Regulatory Approval of PI3K/AKT/mTOR Inhibitors
| Study | Regimen/Design | N | PFS or RR | OS | Indication |
|---|---|---|---|---|---|
| Hudes et al.5 | IFN-alpha versus temsirolimus versus temsirolimus + IFN-alpha 1:1:1 randomization | 626 | 1.9 versus 3.8 versus 3.7 mo | 0.73; (95% CI: 0.58 to 0.92); p = 0.008 | Advanced RCC with poor prognosis |
| Baselga et al.6 | Everolimus + exemestane versus exemestane 2:1 randomization | 724 | HR: 0.36; (95% CI: 0.27–0.47); p < 0.001 10.6 versus 4.1 mo | Immature data | Hormone-receptor (+) advanced breast cancer patients following failure of a nonsteroidal aromatase inhibitor |
| Motzer et al.8 | Everolimus versus placebo 2:1 randomization | 410 | 0.30 (95% CI:0.22–0.40, p < 0.0001); 4.0 versus 1.9 | NR | Metastatic RCC previously treated with sunitinib, sorafenib, or both |
| Bissler et al.11 | Everolimus versus placebo; 2:1 randomization | 118 | Response rate difference 42% [24–58%]; p < 0.0001 | NR | Angiomyolipoma (sporadic and TSC-associated) |
| Franz et al.10 | Everolimus versus placebo; 2:1 randomization | 117 | RR difference 35% (95% CI: 15–52; p < 0.0001) | NR | Subependymal giant cell astrocytomas associated with TSC |
| Yao et al.7 | Everolimus versus placebo 1:1 randomization | 410 | 0.35 (95% CI:0.27–0.45; p < 0.001) 11.0 versus 4.6 mo | 1.05 (95% CI: 0.71–1.55; p = 0.59 | Low/intermediate-grade advanced pancreatic neuroendocrine tumor |
Everolimus is one of the most investigated mTOR inhibitor to date and has received regulatory approval for various tumor types. In a phase III study in patients with breast cancer previously treated with nonsteroidal hormone therapy, 724 patients randomized to receive everolimus plus exemestane or exemestane plus placebo were compared for progression free survival (PFS). At preplanned interim analysis, the everolimus-containing arm was superior, with median PFS of 6.9 months versus 2.8 months (HR: 0.43; 95% CI: 0.35–0.54; p<0.001) by investigator assessment and 10.6 months versus 4.1 months (HR: 0.36; 95% CI: 0.27–0.47; p < 0.001) by central review.6
The RADIANT3 study randomized 410 patients with advanced, progressing, low-grade, or intermediate-grade pancreatic neuroendocrine tumors to everolimus or placebo. There was signifıcant clinical benefıt of everolimus therapy, evidenced by amedian PFS of 11.0 months versus 4.6 months with placebo (HR: 0.35; 95% CI: 0.27–0.45; p < 0.001).7 Based on these positive results, everolimus is now approved for the treatment of this disease.
Similarly, 410 patients with metastatic renal cell carcinoma previously treated with antiangiogenic agents were randomized to receive everolimus or placebo in conjunction with best supportive care. The study was terminated after a specifıed interim analysis demonstrated a signifıcant PFS benefıt in favor of everolimus (median PFS of 4.0 months [95% CI: 3.7–5.5] vs. 1.9 months [1.8–1.9] months; HR: 0.30, 95% CI: 0.22–0.40, p < 0.0001).8
Tuberous sclerosis complex (TSC) is amultisystem disease mediated by autosomal dominant genetic mutations in TSC1 (hamartin) and TSC2 (tuberin) genes. The disorder is characterized by benign hamartomatous growths in different organs, most commonly skin, brain, kidney, lung, heart, and retina. The TSC genes encode a tumor-suppressor complex that controls activation of the mTOR pathway through the Ras homolog enriched in brain (RHEB) protein. Loss of this suppressor activity as a result of mutation in either TSC1 or TSC2 allows for constitutive signaling and activation of the mTOR pathway, leading to abnormal cellular growth, proliferation, and protein synthesis.9 Elucidation of the TSC1 signaling cascade and its role as a critical node that negatively modulates the propagation of signals from upstream PI3K and AKT to the mTOR complex informed the clinical evaluation of mTOR inhibitors in patient groups with symptomatic manifestations of the TSC. The EXIST-1 study randomized 78 pediatric and adult patients with progressive or symptomatic subependymal giant cell astrocytoma to everolimus and 39 to placebo. Objective response (minimum of 50% reduction in tumor volume) was seen in 35% of patients in the everolimus group compared with 0% in the placebo group (difference 35%, 95% CI: 15–52; p<0.0001).10 In the EXIST-2 study, patients 18 years or older with angiomyolipoma measuring at least 3 cmor larger in diameter (defıned by radiological assessment) in the setting of a defınite TSC diagnosis or sporadic lymphangioleiomyomatosis were assigned to oral everolimus (79 patients) or placebo (39 patients). Similar to the EXIST-1 study, patients treated with everolimus achieved a response rate of 42% (95% CI 31% to 53%) versus 0% for placebo (response rate difference 42% [24% to 58%]; p < 0.0001).11 Everolimus received FDA approval for the treatment of these TSC-associated diseases based on the positive outcome of these studies.
Many other agents currently in preclinical and clinical evaluation specifıcally target PI3K or the AKT protein (Table 2). Although encouraging activity against various cancer types has been recorded, none of these agents has demonstrated suffıcient effıcacy for regulatory approval.
TABLE 2.
Inhibitors of PI3K/AKT/mTOR Pathway in Development
| Class | Compound | Target Selectivity | Stage in Development |
|---|---|---|---|
| PI3K | |||
| AZD6482 | PI3Kβ | Preclinical | |
| AR245408 (XL147) | Pan PI3K | Phase I | |
| PX-866 | Pan PI3K | Phase II | |
| BKM120 | Pan PI3K | Phase II | |
| GDC-0980 | PI3K/mTOR | Phase II | |
| GDC-0941 | PI3K | Phase II | |
| BYL719 | PIK3α | Phase II | |
| PF-04691502 | PI3K/mTOR | Phase II | |
| GSK2636771 | PIK3β | Phase II | |
| BAY 80–6946 | PIK3 | Phase I | |
| ONC-01910 | PI3K and Plk1 | Phase III | |
| AKT | |||
| MK-2206 | AKT | Phase II | |
| VIII | AKT 1 &2 | Preclinical | |
| AZD5363 | Pan AKT | Phase I | |
| Triciribine (API-2) | Akt 1, 2, 3 | Phase I | |
| SR13668 | Akt | Preclinical | |
| AR-67 (DB-67) | Akt | Phase I, II | |
| AR-42 | Akt | Preclinical | |
| GSK690693 | Akt1, 2, 3 | Phase I | |
| KP372–1 | Akt, PDK-1, Flt3 | Preclinical | |
| VQD-002 (API-2) | Akt | Phase I, II | |
| A-443654 | Akt | Preclinical | |
| mTOR | |||
| Rapamycin (Sirolimus) | mTORC1 | FDA approved (non Oncology) Phase II | |
| Everolimus | Allosteric TORC1/2 inhibitor | FDA Approved | |
| Temsirolimus | FKBP-12 | FDA approved | |
| Ridaforolimus | Allosteric TORC1/2 inhibitor | Phase III | |
| NVP-BEZ235 | PIK3/mTOR | Phase II | |
| BGT226 | PIK3/mTOR | Phase II | |
| WYE-354 | mTOR ATP competitive | Preclinical | |
| AZD-8055 | mTORC1/mTORC2 | Phase I, II | |
| OSI-027 | mTORC1/mTORC2 | Phase I | |
| INK-128 | mTORC1/mTORC2 | Phase I | |
| PP-242 | mTORC1/mTORC2 | Phase I | |
| ONC-01910 | Non-ATP Plk1 and PI3K | Phase III | |
BIOMARKERS OF EFFICACY AND RESISTANCE
Genetic Biomarkers
Germline loss or acquired somatic mutations in the mammalian phosphatase and tensin homolog (PTEN) gene locus on chromosome 10q are among the most common aberrations observed in solid malignancies.3,12 In addition, exon 9 (E542K and E545K) and exon 20 (H1047R) mutations of the phosphoinositide-3-kinase, catalytic, polypeptide (PIK3CA) gene also promote oncogenesis.13 Because tumors that harbor these genetic events have uncontrolled constitutively active PI3K enzyme, they are expected to be sensitive to agents targeting this pathway. Robust evidence supports the predictive capability of these genetic aberrations in preclinical models,14,15 but validation in the clinical setting remains limited and, at times, contradictory.16 The interplay between PTEN loss and activating PIK3CA is an interesting example of how a genetic alteration that predicts for sensitivity in one cancer type (endometrial cancer) may fail to predict for effıcacy in another (in breast cancer).16 Activating PIK3CA mutations or HER2 amplifıcation conferred remarkable sensitivity to inhibitors of the PI3K/Akt/mTOR such as BKM120, GDC-0941, everolimus and PP24237, whereas PTEN loss was not predictive in a panel of breast cancer cell lines. Combined presence of HER2 gene amplifıcation along with PIK3CA mutation was found to be highly predictive of sensitivity to GDC-0941.17 The reason for this observation may reside in differences in biologic consequences of each of these specifıc mutations. Although activating PIK3CA mutations and PTEN loss both result in PI3K/AKT/mTOR pathway activation, the downstream effects and the mediators recruited by these genetic alterations are dissimilar. For instance, PIK3CA-mutant tumors require p110-α activation to sustain cellular proliferation, which may occur through AKT or via PDK1 and its substrate SGK3.18 PTEN-defıcient cancer cells, on the other hand, depend on the kinase activity of p110-β, which is not suffıcient to induce sustained cellular proliferation.19 This difference is biologically relevant and demonstrates the need for careful patient and therapeutic agent selection for optimal clinical benefıt. This observation has informed the development of isoform-specifıc PI3K inhibitors and studies designed to evaluate them in PTEN-defıcient tumors.
Gene expression and protein data from approximately 1,800 patients with breast cancer were used to develop a PIK3CA mutation-associated gene signature (PIK3CA-GS). This signature predicted the PIK3CA mutation status in two independent datasets and also identifıed rapamycin-resistant cell lines in preclinical studies.20 The ability of this gene signature to estimate PI3K pathway activation was assessed in tumor samples from patients with breast cancer enrolled in two prospective neoadjuvant clinical trials of everolimus. Relative change from baseline to day 15 in Ki67 (a proliferative and prognostic marker in breast cancer) and pS6 was correlated with the baseline PIK3CA-GS profıle. Patients with the largest relative decreases in Ki67 following combined letrozole/everolimus therapy were identifıed (R = −0.43, p = 0.008) by the PIK3CA-GS profıle. In contrast, there was no signifıcant correlation between PIK3CA-GS profıle and Ki67 in the letrozole/placebo group (R = 0.07, p=0.58). Similarly, PIK3CA-GS profıle was inversely correlated (R=−0.46, p = 0.028) with relative change in pS6 in patients treated with single agent everolimus using an independent dataset obtained from patients enrolled in a neoadjuvant study of everolimus in surgically resectable breast cancer. Although there was no signifıcant correlation of the PIK3CA-GS profıle with any survival end point, the results indicate that the profıle outperforms PIK3CA genotyping as a marker of pathway activation and may be useful for identifying patients with breast and other types of cancer who are likely to respond to this therapeutic strategy.21
De novo and acquired genetically mediated treatment resistance
The existence of de novo resistance to inhibitors of the PI3K/AKT/mTOR pathway is indicated by the large number of patients treated on studies who derive no meaningful clinical benefıt. Understanding the biologic basis of de novo resistance to therapy may therefore help in identifying patients unlikely to benefıt from this class of anticancer agents. Preclinical work showed that an activated MAPK pathway, induced by KRAS mutation, selects for cell lines unlikely to respond to this class of agents, whereas isolated oncogenic PIK3CA alterations sensitized cells to everolimus, both in vitro and in vivo. Concomitant or exogenous introduction of KRAS mutations, however, rendered the cells insensitive, although genetic ablation of mutant KRAS from cells with coexisting PIK3CA and KRAS reinstated drug sensitivity. This lack of benefıt of mTOR inhibitor therapy in the presence of KRAS mutation was reproduced in a cohort of patients treated with everolimus.22 Interestingly, de novo resistance mediated by KRAS is mitigated by coexisting LKB1-defıciency as well as p53 loss.23 Given the co-occurrence of LKB1 and KRAS alterations in lung cancer, this fınding will be especially useful in therapeutic studies of PI3K/AKT/mTOR inhibitors in this population.
Acquired resistance may also be mediated by genetic alteration that develops under selective pressure by the therapeutic agent. Although no such genetic alteration has yet been reported from human trials, basic research in S. cerevisae identifıed a hotspot in Ile800 of the PIK3CA gene, which confers a 5 to 10-fold decrease in potency for a large panel of mTOR and PI3K inhibitors. Interestingly, these resistant mutations do not reside in the classic gatekeeper residues, unlike the observation with tyrosine kinase inhibitors.24
Protein Biomarkers
Preclinical work showed that sensitivity to the PI3K inhibitor, GDC-0941, was associated with high baseline expression of the mTOR pathway protein, p4E-BP1, and pAkt by gene expression assay in the NCI-60 human tumor cell line screening study.25 A predictive model for mTOR inhibitor therapy effıcacy was investigated by using data obtained from extensive pharmacokinetic and pharmacodynamic measurements in human and animal studies treated with various mTOR inhibitors. 26 Univariate analysis showed signifıcant correlation of effıcacy with pS6 (R=0.53, p<0.01), total S6 (R=−0.51, p < 0.02), pAKT (R = 0.66, p < 0.001), pS6/total S6 (R = 0.76, p < 0.0001). Using logistic regression and ROC algorithm, the combination of high pAKT and high p235-S6/total S6 as a predictor of sensitivity and low pAKT and low p235-S6/total S6 as a predictor of insensitivity demonstrated 73% and 100% sensitivity and specifıcity, respectively and an AUC of 0.88.26 Although this combination of biomarkers has not been validated in a prospective human patient study, fındings from early phase clinical studies support the utility of pAKT in tumor samples as a predictor of sensitivity to mTOR inhibitor therapy.27,28
Complementary pathway protein modulation
mTOR signaling inhibition by nonspecifıc allosteric inhibitors such as rapamycin suppressed p70S6 kinase activity but paradoxically also increased the activation of AKT and eIF4E, which attenuated the therapeutic effıcacy of these agents. This observation provided the initial insight into the role that compensatory feedback loop through AKT may play in the ability of treated cells to overcome mTOR inhibitor therapy. 29 It also supported the impetus to develop TORC1 and TORC2-specifıc inhibitors as well as dual mTOR/PI3K inhibitors that can inhibit downstream mTOR signaling with minimal compensatory AKT activation. Several such compounds have entered the clinical testing phase but whether they achieve superior effıcacy over nonselective mTOR inhibitors is still unclear. Other feedback or alternative signaling loops that mediate resistance involve an mTOR-dependent serine phosphorylation of insulin receptor substrate-1 (IRS-1) that enhances insulin-like growth factor-1 (IGF-1) signaling leading to downstream activation of PI3K/AKT. Efforts to exploit these fındings in the clinic include a combination strategy of an mTOR and IGFR inhibitor.30
The effıcacy of mTOR inhibitors has also been ascribed to the involvement of the mTOR pathway in tumor-related angiogenesis and may be signifıcant in renal cell cancer in which loss of the tumor suppressor VHL gene promotes a high level of HIF-α mRNA expression. Similar to observations with cytotoxic chemotherapy in which HIF-1α overexpression induces tumor resistance to chemotherapy, a high level of HIF-1α activity may predict for benefıt from mTOR inhibitor therapy but may therefore provide an escape mechanism leading to treatment resistance. Consistent with this theory, the level of expression of the proangiogenic factor, VEGF-D, has been shown to correlate with disease burden and decreases following treatment with sirolimus in patients with TSC.31
A newly identifıed biomarker of resistance is the p21-activated kinase 1 (PAK1) protein, which is involved in pro-survival cell signaling and was previously reported as a marker of poor prognosis in patients with solid malignancies. PAK1 protein expression was shown to mediate resistance to PI3K and PI3K/mTOR inhibitors in lymphoma cell lines.32 Clinical validation of this biomarker is still awaited.
Drug-Induced Toxicities as Surrogate Biomarker
The currently approved agents targeting the PI3K/AKT/mTOR pathway and those in early stage development have demonstrated a tolerable toxicity profıle. The most common adverse events reported include fatigue, stomatitis, hyperglycemia, hyperlipidemia, and skin rash. Rare but potentially life-threatening noninfectious pneumonitis with mTOR inhibitors and mood disorder with PI3K inhibitors have also been encountered. The metabolic consequence of hyperglycemia and hyperlipidemia is, however, an intriguing class effect of uncertain pathophysiology. By attenuating the expected increase in insulin level as a physiologic response to hyperglycemia, rapalogs induce a state of insulin resistance leading to increased glucose level. Similarly, inhibitors of this pathway cause an impaired hepatic fatty acid metabolism leading to increased β-oxidation of fatty acid along with reduced influx of free fatty acid into anabolic storage pathways, resulting in increased serum levels of triglyceride and cholesterol.33,34 A retrospective analysis of cholesterol, triglycerides, and glucose measurements from patients in a prospective randomized study of IFN-α compared with temsirolimus showed a signifıcant association between increased cholesterol and longer survival (OS: HR = 0.77 per mmol/L, p<0.0001; PFS: HR=0.81 per mmol/L; p<0.0001). Interestingly, the survival benefıt associated with temsirolimus was completely explained by the increase in cholesterol on multivariate analysis. It is plausible that with better understanding of the pathophysiologic basis, these metabolic toxicities may be used as surrogate biomarkers of target modulation similar to the use of skin rash and development of hypertension in patients treated with EGFR and angiogenic inhibitors, respectively.
CONCLUSION
The PI3K/AKT/mTOR pathway is an established driver of oncogenesis in human patients. Agents targeting different components of this pathway are in clinical development with regulatory approval for marketing granted for everolimus and temsirolimus. Increased understanding of the mechanism of action of these agents continues to inform their clinical development including combination approaches to prevent or overcome treatment resistance and the development of isoform specifıc PI3K inhibitors for specifıc patient subsets defıned by driver molecular aberration. Clinical toxicity of hyperglycemia and hyperlipidemia are easily managed class effects of these agents that may also serve as pharmacodynamic markers of activity.
KEY POINTS.
The PI3K/AKT/mTOR pathway is an established oncogenic driver in a variety of tumor types.
Inhibitors of this pathway are already in clinical testing, and U.S. Food and Drug Administration (FDA) approval for everolimus and temsirolimus have validated this pathway as a therapeutic target.
Predictive biomarkers of efficacy (PIK3CA mutation, PTEN loss, and high pAKT and pS6 protein expression by IHC) and resistance (KRAS) developed in the preclinical setting and early phase clinical trials hold promise pending prospective validation.
Adverse events such as metabolic toxicity with impaired glycemic and lipid control and mood alterations are class effects that may be exploited to guide appropriate dosing of these agents in the clinic.
Footnotes
Disclosures of Potential Conflicts of Interest
Relationships are considered self-held and compensated unless otherwise noted. Relationships marked “L” indicate leadership positions. Relationships marked “I” are those held by an immediate family member; those marked “B” are held by the author and an immediate family member. Relationships marked “U” are uncompensated.
Employment or Leadership Position: None. Consultant or Advisory Role: None. Stock Ownership: None. Honoraria: None. Research Funding: Fadlo R. Khuri, Novartis; Pfizer. Taofeek K. Owonikoko, Novartis Oncology. Expert Testimony: None. Other Remuneration: None.
References
- 1.Yuan TL, Cantley LC. PI3K pathway alterations in cancer: variations on a theme. Oncogene. 2008;27:5497–5510. doi: 10.1038/onc.2008.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhao L, Vogt PK. Class I PI3K in oncogenic cellular transformation. Oncogene. 2008;27:5486–5496. doi: 10.1038/onc.2008.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Engelman JA, Luo J, Cantley LC. The evolution of phosphatidylinositol 3-kinases as regulators of growth and metabolism. Nat Rev Genet. 2006;7:606–619. doi: 10.1038/nrg1879. [DOI] [PubMed] [Google Scholar]
- 4.Memmott RM, Dennis PA. Akt-dependent and -independent mechanisms of mTOR regulation in cancer. Cell Signal. 2009;21:656–664. doi: 10.1016/j.cellsig.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hudes G, Carducci M, Tomczak P, et al. Temsirolimus, interferon alfa, or both for advanced renal-cell carcinoma. N Engl J Med. 2007;356:2271–2281. doi: 10.1056/NEJMoa066838. [DOI] [PubMed] [Google Scholar]
- 6.Baselga J, Campone M, Piccart M, et al. Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med. 2012;366:520–529. doi: 10.1056/NEJMoa1109653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yao JC, Shah MH, Ito T, et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011;364:514–523. doi: 10.1056/NEJMoa1009290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Motzer RJ, Escudier B, Oudard S, et al. Effıcacy of everolimus in advanced renal cell carcinoma: a double-blind, randomised, placebo-controlled phase III trial. Lancet. 2008;372:449–456. doi: 10.1016/S0140-6736(08)61039-9. [DOI] [PubMed] [Google Scholar]
- 9.Crino PB, Nathanson KL, Henske EP. The tuberous sclerosis complex. N Engl J Med. 2006;355:1345–1356. doi: 10.1056/NEJMra055323. [DOI] [PubMed] [Google Scholar]
- 10.Franz DN, Belousova E, Sparagana S, et al. Effıcacy and safety of everolimus for subependymal giant cell astrocytomas associated with tuberous sclerosis complex (EXIST-1): a multicentre, randomised, placebo-controlled phase 3 trial. Lancet. 2013;381:125–132. doi: 10.1016/S0140-6736(12)61134-9. [DOI] [PubMed] [Google Scholar]
- 11.Bissler JJ, Kingswood JC, Radzikowska E, et al. Everolimus for angiomyolipoma associated with tuberous sclerosis complex or sporadic lymphangioleiomyomatosis (EXIST-2): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2013 doi: 10.1016/S0140-6736(12)61767-X. [DOI] [PubMed] [Google Scholar]
- 12.Liaw D, Marsh DJ, Li J, et al. Germline mutations of the PTEN gene in Cowden disease, an inherited breast and thyroid cancer syndrome. Nat Genet. 1997;16:64–67. doi: 10.1038/ng0597-64. [DOI] [PubMed] [Google Scholar]
- 13.Samuels Y, Wang Z, Bardelli A, et al. High frequency of mutations of the PIK3CA gene in human cancers. Science. 2004;304:554. doi: 10.1126/science.1096502. [DOI] [PubMed] [Google Scholar]
- 14.Serra V, Markman B, Scaltriti M, et al. NVP-BEZ235, a dual PI3K/mTOR inhibitor, prevents PI3K signaling and inhibits the growth of cancer cells with activating PI3K mutations. Cancer Res. 2008;68:8022–8030. doi: 10.1158/0008-5472.CAN-08-1385. [DOI] [PubMed] [Google Scholar]
- 15.Mueller A, Bachmann E, Linnig M, et al. Selective PI3K inhibition by BKM120 and BEZ235 alone or in combination with chemotherapy in wild-type and mutated human gastrointestinal cancer cell lines. Cancer Chemother Pharmacol. 2012;69:1601–1615. doi: 10.1007/s00280-012-1869-z. [DOI] [PubMed] [Google Scholar]
- 16.Gonzalez-Angulo AM, Blumenschein GR., Jr Defıning biomarkers to predict sensitivity to PI3K/Akt/mTOR pathway inhibitors in breast cancer. Cancer Treat Rev. 2012 doi: 10.1016/j.ctrv.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Brien C, Wallin JJ, Sampath D, et al. Predictive biomarkers of sensitivity to the phosphatidylinositol 3′ kinase inhibitor GDC-0941 in breast cancer preclinical models. Clin Cancer Res. 2010;16:3670–3683. doi: 10.1158/1078-0432.CCR-09-2828. [DOI] [PubMed] [Google Scholar]
- 18.Vasudevan KM, Barbie DA, Davies MA, et al. AKT-independent signaling downstream of oncogenic PIK3CA mutations in human cancer. Cancer Cell. 2009;16:21–32. doi: 10.1016/j.ccr.2009.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wee S, Wiederschain D, Maira SM, et al. PTEN-defıcient cancers depend on PIK3CB. Proc Natl Acad Sci U S A. 2008;105:13057–13062. doi: 10.1073/pnas.0802655105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Loi S, Haibe-Kains B, Majjaj S, et al. PIK3CA mutations associated with gene signature of low mTORC1 signaling and better outcomes in estrogen receptor-positive breast cancer. Proc Natl Acad Sci U S A. 2010;107:10208–10213. doi: 10.1073/pnas.0907011107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Loi S, Michiels S, Baselga J, et al. PIK3CA Genotype and a PIK3CA Mutation-Related Gene Signature and Response to Everolimus and Letrozole in Estrogen Receptor Positive Breast Cancer. PLoS ONE. 2013;8:e53292. doi: 10.1371/journal.pone.0053292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Di Nicolantonio F, Arena S, Tabernero J, et al. Deregulation of the PI3K and KRAS signaling pathways in human cancer cells determines their response to everolimus. J Clin Invest. 2010;120:2858–2866. doi: 10.1172/JCI37539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mahoney CL, Choudhury B, Davies H, et al. LKB1/KRAS mutant lung cancers constitute a genetic subset of NSCLC with increased sensitivity to MAPK and mTOR signalling inhibition. Br J Cancer. 2009;100:370–375. doi: 10.1038/sj.bjc.6604886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zunder ER, Knight ZA, Houseman BT, Apsel B, Shokat KM. Discovery of drug-resistant and drug-sensitizing mutations in the oncogenic PI3K isoform p110 alpha. Cancer Cell. 2008;14:180–192. doi: 10.1016/j.ccr.2008.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kwei KA, Baker JB, Pelham RJ. Modulators of sensitivity and resistance to inhibition of PI3K identifıed in a pharmacogenomic screen of the NCI-60 human tumor cell line collection. PLoS ONE. 2012;7:e46518. doi: 10.1371/journal.pone.0046518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O’Reilly T, McSheehy PM. Biomarker Development for the Clinical Activity of the mTOR Inhibitor Everolimus (RAD001): Processes. Limitations, and Further Proposals Transl Oncol. 2010;3:65–79. doi: 10.1593/tlo.09277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Owonikoko TK, Ramalingam S, Subramanian J, et al. Analysis of mTOR signaling pathway biomarkers in nonsmall cell lung cancer patients treated with everolimus and docetaxel in a phase II clinical trial. J Thorac Oncol. 2011;6:S1039–S1040. [Google Scholar]
- 28.Meric-Bernstam F, Akcakanat A, Chen H, et al. PIK3CA/PTEN mutations and Akt activation as markers of sensitivity to allosteric mTOR inhibitors. Clin Cancer Res. 2012;18:1777–1789. doi: 10.1158/1078-0432.CCR-11-2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sun SY, Rosenberg LM, Wang X, et al. Activation of Akt and eIF4E survival pathways by rapamycin-mediated mammalian target of rapamycin inhibition. Cancer Res. 2005;65:7052–7058. doi: 10.1158/0008-5472.CAN-05-0917. [DOI] [PubMed] [Google Scholar]
- 30.Shi Y, Yan H, Frost P, Gera J, Lichtenstein A. Mammalian target of rapamycin inhibitors activate the AKT kinase in multiple myeloma cells by up-regulating the insulin-like growth factor receptor/insulin receptor substrate-1/phosphatidylinositol 3-kinase cascade. Mol Cancer Ther. 2005;4:1533–1540. doi: 10.1158/1535-7163.MCT-05-0068. [DOI] [PubMed] [Google Scholar]
- 31.Dabora SL, Franz DN, Ashwal S, et al. Multicenter phase 2 trial of sirolimus for tuberous sclerosis: Kidney angiomyolipomas and other tumors regress and VEGF-D levels decrease. PLoS ONE. 2011;6:e23379. doi: 10.1371/journal.pone.0023379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Walsh K, McKinney MS, Love C, et al. PAK1 Mediates Resistance to PI3K Inhibition in Lymphomas. Clin Cancer Res. 2013 doi: 10.1158/1078-0432.CCR-12-1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee CK, Marschner IC, Simes RJ, et al. Increase in cholesterol predicts survival advantage in renal cell carcinoma patients treated with temsirolimus. Clin Cancer Res. 2012;18:3188–3196. doi: 10.1158/1078-0432.CCR-11-3137. [DOI] [PubMed] [Google Scholar]
- 34.Busaidy NL, Farooki A, Dowlati A, et al. Management of metabolic effects associated with anticancer agents targeting the PI3K-Akt-mTOR pathway. J Clin Oncol. 2012;30:2919–2928. doi: 10.1200/JCO.2011.39.7356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hoeffer CA, Klann E. mTOR signaling: at the crossroads of plasticity, memory and disease. Trends Neuro. 2010;33:67–75. doi: 10.1016/j.tins.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]