Abstract
Objective
This study investigated whether temporomandibular joint (TMJ) condyle-fossa relationships are bilaterally symmetric in class III malocclusion patients with and without asymmetry and compared to those with normal occlusion. The hypothesis was a difference in condyle-fossa relationships exists in asymmetric patients.
Methods
Group 1 comprised 40 Korean normal occlusion subjects. Groups 2 and 3 comprised patients diagnosed with skeletal class III malocclusion, who were grouped according to the presence of mandibular asymmetry: Group 2 included symmetric mandibles, while group 3 included asymmetric mandibles. Pretreatment three-dimensional cone-beam computed tomography (3D CBCT) images were obtained. Right- and left-sided TMJ spaces in groups 1 and 2 or deviated and non-deviated sides in group 3 were evaluated, and the axial condylar angle was compared.
Results
The TMJ spaces demonstrated no significant bilateral differences in any group. Only group 3 had slightly narrower superior spaces (p < 0.001). The axial condylar angles between group 1 and 2 were not significant. However, group 3 showed a statistically significant bilateral difference (p < 0.001); toward the deviated side, the axial condylar angle was steeper.
Conclusions
Even in the asymmetric group, the TMJ spaces were similar between deviated and non-deviated sides, indicating a bilateral condyle-fossa relationship in patients with asymmetry that may be as symmetrical as that in patients with symmetry. However, the axial condylar angle had bilateral differences only in asymmetric groups. The mean TMJ space value and the bilateral difference may be used for evaluating condyle-fossa relationships with CBCT.
Keywords: TMJ, Facial asymmetry, Class III diagnosis, Three-dimensional cone-beam computed tomography, Condyle-fossa relationship
INTRODUCTION
Temporomandibular joint (TMJ) differences such as condyle-fossa relationships and condylar morphology in relation to different malocclusions have been previously studied.1-5 Compared to a class II malocclusion patient, in a class III malocclusion patient, the condyle was reported to be closer to the fossa roof.1 Meanwhile, other studies showed that the condyle was positioned more forward in class II division 1 and more backward in class III patients.6 However, the influence of occlusions on the TMJ is still controversial. Many investigators reported a correlation between occlusal factors and joint morphology or the condyle-fossa relationship;1-5 however, Cohlmia et al.7 reported no correlations between them. The lack of centralization of the mandibular condyles was a characteristic in class II division 1 subdivision malocclusion patients,8,9 and it was also seen in other studies of patients with malocclusion.5,7,10
The condyle-fossa relationship can be interpreted differently, depending on the type of radiograph used, as well as differing references and patient positioning.11 Many studies adopted various modes of imaging techniques for the TMJ, such as lateral cephalograms and axially corrected tomograms,7,12 dry skulls,11 multislice conventional computed tomography (CT),4,5,13 and three-dimensional cone-beam computed tomography (3D CBCT).14,15 Moreover, different reference lines and planes with inconsistent head orientations were used, potentially causing clinician confusion.1-5 Further, conventional CT was performed with the patient in the supine position, rather than in the upright position, which may have led to errors in the evaluation of the condyle-fossa relationships.
The TMJ condyles are easily visible in the images of CBCT, which is increasingly used, but sometimes, the condyle-fossa relationship appears different in patients with asymmetry. It has been postulated that the condylar position, size, and shape may be associated with asymmetry.6,16 The condylar position may naturally vary in each individual and also in patients with asymmetry. Therefore, questions as to what the normal ranges of the anatomic condylar position are in 3D CBCT images, as well as their bilateral positional difference, remain unanswered.
Therefore, the purpose of this study was to investigate whether TMJ condyle-fossa relationships are bilaterally symmetrical in class III patients with and without asymmetry, to compare those with normal occlusion, and to help develop quantitative standards regarding the mean differences between the right and left TMJ spaces to aid in diagnosis. The hypothesis was that a difference in the condyle-fossa relationship exists in patients with asymmetry.
MATERIALS AND METHODS
The study comprised class I normal occlusion (group 1) and skeletal class III malocclusion subjects (groups 2 and 3). Group 1 consisted of 40 subjects (19 males; 21 females; mean age, 22.3 years) selected from the normal occlusion sample data in Department of Orthodontics at Seoul St. Mary's Hospital, the Catholic University of Korea (Seoul, Korea). The subjects were screened and selected from 480 Korean students (mean age, 24.3 years; range, 19.1 - 34.0 years) at Wonkwang University (Iksan, Korea) using the following selection criteria. The exclusion criteria included: (1) missing or decayed teeth; (2) prosthetic crowns; (3) crowding of > 3 mm or spacing of > 1 mm; (4) midline deviation of > 1 mm; and (5) noticeable periodontal diseases. All subjects had fully developed permanent dentition with normal overbite and overjet between 1 - 3 mm.
Groups 2 and 3 were selected from 1,181 patients who visited Department of Orthodontics at Seoul St. Mary's Hospital (Seoul, Korea) from July 2010 to July 2012; were diagnosed with skeletal class III malocclusion; required orthognathic surgery; and were grouped according to the presence of mandibular asymmetry that was assessed by routine diagnostic records and CBCT. Group 2 (14 males, 26 females; mean age, 24.9 years) had symmetric mandibles with a chin deviation of < 2 mm as measured at Menton and with no maxillary cant, and group 3 (23 males, 17 females; mean age, 23.8 years) had asymmetric mandibles with a chin deviation of > 3 mm and with no maxillary cant. Patients with a dental midline deviation of < 3 mm were included in group 3, if the patient had a chin deviation of > 3 mm. Patients with TMJ pain or discomfort, noticeable periodontal diseases, other craniofacial anomalies, and facial trauma history were excluded. The institutional review board of the Catholic University of Korea approved the experimental protocols (KC11EISI0740; KC12RISI0662).
CBCT images were obtained before orthodontic treatment with an iCAT scanner (Imaging Science International, Hatfield, PA, USA) using a 200 × 400 mm field of view, 120 kVp, 47.7 mA and resulting in a 0.4-mm voxel size. The obtained data were exported in the DICOM format into the InVivo Dental software (Anatomage, San Jose, CA, USA), and the 3D reconstructions were created. The CBCT images were reoriented with the horizontal reference plane connecting the bilateral orbitales and Frankfurt horizonal (FH) plane as previously reported,17,18 and the vertical midline and horizontal reference planes were set accordingly. The sagittal slices were evaluated where the mediolateral diameter of the right or left condyle was the greatest (Figure 1). The linear measurements of the right and left joint spaces were assessed, and the anterior joint space (AS), superior joint space (SS), and posterior joint space (PS) were measured from the most prominent anterior, posterior, and superior condylar points to the glenoid fossa.7 The plane parallel to the FH plane was used as the reference plane (Figure 2). The SS was measured from the most superior glenoid fossa point to the superior condylar aspect. The axial condylar angle was defined as the angle between the long axis of the condylar process and a perpendicular line to the midsagittal plane in the axial view (Figure 3).4,16 The mean and the difference in the bilateral means, as well as the absolute values of the bilateral mean difference in each group, were compared among the groups. In group 3 with asymmetric mandibles, the difference was calculated by subtracting the non-deviated side values from that of the deviated side values. The same operator (Y Kim) performed all measurements.
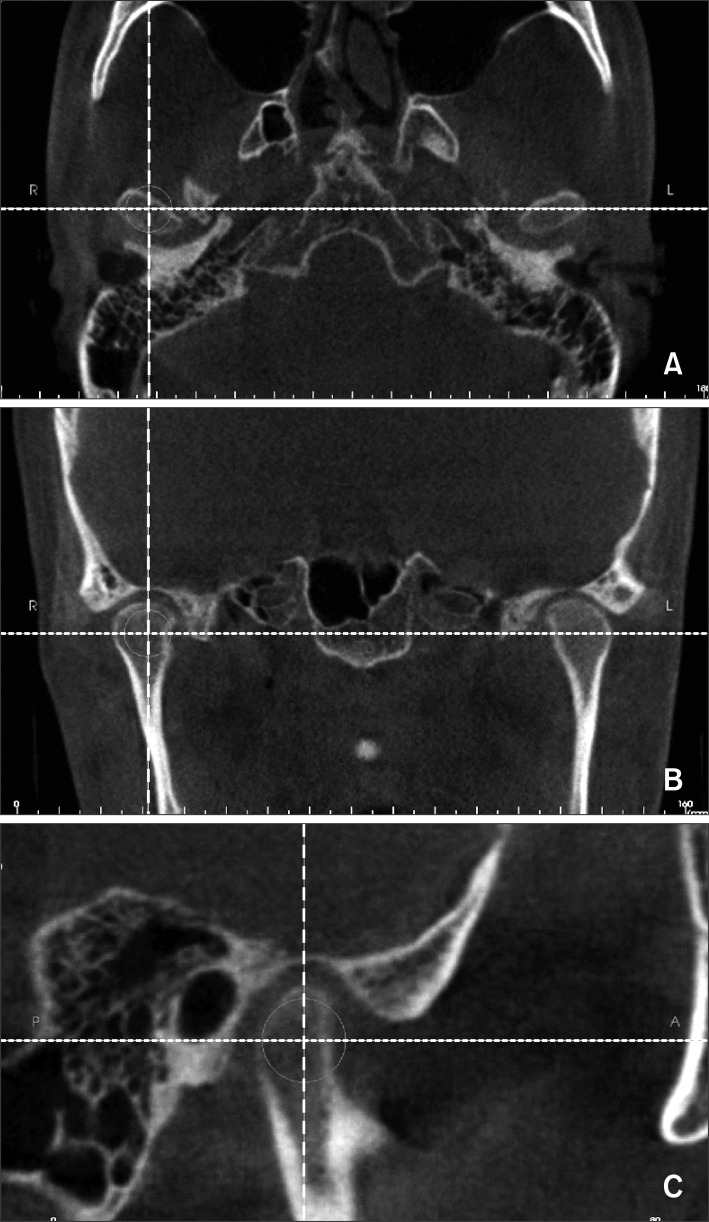
Figure 1.
The 3 views of the condyle in the cone-beam computed tomography (CBCT) image: A, axial view; B, coronal view; C, sagittal view. The CBCT images were reoriented with the horizontal reference plane connecting the bilateral orbitales and Frankfurt horizontal plane,17,18 and the vertical midline and horizontal reference planes were set accordingly. The sagittal slice (C) was evaluated at the point where the mediolateral diameter of the right or left condyles was greatest (A) in the axial view.
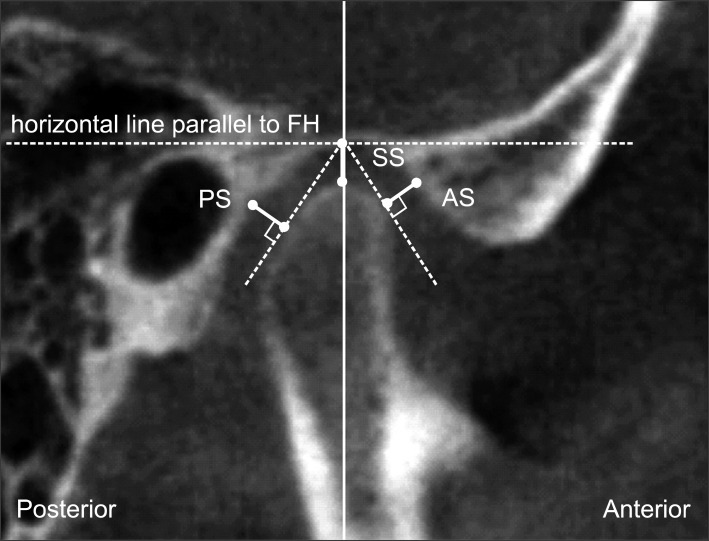
Figure 2.
Measurement of the joint space in the sagittal view. Anterior joint space (AS), superior joint space (SS), and posterior joint space (PS) were measured from the most prominent anterior, posterior, and superior condylar points to that of the glenoid fossa with the methods previously reported.7 The plane parallel to the Frankfurt horizontal (FH) plane was used as the reference plane.
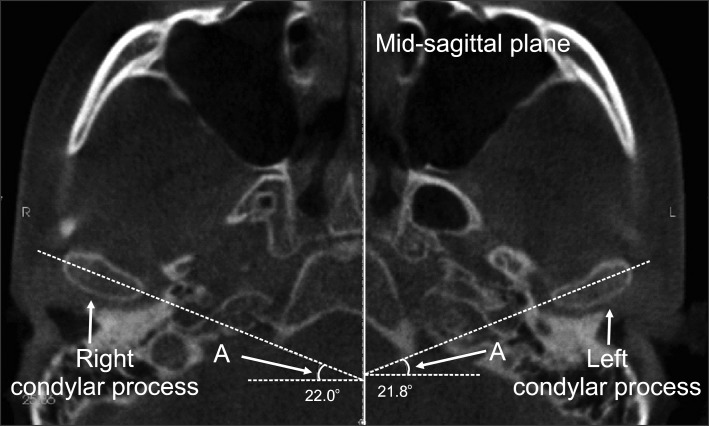
Figure 3.
Measurement of the axial condylar angle of the condylar process (A). It was defined as the angle between the long axis of the mandibular condylar process and a perpendicular line to the midsagittal plane.7
Statistical analyses
All measurements were repeated after 2 weeks by the same investigator, and the mean of the 2 measurements was used in the statistical analysis. The systemic intraexaminer error between the 2 measurements was determined using a paired t-test. Moreover, the magnitude of the measurement error was assessed by calculating the intraclass correlation coefficient (ICC). For statistical analyses, one-way ANOVA, Scheffé test, Kruskal-Wallis test, and paired t-test were used with a standard statistical software package (SAS version 8.02; SAS Institute, Cary, NC, USA). A p-value of < 0.05 was chosen for the significance level in all tests.
RESULTS
The systemic intra-examiner error was evaluated at p < 0.05 and found to be statistically insignificant. The ICC measurement indicated good reliability with a mean ICC of 0.836 (ICC = 0.719 - 0.890). The amount of asymmetry in each group, including the chin deviation mean, standard deviation, and range, is described in Table 1. Group 1 (with normal occlusion) had minimal asymmetry with a chin deviation mean of < 1 mm. The samples' cephalometric characteristics are described in Table 2 and showed statistically significant differences among the groups with respect to the sagittal measurements, e.g., SNB, ANB difference, APDI, and Wits analysis. Compared to group 1 and 2, group 3 showed statistically significant labioversion of the upper incisors and linguoversion of the lower incisors (p < 0.001).
Table 1.
Measurement of the amount of asymmetry in the sample
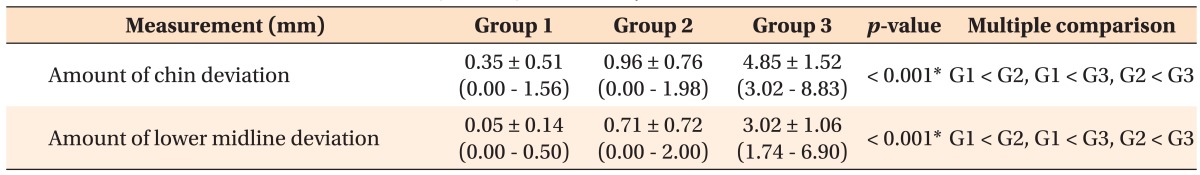
Values are presented as mean ± standard deviation (range). Amount of chin deviation was measured at Menton point.
Group 1 (G1), Normal occlusion; group 2 (G2), symmetric class III; group 3 (G3), asymmetric class III.
*p = 0.001 (one-way analysis of variance, Scheffé test, and Kruskal Wallis test).
Table 2.
Cephalometric characteristics of the sample
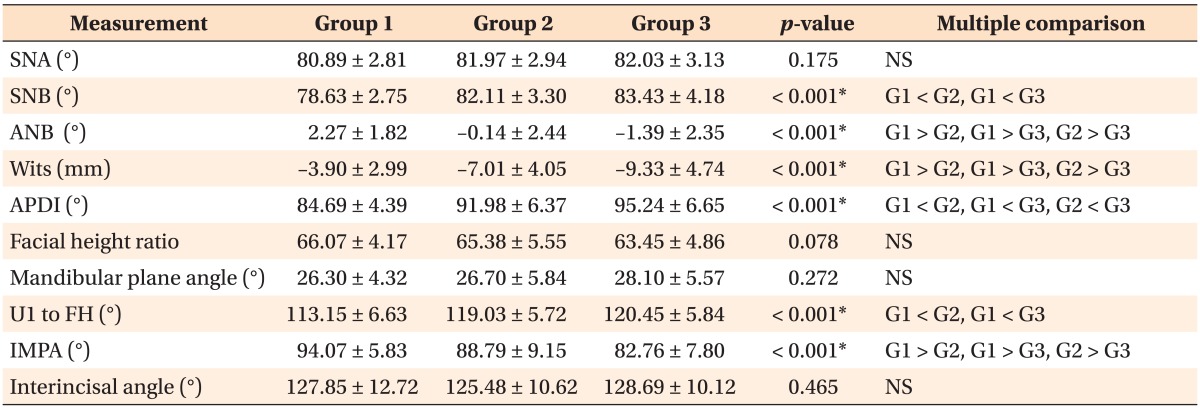
Values are presented as mean ± standard deviaton.
Group 1 (G1), Normal occlusion; group 2 (G2), symmetric class III; group 3 (G3), asymmetric class III.
*p = 0.001 (one-way analysis of variance, Scheffé test, and Kruskal Wallis test).
NS, Not significant; SNA, angle between sella-nasion-A point; SNB, angle between sella-nasion-B point; ANB, angle between A point to nasion, B point to nasion; Wits, Wits appraisal; APDI, anteroposterior dysplasia index; U1, upper incisor inclination; FH, Frankfurt horizontal plane; IMPA, incisor mandibular plane angle.
The joint space measurements in the sagittal view are shown in Table 3. The 3 groups did not demonstrate significant differences in AS and PS. With only the SS, group 3 showed a slightly superior condylar position than group 1 and 2 on the deviated side (p < 0.05) and the non-deviated side (p < 0.01). The mean absolute value differences in the right and left joint spaces were 0.54 mm (AS), 0.45 mm (SS), and 0.41 mm (PS) in group 1, with no significant differences among the 3 groups. The means of the right and left joint spaces are described in Table 4. Moreover, only the SS of group 3, compared to that of groups 1 and 2, showed a statistically superior position (p < 0.01).
Table 3.
Measurement of the joint space in the sagittal view
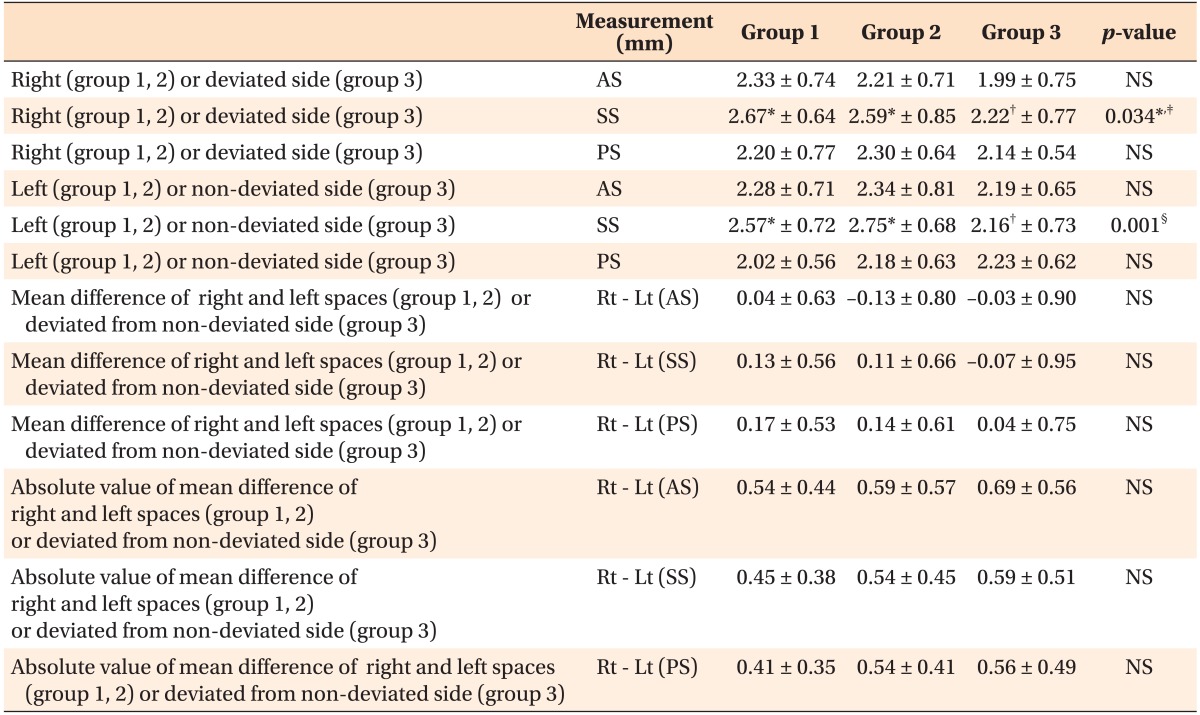
Values are presented as mean ± standard deviaton.
Group 1, Normal occlusion; group 2, symmetric class III; group 3, asymmetric class III.
AS, Anterior joint space; SS, superior joint space; PS, posterior joint space; Rt, right; Lt, left; NS, not significant.
Groups with different marks (*, †) are significantly different from each other; ‡p = 0.05; §p = 0.01 (one-way analysis of variance, Scheffé test, and Kruskal Wallis test).
Table 4.
Means of the right and left joint spaces
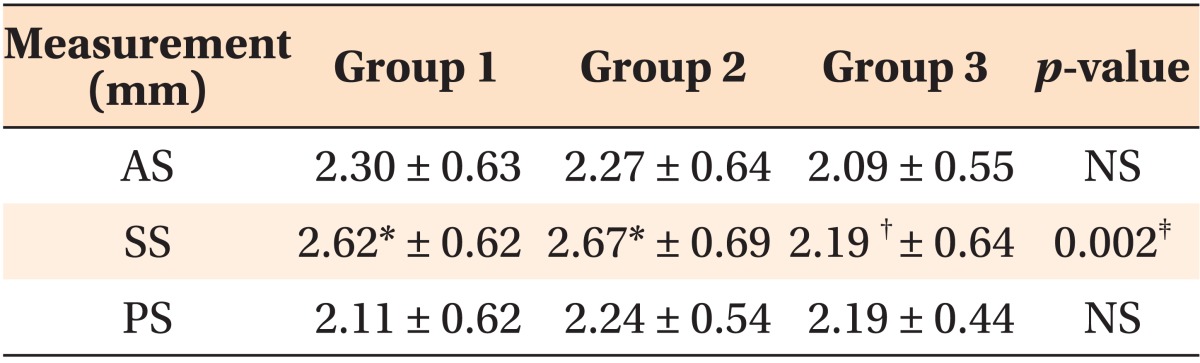
Values are presented as mean ± standard deviaton.
Group 1, normal occlusion; group 2, symmetric class III; group 3, asymmetric class III.
AS, Anterior joint space; SS, superior joint space; PS, posterior joint space; NS, not significant.
Groups with different marks (*, †) are significantly different from each other; ‡p = 0.01 (one-way analysis of variance, Scheffé test, and Kruskal Wallis test).
The axial condylar angle was significantly flatter in group 2 and 3 than that on both sides in group 1 (Table 5). In groups 1 and 2, the mean differences between the right and left sides, or in group 3, the difference calculated by subtracting the non-deviated side values from that of the deviated side values, were significantly larger in group 3 than that of groups 1 and 2. On the deviated side in group 3, the axial condylar angle was significantly larger (p < 0.01) (Tables 5 and 6). Further, the absolute mean difference value showed a similar trend of an increasing or a steeper axial condylar angle on the deviated side in group 3. This indicated that the patients with asymmetry had significantly different bilateral axial condylar angle than those with symmetry, and the axial condylar angle was significantly larger in the condyles on the deviated side.
Table 5.
Measurement of the axial condylar angle of the condylar process
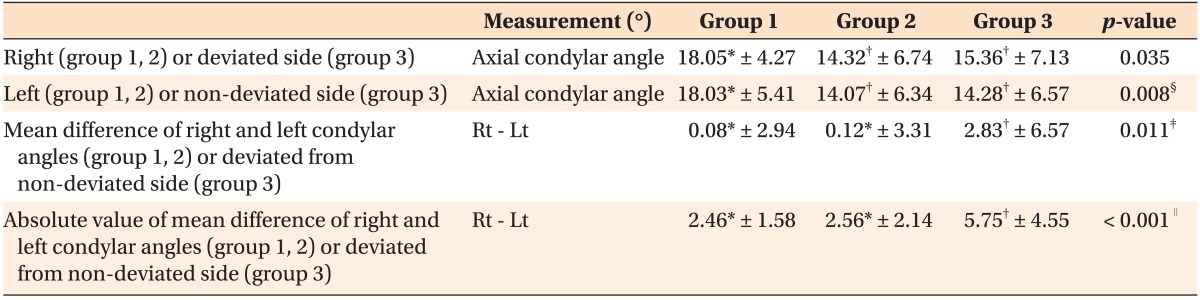
Values are presented as mean ± standard deviaton.
Group 1, Normal occlusion; group 2, symmetric class III; group 3, asymmetric class III.Rt, Right; Lt, left; NS, not significant.
Groups with different letters (*, †) are significantly different from each other; ‡p = 0.05; §p = 0.01; ∥p = 0.001 (one-way analysis of variance, Scheffé test, and Kruskal Wallis test).
Table 6.
Comparison of the axial condylar angle between right and left, or deviated and non-deviated side
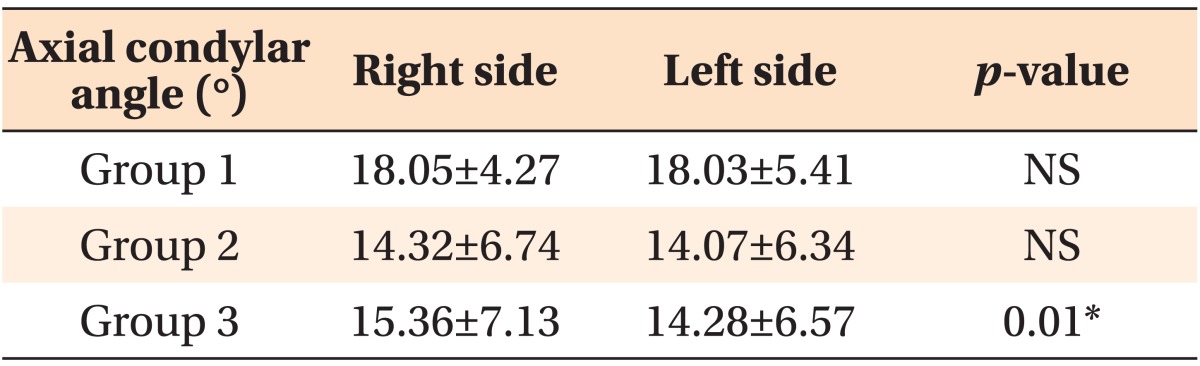
Values are presented as mean ± standard deviaton.
Group 1, Normal occlusion; group 2, symmetric class III; group 3, asymmetric class III; right side, deviated side in group 3; left side, non-deviated side in group 3; NS, not significant.
*p = 0.01 (paired t-test).
DISCUSSION
There has been much controversy regarding whether the condyle-fossa relationships are normal in patients with malocclusion. Previous studies concluded that asymmetric TMJ spaces were usually associated with TMJ dysfunction;2 conversely, bilateral condylar concentricity was associated with an absence of clinical symptoms. Moreover, questions have not been clearly answered regarding the potential of any differences in patients with or without symmetry as to the right-sided or left-sided condylar positioning or deviated or non-deviated sides, as well as how much of a difference between the right and left sides exists.
This study investigated whether the condylar-fossa relation is bilaterally symmetrical in class III patients with or without asymmetry, compared to that of the subjects with normal occlusion and found that the condylar space of AS, SS, and PS were not significantly different whether the patient had a class III malocclusion (groups 2 and 3) or class I normal occlusion (group 1) and whether the patient had symmetry (groups 1 and 2) or asymmetry (group 3) (Table 3). Although group 3 showed a more superiorly positioned condyle, the difference was relatively small. This result showed that the TMJ space were not significantly different regardless of the presence of asymmetry.
For the comparison of the mean bilateral space difference, both the mean difference and the absolute value of the difference were used (Table 3). For the symmetric groups (groups 1 and 2), the absolute value may present valid information; however, in group 3 patients who had asymmetry, discrimination of the deviated and non-deviated sides was performed. The absolute mean difference values between the right and left spaces were approximately 0.4 mm to 0.5 mm in all groups; therefore, these values may be used as standards in diagnosing the condyle-fossa relationship in CBCT images. This bilateral difference might be used as an adaptation for the changing functional demands.19 The mean values of the right and left AS, SS, and PS that are shown in Table 4 revealed the approximate condylar position, as measured by CBCT. The spaces were not very different between group 1 and group 2. Thus, group 1 mean may also be used as a guideline during diagnosis with CBCT images with its measurements being as follows: AS, 2.30 mm; SS, 2.62 mm; and PS, 2.11 mm.
Westesson et al.20 advocated that the mean axial condylar angle was smallest in joints with a normal disk position (mean, 21.2°) and became larger in joints with disk displacement (33.5° for disk displacement without reduction), degenerative joint disease (36.5°), or both. Ueki et al.21 reported a mean axial condylar angle for the class III symmetry group as 12.0° on the right and 11.8° on the left. Compared to prior studies, this study revealed an approximate 18.0° mean axial condylar angle for the normal occlusion patients, with a 2.46° mean bilateral difference (Table 5). The skeletal class III patients without asymmetry (group 2) had a smaller angle of approximately 14°, with a similar bilateral difference as that of group 1 patients. These results showed that skeletal class III patients had flatter or smaller axial condylar angles than the normal occlusion patients, which grossly coincided with prior studies.20,21 In contrast, group 3 with asymmetry had the same tendency of an increasing bilateral difference between the deviated and non-deviated sides in both the mean difference (2.83°; p < 0.05) and in the absolute values of the differences (5.75°; p < 0.001), as shown in Table 5. These values were significantly different from those of group 1 and 2 patients and indicated that the axial condylar angle was steeper or larger on the deviated side with more shape variability. It would be reasonable to assume that as the mandible grows asymmetrically to the deviated side, the condyle should adjust and rotate in a certain direction, to maintain the same condyle-fossa relationship with similar bilateral joint spaces as shown in this study (Table 3). From this study result, the condyles rotate inwardly with an increasing axial condylar angle. A CBCT image of a sample case showing the largest axial condylar angle difference between deviated and non-deviated sides can be viewed in Figure 4. From the results of this and prior studies,20,21 the skeletal class III patients had flatter or smaller axial condylar angles than the normal occlusion patients, and the class II malocclusion patients had steeper or larger axial condylar angles. Therefore, from the viewpoint of malocclusion, the deviated side had less of a class III molar relationship than the non-deviated side, although both sides reflect the overgrown nature of the condyles; thus, a larger axial condylar angle on the deviated side might be consistent with the findings. However, the reasons why and how these differences in the axial condylar angle between the malocclusion groups occurred should be further investigated. Conversely, it would be meaningful to study patients who are still growing and have different bilateral condylar axial angles and to determine if it is possible to predict whether the mandible can grow in an asymmetrical manner. In addition, the finding that the joint spaces and their bilateral differences were not significantly different between symmetric and asymmetric groups, and that the condylar rotation occurred in the asymmetric group, imply that the joint space adapts to the condylar rotation and maintains the condyle-fossa relationship.
Figure 4.
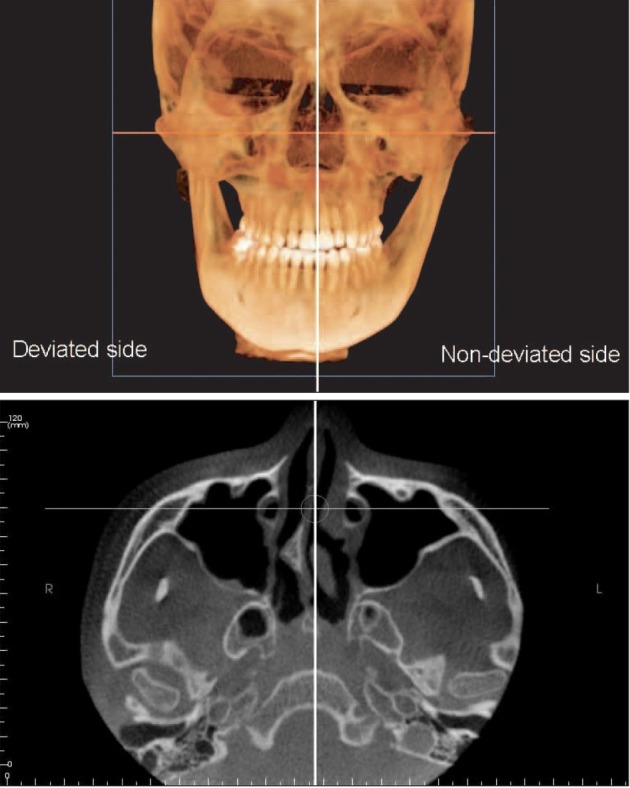
Cone-beam computed tomography image of a sample case showing the largest axial condylar angle difference between the deviated and non-deviated sides.
Traditionally, many studies have measured the joint space on a plane made along the axial condylar angle,13,21 either using corrected tomography1,12 or multislice medical CT.4,5,13 However, in this study, it was not possible to reorient the slices after the images were already obtained. Nonetheless, with CBCT images, spatial reorientation of the volumetric data is now possible, and the orientation of the slice can also be chosen. With the increasing use of CBCT, simple and easier methods for evaluating the condyle-fossa relationship may become necessary. Further, in this study, the measurements were assessed on a sagittal plane parallel to the midsagittal plane. Clipping the slice along the midsagittal plane during the volumetric rendering with commercial software is much easier than slicing along the axial condylar angle. Moreover, these data may also have meaningful clinical implications. More importantly, the study results had consistent means without significant variations in any group, so these data may be used, along with the prior data regarding the measurements along the condylar angles. A similar study, which measured the TMJ spaces of skeletal class III malocclusion patients with CBCT along the axial condylar angle,16 determined the AS was around 1.68 mm to 1.81 mm, while the SS was around 2.67 mm and PS was around 2.43 mm to 2.69 mm; however, in that study, no description indicated whether the patients had asymmetry. Further studies comparing these 2 methods of measuring the TMJ spaces may be necessary. In addition, conventional CT was obtained in the supine position, rather than in upright position in which the condyle may be placed more posteriorly in the supine position, and in this regard, CBCT may have some merits in evaluating the condyle-fossa relationships.
Although this study did not assess the disk position by magnetic resonance imaging (MRI), the incidence of internal derangement in skeletal class III patients was reported to be much less than that of class II patients.22 With the increasing use of CBCT, the mean joint space value and its bilateral difference may be useful for diagnosis; thus, a future study combining MRI with CBCT may be helpful for understanding TMJ. Moreover, additional study regarding skeletal class III patients with maxillary canting may be required.
CONCLUSION
The hypothesis was rejected. Even in the asymmetric groups, the TMJ spaces (anterior and posterior) in the sagittal view were not significantly different, indicating that the bilateral condylar position in patients with asymmetry may be as symmetrical as in patients with symmetry. However, the axial condylar angle was significantly different in group 3 and significantly larger on the side of the deviated condyles of the asymmetry group. This may indicate although functional or normal condylar growth rotation occurs, the joint space adapts to this rotation. The mean of AS, SS, and PS were 2.30 mm, 2.62 mm, and 2.11 mm, respectively, and the mean bilateral TMJ space difference was 0.54 mm (AS), 0.45 mm (SS), and 0.41 mm (PS) in group 1. These findings may be used when evaluating the condylar position with CBCT images.
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
This study was partially supported by the alumni fund of the Department of Dentistry and Graduate School of Clinical Dental Science, The Catholic University of Korea.
References
- 1.Katsavrias EG, Halazonetis DJ. Condyle and fossa shape in Class II and Class III skeletal patterns: a morphometric tomographic study. Am J Orthod Dentofacial Orthop. 2005;128:337–346. doi: 10.1016/j.ajodo.2004.05.024. [DOI] [PubMed] [Google Scholar]
- 2.Ahn SJ, Lee SP, Nahm DS. Relationship between temporomandibular joint internal derangement and facial asymmetry in women. Am J Orthod Dentofacial Orthop. 2005;128:583–591. doi: 10.1016/j.ajodo.2004.06.038. [DOI] [PubMed] [Google Scholar]
- 3.Byun ES, Ahn SJ, Kim TW. Relationship between internal derangement of the temporomandibular joint and dentofacial morphology in women with anterior open bite. Am J Orthod Dentofacial Orthop. 2005;128:87–95. doi: 10.1016/j.ajodo.2004.01.028. [DOI] [PubMed] [Google Scholar]
- 4.Vitral RW, da Silva Campos MJ, Rodrigues AF, Fraga MR. Temporomandibular joint and normal occlusion: Is there anything singular about it? A computed tomographic evaluation. Am J Orthod Dentofacial Orthop. 2011;140:18–24. doi: 10.1016/j.ajodo.2009.07.030. [DOI] [PubMed] [Google Scholar]
- 5.Rodrigues AF, Fraga MR, Vitral RW. Computed tomography evaluation of the temporomandibular joint in Class I malocclusion patients: condylar symmetry and condyle-fossa relationship. Am J Orthod Dentofacial Orthop. 2009;136:192–198. doi: 10.1016/j.ajodo.2007.07.032. [DOI] [PubMed] [Google Scholar]
- 6.Pullinger AG, Solberg WK, Hollender L, Petersson A. Relationship of mandibular condylar position to dental occlusion factors in an asymptomatic population. Am J Orthod Dentofacial Orthop. 1987;91:200–206. doi: 10.1016/0889-5406(87)90447-1. [DOI] [PubMed] [Google Scholar]
- 7.Cohlmia JT, Ghosh J, Sinha PK, Nanda RS, Currier GF. Tomographic assessment of temporomandibular joints in patients with malocclusion. Angle Orthod. 1996;66:27–35. doi: 10.1043/0003-3219(1996)066<0027:TAOTJI>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Vitral RW, Telles Cde S, Fraga MR, de Oliveira RS, Tanaka OM. Computed tomography evaluation of temporomandibular joint alterations in patients with class II division 1 subdivision malocclusions: condyle-fossa relationship. Am J Orthod Dentofacial Orthop. 2004;126:48–52. doi: 10.1016/j.ajodo.2003.06.012. [DOI] [PubMed] [Google Scholar]
- 9.Zuckerberg Al, Yaster M. Chapter 26. Anesthesia for orthopedic surgery. In: Davis PJ, Cladis FP, Motoyama EK, Smith RM, editors. Smith's anesthesia for infants and children. 8th ed. Philadelphia: Elsevier Mosby; 2011. pp. 842–869. [Google Scholar]
- 10.Rodrigues AF, Fraga MR, Vitral RW. Computed tomography evaluation of the temporomandibular joint in Class II Division 1 and Class III malocclusion patients: condylar symmetry and condyle-fossa relationship. Am J Orthod Dentofacial Orthop. 2009;136:199–206. doi: 10.1016/j.ajodo.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 11.Pandis N, Karpac J, Trevino R, Williams B. A radiographic study of condyle position at various depths of cut in dry skulls with axially corrected lateral tomograms. Am J Orthod Dentofacial Orthop. 1991;100:116–122. doi: 10.1016/S0889-5406(05)81518-5. [DOI] [PubMed] [Google Scholar]
- 12.Burke G, Major P, Glover K, Prasad N. Correlations between condylar characteristics and facial morphology in Class II preadolescent patients. Am J Orthod Dentofacial Orthop. 1998;114:328–336. doi: 10.1016/s0889-5406(98)70216-1. [DOI] [PubMed] [Google Scholar]
- 13.Lee W, Park JU. Three-dimensional evaluation of positional change of the condyle after mandibular setback by means of bilateral sagittal split ramus osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:305–309. doi: 10.1067/moe.2002.126452. [DOI] [PubMed] [Google Scholar]
- 14.Hilgers ML, Scarfe WC, Scheetz JP, Farman AG. Accuracy of linear temporomandibular joint measurements with cone beam computed tomography and digital cephalometric radiography. Am J Orthod Dentofacial Orthop. 2005;128:803–811. doi: 10.1016/j.ajodo.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 15.Librizzi ZT, Tadinada AS, Valiyaparambil JV, Lurie AG, Mallya SM. Cone-beam computed tomography to detect erosions of the temporomandibular joint: Effect of field of view and voxel size on diagnostic efficacy and effective dose. Am J Orthod Dentofacial Orthop. 2011;140:e25–e30. doi: 10.1016/j.ajodo.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 16.Kim YI, Cho BH, Jung YH, Son WS, Park SB. Cone-beam computerized tomography evaluation of condylar changes and stability following two-jaw surgery: Le Fort I osteotomy and mandibular setback surgery with rigid fixation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:681–687. doi: 10.1016/j.tripleo.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Kook YA, Kim Y. Evaluation of facial asymmetry with three-dimensional cone-beam computed tomography. J Clin Orthod. 2011;45:112–115. quiz 92. [PubMed] [Google Scholar]
- 18.Park JU, Kook YA, Kim Y. Assessment of asymmetry in a normal occlusion sample and asymmetric patients with three-dimensional cone beam computed tomography: a study for a transverse reference plane. Angle Orthod. 2012;82:860–867. doi: 10.2319/102911-668.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blackwood HJ. Pathology of the temporomandibular joint. J Am Dent Assoc. 1969;79:118–124. doi: 10.14219/jada.archive.1969.0217. [DOI] [PubMed] [Google Scholar]
- 20.Westesson PL, Bifano JA, Tallents RH, Hatala MP. Increased horizontal angle of the mandibular condyle in abnormal temporomandibular joints. A magnetic resonance imaging study. Oral Surg Oral Med Oral Pathol. 1991;72:359–363. doi: 10.1016/0030-4220(91)90233-3. [DOI] [PubMed] [Google Scholar]
- 21.Ueki K, Nakagawa K, Takatsuka S, Shimada M, Marukawa K, Takazakura D, et al. Temporomandibular joint morphology and disc position in skeletal class III patients. J Craniomaxillofac Surg. 2000;28:362–368. doi: 10.1054/jcms.2000.0181. [DOI] [PubMed] [Google Scholar]
- 22.Ahn SJ, Lee SJ, Kim TW. Orthodontic effects on dentofacial morphology in women with bilateral TMJ disk displacement. Angle Orthod. 2007;77:288–295. doi: 10.2319/0003-3219(2007)077[0288:OEODMI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]