Abstract
Background and purpose
Rapid recovery protocols after total hip arthroplasty (THA) have been introduced worldwide in the last few years and they have reduced the length of hospital stay. We show the results of the introduction of a rapid recovery protocol for primary THA for unselected patients in our large teaching hospital.
Patients and methods
In a retrospective cohort study, we included all 1,180 patients who underwent a primary THA between July 1, 2008 and June 30, 2012. These patients were divided into 3 groups: patients operated before, during, and after the introduction of the rapid recovery protocol. There were no exclusion criteria. All complications, re-admissions, and reoperations were registered and analyzed.
Results
The mean length of hospital stay decreased from 4.6 to 2.9 nights after the introduction of the rapid recovery protocol. There were no statistically significant differences in the rate of complications, re-admissions, or reoperations between the 3 groups.
Interpretation
In a large teaching hospital, the length of hospital stay decreased after introduction of our protocol for rapid recovery after THA in unselected patients, without any increase in complications, re-admissions, or reoperation rate.
Historically, the length of hospital stay after primary THA has exceeded several weeks (Berger et al. 2009), with a subsequent period of bed rest. In the last few years, rapid recovery protocols have been introduced worldwide for elective primary THA. Various studies have shown that these protocols have reduced the length of hospital stay and the length of rehabilitation after primary THA (Weingarten et al. 1998, Dowsey et al. 1999, Husted and Holm 2006, Barbieri et al. 2009, Berger et al. 2009, Husted et al. 2008, 2010, 2011, 2012). Also a decrease in complication rate (Barbieri et al. 2009) and in re-admission rate (Dowsey et al. 1999) has been described. These rapid recovery protocols are based on analysis of clinical care principles and pain management in combination with revision of organizational factors, giving an optimized perioperative period that is safe for the patient (Kehlet and Wilmore 2002, Husted et al. 2012).
Reinier de Graaf Hospital (RdGG) is a large teaching hospital in the Netherlands. Introduction of the rapid recovery protocol for primary THA started in 2009, was done in several stages, and was complete in February 2011. In the present study, we analyzed the difference in length of hospital stay before, during, and after introduction of the rapid recovery protocol for primary THA procedures in a group of unselected patients at RdGG. We also examined the amount of complications, re-admissions, and reoperations for this group after introduction of the rapid recovery protocol.
Patients and methods
In this retrospective cohort study, we included all the patients who underwent a primary THA procedure between July 1, 2008 and June 30, 2012. There were no exclusion criteria; every patient who received a primary THA was included. The patients were divided into 3 groups, based on the period in which the surgery was performed. Group 1 had patients who were operated in the period before the rapid recovery protocol was introduced. Group 2 had patients who were operated between January 1, 2009 and January 31, 2011, during the period in which the rapid recovery protocol was introduced in several stages. Group 3 had patients who were operated after all the stages of the rapid recovery protocol had been introduced (Table 1).
Table 1.
The different stages of the rapid recovery protocol. Group 1 represents the patients who were operated in the period before the protocol was introduced. Group 2 represents the patients who were operated during the period in which the rapid recovery protocol was introduced in several stages. Group 3 represents the patients who were operated after all the stages of the rapid recovery protocol had been introduced
| • Preoperative education |
| • Local infiltration anesthesia |
| • Standardized protocol for pain medication |
| • Opioid medication only on request (rescue medication) |
| • No compression bandages |
| • No drains |
| • No standard urine catheters |
| • Start rehabilitation and mobilization on day of surgery |
| • Checking the fulfillment of discharge criteria twice a day |
| • Optimization of the aftercare |
All the patients had the same regimen. The discharge criteria were functional: patient able to walk 30 meters with crutches, to climb stairs, to dress independently, and to go to the toilet independently. In addition, sufficient pain treatment had to be achieved by oral medication before discharge, with VAS below 3 at rest and below 5 during mobilization.
Various surgical approaches were used—the straight lateral (SL) approach, the anterior supine intermuscular (ASI) approach, and the posterolateral (PL) approach—according to the preference of the surgeon. 15 orthopedic surgeons performed the THA procedures during this period, either by themselves or by supervising a resident in orthopedic surgery.
The fulfillment of discharge criteria was analyzed twice a day. Length of hospital stay was measured by number of nights. All patients were admitted on the day of surgery. Outliers in length of hospital stay were defined as being equal to or more than the ninety-fifth percentile. All outliers were registered, analyzed, and replaced with the ninety-fifth percentile. All complications, re-admissions, and reoperations were registered and analyzed.
Statistics
Since the data were not normally distributed according to the Kolmogorov-Smirnoff test, they were analyzed using the Kruskal-Wallis test and the Mann-Whitney test with Bonferroni correction. Values of p < 0.05 were considered significant. Data analysis was done with IBM SPSS Statistics for Mac, version 20.
Results
For the total group of 1,180 patients, the mean age was 71 (22–94) years. More women than men were operated (815 as opposed to 265). The main indication for operation was primary osteoarthritis (89%). Other indications were posttraumatic arthritis, fracture of the femoral neck, avascular necrosis, and development disorders. Mean BMI was 27 (17–58). The most common ASA classification was ASA II (66%). Spinal anesthesia was given in 88% of the cases. Almost all operations were performed in an elective setting (98%). Most patients were discharged postoperatively to their own home (81%); others went to a temporary nursing home for further rehabilitation (18%) or were discharged to another department of our hospital for treatment for non-orthopedic pathology (0.4%). The SL approach was mostly used, followed by the ASI approach and the PL approach. The demographic characteristics were equal for the 3 groups; only the surgical approach used was significantly different in groups 1 and 2 (Table 2).
Table 2.
Demographics. For an explanation of the 3 groups, see Table 1
| Group 1 | Group 2 | Group 3 | p-value | |
|---|---|---|---|---|
| Age (years) | 71 | 71 | 71 | 0.2 |
| SD | 10 | 9 | 10 | |
| Gender, % female | 68 | 69 | 69 | 1.0 |
| BMI, kg/m² | 26.7 | 27.1 | 26.9 | 0.3 |
| SD | 4.3 | 4.3 | 4.2 | |
| ASA classification | ||||
| I | 22 | 20 | 20 | 0.9 |
| II | 66 | 66 | 66 | |
| III | 13 | 14 | 14 | |
| IV | – | – | 0.3 | |
| Anesthesia, % spinal | 91 | 87 | 90 | 0.06 |
| Priority, % elective | 99 | 99 | 98 | 0.3 |
| Diagnosis, % primary | 93 | 88 | 88 | 0.2 |
| Direction of discharge, % | ||||
| home | 82 | 82 | 80 | 0.7 |
| TNH a | 19 | 18 | 19 | |
| AD b | – | 0.2 | 0.8 | |
| Approach, % | ||||
| ASI | 27 | 45 | 52 | < 0.001 |
| SL | 73 | 49 | 45 | |
| PL | – | 6 | 4 | |
| Side, % right | 56 | 55 | 55 | 1.0 |
TNH: temporary nursing home for further rehabilitation.
AD: another department of our hospital for treatment for non-orthopedic pathology.
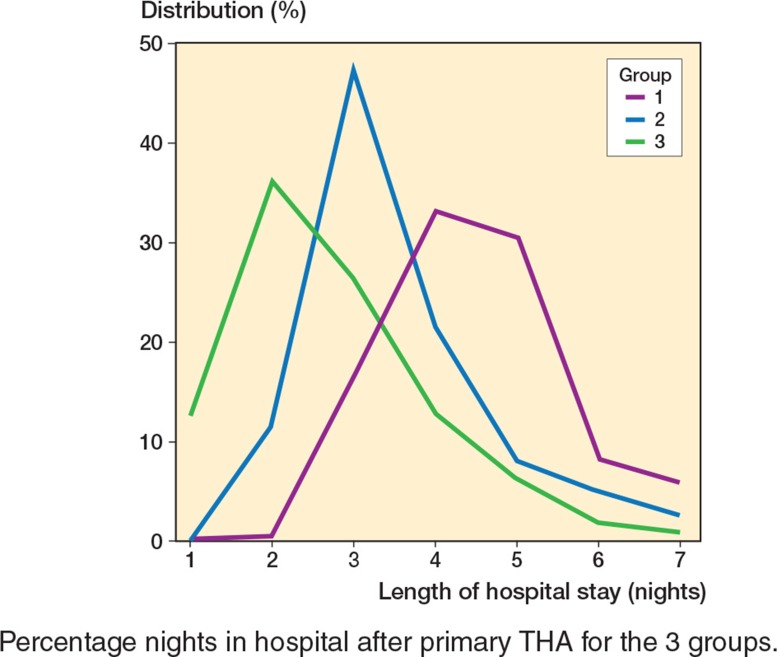
1,180 patients received a unilateral primary THA between July 1, 2008 and June 30, 2012. In group 1, 157 patients were operated with a mean length of hospital stay of 4.6 (SD 1.2) nights. Group 2 consisted of 639 patients with a mean hospital stay of 3.7 (SD 1.3) nights, and group 3 consisted of 384 patients with a mean hospital stay of 2.9 (SD 1.4) nights. The differences in length of hospital stay were statistically significant between all 3 groups (p < 0.001). Median length of hospital stay decreased from 4 nights to 3 nights after the introduction of the rapid recovery protocol (p < 0.001) (Table 3 and Figure).
Table 3.
Length of hospital stay, complications, re-admissions, and reoperations after primary THA
| Group 1 | Group 2 | Group 3 | p-value | |
|---|---|---|---|---|
| Length of hospital stay, days | ||||
| Mean | 4.6 | 3.7 | 2.9 | < 0.001 |
| SD | 1.2 | 1.3 | 1.4 | < 0.001 |
| Median | 4 | 3 | 3 | < 0.001 |
| Complications, % | 7.6 | 7.0 | 7.8 | 0.9 |
| Re-admissions in < 3 months, % | 4.5 | 3.4 | 4.4 | 0.7 |
| Reoperations, % | 7.0 | 4.4 | 3.9 | 0.3 |
| Reoperations in < 3 months, % | 3.8 | 2.3 | 2.9 | 0.5 |
Percentage nights in hospital after primary THA for the 3 groups.
For the total group of 1,180 patients, 3.9% were re-admitted and 2.7% of them underwent a reoperation within the first 3 months after primary THA. The total reoperation rate was 4.6%. There was a decrease in re-admission rate and reoperation rate within the first 3 months after surgery and also a decrease in reoperation rate in total, after the introduction of the rapid recovery protocol, but these decreases were not statistically significant (Table 3).
Complications after primary THA occurred in 7.4% of the 1,180 patients, with no statistically significant differences between the 3 groups. The most common reason for both re-admission and reoperation within the first 3 months was infection, followed by dislocation, wound problems, and fracture of the femur (Table 4).
Table 4.
Reasons for re-admission within the first 3 months after primary THA
| Group 1 n = 157 |
Group 2 n = 639 |
Group 3 n = 384 |
|
|---|---|---|---|
| Infection | 5 (3.2%) | 6 (0.9%) | 7 (1.8%) |
| Dislocation | 2 (1.3%) | 9 (1.4%) | 3 (0.8%) |
| Fracture | – | 2 (0.3%) | – |
| Wound problems | – | 5 (0.8%) | 2 (0.5%) |
| Malposition of prosthesis | – | – | 1 (0.3%) |
| Anemia | – | – | 3 (0.8%) |
| Pain, unknown cause | – | – | 1 (0.3%) |
| Total | 7 (4.5%) | 22 (3.4%) | 17 (4.4%) |
In group 1 there were 17 outliers in length of hospital stay (11%), in group 2 there were 41 outliers (6%), and in group 3 there were 15 outliers (4%). Most outliers in group 1 had a prolonged hospital stay without any reason given in the patient charts.
Discussion
Our findings of reduced length of hospital stay for primary THA after introduction of a rapid recovery protocol are in accordance with the results of various other studies (Husted and Holm 2006, Barbieri et al. 2009, Husted et al. 2008, 2010, 2011, 2012).
We found a decrease in re-admission rate and reoperation rate within the first 3 months after surgery, and also a decrease in reoperation rate in total, but these decreases were not statistically significant. This contrasts with previous studies showing a significant reduction in complication rate (Barbieri et al. 2009) and re-admission rate (Dowsey et al. 1999) within the first 3 months after THA after the introduction of a rapid recovery protocol. However, our re-admission rates were less than described in other studies even though the reasons for re-admission were the same (Mahomed et al. 2003, Cullen et al. 2006, Husted and Holm 2006, Husted et al. 2008, 2010). Our reoperation rate is in accordance with the only other study that published the reoperation rate for primary THA after the introduction of a rapid recovery protocol (Husted et al. 2008).
The proportion of patients discharged to their own home or discharged to a temporary nursing home for further rehabilitation did not change after the introduction of the rapid recovery protocol. This is in accordance with the results of a meta-analysis (Barbieri et al. 2009), although another study showed a decrease in patients discharged to their own home after the length of hospital stay decreased (Weingarten et al. 1998).
For group 1, there were 17 outliers in length of hospital stay (10.8%), for group 2 there were 41 outliers (6.4%), and for group 3 there were 15 outliers (3.9%). These outliers were mainly for medical reasons. The introduction of pre-emptive delirium therapy for patients at risk reduced the prevalence of delirium and therefore reduced the length of prolonged hospital stay. This could explain the decline in outliers after the introduction of the rapid recovery protocol. However, postoperative delirium still occurred after the introduction of the rapid recovery protocol, although lack of postoperative delirium has been described in fast track THA and total knee artoplasty as well (Krenk et al. 2012). A possible reason for this occurrence could be the use of tramadol and piritramide in our standardized protocol for pain medication, both of which are opioids.
In conclusion, in our large teaching hospital implementation of the rapid recovery protocol led to a decrease in length of hospital stay for unselected THA patients, without any change in complication rate, re-admission rate, or reoperation rate. The re-admission rate was less than reported in other studies, but the reoperation rate was similar to that in other studies.
Acknowledgments
YH coordinated the study and drafted the manuscript. NM assisted in performing the analysis and in drafting the manuscript. All authors read and approved the final manuscript.
SV has a consultant contract with Biomet.
References
- Barbieri A, Vanhaecht K, Van Herck P, Sermeus W, Faggiano F, Marchisio S, Panella M. Effects of clinical pathways in the joint replacement: a meta-analysis . BMC Med. 2009;7:32. doi: 10.1186/1741-7015-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger RA, Sanders SA, Thill ES, Sporer SM, Della Valle C. Newer anesthesia and rehabilitation protocols enable outpatient hip replacement in selected patients . Clin Orthop. 2009;6(467):1424–30. doi: 10.1007/s11999-009-0741-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen C, Johnson DS, Cook G. Re-admission rates within 28 days of total hip replacement . Ann R Coll Surg Engl. 2006;88(5):475–8. doi: 10.1308/003588406X116909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowsey MM, Kilgour ML, Santamaria NM, Choong PF. Clinical pathways in hip and knee arthroplasty: a prospective randomised controlled study . Med J Aust. 1999;170(2):59–62. doi: 10.5694/j.1326-5377.1999.tb126882.x. [DOI] [PubMed] [Google Scholar]
- Husted H, Holm G. Fast track in total hip and knee arthroplasty--experiences from Hvidovre University Hospital . Denmark. Injury (Suppl 5) 2006;37:S31–5. doi: 10.1016/S0020-1383(07)70009-8. [DOI] [PubMed] [Google Scholar]
- Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients . Acta Orthop. 2008;79(2):168–73. doi: 10.1080/17453670710014941. [DOI] [PubMed] [Google Scholar]
- Husted H, Otte KS, Kristensen BB, Orsnes T, Kehlet H. Readmissions after fast-track hip and knee arthroplasty . Arch Orthop Trauma Surg. 2010;130(9):1185–91. doi: 10.1007/s00402-010-1131-2. [DOI] [PubMed] [Google Scholar]
- Husted H, Lunn TH, Troelsen A, Gaarn-Larsen L, Kristensen BB, Kehlet H. Why still in hospital after fast-track hip and knee arthroplasty? . Acta Orthop. 2011;82(6):679–84. doi: 10.3109/17453674.2011.636682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husted H, Jensen CM, Solgaard S, Kehlet H. Reduced length of stay following hip and knee arthroplasty in Denmark 2000-2009: from research to implementation . Arch Orthop Trauma Surg. 2012;132(1):101–4. doi: 10.1007/s00402-011-1396-0. [DOI] [PubMed] [Google Scholar]
- Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome . Am J Surg. 2002;183(6):630–41. doi: 10.1016/s0002-9610(02)00866-8. [DOI] [PubMed] [Google Scholar]
- Krenk L, Rasmussen LS, Hansen TB, Bogø S, Søballe K, Kehlet H. Delirium after fast-track hip and knee arthroplasty . Br J Anaesth. 2012;108(4):607–11. doi: 10.1093/bja/aer493. [DOI] [PubMed] [Google Scholar]
- Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Rates and outcomes of primary and revision total hip replacement in the United States medicare population . J Bone Joint Surg (Am) 2003;85(1):27–32. doi: 10.2106/00004623-200301000-00005. [DOI] [PubMed] [Google Scholar]
- Weingarten S, Riedinger MS, Sandhu M, Bowers C, Ellrodt AG, Nunn C, Hobson P, Greengold N. Can practice guidelines safely reduce hospital length of stay? Results from a multicenter interventional study . Am J Med. 1998;105(1):33–40. doi: 10.1016/s0002-9343(98)00129-6. [DOI] [PubMed] [Google Scholar]