Abstract
Background and purpose
Humeral resurfacing has shown promising results for osteoarthritis, but revisions for glenoid erosion have been reported frequently. We investigated the hypothesis that preoperative glenoid wear and postoperative progress of glenoid erosion would influence the clinical outcome.
Methods
We reviewed 61 resurfacing hemiarthroplasties (55 patients) for primary osteoarthritis. 6 patients were lost to follow-up and 5 had undergone revision arthroplasty. This left 50 shoulders in 44 patients (mean age 66 years) that were followed for mean 30 (12–44) months. Complications, revisions, and the age- and sex-related Constant score were assessed. Radiographs were evaluated for loosening and glenoid erosion according to Walch.
Results
Of the 50 shoulders that were functionally assessed, the average age- and sex-related Constant score was 73%. In patients with preoperative type-B2 glenoids, at 49% it was lower than in type-A1 glenoids (81%, p = 0.03) and in type-B1 glenoids (84%, p = 0.02). The average age- and sex-related Constant score for patients with type-A2 glenoids (60%) was lower than for type-A1 and -B1 glenoids and higher than for type-B2 glenoids, but the differences were not statistically significant. In the total population of 61 shoulders, the radiographs showed postoperative glenoid erosion in 38 cases and no humeral prosthetic loosening. Revision arthroplasty was performed in 11 cases after 28 (7–69) months. The implant size had no statistically significant influence on the functional outcome. The size was considered to be adequate in 28 of the 50 functionally assessed shoulders. In 21 cases, the implant size was too large and in 1 case it was too small.
Interpretation
We found frequent postoperative glenoid erosion and a high rate of revision arthroplasty after humeral resurfacing for primary osteoarthritis. Oversizing of the implants was common, but it had no statistically significant influence on the functional outcome. Inferior results were found in the presence of increased eccentric preoperative glenoid wear. Total shoulder arthroplasty should be considered in these patients.
Humeral resurfacing arthroplasty has been described as a successful treatment option for many indications such as osteoarthritis, avascular necrosis, rheumatoid arthritis, cuff tear arthropathy, and posttraumatic arthritis (Alund et al. 2000, Levy and Copeland 2001, 2004. Fink et al. 2004, Levy et al. 2004, Thomas et al. 2005, Fuerst et al. 2007, Jensen 2007, Jerosch et al. 2008, Burgess et al. 2009, Raiss et al. 2009, Pape et al. 2010, Pritchett 2011). Some authors have reported that the individual anatomy of the humerus is maintained regarding inclination angle, offset, and version (Levy and Copeland 2001,Thomas et al. 2005, Copeland 2006, Burgess et al. 2009). The procedure has advantages compared to stemmed hemiarthroplasty because the bone stock is preserved and intraoperative humeral fractures are avoided (Levy and Copeland 2001, Burgess et al. 2009).
However, glenoid wear has been found to be a critical factor influencing patient outcome after stemmed hemiarthroplasty (Boyd et al.1990, Levine et al. 1997, Gartsman et al. 2000, Hasan et al. 2002, Parsons et al. 2004, Rispoli et al. 2006, Radnay et al. 2007). For osteoarthritis, overall promising results were published for total resurfacing and hemiresurfacing (Levy and Copeland 2001, 2004, Rispoli et al. 2006, Pritchett 2011), but revisions have been reported for glenoid erosion, and the preoperative glenoid wear status has influenced the individual indication for glenoid replacement (Levy and Copeland 2001, 2004, Bailie et al. 2008, Buchner et al. 2008, Burgess et al. 2009, Pritchett 2011).
This retrospective study was conducted in order to determine the outcome of humeral resurfacing arthroplasty for primary osteoarthritis as related to the preoperative centering of the humeral head and glenoid erosion. We investigated the hypothesis that preoperative glenoid wear influences the results after humeral resurfacing.
Patients and methods
We conducted a retrospective study of patients who had undergone cementless hydroxyapatite-coated humeral resurfacing arthroplasty (Global C.A.P., DePuy Orthopaedics Inc., Warsaw, IN) at our institution. The study protocol was approved by the institutional ethical committee of Hanover Medical School (study number 731) and all enrolled patients provided informed consent for the follow-up examinations. Between 2004 and 2009, 61 consecutive hemiarthroplasties (in 55 patients) were performed for primary osteoarthritis. 6 patients were lost to follow-up and 5 had undergone revision shoulder arthroplasty by the time of the review. This left 50 shoulders (6 bilateral) in 44 patients (21 females and 23 males) for functional assessment. In the total population of 61 shoulders, the mean age of the patients was 66 (45–85) years. The mean time between surgery and final review was 30 (12–44) months. All 50 functionally assessed shoulders were evaluated postoperatively using the Constant score (Constant and Murley 1987, Constant 1997) adjusted for age and gender. Range of motion was measured using a goniometer, while strength was measured with the Iso Force Control unit (MDS AG, Oberburg, Switzerland).
Routine antero-posterior and axillary radiographs were taken preoperatively, at the first postoperative visit, at 3 months, at 1 year, and then annually thereafter. They were evaluated by 2 independent observers for centering of the humeral head, implant size and position, and signs of loosening according to Throckmorton et al. (2010). The degree of osteoarthritis was determined according to the criteria described by Samilson and Prieto (1983). Preoperative glenoid wear patterns were classified on the basis of the criteria described by Walch et al. (1999).
The indications for humeral resurfacing included pain and reduced function after failed closed treatment. In the time period between 2004 and 2009, humeral resurfacing was the standard prosthetic treatment for primary osteoarthritis at our institution, and no parallel series of stemmed arthroplasties or glenoid replacements was used. Patients with posttraumatic arthritis, cuff tear arthropathy, rheumatoid arthritis and avascular necrosis were excluded.
Surgical procedure
The procedures were performed in the beach-chair position with general anesthesia in combination with an interscalene catheter. A deltopectoral approach 4–5 inches in length was used. The subscapularis was incised vertically close to the lesser tuberosity, and the tendon of the long head of the biceps was tenodesed in the bicipital groove with sutures. An anterior and inferior humeral sided capsular release was performed in order to deliver the humeral head out of the wound. Osteophytes were removed and the head size was measured. The glenoid surface was only inspected and the labrum was left intact. A guide-wire was placed in the humeral head in anatomic inclination and retroversion and the surface was reamed to the appropriate size. A cruciform path for the central stem of the prosthesis was prepared in order to improve rotational stability, and the final hydroxyapatite-coated humeral resurfacing implant was seated. The subscapularis was re-attached to the lesser tuberosity with transosseous non-absorbable sutures and the wound was closed.
After the operation, the patients underwent a standard rehabilitation program. The arm was placed in a splint in 15° of abduction for 4 weeks. Active assisted exercises with limitation of abduction and forward flexion to 90° were allowed and the subscapularis was protected during the first 6 weeks after surgery. This involved restriction of active internal rotation and limitation of external rotation within 20° of the maximal external rotation obtained during the operative procedure after subscapularis tendon repair. Strengthening exercises of the rotator cuff, deltoid, and scapular muscles were started 6 weeks after surgery. This program progressed as tolerated during the next 3–6 months.
Statistics
Paired t-tests were used to test for differences between the follow-up scores of the different osteoarthritis stages and glenoid types measured with the outcome scores. The level of significance was set at p = 0.05 with use of a Bonferroni adjustment. All analyses were performed using PASW Statistics 18.
Results
Preoperative radiographic assessment
In the total population of 61 shoulders, 12 patients were graded as mild cases of osteoarthritis (S1, osteophytes < 3 mm) according to the Samilson and Prieto classification (1983), 18 patients as moderate cases (S2, osteophytes 3–7 mm), and 31 patients as severe cases of osteoarthritis (S3, osteophytes > 7 mm). According to Walch et al. (1999), 38 shoulders had a concentric glenohumeral relationship of type A, 24 cases were type A1 with mild erosion, and 14 cases were type A2 with severe erosion of the glenoid. In 23 cases, the glenohumeral relationship showed a posterior subluxation of the humeral head of type B, 15 cases were type B1 with mild posterior erosion, and 8 cases were type B2 with advanced biconcave posterior erosion of the glenoid surface. No type-C glenoids were found.
Functional outcome
Of the 50 shoulders that were functionally assessed, the average age- and sex-adjusted Constant score was 73% (SD 27) after a mean follow-up period of 30 months. The results were also evaluated according to the stage of osteoarthritis using the radiological classification by Samilson and Prieto (1983). The age- and sex-adjusted Constant score for stage 1 was 76% (SD 23), for stage 2 it was 72% (SD 27), and for stage 3 it was 74% (SD 29). The differences between stages 1–3 were not statistically significant. The average age- and sex-adjusted Constant scores for patients with type-B2 glenoids were lower than for patients with type-A1 glenoids and for type-B1 glenoids (Table 1). The average age- and sex-adjusted Constant score value for patients with type-A2 glenoids was lower than for type-A1 and -B1 glenoids and higher than for type-B2 glenoids, but the differences were not statistically significant (Table 2).
Table 1.
Age- and sex-related follow-up Constant score results according to the glenoid type
| Glenoid type | n | Mean Constant score, % (SD) | Range, % |
|---|---|---|---|
| A1 | 21 | 81 (22) | 35–113 |
| A2 | 9 | 60 (31) | 22–114 |
| B1 | 13 | 84 (25) | 30–115 |
| B2 | 7 | 49 (20) | 23–74 |
| Total | 50 | 73 (27) | 22–115 |
Table 2.
Comparative functional age- and sex-related Constant score differences (%) according to the glenoid type
| Glenoid type | Glenoid type compared | Mean difference, % | p-value |
|---|---|---|---|
| A1 | –31 | 0.03 | |
| B2 | A2 | –11 | 1.0 |
| B1 | –35 | 0.02 |
Regarding the 50 functionally assessed shoulders, 6 patients had undergone bilateral humeral resurfacing. The comparison between the 38 unilaterally and 6 bilaterally operated patients showed no statistically significant difference in the average age- and gender-adjusted Constant score value (72% (SD 6) vs. 78% (SD 31); p = 0.5).
The correctness of the implant size had no significant influence on the functional outcome. The average age- and sex-adjusted Constant score value for the correctly-sized shoulders was 71% (SD 26), as opposed to 77% (SD 29) for the inadequately-sized shoulders (p = 0.5).
Complications and reoperations (61 shoulders)
1 intraoperative diaphyseal fracture of the humerus was treated by plate osteosynthesis. The further recovery of this patient was unremarkable. Other major early complications such as injury of neurovascular structures or gross malpositioning of the implants did not occur. In 1 case, a deep hematoma developed and required revision 7 days after surgery. 1 early infection was revised successfully 20 days postoperatively without implant removal. In 5 cases, arthrofibrosis developed, defined as substantial loss of motion that did not respond to closed treatment for 3 months. These patients underwent arthroscopic capsular release with good functional results. Revision arthroplasty was performed in 11 cases after 28 (7–69) months. At the time of the final follow-up, 5 patients had already undergone revision arthroplasty; in 6 cases the revisions were carried out later. In 4 cases, a reverse shoulder was indicated. In 1 case, a 2-stage revision to a reverse shoulder was performed for a late prosthetic infection 36 months postoperatively. In 1 case, a traumatic massive rotator cuff tear occurred 3 months after humeral resurfacing and was revised to a reverse shoulder arthroplasty. 2 patients with severe glenoid erosion and rotator cuff scarring were converted to a reverse shoulder implant. 7 cases with intact rotator cuff status but glenoid erosion and persistent pain underwent revision to anatomic stemmed total shoulder arthroplasty with good results.
Postoperative radiographic results
In the total population of 61 shoulders, radiographs showed no signs of loosening at the time of final follow-up. The size of the implants chosen was considered to be adequate in 28 of the 50 functionally assessed shoulders. In 21 cases, the implant size was too large and in 1 case it was too small. Only 1 case showed superior migration of the humeral head after a traumatic massive rotator cuff tear and was revised to a reverse prosthesis 3 months after humeral resurfacing. The qualitative review of the radiographs (i.e. without specific measurements) of all 61 osteoarthritis patients showed increased postoperative glenoid erosion in 38 cases at the time of the last follow-up examination (Figure A–D). Of the 11 cases of revision arthroplasty, 8 had glenoid erosion. There was no statistically significant correlation between the frequency of revision arthroplasty procedures and the different glenoid types according to Walch et al. (1999), the stages of osteoarthritis according to Samilson and Prieto (1983), or the correctness of the implant size chosen.
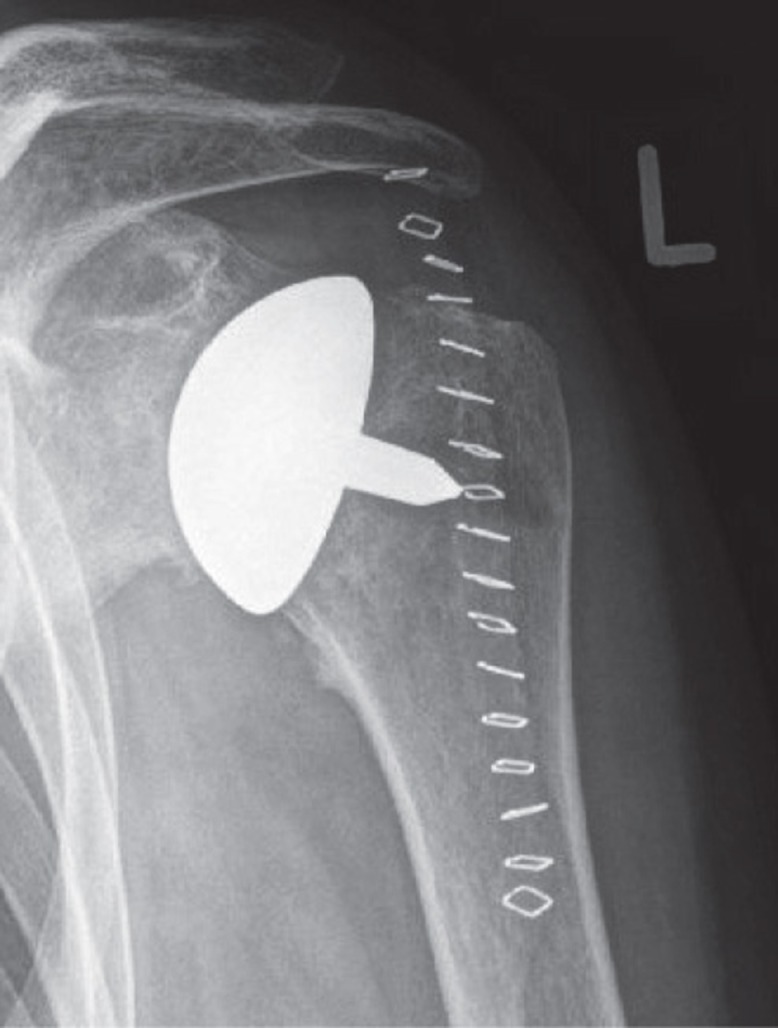
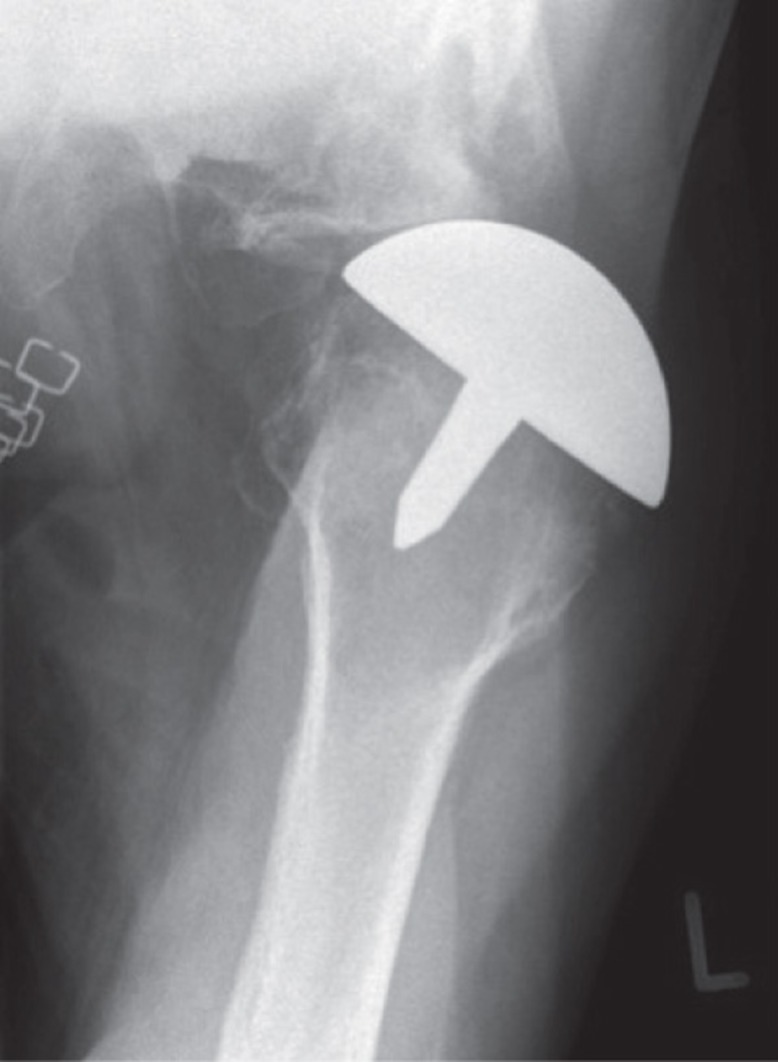

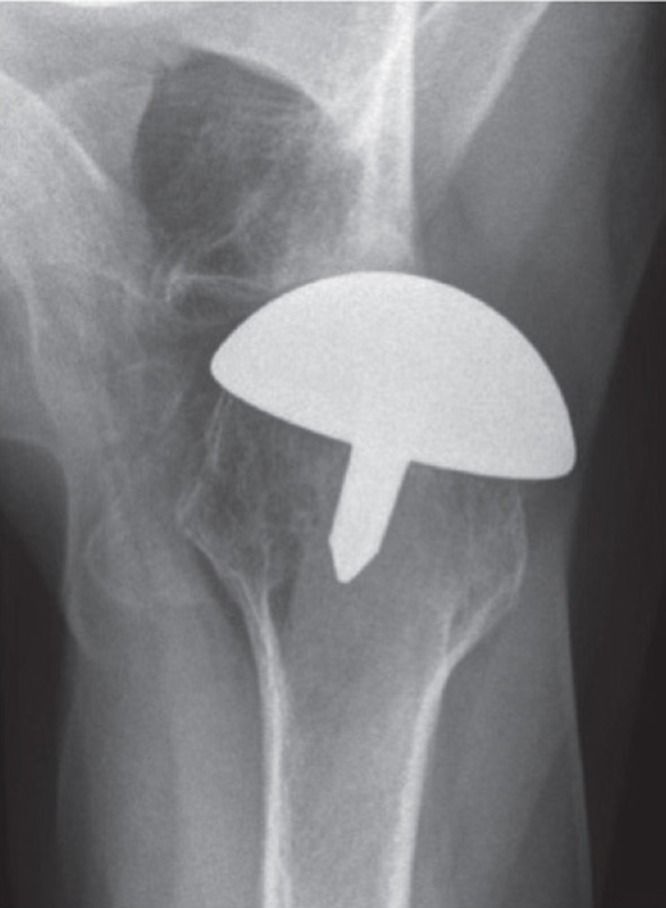
A. Antero-posterior view 2 days postoperatively. B. Axial view 2 days postoperatively, with posterior subluxation of the humeral head. C. Antero-posterior view 2 years postoperatively, with increased glenoid erosion and medialization of the joint line. D. Axial view 2 years postoperatively, with posterior subluxation of the humeral head and increased posterior glenoid erosion.
Discussion
We found that preoperative glenoid wear had a negative influence on the patient outcome after humeral resurfacing for primary osteoarthritis, and the rate of revision arthroplasty was high. The functional results were inferior in the presence of preoperative type-B2 glenoid. These results confirm previous reports after stemmed hemiarthroplasty for primary osteoarthritis (Boyd et al. 1990, Levine et al. 1997, Gartsman et al. 2000, Hasan et al. 2002, Parsons et al. 2004, Rispoli et al. 2006, Radnay et al. 2007). With longer follow-up, increasing pain and the radiographic appearance of both subchondral sclerosis of the glenoid and joint space narrowing have been reported (Boyd et al. 1990). In the series of Levine et al. (1997), patients with non-concentric glenoids had a higher rate of unsatisfactory results than with concentric glenoids and the outcome was found to be strongly correlated with the preoperative status of posterior glenoid wear.
Numerous studies have shown that the results of stemmed shoulder implants are improved if the glenoid is replaced (Boyd et al. 1990, Sperling et al. 1998, Gartsman et al. 2000, Radnay et al. 2007, Buchner et al. 2008, Burgess et al. 2009). For resurfacing arthroplasty, there is controversy about whether a glenoid component must be implanted, and surgical access may be difficult (Burgess et al. 2009). Levy and Copeland (2001) published results for a series of 41 patients with primary osteoarthritis. The age- and gender-adjusted Constant scores were 94% for total resurfacing and 74% for hemiresurfacing, which is comparable with our results for hemiresurfacing (74%). In their early patients, a total replacement was attempted in all patients and the glenoid component was only omitted if adequate fixation could not be achieved. Later in the study, hemiarthroplasty was preferred and a glenoid implant was only added where there was a non-concentric glenoid shape. In 2004, the same authors reported on 42 total resurfacing and 37 hemiresurfacing arthroplasties for primary osteoarthritis, and the age-adjusted Constant score improved to 94% for total resurfacing and to 91% for hemiresurfacing arthroplasty. The authors concluded that the results in this series were comparable, and that it seemed to be reasonable to perform hemiarthroplasty unless there were specific indications for insertion of a glenoid component (non-concentric erosion or saddle-shaped erosion of the glenoid). This indicates that glenoid wear influenced the treatment algorithm in both series (Levy and Copeland 2001, 2004). Buchner et al. (2008) performed a matched-pair analysis of the short-term functional results after 22 humeral surface replacements and 22 stemmed total shoulder arthroplasties for osteoarthritis. Patients with type-B2 and type-C glenoids according to Walch were excluded, and better outcome was obtained in the total shoulder arthroplasty group. In their series, 2 patients required conversion to a total shoulder arthroplasty due to glenoid erosion and both had been classified preoperatively as type B1. The authors concluded that hemiresurfacing arthroplasty should not be performed in cases with subluxation of the humeral head and damage or biconcavity of the glenoid.
In the present study, the functional results were inferior with type B2 glenoids compared to type A1 and B1 glenoids, and also the frequency of increased glenoid erosion and revision arthroplasty were remarkably high. In contrast, Mansat et al. (2013) did not find any correlation between the preoperative glenoid type according to Walch and the functional outcome, but medialization of the humerus with glenoid wear was observed with further follow-up, which was correlated in some patients with reappearance of pain.
Some authors reported that the individual anatomy of the humerus is maintained regarding inclination angle, offset, and version (Levy and Copeland 2001, Thomas et al. 2005, Copeland 2006, Burgess et al. 2009). In contrast, Mechlenburg et al. (2013) found an increased offset after humeral resurfacing with the Copeland cup implant, causing overstuffing of the joint.
In the study by Mansat et al. (2013), the postoperative radiographs showed a decrease in humeral head diameter and in the height of the humeral head, without modification of the radius of curvature or the height of the center of rotation. The humeral offset was increased and the implants were mainly positioned in varus postoperatively. In contrast to our study, the implant size was often too small compared to the preoperative humeral diameter. However, in accordance with our findings, the implant size did not influence the postoperative functional outcome.
The present study had some limitations. We had no control group after stemmed hemiarthroplasty or after nonoperative treatment, and the duration of follow-up was limited. Despite our relatively large total series of osteoarthritis patients after humeral resurfacing, the subgroups investigated according to the Walch and the Samilson and Prieto classification were small. Larger prospective randomized studies are needed to investigate the effectiveness of humeral resurfacing compared to stemmed hemiarthroplasty. Furthermore, the quantity of glenoid bone loss could not be exactly measured on plain radiographs. For this purpose, the comparison of preoperative and postoperative CT scans would have been necessary.
In our series, the indication for resurfacing arthroplasty was not primarily because of a potentially higher risk of later revision, since it was our standard treatment for primary osteoarthritis. However, the threshold for revision surgery may perhaps have been lower in our series, since the removal of a resurfacing implant is usually less complicated than that of a stemmed implant.
In this study, preoperative glenoid wear had a negative effect on patient outcome after humeral resurfacing for primary osteoarthritis, and the high rate of revision arthroplasty gives cause for concern. We have therefore modified the treatment algorithm at our institution, and the indication for humeral resurfacing is restricted to mild cases of osteoarthritis with Walch type-A1 glenoids. Otherwise, we perform stemmed total shoulder arthroplasty.
Acknowledgments
TS wrote the manuscript, operated on most of the patients, and evaluated all the patients. AG and FP examined patients and reviewed the manuscript. MW examined patients, reviewed the manuscript, and did the radiographic analysis together with MS. MS examined patients, reviewed the manuscript, contributed to the statistical analysis, and was involved in the radiographic evaluation.
No competing interests declared.
References
- Alund M, Hoe-Hansen C, Tillander B, Heden BA, Norlin R. Outcome after cup hemiarthroplasty in the rheumatoid shoulder: a retrospective evaluation of 39 patients followed for 2-6 years . Acta Orthop Scand. 2000;71:180–4. doi: 10.1080/000164700317413166. [DOI] [PubMed] [Google Scholar]
- Bailie DS, Llinas PJ, Ellenbecker TS. Cementless humeral resurfacing arthroplasty in active patients less than fifty-five years of age . J Bone Joint Surg (Am) 2008;90:110–7. doi: 10.2106/JBJS.F.01552. [DOI] [PubMed] [Google Scholar]
- Boyd AD. Jr., Thomas WH, Scott RD, Sledge CB, Thornhill TS. Total shoulder arthroplasty versus hemiarthroplasty. Indications for glenoid resurfacing . J Arthroplasty. 1990;5:329–36. doi: 10.1016/s0883-5403(08)80092-7. [DOI] [PubMed] [Google Scholar]
- Buchner M, Eschbach N, Loew M. Comparison of the short-term functional results after surface replacement and total shoulder arthroplasty for osteoarthritis of the shoulder: a matched-pair analysis . Arch Orthop Trauma Surg. 2008;128:347–54. doi: 10.1007/s00402-007-0404-x. [DOI] [PubMed] [Google Scholar]
- Burgess DL, McGrath MS, Bonutti PM, Marker DR, Delanois RE, Mont MA. Shoulder resurfacing . J Bone Joint Surg (Am) 2009;91:1228–38. doi: 10.2106/JBJS.H.01082. [DOI] [PubMed] [Google Scholar]
- Constant CR. An evaluation of the Constant-Murley shoulder assessment . J Bone Joint Surg (Br) 1997;79:695–6. [PubMed] [Google Scholar]
- Constant CR, Murley AH. A clinical method of functional assessment of the shoulder . Clin Orthop. 1987;(214):160–4. [PubMed] [Google Scholar]
- Copeland S. The continuing development of shoulder replacement: “reaching the surface” . J Bone Joint Surg (Am) 2006;88:900–5. doi: 10.2106/JBJS.F.00024. [DOI] [PubMed] [Google Scholar]
- Fink B, Singer J, Lamla U, Ruther W. Surface replacement of the humeral head in rheumatoid arthritis . Arch Orthop Trauma Surg. 2004;124:366–73. doi: 10.1007/s00402-004-0661-x. [DOI] [PubMed] [Google Scholar]
- Fuerst M, Fink B, Ruther W, The J Bone Joint Surg (Am) 2007;89:1756–62. doi: 10.2106/JBJS.F.01290. DUROM cup humeral surface replacement in patients with rheumatoid arthritis. [DOI] [PubMed] [Google Scholar]
- Gartsman GM, Roddey TS, Hammerman SM. Shoulder arthroplasty with or without resurfacing of the glenoid in patients who have osteoarthritis . J Bone Joint Surg (Am) 2000;82:26–34. doi: 10.2106/00004623-200001000-00004. [DOI] [PubMed] [Google Scholar]
- Hasan SS, Leith JM, Campbell B, Kapil R, Smith KL, Matsen FA. III. Characteristics of unsatisfactory shoulder arthroplasties . J Shoulder Elbow Surg. 2002;11:431–41. doi: 10.1067/mse.2002.125806. [DOI] [PubMed] [Google Scholar]
- Jensen KL. Humeral resurfacing arthroplasty: rationale, indications, technique, and results . Am J Orthop (Belle Mead NJ) 2007;36:4–8. [PubMed] [Google Scholar]
- Jerosch J, Schunck J, Morsy MG. Shoulder resurfacing in patients with rotator cuff arthropathy and remaining subscapularis function . Z Orthop Unfall. 2008;146:206–10. doi: 10.1055/s-2007-989313. [DOI] [PubMed] [Google Scholar]
- Levine WN, Djurasovic M, Glasson JM, Pollock RG, Flatow EL, Bigliani LU. Hemiarthroplasty for glenohumeral osteoarthritis: results correlated to degree of glenoid wear . J Shoulder Elbow Surg. 1997;6:449–54. doi: 10.1016/s1058-2746(97)70052-1. [DOI] [PubMed] [Google Scholar]
- Levy O, Copeland SA. Cementless surface replacement arthroplasty of the shoulder. 5- to 10-year results with the Copeland mark-2 prosthesis . J Bone Joint Surg (Br) 2001;83:213–21. doi: 10.1302/0301-620x.83b2.11238. [DOI] [PubMed] [Google Scholar]
- Levy O, Copeland SA. Cementless surface replacement arthroplasty (Copeland CSRA) for osteoarthritis of the shoulder . J Shoulder Elbow Surg. 2004;13:266–71. doi: 10.1016/j.jse.2004.01.005. [DOI] [PubMed] [Google Scholar]
- Levy O, Funk L, Sforza G, Copeland SA. Copeland surface replacement arthroplasty of the shoulder in rheumatoid arthritis . J Bone Joint Surg (Am) 2004;86:512–8. doi: 10.2106/00004623-200403000-00008. [DOI] [PubMed] [Google Scholar]
- Mansat P, Coutie AS, Bonnevialle N, Rongieres M, Mansat M, Bonnevialle P. Resurfacing humeral prosthesis: do we really reconstruct the anatomy? . J Shoulder Elbow Surg. 2013;22:612–9. doi: 10.1016/j.jse.2012.07.014. [DOI] [PubMed] [Google Scholar]
- Mechlenburg I, Amstrup A, Klebe T, Jacobsen SS, Teichert G, Stilling M. The Copeland resurfacing humeral head implant does not restore humeral head anatomy. A retrospective study . Arch Orthop Trauma Surg. 2013;133:615–9. doi: 10.1007/s00402-013-1715-8. [DOI] [PubMed] [Google Scholar]
- Pape G, Zeifang F, Bruckner T, Raiss P, Rickert M, Loew M. Humeral surface replacement for the sequelae of fractures of the proximal humerus . J Bone Joint Surg (Br) 2010;92:1403–9. doi: 10.1302/0301-620X.92B10.24316. [DOI] [PubMed] [Google Scholar]
- Parsons IM, Millett PJ, Warner JJ. Glenoid wear after shoulder hemiarthroplasty: quantitative radiographic analysis . Clin Orthop. 2004;(421):120–5. doi: 10.1097/01.blo.0000119249.61696.f1. [DOI] [PubMed] [Google Scholar]
- Pritchett JW. Long-term results and patient satisfaction after shoulder resurfacing . J Shoulder Elbow Surg. 2011;20:771–7. doi: 10.1016/j.jse.2010.08.014. [DOI] [PubMed] [Google Scholar]
- Radnay CS, Setter KJ, Chambers L, Levine WN, Bigliani LU, Ahmad CS. Total shoulder replacement compared with humeral head replacement for the treatment of primary glenohumeral osteoarthritis: a systematic review . J Shoulder Elbow Surg. 2007;16:396–402. doi: 10.1016/j.jse.2006.10.017. [DOI] [PubMed] [Google Scholar]
- Raiss P, Aldinger PR, Kasten P, Rickert M, Loew M. Humeral head resurfacing for fixed anterior glenohumeral dislocation . Int Orthop. 2009;33:451–6. doi: 10.1007/s00264-007-0487-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rispoli DM, Sperling JW, Athwal GS, Schleck CD, Cofield RH. Humeral head replacement for the treatment of osteoarthritis . J Bone Joint Surg (Am) 2006;88:2637–44. doi: 10.2106/JBJS.E.01383. [DOI] [PubMed] [Google Scholar]
- Samilson RL, Prieto V. Dislocation arthropathy of the shoulder . J Bone Joint Surg (Am) 1983;65:456–60. [PubMed] [Google Scholar]
- Sperling JW, Cofield RH, Rowland CM. Neer hemiarthroplasty and Neer total shoulder arthroplasty in patients fifty years old or less. Long-term results . J Bone Joint Surg (Am) 1998;80:464–73. doi: 10.2106/00004623-199804000-00002. [DOI] [PubMed] [Google Scholar]
- Thomas SR, Wilson AJ, Chambler A, Harding I, Thomas M. Outcome of Copeland surface replacement shoulder arthroplasty . J Shoulder Elbow Surg. 2005;14:485–91. doi: 10.1016/j.jse.2005.02.011. [DOI] [PubMed] [Google Scholar]
- Throckmorton TW, Zarkadas PC, Sperling JW, Cofield RH. Radiographic stability of ingrowth humeral stems in total shoulder arthroplasty . Clin Orthop. 2010;(468):2122–8. doi: 10.1007/s11999-010-1299-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walch G, Badet R, Boulahia A, Khoury A. Morphologic study of the glenoid in primary glenohumeral osteoarthritis . J Arthroplasty. 1999;14:756–60. doi: 10.1016/s0883-5403(99)90232-2. [DOI] [PubMed] [Google Scholar]


