Abstract
Tuberous sclerosis is a rare genetic disease which leads to formation of benign tumours in the brain and other organs of the body. It is a multisystem disease with various clinical manifestations. Renal angiomyolipomas are the most common renal manifestations whereas renal cell carcinoma is the least. Renal cysts are found in around 20% of the patients but polycystic kidney disease is present in less than 2% cases and is relatively rare manifestation of the disease. We present a case of tuberous sclerosis in a 60-year-old man who presented to the medicine outpatient department for routine evaluation of his hypertension. He was diagnosed as tuberous sclerosis. His ultrasound and CT scan of abdomen revealed polycystic kidney disease. His kidney function test and urine analysis were suggestive of chronic kidney disease.
Background
Tuberous sclerosis is a rare genetic disease and is caused by mutation of either of the two genes namely TSC1 or TSC2 which results in the loss of control of cell growth and cell division, leading to tumour formation in various organs of the body.1 The disease affects men and women, all races and ethnic groups.2 It affects 1 in 6000 to 1 in 12 000 population.3 This autosomal dominant disease was first described by Bourneville.4 It is a multisystem disease with various clinical presentations. The diagnosis of tuberous sclerosis epends on presence of combination of signs and symptoms of the disease as described. Diagnostic criteria includes 11 major and 9 minor features. Major ones are facial angiofibromas or forehead plaque, non-traumatic ungual or periungual fibroma, hypomelanotic macules, shagreen patch, cortical tuber, multiple retinal nodular hamartomas, subependymal nodule, subependymal giant cell astrocytoma, cardiac rhabdomyoma, lymphangioleiomyomatosis and renal angiomyolipoma where as minor features include pits in dental enamel, hamartomatous rectal polyps, cerebral white-matter migration tracts, bone cysts, retinal achromic patch, gingival fibromas, non-renal hamartoma, Confetti skin lesions and multiple renal cysts. These clinical findings vary according to age. Either two major or one major plus two minor features are required to make a definite diagnosis of the disease.5
Kidneys are commonly involved in this disease and various manifestations of tuberous sclerosis include renal angiomyolipomas, renal cysts and renal cell carcinoma. Renal angiomyolipomas are the most common renal manifestation where as renal cell carcinoma is the least common. Single or multiple renal cysts are found in about 14–53% of cases.6–8 Polycystic kidney disease is present in less than 2% of cases and is a relatively rare manifestation of this disease. Renal involvement is one of the leading cause of mortality and morbidity in these patients and approximately 9/100 000 patients develop renal failure in long run.9 This complication is usually associated with cystic renal disease.10 Polycystic kidney disease in tuberous sclerosis is reported to cause end-stage renal disease.11 12
Making diagnosis of this disease is not difficult because of its classical presentation. Once the diagnosis is complete, search for associated finding can help in managing various complications of the disease. This patient with typical manifestations of tuberous sclerosis was found to have chronic renal failure due to polycystic kidney disease, a relatively rare manifestation of this disease leading to this rare complication of the disease. This association is uncommonly observed in this disease.
Case presentation
The patient, a 60-year-old Indian, hypertensive man, reported in medicine outpatient department for routine evaluation of hypertension. He had typical skin lesions on his face and body. His physical examination revealed various cutaneous manifestations of tuberous sclerosis like facial angiofibromas (figure 1), shagreen patches (figure 2), molluscum fibrosum (figure 3), forehead plaques (figure 4), periungual fibromas (figures 5 and 6), ash leaf spots (figure 7) and cafe au lait spots (figure 8). His kidney function test showed creatine of 2.5 mg/dL and urea 124 mg/dL with normal electrolytes. He was categorised to have stage 3 chronic kidney disease. Other investigations like complete blood count, liver function test, lipid profile and sugar were normal. His urine examination revealed proteinuria. A radiological examination showed normal X-ray of the chest, skull and hands. His ultrasound and the CT scan of the abdomen showed roundish, hypoechoic, numerous cysts of varying size in both the kidneys, meeting the criteria of polycystic kidney disease (figures 9–13). A brain CT revealed bilateral periventricular and cortical calcified tubers (figure 14). Fundus examination showed retinal and choroidal atrophy on left eye. His echocardiography was normal. Sigmoidoscopy showed multiple polyps in sigmoid colon and rectum.
Figure 1.
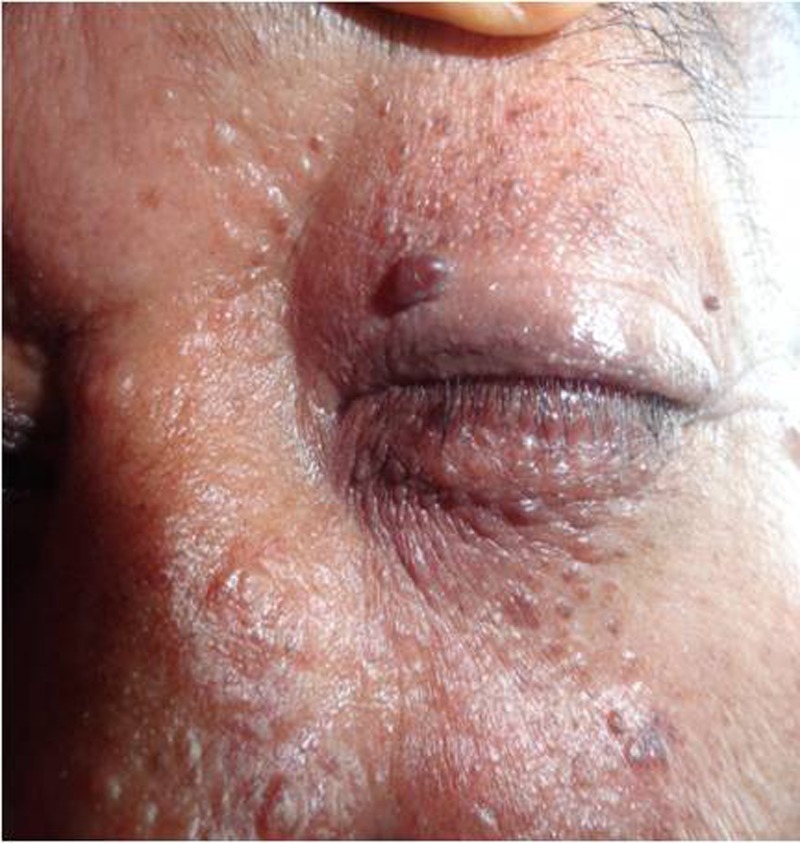
Facial angiofibromas.
Figure 2.

Shagreen patch.
Figure 3.

Molluscum fibrosum.
Figure 4.

Forehead plaque.
Figure 5.

Periungual fibromas.
Figure 6.

Periungual fibromas.
Figure 7.

Ash-leaf spots.
Figure 8.

Cafe au lait spots.
Figure 9.
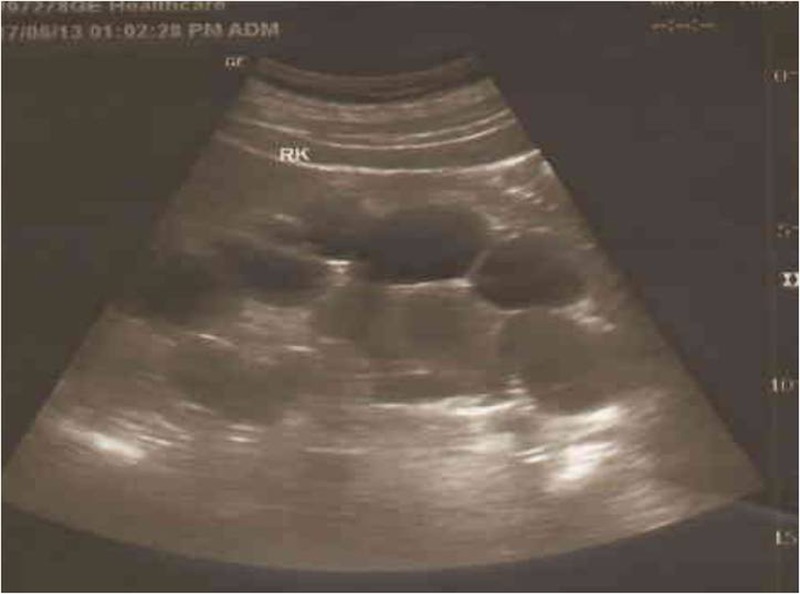
Ultrasonography of the right kidney showing enlargement with numerous cysts of varying sizes.
Figure 10.

Ultrasonography of the left kidney showing enlargement with numerous cysts of varying sizes.
Figure 11.

CT scan of the abdomen showing numerous cysts of varying sizes in both the kidneys.
Figure 12.
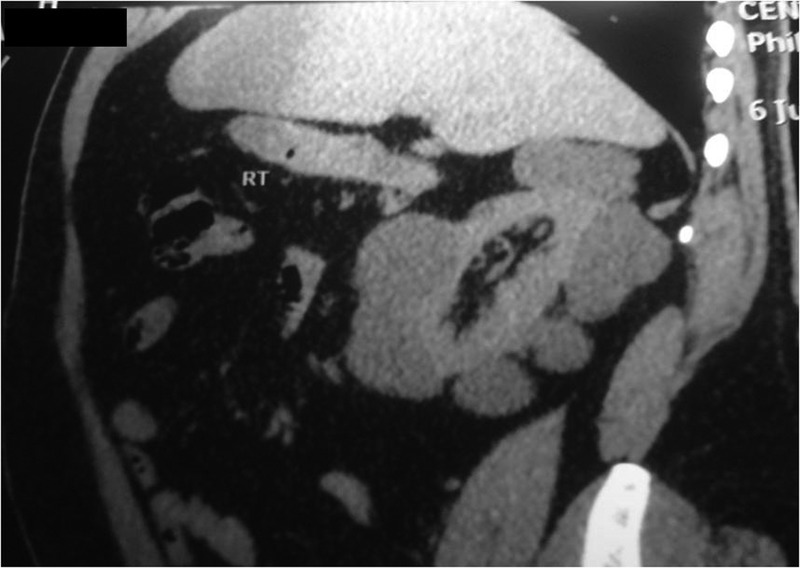
CT scan of the abdomen showing numerous cysts of varying sizes in right kidney.
Figure 13.
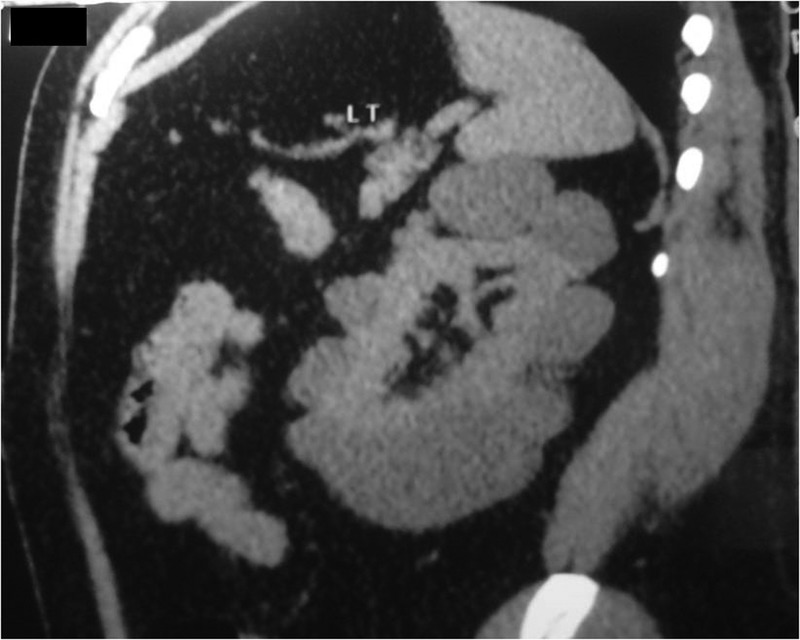
CT scan of the abdomen showing numerous cysts of varying sizes in left kidney.
Figure 14.
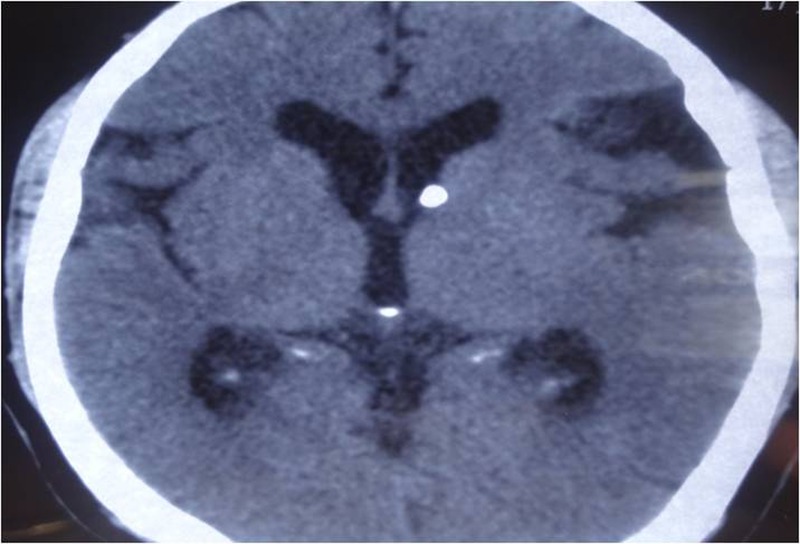
CT scan (brain) showing calcified subependymal tubers.
A detailed history suggested learning disabilities in childhood and epilepsy at the age of 3 years. He also gave history of surgical removal of skin tags on the back of neck and fleshy tumours on nail beds several times. His family history confirmed existence of the disease in three generations.
Outcome and follow-up
The patient is on regular follow-up and need of renal replacement therapy has been explained.
Discussion
Tuberous sclerosis is a congenital autosomal dominant disease leading to formation of tumours in various organs like central nervous system, kidneys, lungs, heart, retina and skin.1 A combination of signs, including major or minor are described for diagnosis. Two major features or one major and two minor are required to make a definite diagnosis.5 Our patient had six major and three minor features, so definite diagnosis of tuberous sclerosis was found. Cutaneous and neurological manifestations are the most common manifestation of tuberous sclerosis.13–15 Renal manifestations are also very common and include renal angiomyolipomas, renal cysts and renal cell carcinoma. Our patient presented with hypertension and chronic renal disease and ultrasound and CT scan of abdomen revealed polycystic kidney disease. Renal angiomyolipomas are the most common renal manifestations and are present in approximately 75–80% where as renal cell carcinoma is the least. Single or multiple renal cysts are found in 14–53% cases.6–8 Tuberous sclerosis leading to chronic renal failure is rare.16 17 This complication is usually associated with cystic renal disease.10 Polycystic kidney disease is present in less than 2% cases and is relatively rare manifestation of the disease. On reviewing various literatures, we found various case reports on association of autosomal dominant polycystic kidney disease with tuberous sclerosis.18 19 Deletion of all or part of the tuberous sclerosis complex 2 and autosomal dominant polycystic kidney disease 1 genes, which are located in proximity in the same chromosome leads to this association.20 21 This is tuberous sclerosis complex 2 autosomal dominant polycystic kidney disease 1 contiguous gene syndrome and is diagnosed in the presence of typical renal lesions in a patient with tuberous sclerosis complex.22 Polycystic kidney disease is reported to cause end-stage renal disease in patients with tuberous sclerosis.11 12 and is frequently complicated by chronic renal failure.23 A CT scan or an ultrasound of the abdomen is almost always sufficient to diagnose polycystic kidney disease due presence of some specific features. This also differentiates cystic renal lesions from angiomyolipomas.24 ACE inhibitors are preferred antihypertensive drugs in these patients due to their renoprotective effect. Nephrectomy or renal replacement therapy is treatment of choice and rapamycin is found to be very useful immunosuppressive drug after renal transplant.12 18 Our patient presented with hypertension and chronic renal failure due to polycystic kidney disease. Tuberous sclerosis is a relatively rare genetic disease, polycystic kidney disease is a relatively rare manifestation and chronic renal failure is very rare complication of the disease, so we thought it was worth reporting this rare association.
Learning points.
Though tuberous sclerosis is a rare disease, diagnosis is not difficult due to its characteristic clinical presentation.
Various pathological and radiological investigations are important for early detection and managing its complications.
Polycystic kidney disease is a relatively rare manifestation but an important predisposing factor for developing chronic renal failure in these patients.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Wienecke R, Klemm E, Karparti S, et al. Reduction of expression of tuberin, the tuberous-sclerosis-complex-gene-2 product in tuberous sclerosis complex associated connective tissue nevi and sporadic squamous and basal cell carcinomas. J Cutan Pathol 2002;2013:287–90 [DOI] [PubMed] [Google Scholar]
- 2.O Callaghan FJ, Shiell AW, Osborne JP, et al. Prevalence of tuberous sclerosis estimated by capture-recapture analysis. Lancet 1998;2013:1490. [DOI] [PubMed] [Google Scholar]
- 3.Tuberous sclerosis fact sheet National Institute of Neurological Disorders and Stroke. April 2006
- 4.Stoian M, Chitac D, Stoian S, et al. Tuberous sclerosis—a case report. Eur J Anaesthesiol 2008;2013:46 [Google Scholar]
- 5.Hyman MH, Whittemore VH. National Institutes of Health Consensus Conference. Tuberous sclerosis complex. Arch Neurol 2000;2013:662–5 [DOI] [PubMed] [Google Scholar]
- 6.Ewalt DH, Sheffield E, Sparagana SP, et al. Renal lesion growth in children with tuberous sclerosis complex. J Urol 1998;2013:141–5 [PubMed] [Google Scholar]
- 7.Roach ES. Sparagana SP. Diagnosis of tuberous sclerosis complex. J Child Neurol 2004;2013:643–9 [DOI] [PubMed] [Google Scholar]
- 8.Rakowski SK, Winterkorn EB, Paul E, et al. Renal manifestations of tuberous sclerosis complex: incidence, prognosis, and predictive factors. Kidney Int 2006;2013:1777–82 [DOI] [PubMed] [Google Scholar]
- 9.Levy M, Feingold J. Estimating prevalence in single gene kidney disease progressing to renal failure. Kidney Int 2000;2013:925. [DOI] [PubMed] [Google Scholar]
- 10.Nimr AB, Patel PJ, Tongia RK, et al. Chronic renal failure and tuberous sclerosis: a rare association. Post Grad Med J 1987;2013:811–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Minz M, Sharma A, Mahawar K, et al. Successful live related renal transplant in a case of tuberous sclerosis. Assoc Physicians India 2005;2013:43–5 [PubMed] [Google Scholar]
- 12.Choi KC, Kim SW, Kim NH, et al. Tuberous sclerosis and polycystic kidney disease. A case report. J Korean Med Sci 1996;2013:526–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crino PB, Nathanson KL, Henske EP. The tuberous sclerosis complex. N Engl J Med 2006;2013:1345–56 [DOI] [PubMed] [Google Scholar]
- 14.Thiele EA. Managing epilepsy in tuberous sclerosis complex. J Child Neurol 2004;2013:680–6 [DOI] [PubMed] [Google Scholar]
- 15.Van Tassel P, Cure JK, Holden KR. Cyst like white matter lesions in tuberous sclerosis. Am J Neuroradiol 1997;2013:1367–73 [PMC free article] [PubMed] [Google Scholar]
- 16.Schillinger F, Montagnac R. Renal lesions in tuberous sclerosis. Nephrol Ther 2006;2013:123–6 [PubMed] [Google Scholar]
- 17.Manno C, Claudatus J, La Raia E, et al. Chronic renal failure for bilateral spontaneous kidney rupture in a case of tuberous sclerosis. Case report and review of the literature. Am J Nephrol 1991;2013:416. [DOI] [PubMed] [Google Scholar]
- 18.Lewis JC, Thomas HV, Murphy KC, et al. Genotype and psychological phenotype in tuberous sclerosis. J Med Genet 2004;2013:203–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kariuki N, Karanja MN, McLigeyo SO. Polycystic kidney disease in tuberous sclerosis complex. case report. East Afrl Med J 1998;2013:616–18 [PubMed] [Google Scholar]
- 20.Book-Carter PT, Peral B, Ward CJ, et al. Deletion of the TSC2 and PKD1 genes associated with severe infantile polycystic kidney disease. a contiguous gene syndrome. Nat Genet 1994;2013:328–32 [DOI] [PubMed] [Google Scholar]
- 21.Sampson JR, Maheshwar MM, Aspinwall R, et al. Renal cystic disease in tuberous sclerosis: the role of the polycystic kidney disease 1 gene. Am J Hum Genet 1997;2013:843–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bisceglia M, Galliani C, Carosi I, et al. Tuberous sclerosis complex with polycystic kidney disease of the adult type: the TSC2/ADPKD1 contiguous gene syndrome. Int J Surg pathol 2008;2013:375–85 [DOI] [PubMed] [Google Scholar]
- 23.Rosado C, Garcia-Cosmes P, Fraile P. Tuberous sclerosis associated with polycystic kidney disease: effects of rapamycin after renal transplantation. Case Rep Transplant 2013:397087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu DT, Sheth KJ. Cystic renal involvement in tuberous sclerosis. Clin Pediatrl 1985;2013:36–9 [DOI] [PubMed] [Google Scholar]


