Abstract
Spontaneous coronary artery dissection (SCAD) involving multiple coronary arteries simultaneously is extremely rare. It should be considered in younger patients, especially who do not have traditional cardiac risk factors. We present a case of young male patient presenting with acute coronary syndrome associated with ST segments elevation on ECG following physical stress whose coronary angiography revealed SCAD of the left anterior descending as well as the right coronary artery and discuss the therapeutic options with a brief review of the limited evidence.
Background
The reported occurrence of spontaneous coronary artery dissection (SCAD) is around 0.07–1.1% of people presenting with acute coronary syndrome (ACS).1–4 Predisposing conditions include pregnancy, fibromuscular dysplasia, Marfan's syndrome, Ehler-Danlos syndrome, sarcoidosis, drugs (eg, cocaine, oral contraceptives and cyclosporine), atherosclerosis, hypertension, retching and strenuous exercise. Over 80% of the documented cases are postpartum.5
Multivessel SCAD is extremely rare. Fewer than 10 cases with three vessels have been published in the English literature. Mostly the involvement of more than one coronary artery simultaneously has either occurred postpartum or resulted from underlying abnormalities. To the best of our knowledge two cases of SCAD involving the left as well as the right coronary arterial systems in otherwise normal vessels have been documented previously.6 7 We describe the case of a young man presenting with ACS associated with ST segments elevation on ECG following physical stress, found to have SCAD of the left anterior descending (LAD) and the right coronary artery (RCA), and discuss the available treatment options.
Case presentation
A 54-year-old man was admitted to the emergency department with acute anterior myocardial infarction. The patient was previously a very active person and had no cardiac or any other medical history of note. There were no significant cardiovascular risk factors and no history of drug use or misuse. The symptoms started while swimming 3 h prior to presentation. The physical examination revealed a blood pressure of 170/95 mm Hg and pulse rate 80 bpm with intermittent left bundle branch block on monitor. The ECG revealed significant ST elevation in anterolateral leads, with ST depression in leads III and aVF (figure 1). Cardiovascular and other system examinations were unremarkable. The emergent coronary angiography showed extensive type E dissection in the LAD as well as the RCA with significant flow disturbance (TIMI II) in LAD. These findings were confirmed on intravascular ultrasound (IVUS; figure 2). The dissection involved almost the entire length of both the vessels starting from the proximal segments (figure 3). No collateral formation was observed. The left circumflex artery was normal. A ventriculogram revealed apical and distal left ventricle (LV) wall akinesis.
Figure 1.
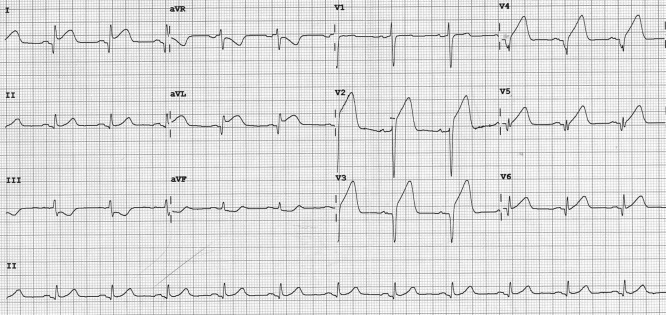
ECG showing ST elevation in anterolateral leads, with ST depression in leads III and aVF.
Figure 2.
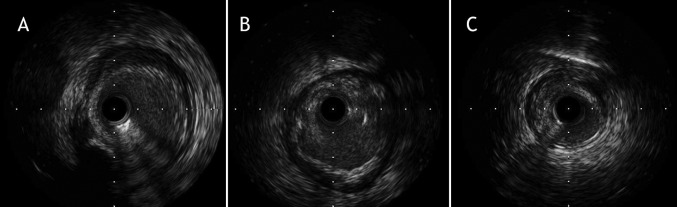
Dissection of the left anterior descending coronary artery on intravascular ultrasound: (A) proximal, (B) midvessel and (C) distal segment.
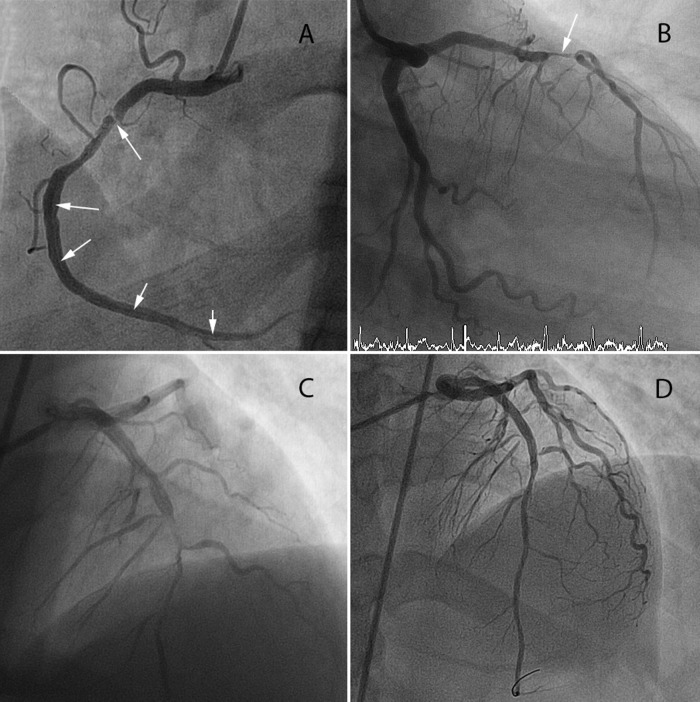
Figure 3.
Angiographic findings of spontaneous coronary artery dissection: (A) right coronary artery, (B) left anterior descending (LAD) artery, (C) LAD before percutaneous intervention (PCI) and (D) LAD post PCI; arrows mark the dissection flap.
Percutaneous angioplasty was performed using two drug-eluting stents (3.5×22 and 3×15 mm resolute integrity) for the LAD lesion sealing its proximal entry point (figure 3D). This led to resolution of ST segments on ECG and patient became pain free (pain to balloon time 147 min; door to balloon time 57 min). An initial attempt to intervene on the RCA was not pursued given difficulty wiring the true lumen and the lesion was managed conservatively, particularly in view of a stable condition of the patient after percutaneous intervention (PCI) to LAD, TIMI III flow in RCA and lack of convincing inferior ECG changes. G2b3a inhibitors, heparin and nitrates were given during the procedure as per standard care.
Subsequent investigations ruled out an aortic dissection. An echocardiogram performed 48 h after the angiogram revealed moderate segmental LV dysfunction (apical and distal LV wall akinesis; biplane ejection fraction 50%) with apical thrombus requiring an addition of warfarin to his dual antiplatelet therapy.
The patient was discharged home after a period of close monitoring. He remained stable during his rest of the in-hospital stay, as well as outpatient follow-up at 1 week and 5 weeks. A repeat angiogram at 8 weeks was organised to decide on the need of further intervention depending on clinical symptoms and angiographic findings. The patient was asked to refrain from high-impact sports and strenuous activity.
Discussion
Despite being a life-threatening condition, there is no consensus about management of SCAD and no guidelines exist. Medical treatment is usually considered for asymptomatic patients and satisfactory results have been reported in selected patients, for example, distal segment lesions with preserved flow.8 β-Blockers can further aid by reducing the artery wall sheer stress and thus helping in the healing process.9 The role of long-term antiplatelet agents in patients with SCAD not receiving stent is uncertain. Follow-up IVUS can be useful to track the healing of SCAD when appropriate. CT coronary angiography has also been used for following up stable patients.10 11 This decision, however needs to be individualised as an invasive angiogram may provide an added benefit of treatment option if clinically indicated.
In symptomatic or severe cases, a more aggressive approach is usually adopted, such as PCI or coronary artery bypass grafting (CABG). Left main coronary artery (LM) involvement or diffuse/multivessel disease favours CABG. Fibrinolytic agents are not routinely recommended as they can extend the dissection.1 Focal dissections not involving LM can be treated with stents. Wiring the true lumen in the presence of dissection can be challenging. IVUS and optical coherence tomography have been used to a identify double-lumen, intramural haematoma or thrombi, intimal rupture site, as well as any underlying atherosclerosis.12–14 Choosing the right type of stent is another dilemma, as no data exists to compare drug-eluting stents with bare metal stents in these patients. The incidence of in-stent restenosis in this population is unknown. Although in theory drug eluting stents may adversely affect arterial healing, this effect on non-atheromatous vessel has not been assessed and a clinical decision should be made using the existing criteria for appropriate stent use.
In our case the patient presented with dissection of the LAD and the RCA, associated with acute anterior ST elevation on ECG. Urgent PCI was performed to treat the culprit vessel. An attempt to intervene the RCA was aborted early given difficulty finding the true lumen as risks of complications in such situations can be high15 and can outweigh the benefits by compromising further myocardial tissue in an already significantly impaired LV. Therefore, a decision was made to manage the RCA lesion conservatively. The incidence of recurrent SCAD is unknown and no specific data exist regarding whether or not the patient should be allowed strenuous activities and for how long. This decision should therefore be carefully individualised.
Learning points.
Spontaneous coronary artery dissection is an uncommon presentation of acute coronary syndrome (ACS) and should be included in the differentials, especially for young patients who would otherwise be considered ‘low risk’ for ACS.
Appropriate treatment options depend on clinical presentation, type and extent of dissection.
Conservative approach is reasonable in the absence of underlying coronary atheroma and allows healing of the vessel without intervention in patients who are otherwise stable.
CT coronary angiography could prove useful for the follow-up of some patients.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.McCann AB, Whitbourn RJ. Spontaneous coronary artery dissection: a review of the etiology and available treatment options. Heart Vessels 2009;2013:463–5 [DOI] [PubMed] [Google Scholar]
- 2.Mortensen KH, Thuesen L, Kristensen IB, et al. Spontaneous coronary artery dissection: a Western Denmark Heart Registry study. Catheter Cardiovasc Interv 2009;2013:710–17 [DOI] [PubMed] [Google Scholar]
- 3.Hering D, Piper C, Hohmann C, et al. [Prospective study of the incidence, pathogenesis and therapy of spontaneous, by coronary angiography diagnosed coronary artery dissection]. Z Kardiol 1998;2013:961–70 Prospektive Untersuchung zu Haufigkeit, Pathogenese und Therapie spontaner, koronarangiographisch diagnostizierter Koronararteriendissektionen [DOI] [PubMed] [Google Scholar]
- 4.Vanzetto G, Berger-Coz E, Barone-Rochette G, et al. Prevalence, therapeutic management and medium-term prognosis of spontaneous coronary artery dissection: results from a database of 11,605 patients. Eur J Cardiothorac Surg 2009;2013:250–4 [DOI] [PubMed] [Google Scholar]
- 5.Kanwar M, Gill N. Spontaneous multivessel coronary artery dissection. J Invasive Cardiol 2010;2013:E5–6 [PubMed] [Google Scholar]
- 6.Kim YH, Kim SH, Lim SY, et al. Simultaneous and spontaneous multivessel coronary artery dissection presenting as congestive heart failure. Heart Vessels 2011;2013:338–41 [DOI] [PubMed] [Google Scholar]
- 7.Cohen DE, Strimike CL. A case of multiple spontaneous coronary artery dissections. Catheter Cardiovasc Interv 2000;2013:318–20 [DOI] [PubMed] [Google Scholar]
- 8.Motreff P, Souteyrand G, Dauphin C, et al. Management of spontaneous coronary artery dissection: review of the literature and discussion based on a series of 12 young women with acute coronary syndrome. Cardiology 2010;2013:10–18 [DOI] [PubMed] [Google Scholar]
- 9.Choi JW, Davidson CJ. Spontaneous multivessel coronary artery dissection in a long-distance runner successfully treated with oral antiplatelet therapy. J Invasive Cardiol 2002;2013:675–8 [PubMed] [Google Scholar]
- 10.Vrints CJ. Spontaneous coronary artery dissection. Heart 2010;2013:801–18 [DOI] [PubMed] [Google Scholar]
- 11.Russo V, Marrozzini C, Zompatori M. Spontaneous coronary artery dissection: role of coronary CT angiography. Heart 2013;2013:672–3 [DOI] [PubMed] [Google Scholar]
- 12.Alfonso F, Canales E, Aleong G. Spontaneous coronary artery dissection: diagnosis by optical coherence tomography. Eur Heart J 2009;2013:385. [DOI] [PubMed] [Google Scholar]
- 13.Alfonso F, Paulo M, Gonzalo N, et al. Diagnosis of spontaneous coronary artery dissection by optical coherence tomography. J Am Coll Cardiol 2012;2013:1073–9 [DOI] [PubMed] [Google Scholar]
- 14.Poon K, Bell B, Raffel OC, et al. Spontaneous coronary artery dissection: utility of intravascular ultrasound and optical coherence tomography during percutaneous coronary intervention. Circ Cardiovasc Interv 2011;2013:e5–7 [DOI] [PubMed] [Google Scholar]
- 15.Tweet MS, Hayes SN, Pitta SR, et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation 2012;2013:579–88 [DOI] [PubMed] [Google Scholar]