Abstract
The McKenzie method, also known as Mechanical Diagnosis and Therapy (MDT), is primarily recognized as an evaluation and treatment method for the spine. However, McKenzie suggested that this method could also be applied to the extremities. Derangement is an MDT classification defined as an anatomical disturbance in the normal resting position of the joint, and McKenzie proposed that repeated movements could be applied to reduce internal joint displacement and rapidly reduce derangement symptoms. However, the current literature on MDT application to shoulder disorders is limited. Here, we present a case series involving four patients with chronic shoulder pain from a duration of 2–18 months classified as derangement and treated using MDT principles. Each patient underwent mechanical assessment and was treated with repeated movements based on their directional preference. All patients demonstrated rapid and clinically significant improvement in baseline measures and the disabilities of the arm, shoulder, and hand (QuickDASH) scores from an average of 38% at initial evaluation to 5% at discharge within 3–5 visits. Our findings suggest that MDT may be an effective treatment approach for shoulder pain.
Keywords: Chronic, Shoulder pain, McKenzie method, MDT
Background
Shoulder pain is a common symptom frequently consulted for in primary care. While highly variable, the prevalence rate ranges from 6.7 to 46.7% per year in the general population.1,2 The process of diagnosing shoulder-related problems is difficult given the poor reliability and validity of most specialized orthopedic testing procedures and the pathoanatomical model used as a basis shoulder pain diagnosis and treatment.3 Incidental findings in magnetic resonance imaging (MRI) studies such as the presence of rotator cuff tears in 65% of asymptomatic individuals are common, and failure to correlate imaging results with the patient’s clinical presentation may complicate shoulder pain diagnoses.4 The use of sub-classifications, assessment, and treatment methods that are patient-driven has been suggested as a more practical alternative in diagnosing shoulder pathology.5,6
Mechanical Diagnosis and Therapy (MDT) utilizes classifications based on the patient’s response to repeated movements, positioning, and other loading strategies instead of relying on the identification of a specific pathoanatomical structure. The application of MDT in the spine has a high degree of reliability and prognostic validity when performed by trained clinicians.7,8 McKenzie proposed that the same principles used in the spine could also be applied to the peripheral joints.9,10 Using MDT, patients can be classified into posture, dysfunction, or derangement syndromes. Posture syndrome occurs in normal tissues subjected to abnormal stress during sustained positioning. Ischemia and irritation of mechanoreceptors from sustained positioning result in discomfort, which resolves the following position change. Dysfunction syndrome is defined as the deformation of structurally impaired or shortened soft tissues due to scarring or adaptive shortening. Pain in dysfunction is chronic and intermittent. In the extremities, dysfunction syndrome is further categorized into contractile or articular dysfunction. In contractile dysfunction, pain is provoked upon loading of impaired contractile tissues and is therefore felt during active or resisted movement. In articular dysfunction, pain is felt at endrange when shortened articular tissues, such as ligaments, tendons, and joint capsules, are passively stretched. No rapid changes can be expected in dysfunction syndrome because it takes time to remodel scarred or adaptively shortened tissues.
Derangement is defined as an internal disturbance in the normal resting position of the joint that results in pain and movement obstruction.11 It can occur in acute, sub-acute, or chronic conditions. A survey on the prevalence of mechanical syndromes in the extremities using the MDT classification system showed a predominance of derangements.12 The interest in this classification lies in claims that patients can exhibit rapid changes in their symptoms and mechanical presentation in response to repeated movements, even in chronic conditions. Movements that increase internal joint displacement can cause further pain and movement loss. Conversely, movements that reduce displacement (also known as directional preference) can reduce pain and improve function.9,10 Following MDT principles, successfully diagnosing derangements can identify patients who are likely to be rapid responders when matched with their directional preference. Indeed, matching patients with their directional preference resulted in good treatment outcomes in the spine.13,14,15 A reliability study into the MDT classification system for the extremities showed a 92% agreement when used by trained clinicians.16 In 2005, Aina and May reported a case of shoulder derangement managed in four visits using MDT.17 However, evidence for the application and outcomes of MDT to the extremities, particularly at the shoulder joint, is limited.
The purpose of this report is to present the assessment, clinical intervention, and outcomes of four patients classified as having shoulder derangement using MDT principles. The report also aims to demonstrate the relationship between directional preference during assessment and rapid improvement of symptoms and function in patients with shoulder pain.
Methods
Four patients with primary complaints of shoulder pain between 2 and 18 months in duration were evaluated in an outpatient clinic by MDT-trained clinicians. All patients were cleared for cervical spine involvement using the McKenzie principles of spinal evaluation. Repeated movements of the cervical spine did not have significant effects on the symptoms. Therefore, the shoulder joint became the focus of the examination.
Case 1
Patient characteristics
A 53-year-old male presented with a 2-month history of right anterolateral shoulder pain following tripping and falling on his right side (Table 1). He was in good health and had no previous history of shoulder problems. He was an avid boomerang-thrower and also enjoyed working in his yard but was unable to do either activity after the fall. The pain was generally intermittent but could linger at rest after continued use of the arm. Symptoms were also provoked by shoulder horizontal adduction and lying down on his right side. Avoiding use of the right shoulder relieved the symptoms. No X-rays were taken. He denied having any neck pain or arm paresthesia. His disabilities of the arm, shoulder, and hand (QuickDASH) Score was 36% at the initial visit. The patient denied having previous treatment besides taking ibuprofen as needed.
Table 1. Patient characteristics.
| Patient | Age/Gender | Symptom location | Symptom duration | Injury mechanism |
| 1 | 53/M | Right anterolateral | 2 months | Fall/trauma |
| 2 | 64/M | Right anterior | 5 months | Gradual onset |
| 3 | 50/M | Right anterior | 18 months | Throwing/sudden |
| 4 | 40/F | Left posterolateral | 6 months | Gradual onset |
Examination and clinical impression
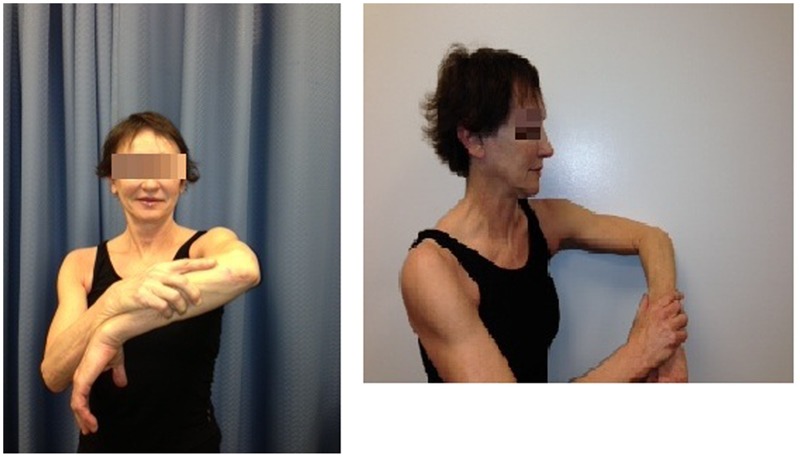
He demonstrated major loss of motion in right shoulder internal rotation (IR) with endrange pain and minimal loss in shoulder flexion, extension, and abduction but with pain during movement (Table 2). Strength testing revealed 3+/5 internal rotators and 4-/5 deltoids, and both movements resulted in a 7/10 pain rating. Repeated IR of the right shoulder (Fig. 1) decreased the pain rating to 2/10 and increased IR by 25°. Internal rotator and deltoid strength improved to 4/5. A classification of shoulder derangement with a directional preference of IR was made because of the rapid changes in symptoms and range of motion (ROM) in response to repeated movement testing.
Table 2. Summary of findings.
| Patient | Tests | Baseline measures | At discharge | Directional preference | Number of visits |
| 1 | QuickDASH | 36% | 4% | Internal rotation (IR) | 3 |
| Active/passive(degrees) | 165/170 | (within normal limits) WNL | |||
| Flexion | |||||
| Abduction | 160/163 | WNL | |||
| Extension | 50/55 | WNL | |||
| IR at 90° | 20/24 | WNL | |||
| External rotation (ER) at 90° | WNL | WNL | |||
| Strength | Internal rotators-3+/range, deltoids-4/range | 5/5 | |||
| 2 | QuickDASH | 50% | 11% | Extension | 4 |
| Active/passive(degrees) | 90/95 | WNL | |||
| Flexion | |||||
| Abduction | 100/104 | WNL | |||
| Extension | 20/30 | 50/60 | |||
| IR at 90 | 25/28 | 60/70 | |||
| ER at 90 | 40/42 | WNL | |||
| Strength | Deltoids — 4-/range | 4+/5 | |||
| 3 | QuickDASH | 41% | 2% | IR (1st visit), changed to extension (3rd visit) | 5 |
| Active/passive | 165/180 | WNL | |||
| Flexion | |||||
| Abduction | 130/170 | WNL | |||
| Extension | 40/50 | WNL | |||
| IR (functional) | L1 level | T8 | |||
| ER | T1 | T3 | |||
| Strength | Deltoids-3-/range | 4+/5 | |||
| 4 | QuickDASH | 25% | 4% | IR with shoulder flexed at 90° | 3 |
| Active/passive(degrees) | 165/170 | WNL | |||
| Flexion | |||||
| Abduction | 168/175 | WNL | |||
| Extension | 48/55 | WNL | |||
| IR at 0 | WNL | WNL | |||
| ER at 0 | 50 | WNL | |||
| Strength | painful abduction | 5/5 with no pain |
Figure 1.

Internal rotation/hand behind back and extension.
Intervention, follow up, and outcome
Instructions to be followed at home included 10 repetitions of IR every 3 hours (Fig. 1). He returned 2 days later with 75% perceived improvement. He was encouraged to perform the exercise to endrange with overpressure every 3 hours and following performance of aggravating movements. The patient was discharged a week later after three visits with a QuickDASH score of 4%, full ROM, and normal strength (Table 2).
Case 2
Patient characteristics
A 64-year-old retired male was referred to physiotherapy with a diagnosis of right rotator cuff strain. He presented with a 5-month history of gradual onset right anterior shoulder pain. He denied any specific injury to his shoulder. He described his pain as intermittent, provoked by lifting, reaching behind to scratch his back, and continued use of his right shoulder. He felt better at rest but had difficulties sleeping on his right side due to pain. He was prescribed anti-inflammatories, which he took twice a day for 2 months with minimal relief. He had a history of right rotator cuff tear and repair 2 years prior to this assessment for which he underwent post-surgical physiotherapy, including rotator cuff strengthening. He was otherwise in excellent health and was relatively asymptomatic until this recent episode.
Examination and clinical impression
He demonstrated significant loss of motion and pain during right shoulder flexion, abduction, extension, and IR (Table 2). Testing revealed 4-/5 right deltoid strength. Repeated movement testing showed a directional preference of shoulder extension with immediate improvement in shoulder flexion and abduction by 20° and less pain during movement (Fig. 1). The case was classified as shoulder derangement in accordance with MDT principles.
Intervention, follow up, and outcome
He was given shoulder extension exercises with the involved arm supported on the counter (Fig. 1) and was instructed to perform 10 repetitions every 2 to 3 hours and when needed for pain relief. He returned a week later with 50% perceived improvement. The same exercise was maintained, but the patient was encouraged to go further into endrange. He returned 2 later for the third visit and reported 80% perceived improvement. The patient reported that he could use his right shoulder with minimal discomfort. Instructions were given to continue with his home program at least 3×/day. He was seen for a total of four visits in 3 weeks and was discharged within functional limits of ROM and a QuickDASH score of 11% (Table 2).
Case 3
Patient characteristics
A 50-year-old male complained of right anterior shoulder pain for 18 months resulting from throwing a ball while playing baseball. He had 12 physiotherapy visits in another clinic consisting of heat, ultrasound, and an unspecified rotator cuff strengthening program without relief. Magnetic resonance imaging revealed arthritic changes with impingement in the right acromioclavicular joint. He also underwent a series of cortisone injections in the shoulder with minimal relief. The patient had a QuickDASH score of 41% and a 7/10 pain rating. He had intermittent pain aggravated by lifting, reaching overhead, and lying on his right side. Continued use of the arm also worsened his symptoms. Rest and hydrocodone relieved the pain.
Examination and clinical impression
Significant loss in shoulder abduction, flexion, and IR with pain during movement was noted. There was minimal shoulder extension loss. Shoulder abduction was painful and weak at 3-/5 (Table 2). Repeated movement testing indicated a directional preference of IR resulting in 25% improvement in overall ROM and pain reduction from 7/10 to 3/10. A classification of shoulder derangement was made.
Intervention, follow up, and outcome
Three days later, he returned with 50% perceived improvement from performance of repeated IR every 3 hours. He was advised to add self-overpressure using the left hand (Fig. 1). He returned 2 days later with reports of worse pain in the shoulder and decreased right shoulder flexion and abduction range. The patient was reassessed and demonstrated a change in directional preference from IR to extension. The home program was revised to supported extension (Fig. 2) to be performed as 10 repetitions every 3 hours and for pain relief. He returned for the 4th visit and reported 75% improvement. Range of motion was within normal limits (WNL) and with 4/5 manual muscle test (MMT) of the right shoulder abductors. He was encouraged to continue with extension exercises every 3 hours. He was discharged the following week after five visits with WNL ROM and 4+/5 MMT. He was able to sleep on the right side without pain and resumed sports activities with 2/10 worst pain rating. He was advised to continue with the exercise program and to perform shoulder extension exercises before and after sports activities.
Figure 2.
Internal rotation in flexion and internal rotation in flexion against wall.
Case 4
Patient characteristics
A 40-year-old female physiotherapist presented with insidious onset of left posterior shoulder and lateral scapular pain for 6 months. Pain improved a month after onset with ibuprofen but had since remained unchanged. Symptoms were intermittent but were provoked by reaching for the driver’s side seat belt or putting a jacket on with the left arm. Lying on her left side with the shoulder in external rotation (ER) also produced pain. Prior to assessment, she tried self-treatment techniques including shoulder horizontal adduction stretch but did not experience any relief. She also tried IR exercises with her hand behind her back without success. The patient’s QuickDASH score on assessment was 25%. She had a history of neck pain but denied arm symptoms. Repeated neck movements did not affect her symptoms.
Examination and clinical impression
Examination of the left shoulder revealed major ER loss with pain during movement and minimal loss in flexion, abduction, and IR with pain at endrange. No significant weakness was noted, but she had slight pain during resisted abduction. Repeated ER worsened the symptoms during assessment. Modified IR with the shoulder flexed at 90° reduced pain and improved ER by 50% (Fig. 2). Resisted abduction was pain-free afterward, and a classification of shoulder derangement was made.
Intervention, follow up, and outcome
She was prescribed 10 to 15 repetitions of IR with the shoulder flexed at 90° to be performed every 2–3 hours (Fig. 2). The next day, she reported at least 50% perceived improvement, and 2 weeks later, she recovered full ROM in the left shoulder with minimal pain only when sustaining ER. Her QuickDASH score had improved to 4%.
Discussion
The use of sub-classifications based on patient characteristics and prognostic factors has been recommended due to the poor validity and reliability of pathoanatomical models in diagnosing shoulder disorders.5 Rather than using pathoanatomical-based diagnoses, the MDT system utilizes a classification system based on symptomatic and mechanical responses to repeated movements, which allows the clinician to optimize treatment according to directional preference.18
Following the principles of MDT, all four patients in this study were classified as having shoulder derangement based on the rapid changes in baseline measures in response to repeated movements during examination alone. Despite their pain chronicity, all patients demonstrated significantly decreased pain intensity accompanied by improvement in motion, strength, and function within a short period of time, reducing the likelihood of natural history as a factor influencing outcome. The patients here were discharged between three and five visits within 4 weeks with minimal to no pain and significantly improved QuickDASH scores (greater than the minimal clinically important difference (MCID) of 8 points). The QuickDASH Scoring system was used due to its high test-retest reliability for shoulder patients.19
Although the number of participants was limited, there was a clear preference toward IR and extension in shoulder derangement reduction in this study. IR combined with flexion was required to reduce the symptoms of Case 4, who had a less typical symptom presentation of posterior shoulder and scapular pain. The directional preference remained unchanged from initial visit to discharge except in Case 3; the patient initially responded to IR but exhibited a change in directional preference to extension after two visits. A recent survey on the preferred loading strategies using the MDT classification system for the extremities indicated similar findings of IR and extension as the most common directional preference at the shoulder.12
There is speculation regarding the structures that could obstruct movement in the extremities. Cadaveric studies by Susan Mercer and Nikolai Bogduk revealed deformable space fillers in the form of fat pads and fibroadipose meniscoids that can proliferate within joints. Also known as intra-articular intrusions, these structures have been implicated as a potential cause of derangements in the extremities.20 However, the exact mechanism for shoulder derangements still requires further investigation.
Although this study has limitations including the inability to establish the cause-and-effect relationship from a case series and the lack of long-term follow ups, the rapid improvement in symptoms observed in all patients suggests that using the MDT algorithm may be a useful approach to manage shoulder pain and that matching shoulder pain to a directional preference may result in good outcomes. Further controlled research and large-scale outcome studies are required to establish the validity of MDT for shoulder pain.
References
- 1.Feleus A, Bierma-Zeinstra SM, Miedema HS, Bernsent RM, Verhaar JA, Koes BW. Incidence of non-traumatic complaints of arm, neck and shoulder in general practice. Man Ther. 2008;13(5):426–33 [DOI] [PubMed] [Google Scholar]
- 2.Luime JJ, Koes BW, Hendriksen IJ, Burdorf A, Verhagen AP, Miedema HS, et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol. 2004;33(2):73–81 [DOI] [PubMed] [Google Scholar]
- 3.May S, Chance-Larsen K, Littlewood C, Lomas D, Saad M. Reliability of physical examination tests used in the assessment of patient with shoulder problems: a systematic review. Physiotherapy. 2010;96:179–90 [DOI] [PubMed] [Google Scholar]
- 4.Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19:116–20 [DOI] [PubMed] [Google Scholar]
- 5.Schillingertout JM, Verhagen AP, Thomas S, Koes BW. Lack of uniformity in diagnostic labeling of shoulder pain: time for a different approach. Man Ther. 2008;13:478–8 [DOI] [PubMed] [Google Scholar]
- 6.Kuipers T, van der Windt D, van der Heijden J, Bouter L. Systematic review of prognostic cohort studies on shoulder disorder. Pain. 2004;109:420–31 [DOI] [PubMed] [Google Scholar]
- 7.Fritz JM, Delitto A, Vignovic M, Busse RG. Interrater reliability of judgements of the centralization phenomenon and status change during movement testing in patients with low back pain. Arch Phys Med Rehabil. 2000;81:57–61 [DOI] [PubMed] [Google Scholar]
- 8.Kilpikoski S, Airaksinen O, Kankaanpaa M, Leminen P, Videman T, Alen M. Interexaminer reliability of low back pain assessment using the McKenzie method. Spine. 2002;27:207–14 [DOI] [PubMed] [Google Scholar]
- 9.McKenzie R. The lumbar spine: mechanical diagnosis and therapy. Wellington: Spinal Publications New Zealand Ltd; 1981 [Google Scholar]
- 10.McKenzie R, May S. The human extremities: mechanical diagnosis and therapy. 2nd edn. Wellington: Spinal Publications New Zealand Ltd; 2003 [Google Scholar]
- 11.McKenzie RA, May S. The lumbar spine: mechanical diagnosis and therapy. 2nd edn. Waikanae: Spinal Publications Ltd; 2003 [Google Scholar]
- 12.May SJ, Rosedale R. A survey of the McKenzie classification system in the extremities: prevalence of the mechanical syndromes and preferred loading strategy. Phys Ther. 2012;92:1175–86 [DOI] [PubMed] [Google Scholar]
- 13.Aina A, May S, Clare H. The centralization phenomenon of spinal symptoms – a systematic review. Man Ther. 2004;9:134–43 [DOI] [PubMed] [Google Scholar]
- 14.Kilpikoski S, Alen M, Simonen R, Heinonen A, Videman T. Does centralizing pain on the initial visit predict outcomes among adults with low back pain? Manuelle Therapie 2010;14:136–41 [Google Scholar]
- 15.Long A, May S, Fung T. The comparative prognostic value of directional preference and centralization: a useful tool for front-line clinicians? J Man Manip Ther. 2008;16:248–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.May S, Ross J. The McKenzie classification system in the extremities: a reliability study using McKenzie assessment forms and experienced clinicians. J Manipulative Physiol Ther. 2009;32:556–63 [DOI] [PubMed] [Google Scholar]
- 17.Aina A, May S. Case report – a shoulder derangement. Man Ther. 2005;10:159–63 [DOI] [PubMed] [Google Scholar]
- 18.Littlewood C, May S. A contractile dysfunction of the shoulder. Man Ther. 2007;12(10):80–3 [DOI] [PubMed] [Google Scholar]
- 19.MIntken PE, Glynn P, Cleland JA. Psychometric properties of the shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH) and numeric pain rating scale in patients with shoulder pain. J Shoulder Elbow Surg. 2009;18:920–6 [DOI] [PubMed] [Google Scholar]
- 20.Mercer SR, Bogduk N. Intra-articular inclusions of the elbow joint complex. Clin Anat. 2007;20:668–76 [DOI] [PubMed] [Google Scholar]


