Abstract
Introduction:
Caliceal diverticulae are a frequent surgical problem. We present our experience with caliceal diverticular stones (CDS) managed with percutaneous nephrolithotomy (PCNL) and describe the two different techniques to deal with diverticula after stone retrieval.
Materials and Methods:
We retrospectively analyzed 10-year data of 44 consecutive patients who underwent PCNL for CDS. During PCNL, if the guide wire could be negoted through the neck of the diverticula, we dilated and stented it. If we couldnot find the neck, we fulgurated the diverticular walls. Follow-up included intravenous urogram at 3 months and annual plain films thereafter. We analyzed the outcome, complications, and recurrence rate.
Results:
Total stone clearance was obtained in 40 (90.90%) patients. We dilated and stented the diverticula in 35 (79.5%) patients and fulgurated the walls in nine (20.5%) patients. Complications occurred in three patients. The postoperative intravenous urogram showed obliteration of diverticula in seven patients and the improved drainage in 37 patients. At the average follow-up of 2 years, 41 (93.18%) patients were asymptomatic and two (4.5%) patients showed the recurrence of stone.
Conclusions:
PCNL can clear calculi from caliceal diverticula in most cases with minimal morbidity. After stone retrieval, the diverticula may be drained into the pyelocaliceal system, if the neck is negotiable and fulgurated if the neck cannot be dilated.
Keywords: Caliceal diverticula, Caliceal diverticular stones, percutaneous nephrolithotomy
INTRODUCTION
Caliceal diverticuli are nonsecretory urothelium lined cystic cavities within the renal parenchyma that harbor static urine.[1] Upto 0.45% of routine intravenous urogram (IVU) may show the presence of caliceal diverticulum.[2] A narrow neck usually communicates between the diverticulum and the rest of pyelocaliceal system (PCS) and allows passive filling with urine. They are associated with calculi in upto 50% of patients.[3] The indications for treatment include flank pain, pyuria, and urinary tract infection (UTI).[4] In the era of minimally invasive surgery, various procedures like shockwave lithotripsy (SWL), percutaneous nephrolithotomy (PCNL), ureterorenoscopic surgery (URS), and laparoscopy have been described for the treatment of this entity, but the stone-free and symptom-free rates are found to be best with PCNL.[5,6,7,8] During PCNL, in order to prevent urinary stasis and recurrent stone formation, either the diverticular neck is dilated or the wall is fulgurated.[1,6,9] There is scant literature regarding the outcome, complications, and recurrence rates using these two methods. We present our experience with caliceal diverticular stones managed with PCNL and describe the outcomes of these two techniques to deal with diverticula after stone retrieval.
MATERIALS AND METHODS
We retrospectively analyzed data of 44 consecutive patients, who underwent PCNL for caliceal diverticular stones (CDS) from January 2001 to May 2011 at our tertiary care center. All patients were evaluated preoperatively with IVU to assess the location of diverticula and the size of stone. PCNL was performed in prone position under general anesthesia. Percutaneous access was achieved by direct stone-guided puncture with the bull's eye technique. The guide wire was coiled in the diverticulum as much as possible. The tract was dilated over the guide wire with the sequential dilators. When appropriate coiling of guide wire was not possible, we used the ‘skipping technique’ in which we replaced the thin hydrophilic wire with the stiff guide wire. This stiff guide wire facilitates one-stage tract dilation without the risk of bending. The stones were fragmented with a pneumatic lithoclast or holmium laser. After complete removal of the stones, the diverticular cavity was inspected to locate the neck of diverticula. If the neck could not be localized, methylene blue dye was instilled through the ureteric catheter placed preoperatively to aid visualization.
The diverticula were treated using one of two techniques. If the guide wire could be negotiated through the neck of diverticulum, we dilated the neck and stented it with either a ureteric catheter or double J stent (DJS). If the neck couldnot be canulated or dilated, the cavity was fulgurated using a 24 french resectoscope equipped with roller-ball electrode. A nephrostomy tube was placed for 1 to 2 days. An X-ray kidney ureter bladder (KUB) was obtained on postoperative day 1 to look for any residual stone. Postoperative follow-up included an IVU at around 3 months to assess diverticular resolution or decrease in its size and annual plain films thereafter to look for any stone recurrence. Residual or recurrent stones were treated with SWL.
RESULTS
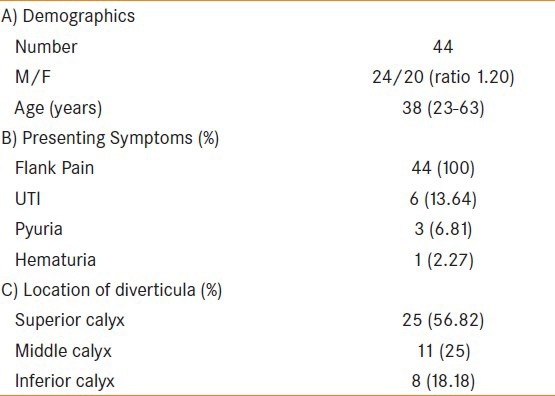
Of the 44 patients studied, 24 (55%) were males and 20 (45%) were females. The mean age was 38 years (range: 23-63 years, table 1]. One patient had CDS in a solitary functioning kidney. Flank pain was the presenting symptom in all patients, whereas six patients had recurrent urinary infection, three had pyuria, and one had hematuria. Most of the diverticula were located at the upper calyx, followed by the middle and lower calyces. The size of stones ranged from 1.1 to 3 cm (mean 1.9 cm).
Table 1.
Patient characteristics
Percutaneous access was obtained through direct stone-guided puncture in all patients. The access was infracostal in 37 and supracostal in 7 patients. The supracostal puncture was placed between the11th and 12th ribs. Stones were fragmented with a pneumatic lithoclast in 39 and with a holmium laser in 3 patients. In two patients, stones were removed in toto. We were able to cannulate and dilate the neck of diverticula in 35 (79.5%) patients, among which the ureteric catheter was placed in 29 and DJS was kept in 6 patients. In the remaining nine (20.5%) patients, the neck couldnot be localized and the walls of diverticula were fulgurated and 20 Fr nephrostomy tube was placed. The mean operative time was 87 min (range: 60-130 min). The average hospital stay was 3 days (range: 2-5 days). The nephrostomy output from fulgurated cavity ranged from 50 to 200 mL (mean: 78 mL).
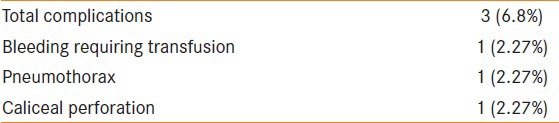
Complications occurred in three patients [Table 2]. Pneumothorax occurred in one patient with a supracostal puncture, which necessitated the placement of an intercostal drain for 4 days. One patient had caliceal perforation due to overdilatation. One patient had significant bleeding, which was diagnosed intraoperatively and responded to nephrostomy clamping and blood transfusion. This was probably venous hemorrhage. No patient had fever or UTI.
Table 2.
Operative details
Total stone clearance was obtained in 40 (90.90%) patients with PCNL alone. Four patients with incomplete clearance were successfully cleared of stones with either single (in three patients) or two (in one patient) applications of SWL. Relook PCNL was not performed in any of them. The size of residual stones ranged from 8 to 10 mm. In all of these cases, the neck could be negotiated and dilated. In two patients, a DJS was placed. The SWL was done at the interval of 7 days.
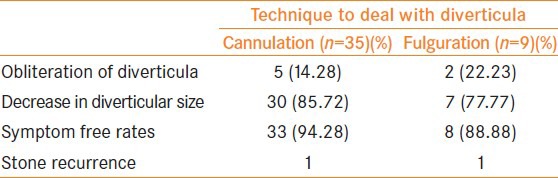
The average follow-up was 2 years (6-36 months). Postoperative IVU showed obliteration of diverticula in 7 patients and the improved drainage in 37 patients. Two patients developed recurrence of stone on yearly X-ray KUB. Forty-one patients became asymptomatic, while intermittent pain persisted in three patients. Outcomes in both techniques were similar [Table 3].
Table 3.
Outcomes of PCNL
DISCUSSION
The goals of treatment of CDS are complete removal of stone and obliteration of the diverticulum. Among various available options like SWL, PCNL, URS, and laparoscopy, percutaneous management offers the highest symptomatic relief and stone-free rates.[6,7,10,11,12] Jones et al.,[10] compared the result of SWL and PCNL. In SWL only group, 1 of 26 patients (4%) became completely stone free, although 9 (36%) became asymptomatic. Moreover, 10 patients (38.5%) of SWL group ultimately required PCNL. On the contrary, in the PCNL group, 13 of 14 patients (92.85%) were stone free and all became symptom free. The other attractive option for treatment of CDS is URS, but various studies have found only 20%-55% of stone-free rates.[7,11] Moreover, the identification of lower caliceal diverticula is very difficult by URS.[12] Auge et al.,[7] compared the outcome of PCNL and URS and found a higher stone-free (78% vs. 19%) and symptom-free (86% vs. 35%) rates in the PCNL group.
The preferred approach to PCNL is to puncture directly in the diverticula and to advance the guidewire through the diverticular neck.[13,14,15,16] Lancini et al.,[13] achieved stone-free rate of 95% and symptom-free rate of 100% with this technique. Among 40 patients treated, 35 had complete resolution of their diverticulum and remaining 5 patients had around 50% decrease in diverticular size without any recurrent stone formation. Donnellan et al.,[14] found similar stone-free rate and diverticular resolution in their series, but around 14% patients had recurrent stones, which were managed by SWL. Other studies also confirmed similar outcomes.[15,16]
Several authors have described the fulguration of diverticular cavity at the time of PCNL without making any effort to traverse the neck and establish the continuity with the remainder collecting system.[1,6,17] Usually, a small nephrostomy tube is kept in the diverticulum after the procedure. In the series of Kim et al.,[17] all 16 patients who had postoperative IVU showed a decrease in the size of diverticula and 14 (87.5%) had complete resolution. Other authors also described similar results with no recurrence of symptoms, stones, or infection.[1] Krambeck and Lingeman[6] compared outcomes in patients undergoing fulguration alone to patients who underwent diverticular neck dilatation and found a shorter hospital stay, fewer complications, and higher stone-free rates in the first group. Some authors have combined diverticular fulguration with the conventional technique of diverticular neck cannulation or dilatation in a group of patients with encouraging results.[9,18,19]
In cases where the caliceal neck cannot negotiated, some authors recommend the trans-diverticular approach with creation of a neo-infundibulum.[3,20] Ndez et al.,[3] compared these two techniques and found almost similar stone-free rates without any added complication. Proponents of this technique argue that this technique eliminates the need of prolonged probing with a wire for the neck of diverticulum.[20] We have, however, never performed this technique.
Among management options for CDS, the most versatile approach with maximum stone-free and symptom-free rates is PCNL. We found the stone clearance of 90.90% in our series, which is comparable with that reported in the literature.[13,14,15] The limitation of our study is its retrospective nature. However, the rarity of CSD limits the possibility of a prospective analysis. The importance of our data lies in the fact that we analyzed a relatively large number of patients. We suggest using a method to deal with diverticula after stone extraction depending on the neck of diverticula. If we are able to canulate the neck, drainage of the diverticula to the remaining PCS can be performed by the ureteric catheter or DJS, otherwise simple fulguration of diverticular wall with external drainage by a small nephrostomy tube is a good option.
CONCLUSIONS
PCNL can clear calculi from caliceal diverticula in most cases with minimal morbidity. After stone retrieval, the diverticula may be drained into the PCS if the neck can be negotiated, otherwise it can be fulgurated.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Monga M, Smith R, Ferral H, Thomas R. Percutaneous ablation of caliceal diverticulum: Long-term followup. J Urol. 2000;163:28–32. [PubMed] [Google Scholar]
- 2.Hulbert JC, Reddy PK, Hunter DW, Castaneda-Zuniga W, Amplatz K, Lange PH. Percutaneous techniques for the management of caliceal diverticula containing calculi. J Urol. 1986;135:225–7. doi: 10.1016/s0022-5347(17)45590-x. [DOI] [PubMed] [Google Scholar]
- 3.M Ndez-Probst CE, Fuller A, Nott L, Denstedt JD, Razvi H. Percutaneous nephrolithotomy of caliceal diverticular calculi: A single center experience. J Endourol. 2011;25:1741–5. doi: 10.1089/end.2011.0046. [DOI] [PubMed] [Google Scholar]
- 4.Grasso M, Lang G, Loisides P, Bagley D, Taylor F. Endoscopic management of the symptomatic caliceal diverticular calculus. J Urol. 1995;153:1878–81. [PubMed] [Google Scholar]
- 5.Kriegmair M, Schüller J, Schmeller N, Knipper A, Muschter R, Hofstetter AG. Diverticular calculi of the kidney calices – extracorporeal shockwave lithotripsy, percutaneous extraction or open surgery. Urologe A. 1990;29:204–8. [PubMed] [Google Scholar]
- 6.Krambeck AE, Lingeman JE. Percutaneous management of caliceal diverticuli. J Endourol. 2009;23:1723–9. doi: 10.1089/end.2009.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Auge BK, Munver R, Kourambas J, Newman GE, Preminger GM. Endoscopic management of symptomatic caliceal diverticula: A retrospective comparison of percutaneous nephrolithotripsy and ureteroscopy. J Endourol. 2002;16:557–63. doi: 10.1089/089277902320913233. [DOI] [PubMed] [Google Scholar]
- 8.Waxman SW, Winfield HN. Laparoscopic management of caliceal diverticulum. J Endourol. 2009;23:1731–2. doi: 10.1089/end.2009.1542. [DOI] [PubMed] [Google Scholar]
- 9.Landry JL, Colombel M, Rouviere O, Lezrek M, Gelet A, Dubernard JM, et al. Long term results of percutaneous treatment of caliceal diverticular calculi. Eur Urol. 2002;41:474–7. doi: 10.1016/s0302-2838(02)00039-8. [DOI] [PubMed] [Google Scholar]
- 10.Jones JA, Lingeman JE, Steidle CP. The roles of extracorporeal shock wave lithotripsy and percutaneous nephrostolithotomy in the management of pyelocaliceal diverticula. J Urol. 1991;146:724–7. doi: 10.1016/s0022-5347(17)37906-5. [DOI] [PubMed] [Google Scholar]
- 11.Sejiny M, Al-Qahtani S, Elhaous A, Molimard B, Traxer O. Efficacy of flexible ureterorenoscopy with holmium laser in the management of stone-bearing caliceal diverticula. J Endourol. 2010;24:961–7. doi: 10.1089/end.2009.0437. [DOI] [PubMed] [Google Scholar]
- 12.Batter SJ, Dretler SP. Ureterorenoscopic approach to the symptomatic caliceal diverticulum. J Urol. 1997;158(3 Pt 1):709–13. doi: 10.1097/00005392-199709000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Lancini V, Liatsikos EN, Bernardo NO, Dinlenc CZ, Kapoor R, Smith AD. Percutaneous treatment of calculosis in caliceal diverticulosis: 13-year experience. Arch Ital Urol Androl. 2000;72:59–63. [PubMed] [Google Scholar]
- 14.Donnellan SM, Harewood LM, Webb DR. Percutaneous management of caliceal diverticular calculi: Technique and outcome. J Endourol. 1999;13:83–8. doi: 10.1089/end.1999.13.83. [DOI] [PubMed] [Google Scholar]
- 15.Lagha K, Martin X, Cuzin B, Gelet A, Maréchal JM, Desmettre O, et al. Treatment of intradiverticular lithiasis by percutaneous methods (19 caliceal diverticuli) Prog Urol. 1993;3:959–63. [PubMed] [Google Scholar]
- 16.Bellman GC, Silverstein JI, Blickensderfer S, Smith AD. Technique and follow-up of percutaneous management of caliceal diverticula. Urology. 1993;42:21–5. doi: 10.1016/0090-4295(93)90327-7. [DOI] [PubMed] [Google Scholar]
- 17.Kim SC, Kuo RL, Tinmouth WW, Watkins S, Lingeman JE. Percutaneous nephrolithotomy for caliceal diverticular calculi: A novel single stage approach. J Urol. 2005;173:1194–8. doi: 10.1097/01.ju.0000152320.41995.c2. [DOI] [PubMed] [Google Scholar]
- 18.Shalhav AL, Soble JJ, Nakada SY, Wolf JS, Jr, McClennan BL, Clayman RV. Long-term outcome of caliceal diverticula following percutaneous endosurgical management. J Urol. 1998;160:1635–9. [PubMed] [Google Scholar]
- 19.Ellis JH, Patterson SK, Sonda LP, Platt JF, Sheffner SE, Woolsey EJ. Stones and infection in renal caliceal diverticula: Treatment with percutaneous procedures. AJR Am J Roentgenol. 1991;156:995–1000. doi: 10.2214/ajr.156.5.1902014. [DOI] [PubMed] [Google Scholar]
- 20.Al-Basam S, Bennett JD, Layton ZA, Denstedt JD, Razvi H. Treatment of caliceal diverticular stones: Transdiverticular percutaneous nephrolithotomy with creation of a neoinfundibulum. J Vasc Interv Radiol. 2000;11:885–9. doi: 10.1016/s1051-0443(07)61806-5. [DOI] [PubMed] [Google Scholar]


