Abstract
Introduction:
Micropenis is defined as a stretched penile length 2.5 standard deviations less than the mean for age without the presence of any other penile anomalies, such as hypospadias. The term refers to a specific disorder that has a known set of causative factors and defined treatment modalities. The purpose of this study was to determine the effect of hormonal therapy on the gonadal response and penile growth in children who presented with micropenis.
Materials and Methods:
Children (<18 years) who met the criteria for micropenis were included in this study. Children more than 11 years old were treated using a standard protocol of 1,500 to 2,000 IU human chorionic gonadotrophin administrated intramuscularly, once per week, for 6 weeks. Children less than 11 years old were treated with parenteral testosterone enanthate 25 mg once a month for 3 months. Response was evaluated in terms of change in testosterone levels and size of penis.
Results:
Serum testosterone levels at baseline and after 8 weeks of hormonal treatment were <20 and 449.4 ng/mL, respectively (P < 0.0001) in all children more than 11 years old. Stretched penile length after hormonal treatment increased from 15.54 to 37.18 mm in children less than 11 years old and from 26.42 to 64.28 mm in children more than 11 years old (P < 0.001).
Conclusions:
Management of isolated micropenis revolves around testosterone (direct administration or encouraging the patient's body to make its own), and results with respect to increase in penile length are promising.
Keywords: Children, human chorionic gonadotropin, micropenis, testosterone
INTRODUCTION
The mean stretched penile length in a full-term newborn male is 3.5 cm. Measurements of less than 2-2.5 cm (2.5 standard deviations (SDs) below the mean) in a full-term newborn male meet the definition of micropenis and warrant further evaluation.[1,2] The growth of penis during mid to late gestation is essentially linear. The following formula is commonly used to determine penile length in relation to gestational age[3]: Penile length (cms) = 2.27 + 0.16 × (gestational age in weeks).
At times, micropenis may be considered a form of ambiguous genitalia. However, presence of a normal scrotum and palpable testes indicate a high probability of normal male karyotype. Micropenis may be caused by a defect anywhere along the hypothalamic-pituitary-gonadal axis, a defect in peripheral androgen action, isolated growth hormone (GH) deficiency, a primary structural anomaly, or may be part of a genetic syndrome. The most common cause of micropenis is abnormal hypothalamic or pituitary function. In the absence of normal hypothalamic or pituitary function, a normally shaped penis may develop due to maternal human chorionic gonadotrophin (hCG) effect on fetal testosterone production, but adequate penile growth does not occur after 14 weeks’ gestation when testosterone production depends on intact fetal pituitary luteinizing hormone (LH) secretion. Failure of adequate testosterone production toward the end of gestation due to a primary testicular disorder can also result in inadequate penis growth.
Micropenis can also occur in children with LH-receptor defects and defects in testosterone biosynthesis (e.g., 17-beta hydroxysteroid dehydrogenase deficiency).[4] The genitalia of individuals with LH-receptor defects vary from normal female-appearing to male-appearing with micropenis. Individuals with 17-beta hydroxysteroid dehydrogenase deficiency most often have female-appearing genitalia and, less often, ambiguous genitalia.[5] Defects in peripheral androgen action include failure of conversion of testosterone to dihydrotestosterone and partial responsiveness due to an androgen receptor defect. However, most children with these conditions have varying degrees of incomplete labioscrotal fusion, resulting in hypospadias and genital ambiguity.[5] Last, genetic syndromes in which micropenis may be a feature include Klinefelter and Noonan syndromes, among others.[5]
Some studies[6] have evaluated the response of micropenis to hCG therapy in adolescent or adult men with idiopathic hypogonadotropic hypogonadism (IHH). The purpose of this study was to determine the effect of hormonal therapy on the gonadal response and penile growth in children who presented with micropenis.
MATERIALS AND METHODS
This chart based, retrospective study was approved by our institutional review board and ethics committee. Children (<18 years) who met the criteria for micropenis were included (Figure 1). Children with cryptorchidism or absence of testis according to the imaging studies conducted at the initial presentation were excluded from the study. Similarly, children with hypospadias were also excluded from the study. The protocol we follow in the evaluation of these children is shown in Figure 2. The hCG stimulation test was not performed in any of the children. Pretreatment estimation of serum LH, follicle-stimulating hormone (FSH) and testosterone was done in all (pubertal/postpubertal) children more than 11 years old. A diagnosis of IHH was made on the basis of low or normal serum LH and FSH concentrations associated with low serum testosterone. Testis volume was assessed in children more than 11 years old using the Prader orchidometer. Penis length (flaccid and stretched) and testicular volume were measured before and after hormonal treatment in all children.
Figure 1.
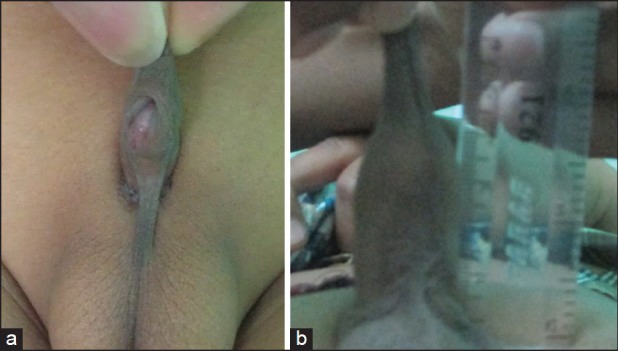
(a) A 10-year-old boy presenting with stretched penile length of 16 mm (b) Post treatment stretched penile length increased to 44 mm
Figure 2.
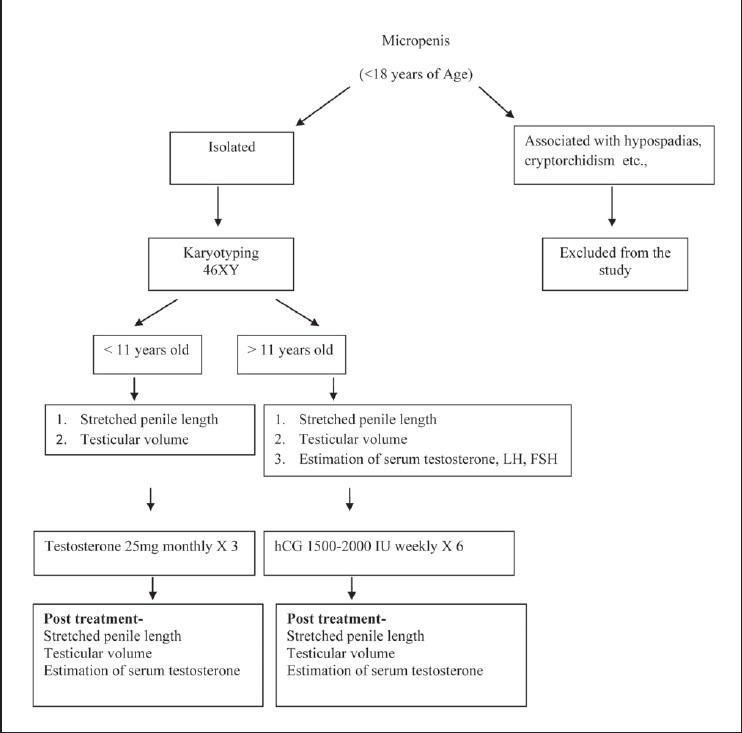
Algorithm for evaluation and management of micropenis
Children more than 11 years old (pubertal/postpubertal) were treated using a standard protocol of 1,500 to 2,000 IU hCG administrated intramuscularly, once per week, for 6 weeks, whereas children less than 11 years old (prepubertal) were treated with parenteral testosterone enanthate 25 mg once a month for 3 months. This change in treatment plan depending on age was followed so as to promote the older child's own testes to produce testosterone. Penile length was measured by the same physician. A wooden spatula was pressed against the pubic ramus depressing the suprapubic pad of fat as completely as possible to ensure that the part of the penis that is buried in the subcutaneous fat was measured. Measurement was made along the dorsum of the penis to the tip of the glans penis. The length of foreskin was not included.
The data are given as the mean ± SD unless otherwise indicated. Comparisons of data within a patient were evaluated by Student's t-test; comparisons of data from different subsets were evaluated by unpaired t test.
RESULTS
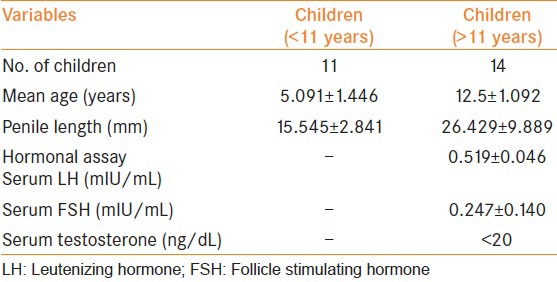
Between July 2000 and June 2009, 25 children presented with micropenis. The clinical features of the children are shown in Table 1. Their mean age was 9.24 ± 3.95 years (range: 3-14 years).
Table 1.
The basal characteristics of the children before hormonal treatment
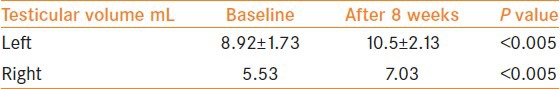
In children less than 11 years of age, mean penile length increased significantly after hormonal treatment from 15.54 mm to 37.18 mm (Table 2). In children greater than 11 years, serum testosterone level increased significantly after 8 weeks of hormonal treatment from <20 to 449.4 ng/ml (P < 0.0001). The mean penile length also increased significantly from 26.42 mm to 64.28 mm (P < 0.001) [Table 2]. In the older children, mean testicular volume increased from 5.45 cc to 6.83 cc on the left side and from 5.53 cc to 7.03 cc on the right side (P < 0.005) after hormonal treatment [Table 3]. There were no significant adverse events related to the hormonal treatment.
Table 2.
Testosterone levels and penile length before and after hormonal treatment
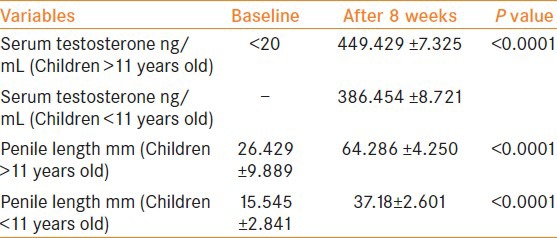
Table 3.
Testicular volumes before and after hormonal treatment
DISCUSSION
Micropenis refers to an extremely small penis with a stretched penile length of less than 2.5 SD below the mean for age or stage of sexual development.[7,8,9,10] The ratio of the length of the penile shaft to its circumference is usually normal, but occasionally, the corpora cavernosa are severely hypoplastic. The testes are usually small and frequently cryptorchid, whereas the scrotum is usually fused. Stretched penile length is used as a measure because it correlates more closely with erectile length than does relaxed penile length. Measurements should be compared with existing standards for penile length. Micropenis needs to be differentiated from a webbed or buried penis.
The initial evaluation of a child with micropenis should include a thorough medical history and a karyotype at birth. Accurate measurement of the penile length, palpation of the corporeal bodies, and evaluation for cryptorchidism are several important aspects of the physical examination. Kumanov et al.,[11] prospectively studied Bulgarian boys and established wide regional variation of normal penile lengths. It is very important to consider regional as well as ethnic differences while approaching diagnostic and therapeutic considerations. Consultation with a pediatric endocrinologist is also usually obtained to determine the cause of micropenis and to assess whether other abnormalities are present. Several issues need to be addressed, including the growth potential of the penis and the etiology of the micropenis. Testicular function may be assessed by measuring serum testosterone levels before and after hCG stimulation. Primary testicular failure produces an absent response and elevated basal concentrations of LH and FSH. Endocrinologic evaluation can also isolate the cause of micropenis to its level in the hypothalamic-pituitary-testicular axis. Specifically, prolactin (PRL) levels help isolate the defect to the hypothalamus (high PRL) versus the pituitary (low PRL).[5] In addition, plasma GH, thyroid stimulating hormone, and adrenocorticotropic hormone (ACTH) can all be used to isolate the dysfunction. Interestingly, it may be difficult to make the diagnosis of hypogonadotrophic hypogonadism in the prepubertal patient with micropenis if they are past infancy, as there is a quiescent phase of the pituitary that sees levels of FSH and LH drop precipitously.[5]
Sometimes, extensive evaluation of the hypothalamic-pituitary-testicular axis needs to be done before androgen therapy is administered to determine the end organ response. Several studieshave shown that patients with IHH had a good response to hCG therapy in terms of penile growth, testicular growth, and elevation of serum testosterone.[6] Treatment of micropenis should focus on penile size sufficient for the child to have an appropriate body image, normal sexual function, and standing micturition. Inability to bring the penis fully to the mean measurement for age does not imply failure. Primary treatment of micropenis revolves around exogenous testosterone administration to increase the length of the penis so that it may be considered within a range of normal. Good responses are typically seen with increases of over 100% in penile length over the course of initial treatment to be expected.[12,13,14]
Kim et al.,[6] included 20 IHH patients who met the criteria for micropenis and were administrated hCG intramuscularly, 3 times per week, for 8 weeks. The mean serum testosterone level was significantly increased after hCG treatment (P < 0.05). Mean penile length also increased significantly 24 weeks after treatment, stretched penile length increased from 5.41 ± 1.43 cm to 7.45 ± 1.70 cm; P < 0.001. Mean testicular volumes increased significantly as well (left: from 5.45 to 6.83 cc; right: from 5.53 to 7.03 cc). Schopohl et al.,[14] reported that gonadotropin therapy with 3 × 2,500 IU hCG as a weekly intramuscular injection restored endocrine and exocrine testicular function to the normal range in male patients with IHH. They showed that the serum level of testosterone, positive sperm count, and testicular volume was increased significantly in the gonadotropin-injected group.
Apart from primary treatment of micropenis, repeat hormone administrations may be performed over short-time periods if the response is not deemed satisfactory.[15] There have been concerns about the administration of testosterone to prepubertal patients and the impact on their ultimate penile length. Current long-term data regarding patients treated in childhood with exogenous testosterone have shown no reduction in adult penile length.[16]
CONCLUSIONS
Exogenous administration of testosterone to pre-pubertal boys and hCG to pubertal or post-pubertal boys results in significant increase in stretched penile length. This may be the primary form of treatment for micropenis in these children.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Wessells H, Lue TF, McAninch JW. Penile length in the flaccid and erect states: Guidelines for penile augmentation. J Urol. 1996;156:995–7. [PubMed] [Google Scholar]
- 2.Feldman KW, Smith DW. Fetal phallic growth and penile standards for newborn male infants. J Pediatr. 1975;86:395–8. doi: 10.1016/s0022-3476(75)80969-3. [DOI] [PubMed] [Google Scholar]
- 3.Tuladhar R, Davis PG, Batch J, Doyle LW. Establishment of a normal range of penile length in preterm infants. J Paediatr Child Health. 1998;34:471–3. doi: 10.1046/j.1440-1754.1998.00278.x. [DOI] [PubMed] [Google Scholar]
- 4.Kallmann FJ, Schoenfeld WA, Barrera SE. The genetic aspects of primary eunuchoidism. Am J Ment Defic. 1944;48:203–36. [Google Scholar]
- 5.Adan L, Couto-Silva AC, Trivin C, Metz C, Brauner R. Congenital gonadotropin deficiency in boys: Management during childhood. J Pediatr Endocrinol Metab. 2004;17:149–55. doi: 10.1515/jpem.2004.17.2.149. [DOI] [PubMed] [Google Scholar]
- 6.6 Kim SO, Ryu KH, Hwang IS, Jung SI, Oh KJ, Park K. penile growth in response to human chorionic gonadotropin (HCG) treatment in patients with idiopathic hypogonadotrophic hypogonadism. Chonnam Med J. 2011;47:39–42. doi: 10.4068/cmj.2011.47.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee PA, Mazur T, Danish R, Amrhein J, Blizzard RM, Money J, et al. Micropenis. I. Criteria, etiologies and classification. Johns Hopkins Med J. 1980;146:156–63. [PubMed] [Google Scholar]
- 8.Al-Herbish AS. Standard penile size for normal full term newborns in the Saudi population. Saudi Med J. 2002;23:314–6. [PubMed] [Google Scholar]
- 9.Allen TD. Microphallus: Clinical and endrocrinological characteristics. J Urol. 1978;119:750–3. doi: 10.1016/s0022-5347(17)57621-1. [DOI] [PubMed] [Google Scholar]
- 10.Savage MO. Ambiguous genitalia, small genitalia and undescended testes. Clin Endocrinol Metab. 1982;11:127–58. doi: 10.1016/s0300-595x(82)80040-6. [DOI] [PubMed] [Google Scholar]
- 11.Kumanov P, Robeva R, Tomova A. Prevalence of micropenis among boys from different regions of Bulgaria. J Pediatr Endocrinol Metab. 2007;20:791–5. doi: 10.1515/jpem.2007.20.7.791. [DOI] [PubMed] [Google Scholar]
- 12.Bin-Abbas B, Conte FA, Grumbach MM, Kaplan SL. Congenital hypogonadotropic hypogonadism and micropenis: Effect of testosterone treatment on adult penile size why sex reversal is not indicated. J Pediatr. 1999;134:579–83. doi: 10.1016/s0022-3476(99)70244-1. [DOI] [PubMed] [Google Scholar]
- 13.Burstein S, Grumbach MM, Kaplan SL. Early determination of androgen-responsiveness is important in the management of microphallus. Lancet. 1979;2:983–6. doi: 10.1016/s0140-6736(79)92560-1. [DOI] [PubMed] [Google Scholar]
- 14.Schopohl J, Mehltretter G, von Zumbusch R, Eversmann T, von Werder K. Comparison of gonadotropin-releasing hormone and gonadotropin therapy in male patients with idiopathic hypothalamic hypogonadism. Fertil Steril. 1991;56:1143–50. [PubMed] [Google Scholar]
- 15.Grumbach MM. A window of opportunity: The diagnosis of gonadotropin deficiency in the male infant. J Clin Endocrinol Metab. 2005;90:3122–7. doi: 10.1210/jc.2004-2465. [DOI] [PubMed] [Google Scholar]
- 16.Cortes D, Müller J, Skakkebaek NE. Proliferation of Sertoli cells during development of the human testis assessed by stereological methods. Int J Androl. 1987;10:589–96. doi: 10.1111/j.1365-2605.1987.tb00358.x. [DOI] [PubMed] [Google Scholar]


