Abstract
Augmentation cystoplasty (AC) has traditionally been used in the treatment of the low capacity, poorly compliant or refractory overactive bladder (OAB). The use of intravesical botulinum toxin and sacral neuromodulation in detrusor overactivity has reduced the number of AC performed for this indication. However, AC remains important in the pediatric and renal transplant setting and still remains a viable option for refractory OAB. Advances in surgical technique have seen the development of both laparoscopic and robotic augmentation cystoplasty. A variety of intestinal segments can be used although ileocystoplasty remains the most common performed procedure. Early complications include thromboembolism and mortality, whereas long-term problems include metabolic disturbance, bacteriuria, urinary tract stones, incontinence, perforation, the need for intermittent self-catheterization and carcinoma. This article examines the contemporary indications, published results and possible future directions for augmentation cystoplasty.
Keywords: Complication, cystoplasty, reconstruction
INTRODUCTION
Augmentation cystoplasty (AC) has been used in adult patients for the treatment of the low capacity, poorly compliant or refractory overactive bladder (OAB). In addition, in the pediatric population, it is an invaluable technique for lower urinary tract reconstruction following congenital urological anomalies for example bladder exstrophy. In principle, it involves the use of bowel segments to increase bladder capacity, thereby protecting the upper tract whilst allowing patients to be continent and improving their symptoms.[1]
Whilst traditionally, AC has been used in the context of OAB management, the past two decades have seen the rise of anticholinergic medications for OAB, intravesical botulinum toxin and more recently sacral neuromodulation.[2,3,4] Those interventions have proved to be safe and effective and are appealing both to patients and doctors. They have therefore reduced the need for AC and certainly in the UK setting, there has been a reduction in the number of AC procedures over the past decade.[1] In addition, 5 years cost analysis appears to favor botulinum toxin compared to AC in refractory detrusor overactivity.[5]
In this review, we re-examine the contemporary indications, technical updates and future of AC.
CURRENT INDICATIONS FOR AC
AC remains an option, with high patient satisfaction rates, in neurogenic and non-neurogenic bladder dysfunction when conservative management, pharmacological methods and minimally invasive treatments have been unsuccessful and exhausted.[6,7] Patients with detrusor overactivity would initially undergo conservative measures with the addition of anticholinergic medications. If these are unsuccessful, the next step would be a trial of intravesical botulinum toxin medications or sacral neuromodulation. Patients who fail treatment with all those modalities are then considered for augmentation cystoplasty. In refractory neurogenic bladder dysfunction, Khastgir et al. (2003) found high satisfaction rates, in addition to successful surgical outcomes (increase in bladder capacity, reduction in detrusor pressure and resolution of concurrent reflux), in 32 spinal cord injured patients following augmentation cystoplasty and Zachoval et al. (2003) reported similar outcomes in patients with multiple sclerosis.[8,9] The literature reveals a satisfactory outcome from AC (as measured by post-operative symptom scores or urodynamic parameters of bladder capacity, detrusor compliance and emptying) in up to 88% of patients with a variable clean intermittent self-catheterization rate (ISC) of 10-75%.[10,11,12,13,14]
AC also retains a role in the management of infective and inflammatory bladder disorders, which lead to a low capacity and poorly compliant bladder. Such conditions include post-radiotherapy cystitis, cystitis following intravesical or systemic chemotherapy, schistosomiasis, tuberculosis and interstitial cystitis.[10,11] In interstitial cystitis/bladder pain syndrome, studies have been limited by small patient numbers and results have been variable.[12,13,14] The best results are seen in patients with interstitial cystitis who have Hunner's ulcers where complete pain relief is seen in 63%, but it is well-reported that patients may get a recurrence of pain in the augmented bladder.[12,13,14] There have been few recent reports on AC in radiotherapy patients, but traditional studies have estimated the success rate at about 70%.[15,16]
In the pediatric population in congenital bladder anomalies (bladder exstrophy, epispadias, posterior urethral valves), AC achieves an increase in bladder capacity and reduces upper tract complications.[17,18,19]
In the setting of renal transplantation, AC is considered to be better than ileal conduit urinary diversion in a recipient with associated lower-urinary tract dysfunction with a lower complication rate.[20,21] AC can be performed before, after or at the time of transplantation with little evidence of difference in graft survival or febrile episodes between each technique.[22,23]
SURGICAL PERSPECTIVE AND TECHNIQUES
Ileocystoplasty is the most common bladder augmentation procedure. Mikulicz initially described augmentation ileocystoplasty in humans in 1889.[24] The technique gained acceptance in the 1950s for the management of tuberculous bladders and was further popularized by Bramble in the 1980s in conjunction with ISC.[6] Several other gastro-intestinal segments have been used in augmentation including stomach, cecum, ascending and sigmoid colon.[1,25] The selection of an intestinal segment for augmentation needs to be given some thought: small bowel is the segment of choice for the majority of surgeons due to its ease of handling; however, post pelvic radiotherapy, this may not be suitable as the bowel is often in the irradiated field and as such a colonic conduit might be preferable. Similar considerations apply in patients undergoing redo – procedures. Gastic segments for augmentation were once popular especially in the pediatric population, but have fallen out of favor due to higher risk of complications.[1,25,26,27]
Open technique
AC has traditionally been performed via an open approach with sagittal bivalving of the bladder and anastomosis of the bowel segment onto the native bladder [Figure 1].[1,6] The most widely used bowel segment for AC is a detubularized patch of ileum, usually taken about 25-40 cm from the ileocecal valve.[6,26] If cecum is used, it is often used in conjunction with the terminal ileum as an ileocaecocystoplasty.[27] Alternatives to using gastrointestinal tissue have been auto-augmentation (detrusor myomectomy) where detrusor muscle is stripped from the bladder with an overall success of 50-70%[28] or ureterocystoplasty using a pre-existing dilated ureter, but up to 24% of those require revision surgery.[29,30] Advances in surgical technique have seen laparoscopic gastrocystoplasty and ileocystoplasty[31] and more recently robotic augmentation ileocystoplasty being performed.[32]
Figure 1.
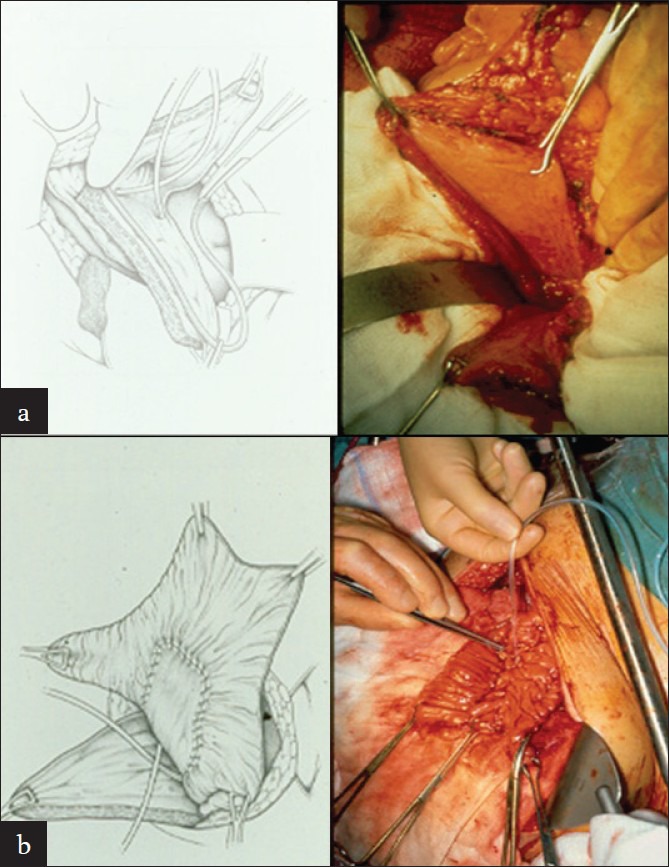
(a) Bivalving of bladder, (b) Anastomosis of detubularized ileal patch
Laparoscopic and robotic approach
Laparoscopic enterocystoplasty was first described by Gill et al. (2000) in a series of three patients with small capacity neurogenic bladders who underwent laparoscopic ileocystoplasty, sigmoidocystoplasty and cystoplasty with cecum and proximal ascending colon. After the creation of a veress needle pneumoperitoneum, a four-port transperitoneal laparoscopic approach was used and an appropriate 15-cm length of bowel was identified. The distal end of the selected bowel segment was marked with a superficial electrocautery burn for identification. After desufflation, the preselected loop of the bowel was delivered outside the abdomen through a 2-cm extension of the umbilical port incision. Using open technique, the appropriate bowel segment with its mesenteric pedicle was isolated, bowel continuity was re-established and the isolated bowel segment was detubularized along its antimesenteric border. An orientation suture was placed at the cephalad end and at the caudal end of the bowel patch to facilitate subsequent laparoscopic identification. The bowel was then returned to the abdominal cavity. An anteroposterior cystotomy incision was created laparoscopically using electrosurgical scissors. Circumferential, continuous, full-thickness, single-layer anastomosis of the bowel mucosa and muscularis with the bladder wall was then created by laparoscopic suturing. [31] A similar surgical approach is used for robot-assisted enterocystoplasty. The robot-assisted laparoscopic operation has merits such as a device with seven degrees of freedom, high-resolution, three-dimensional pictures, direct-view movement and removal of hand shaking, which facilitate intracorporeal dissection and suturing.[32] Those minimally invasive procedures are feasible and efficaciously duplicate the established principles of open enterocystoplasty while minimizing operative morbidity, expediting convalescence and enhancing cosmesis.[31,32] They are however associated with increased operative time.
COMPLICATIONS
AC is a major abdominal operation and hence a variety of early and late complications have been described in the literature. Early complications include thromboembolism and mortality whereas long-term problems include metabolic disturbance, bacteriuria, urinary tract stones, incontinence, perforation, incontinence and carcinoma [Table 1][8,17,18,41,50,51,52].
Table 1.
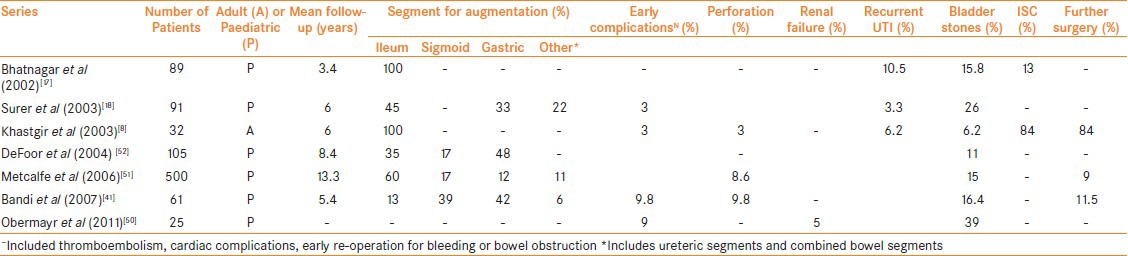
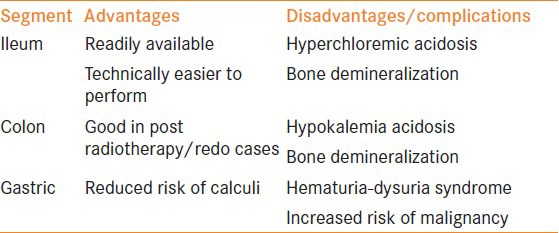
Table 2.
indications and complications of intestinal segments
Thromboembolism, cardiovascular and gastrointestinal complications
Early complications of AC include cardiovascular, thrombo-embolic, respiratory and gastrointestinal complications associated with any major abdominal procedure.[33] The post-operative myocardial infarction rate was up to 2.7% and the incidence of deep vein thrombosis/pulmonary embolism was as high as 7.1% in an early series of 185 patients highlighting the need for adequate thromboprophylaxis.[16,34] The mortality rate from AC is reported to be between 0% and 2.7% with a re-operation rate for bleeding of up to 3.2%,[35] small bowel obstruction of up to 5.7%[34] and wound infection of up to 7.1%.[27]
Metabolic acidosis, calcium balance and hypokalemia in ileo-and colo-cystoplasty
Perhaps the most well-known long-term complication of AC is the metabolic disturbance characterized by hyperchloremic acidosis. This is the result of re-absorption of ammonium and ammonium chloride and the secretion of bicarbonate by the bowel segment and is often seen in the context of ileocystoplasty.[36,37]
This chronic metabolic acidosis can cause mobilization of calcium carbonate from bone to act as a buffer and calcium can therefore be excreted in the urine.[38] Depletion of bone calcium can in turn lead to reduced growth potential in children. Indeed, studies have shown that one in five children having undergone colocystoplasty show a 50% of reduction in growth rate.[33,39,40] Another metabolic disturbance particularly associated with colocystoplasty is hypokalemia due to secretion of potassium by the colonic patch.[41] In the setting of gastrocystoplasty, hypochloremic metabolic alkalosis occurs due to loss of gastric acid in the urine. Kurzrock et al. (1998) noted that this phenomenon occurred in up to 7% of gastrocystoplasties, but rarely required clinical correction.[42,43]
Reflux and renal function
Augmentation lowers intravesical pressure and increases bladder compliance during the urine storage phase and therefore reflux usually improves or resolves post AC.[44] Renal function has variably been reported to improve, remain stable or deteriorate post AC. In studies that have shown deterioration in renal function, the rate of decline appeared to be related to the pre-operative creatinine clearance – one study found deterioration in only 4.1% of patients who had a creatinine clearance of ≥40 mL/min.[34] Therefore, whilst significant renal impairment has traditionally been a relative contraindication, this is now viewed as controversial. Studies in neuropathic pediatric patients with chronic renal impairment undergoing AC showed no change in renal function at 2 year follow-up in 73% using ileal or colonic segments. The specific role of different bowel segments on the rate of decline of renal function has not been extensively studied in the literature – however, in patients with pre-existing renal impairment; thought must be given to re-implanting the ureters in an anti-reflux fashion at the time of AC to minimize the upper tract damage by reflux. In addition, use of gastric segments in those patients is associated with reduced risk of absorption of electrolytes and urinary tract infections (UTIs), but this must be carefully balanced against the other risks of gastrocystoplasty including peptic ulceration of bladder, hematuria– dysuria syndrome and risk of malignancy.[1,42,43]
ISC, UTI AND URINARY TRACT CALCULI
Since the native bladder and intestinal patch cannot contract simultaneously, emptying the augmented bladder is dependent upon abdominal straining to increase abdominal pressure and simultaneous relaxation of the pelvic floor.[45] Many patients are therefore reliant on ISC to reliably empty the augmented bladder. ISC rates vary from 26% to 100%, generally increase with time and are higher in the neuropathic group of patients.[27,46,47] For instance, Greenwell et al.(2001) reported a 60% ISC rate in neuropathic patients compared with 6% in idiopathic patients.[33]
ISC may be associated with UTI in AC. Whilst asymptomatic bacteriuria can be very common in AC, the incidence of symptomatic UTI is reportedly lower. One study showed recurrent bacteriuria rate of 75%, but only a 20% incidence of troublesome UTI.[33] UTIs in AC patients have been associated with large residual volumes, the presence of mucus and the need to use ISC.[1,33,48,49]
UTI in these patients has also been associated with the formation of bladder calculi.
Bladder stones have been reported in up to 40% of AC and are thought to arise as a result of urinary stasis.[1,50] One of the largest series of 500 pediatric patients undergoing AC showed a 15% rate of bladder calculi.[51] Bladder calculi are five times as common in augmented patients who use ISC when the bladder is catheterized urethrally and 10 times as common in patients with Mitrofanoff-type channels.[52,53] The risk factors for urolithiasis post AC include urinary stasis and UTI and patients with inadequate bladder emptying should perform ISC and have UTIs treated promptly. Furthermore in cases where AC is combined with ureteric reimplantation, a non-refluxing ureteroneocystostomy should be considered to reduce the risk of upper tract reflux and calculi.[52,53]
There is however a lower incidence of stones in gastrocystoplasty, which may be related to the lower quantity of mucus production, the lower urinary pH and the lower incidence of bacteriuria.[54] Most of the stones can be removed endoscopically, but patients with large stones and those with no urethral access require open surgery for removal.[54]
Bladder perforation and carcinoma
Both those complications are rare but require a high index of suspicion to diagnose. Spontaneous bladder perforation is a life-threatening complication of augmentation, with a reported mortality of up to 25%.[55] The median time from surgery is about 35 months, with 33% ≤2 years and 35% between 2 and 6 years after augmentation.[56] The most usual site of perforation is the junction between the bowel and bladder wall and rupture may be explained by local ischemia of this area.[57] Most perforations are intra-abdominal and exploratory laparotomy is warranted in clinical cases of suspected balder rupture as the diagnosis can often only be made intraoperatively.[55,58]
The risk of malignancy in the augmented bladder has been estimated to be around 1.2% and a typically exhibits a long latency period (19-22 years).[59,60] The highest risk appears to be following gastrocystoplasty.[61,62] Tumors tend to be adenocarcinoma although transitional cell carcinomas have been reported. Recommendations have been made for routine cystoscopic surveillance to begin 10 years after enterocystoplasty on an annual basis.[60]
Urinary and bowel function
Resection of the terminal ileum can lead to bile acid malabsorption, diarrhea and fat malabsorption.[63] Troublesome gastrointestinal symptoms including diarrhea occur in up to 25% of patients, but augmentation with sigmoid appears to have less effect upon the bowel function than ileocystoplasty.[64] As regards bladder function, incontinence is sometimes a problem after AC, particularly at night. Large series have published continence rates of 78% with cystoplasty alone.[1,33] Management of incontinence post AC includes ISC, anticholinergic medications, further reconstructive bladder neck surgery or urinary diversion, or insertion of an artificial urinary sphincter. The literature shows a continence rate of 80-100% with these adjuvant treatments.[33]
CONCLUSION
AC retains a role in modern urological practice especially in refractory OAB and the pediatric population. Large studies have proven the efficacy of AC by improving patient symptoms and urodynamic parameters. Developments in technique have seen laparoscopic and robotic AC being performed with minimal morbidity. The long-term complications are well-documented in the literature.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Biers SM, Venn SN, Greenwell TJ. The past, present and future of augmentation cystoplasty. BJU Int. 2012;109:1280–93. doi: 10.1111/j.1464-410X.2011.10650.x. [DOI] [PubMed] [Google Scholar]
- 2.Duthie JB, Vincent M, Herbison GP, Wilson DI, Wilson D. Botulinum toxin injections for adults with overactive bladder syndrome. Cochrane Database Syst Rev. 2011 Dec 7;12:CD005493. doi: 10.1002/14651858.CD005493.pub3. [DOI] [PubMed] [Google Scholar]
- 3.Herbison GP, Arnold EP. Sacral neuromodulation with implanted devices for urinary storage and voiding dysfunctionin adults. Cochrane Database Syst Rev. 2009 Apr 15;2:CD004202. doi: 10.1002/14651858.CD004202.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Madhuvrata P, Cody JD, Ellis G, Herbison GP, Hay-Smith EJ. Which anticholinergic drug for overactive bladder symptoms in adults. Cochrane Database Syst Rev. 2012;1:CD005429. doi: 10.1002/14651858.CD005429.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Padmanabhan P, Scarpero HM, Milam DF, Dmochowski RR, Penson DF. Five-year cost analysis of intra-detrusor injection of botulinum toxin type A and augmentation cystoplasty for refractory neurogenic detrusor overactivity. World J Urol. 2011;29:51–7. doi: 10.1007/s00345-010-0618-3. [DOI] [PubMed] [Google Scholar]
- 6.Bramble FJ. The treatment of adult enuresis and urge incontinence by enterocystoplasty. Br J Urol. 1982;54:693–6. doi: 10.1111/j.1464-410x.1982.tb13626.x. [DOI] [PubMed] [Google Scholar]
- 7.Mundy AR, Stephenson TP. “Clam” ileocystoplasty for the treatment of refractory urge incontinence. Br J Urol. 1985;57:641–6. doi: 10.1111/j.1464-410x.1985.tb07023.x. [DOI] [PubMed] [Google Scholar]
- 8.Khastgir J, Hamid R, Arya M, Shah N, Shah PJ. Surgical and patient reported outcomes of ‘clam’ augmentation ileocystoplasty in spinal cord injured patients. Eur Urol. 2003;43:263–9. doi: 10.1016/s0302-2838(03)00008-3. [DOI] [PubMed] [Google Scholar]
- 9.Zachoval R, Pitha J, Medova E, Heracek J, Lukes M, Zalesky M, et al. Augmentation cystoplasty in patients with multiple sclerosis. Urol Int. 2003;70:21–6. doi: 10.1159/000067708. [DOI] [PubMed] [Google Scholar]
- 10.de Figueiredo AA, Lucon AM, Srougi M. Bladder augmentation for the treatment of chronic tuberculous cystitis. Clinical and urodynamic evaluation of 25 patients after long term follow-up. Neurourol Urodyn. 2006;25:433–40. doi: 10.1002/nau.20264. [DOI] [PubMed] [Google Scholar]
- 11.Shawket TN, Muhsen J. Treatment of bilharzial-contracted bladder by ileocystoplasty or colocystoplasty. J Urol. 1967;97:285–7. doi: 10.1016/S0022-5347(17)63028-3. [DOI] [PubMed] [Google Scholar]
- 12.Elzawahri A, Bissada NK, Herchorn S, Aboul-Enein H, Ghoneim M, Bissada MA, et al. Urinary conduit formation using a retubularized bowel from continent urinary diversion or intestinal augmentations: Ii. Does it have a role in patients with interstitial cystitis? J Urol. 2004;171:1559–62. doi: 10.1097/01.ju.0000116772.74358.39. [DOI] [PubMed] [Google Scholar]
- 13.Nurse DE, Parry JR, Mundy AR. Problems in the surgical treatment of interstitial cystitis. Br J Urol. 1991;68:153–4. doi: 10.1111/j.1464-410x.1991.tb15284.x. [DOI] [PubMed] [Google Scholar]
- 14.van Ophoven A, Oberpenning F, Hertle L. Long-term results of trigone-preserving orthotopic substitution enterocystoplasty for interstitial cystitis. J Urol. 2002;167:603–7. doi: 10.1016/S0022-5347(01)69094-3. [DOI] [PubMed] [Google Scholar]
- 15.Shirley SW, Mirelman S. Experiences with colocystoplasties, cecocystoplasties and ileocystoplasties in urologic surgery: 40 patients. J Urol. 1978;120:165–8. doi: 10.1016/s0022-5347(17)57088-3. [DOI] [PubMed] [Google Scholar]
- 16.Smith RB, van Cangh P, Skinner DG, Kaufman JJ, Goodwin WE. Augmentation enterocystoplasty: A critical review. J Urol. 1977;118:35–9. doi: 10.1016/s0022-5347(17)57878-7. [DOI] [PubMed] [Google Scholar]
- 17.Bhatnagar V, Dave S, Agarwala S, Mitra DK. Augmentation colocystoplasty in bladder exstrophy. Pediatr Surg Int. 2002;18:43–9. doi: 10.1007/s003830200010. [DOI] [PubMed] [Google Scholar]
- 18.Surer I, Ferrer FA, Baker LA, Gearhart JP. Continent urinary diversion and the exstrophy-epispadias complex. J Urol. 2003;169:1102–5. doi: 10.1097/01.ju.0000044921.19074.d0. [DOI] [PubMed] [Google Scholar]
- 19.Youssif M, Badawy H, Saad A, Hanno A, Mokhless I. Augmentation ureterocystoplasty in boys with valve bladder syndrome. J Pediatr Urol. 2007;3:433–7. doi: 10.1016/j.jpurol.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 20.Nguyen DH, Reinberg Y, Gonzalez R, Fryd D, Najarian JS. Outcome of renal transplantation after urinary diversion and enterocystoplasty: A retrospective, controlled study. J Urol. 1990;144:1349–51. doi: 10.1016/s0022-5347(17)39737-9. [DOI] [PubMed] [Google Scholar]
- 21.Rigamonti W, Capizzi A, Zacchello G, Capizzi V, Zanon GF, Montini G, et al. Kidney transplantation into bladder augmentation or urinary diversion: Long-term results. Transplantation. 2005;80:1435–40. doi: 10.1097/01.tp.0000174342.19265.f4. [DOI] [PubMed] [Google Scholar]
- 22.Basiri A, Hosseini Moghaddam S, Khoddam R. Augmentation cystoplasty before and after renal transplantation: Long-term results. Transplant Proc. 2002;34:2106–8. doi: 10.1016/s0041-1345(02)02869-5. [DOI] [PubMed] [Google Scholar]
- 23.Dinckan A, Turkyilmaz S, Tekin A, Erdogru T, Kocak H, Mesci A, et al. Simultaneous augmentation ileo-cystoplasty in renal transplantation. Urology. 2007;70:1211–4. doi: 10.1016/j.urology.2007.09.045. [DOI] [PubMed] [Google Scholar]
- 24.Von Mikulicz J. Zur operation der angebarenen blaben-Spalte. Zentralbl Chir. 1889;20:641–3. [Google Scholar]
- 25.Adams MC, Mitchell ME, Rink RC. Gastrocystoplasty: An alternative solution to the problem of urological reconstruction in the severely compromised patient. J Urol. 1988;140:1152–6. doi: 10.1016/s0022-5347(17)41986-0. [DOI] [PubMed] [Google Scholar]
- 26.Hendren WH, Hendren RB. Bladder augmentation: Experience with 129 children and young adults. J Urol. 1990;144:445–53. doi: 10.1016/s0022-5347(17)39486-7. [DOI] [PubMed] [Google Scholar]
- 27.Whitmore WF, 3rd, Gittes RF. Reconstruction of the urinary tract by cecal and ileocecal cystoplasty: Review of a 15-year experience. J Urol. 1983;129:494–8. doi: 10.1016/s0022-5347(17)52198-9. [DOI] [PubMed] [Google Scholar]
- 28.Swami KS, Feneley RC, Hammonds JC, Abrams P. Detrusor myectomy for detrusor overactivity: A minimum 1-year follow-up. Br J Urol. 1998;81:68–72. doi: 10.1046/j.1464-410x.1998.00474.x. [DOI] [PubMed] [Google Scholar]
- 29.Churchill BM, Aliabadi H, Landau EH, McLorie GA, Steckler RE, McKenna PH, et al. Ureteral bladder augmentation. J Urol. 1993;150:716–20. doi: 10.1016/s0022-5347(17)35596-9. [DOI] [PubMed] [Google Scholar]
- 30.Johal NS, Hamid R, Aslam Z, Carr B, Cuckow PM, Duffy PG. Ureterocystoplasty: Long-term functional results. J Urol. 2008;179:2373–5. doi: 10.1016/j.juro.2008.01.170. [DOI] [PubMed] [Google Scholar]
- 31.Gill IS, Rackley RR, Meraney AM, Marcello PW, Sung GT. Laparoscopic enterocystoplasty. Urology. 2000;55:178–81. doi: 10.1016/s0090-4295(99)00526-9. [DOI] [PubMed] [Google Scholar]
- 32.Kang IS, Lee JW, Seo IY. Robot-assisted laparoscopic augmentation ileocystoplasty: A case report. Int Neurourol J. 2010;14:61–4. doi: 10.5213/inj.2010.14.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Greenwell TJ, Venn SN, Mundy AR. Augmentation cystoplasty. BJU Int. 2001;88:511–25. doi: 10.1046/j.1464-4096.2001.001206. [DOI] [PubMed] [Google Scholar]
- 34.Küss R, Bitker M, Camey M, Chatelain C, Lassau JP. Indications and early and late results of intestino-cystoplasty: A review of 185 cases. J Urol. 1970;103:53–63. doi: 10.1016/s0022-5347(17)61891-3. [DOI] [PubMed] [Google Scholar]
- 35.George VK, Russell GL, Shutt A, Gaches CG, Ashken MH. Clam ileocystoplasty. Br J Urol. 1991;68:487–9. doi: 10.1111/j.1464-410x.1991.tb15391.x. [DOI] [PubMed] [Google Scholar]
- 36.Khoury JM, Timmons SL, Corbel L, Webster GD. Complications of enterocystoplasty. Urology. 1992;40:9–14. doi: 10.1016/0090-4295(92)90428-y. [DOI] [PubMed] [Google Scholar]
- 37.McDougal WS. Metabolic complications of urinary intestinal diversion. J Urol. 1992;147:1199–208. doi: 10.1016/s0022-5347(17)37517-1. [DOI] [PubMed] [Google Scholar]
- 38.Lemann J, Jr, Litzow JR, Lennon EJ. The effects of chronic acid loads in normal man: Further evidence for the participation of bone mineral in the defense against chronic metabolic acidosis. J Clin Invest. 1966;45:1608–14. doi: 10.1172/JCI105467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mundy AR, Nurse DE. Calcium balance, growth and skeletal mineralisation in patients with cystoplasties. Br J Urol. 1992;69:257–9. doi: 10.1111/j.1464-410x.1992.tb15524.x. [DOI] [PubMed] [Google Scholar]
- 40.Wagstaff KE, Woodhouse CR, Rose GA, Duffy PG, Ransley PG. Blood and urine analysis in patients with intestinal bladders. Br J Urol. 1991;68:311–6. doi: 10.1111/j.1464-410x.1991.tb15330.x. [DOI] [PubMed] [Google Scholar]
- 41.Bandi G, Al-Omar O, McLorie GA. Comparison of traditional enterocystoplasty and seromuscular colocystoplasty lined with urothelium. J Pediatr Urol. 2007;3:484–9. doi: 10.1016/j.jpurol.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 42.Kurzrock EA, Baskin LS, Kogan BA. Gastrocystoplasty: Long-term followup. J Urol. 1998;160:2182–6. [PubMed] [Google Scholar]
- 43.Kurzrock EA, Baskin LS, Kogan BA. Gastrocystoplasty: Is there a consensus? World J Urol. 1998;16:242–50. doi: 10.1007/s003450050061. [DOI] [PubMed] [Google Scholar]
- 44.Soylet Y, Emir H, Ilce Z, Yesildag E, Buyukunal SN, Danismend N. Quo vadis? Ureteric reimplantation or ignoring reflux during augmentation cystoplasty. BJU Int. 2004;94:379–80. doi: 10.1111/j.1464-410X.2004.04965.x. [DOI] [PubMed] [Google Scholar]
- 45.Strawbridge LR, Kramer SA, Castillo OA, Barrett DM. Augmentation cystoplasty and the artificial genitourinary sphincter. J Urol. 1989;142:297–301. doi: 10.1016/s0022-5347(17)38737-2. [DOI] [PubMed] [Google Scholar]
- 46.Kreder KJ, Webster GD. Management of the bladder outlet in patients requiring enterocystoplasty. J Urol. 1992;147:38–41. doi: 10.1016/s0022-5347(17)37128-8. [DOI] [PubMed] [Google Scholar]
- 47.Lockhart JL, Bejany D, Politano VA. Augmentation cystoplasty in the management of neurogenic bladder disease and urinary incontinence. J Urol. 1986;135:969–71. doi: 10.1016/s0022-5347(17)45941-6. [DOI] [PubMed] [Google Scholar]
- 48.Gearhart JP, Albertsen PC, Marshall FF, Jeffs RD. Pediatric applications of augmentation cystoplasty: The Johns Hopkins experience. J Urol. 1986;136:430–2. doi: 10.1016/s0022-5347(17)44893-2. [DOI] [PubMed] [Google Scholar]
- 49.Hasan ST, Marshall C, Robson WA, Neal DE. Clinical outcome and quality of life following enterocystoplasty for idiopathic detrusor instability and neurogenic bladder dysfunction. Br J Urol. 1995;76:551–7. doi: 10.1111/j.1464-410x.1995.tb07777.x. [DOI] [PubMed] [Google Scholar]
- 50.Obermayr F, Szavay P, Schaefer J, Fuchs J. Outcome of augmentation cystoplasty and bladder substitution in a pediatric age group. Eur J Pediatr Surg. 2011;21:116–9. doi: 10.1055/s-0030-1267223. [DOI] [PubMed] [Google Scholar]
- 51.Metcalfe PD, Cain MP, Kaefer M, Gilley DA, Meldrum KK, Misseri R, et al. What is the need for additional bladder surgery after bladder augmentation in childhood? J Urol. 2006;176:1801–5. doi: 10.1016/j.juro.2006.03.126. [DOI] [PubMed] [Google Scholar]
- 52.DeFoor W, Minevich E, Reddy P, Sekhon D, Polsky E, Wacksman J, et al. Bladder calculi after augmentation cystoplasty: Risk factors and prevention strategies. J Urol. 2004;172:1964–6. doi: 10.1097/01.ju.0000140911.43898.15. [DOI] [PubMed] [Google Scholar]
- 53.Nurse DE, McInerney PD, Thomas PJ, Mundy AR. Stones in enterocystoplasties. Br J Urol. 1996;77:684–7. doi: 10.1046/j.1464-410x.1996.97311.x. [DOI] [PubMed] [Google Scholar]
- 54.Ngan JH, Lau JL, Lim ST, Chan KW, Tam PC, Li MK. Long-term results of antral gastrocystoplasty. J Urol. 1993;149:731–4. doi: 10.1016/s0022-5347(17)36194-3. [DOI] [PubMed] [Google Scholar]
- 55.Couillard DR, Vapnek JM, Rentzepis MJ, Stone AR. Fatal perforation of augmentation cystoplasty in an adult. Urology. 1993;42:585–8. doi: 10.1016/0090-4295(93)90283-g. [DOI] [PubMed] [Google Scholar]
- 56.Metcalfe PD, Casale AJ, Kaefer MA, Misseri R, Dussinger AM, Meldrum KK, et al. Spontaneous bladder perforations: A report of 500 augmentations in children and analysis of risk. J Urol. 2006;175:1466–70. doi: 10.1016/S0022-5347(05)00672-5. [DOI] [PubMed] [Google Scholar]
- 57.Essig KA, Sheldon CA, Brandt MT, Wacksman J, Silverman DG. Elevated intravesical pressure causes arterial hypoperfusion in canine colocystoplasty: A fluorometric assessment. J Urol. 1991;146:551–3. doi: 10.1016/s0022-5347(17)37851-5. [DOI] [PubMed] [Google Scholar]
- 58.Sheiner JR, Kaplan GW. Spontaneous bladder rupture following enterocystoplasty. J Urol. 1988;140:1157–8. doi: 10.1016/s0022-5347(17)41987-2. [DOI] [PubMed] [Google Scholar]
- 59.North AC, Lakshmanan Y. Malignancy associated with the use of intestinal segments in the urinary tract. Urol Oncol. 2007;25:165–7. doi: 10.1016/j.urolonc.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 60.Soergel TM, Cain MP, Misseri R, Gardner TA, Koch MO, Rink RC. Transitional cell carcinoma of the bladder following augmentation cystoplasty for the neuropathic bladder. J Urol. 2004;172:1649–51. doi: 10.1097/01.ju.0000140194.87974.56. [DOI] [PubMed] [Google Scholar]
- 61.Balachandra B, Swanson PE, Upton MP, Yeh MM. Adenocarcinoma arising in a gastrocystoplasty. J Clin Pathol. 2007;60:85–7. doi: 10.1136/jcp.2005.035196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Esquena Fernández S, Abascal JM, Tremps E, Morote J. Gastric cancer in augmentation gastrocystoplasty. Urol Int. 2005;74:368–70. doi: 10.1159/000084441. [DOI] [PubMed] [Google Scholar]
- 63.Hofmann AF, Poley JR. Role of bile acid malabsorption in pathogenesis of diarrhea and steatorrhea in patients with ileal resection. I. Response to cholestyramine or replacement of dietary long chain triglyceride by medium chain triglyceride. Gastroenterology. 1972;62:918–34. [PubMed] [Google Scholar]
- 64.N’Dow J, Leung HY, Marshall C, Neal DE. Bowel dysfunction after bladder reconstruction. J Urol. 1998;159:1470–4. doi: 10.1097/00005392-199805000-00015. [DOI] [PubMed] [Google Scholar]


