Abstract
Context
Dementia care giving can lead to increased stress, physical and psychosocial morbidity, and mortality. Anecdotal evidence suggests that hospice care provided to people with dementia and their caregivers may buffer caregivers from some of the adverse outcomes associated with family caregiving in Alzheimer's Disease (AD).
Objectives
This pilot study examined psychological and physical outcomes among 32 spousal caregivers of patients with AD. It was hypothesized that caregivers who utilized hospice services would demonstrate better outcomes after the death of their spouse than caregivers who did not utilize hospice.
Methods
The charts of all spousal caregivers enrolled in a larger longitudinal study from 2001 to 2006 (N=120) were reviewed, and participants whose spouse had died were identified. Of these, those who received hospice care (n=10) were compared to those who did not (n=22) for various physiological and psychological measures of stress, both before and after the death of the care recipient. An Analysis of Covariance (ANCOVA), with postdeath scores as the dependent variable and pre-death scores as covariates, was used for all variables.
Results
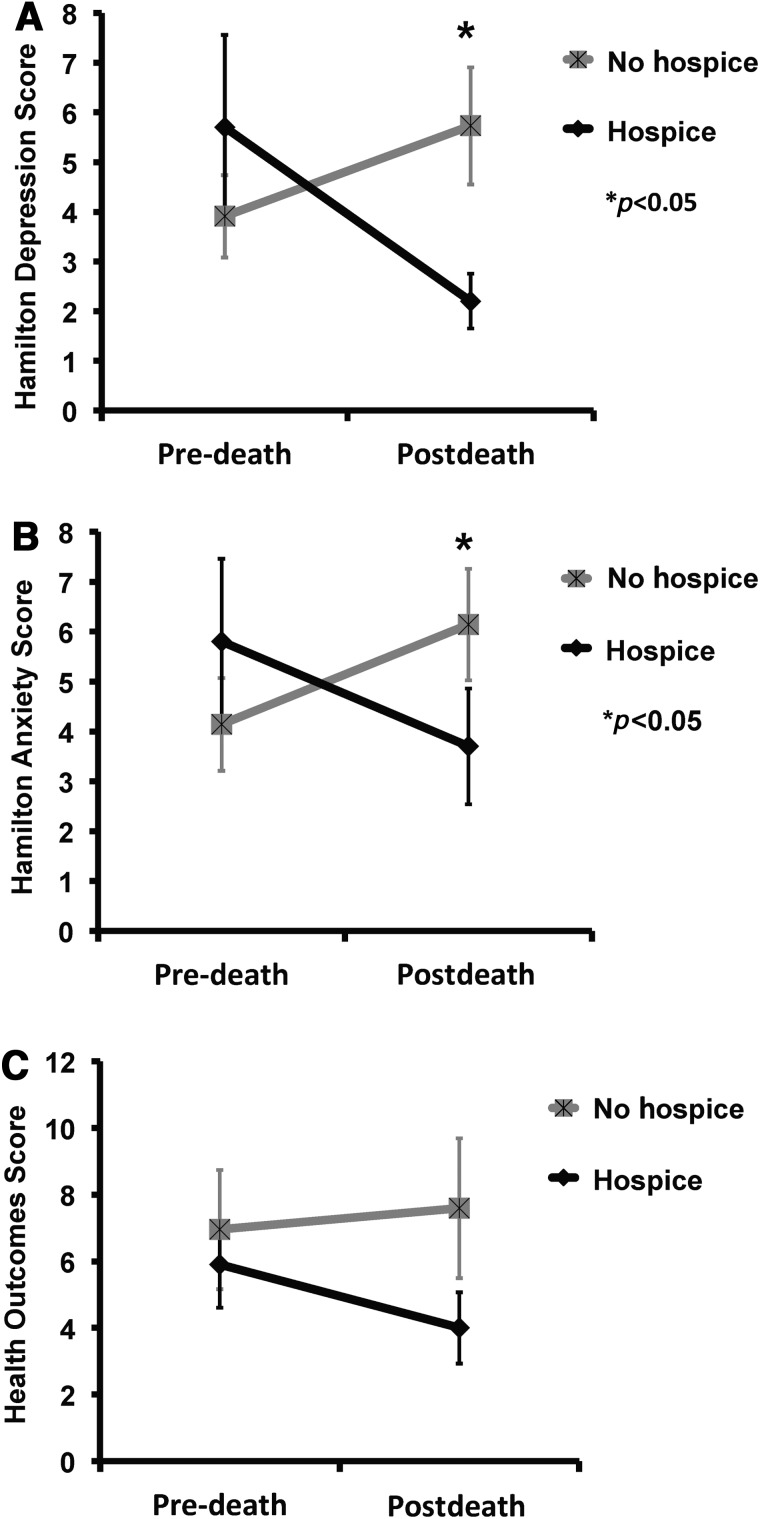
Significant group differences were found in postdeath depressive symptoms (HAM-D; F(1,29)=6.10, p<0.05) and anxiety symptoms (HAM-A; F(1,29)=5.71, p<0.05). Most psychological outcome variables demonstrated moderate effect sizes with a Cohen's d of>0.5 between groups.
Conclusions
These data suggest that hospice enrollment may ameliorate the detrimental psychological effects in caregivers who have lost a spouse with Alzheimer's Disease. Based on these pilot data, further prospective investigation is warranted.
Introduction
Caregivers of patients with Alzheimer's Disease (AD) experience chronic stress, placing them at increased risk for both psychological and physical morbidity. Compared to their noncaregiving counterparts, these caregivers are more likely to experience symptoms of depression,1 anxiety,2 and anger/frustration,3 as well as reduced well-being,4 impaired sleep,5,6 poorer self-rated health,7 increased cardiovascular disease,8–11 and premature death.12 Further, dementia caregivers are more likely to experience emotional or physical problems relative to nondementia caregivers.13 Given the relationship between psychological distress, cardiac health, and the development of cardiovascular disease,14–17 it seems likely that alleviating caregivers' distress might have beneficial impacts on their own long-term physical health, as well as on their ability to provide care. AD caregivers who had placed their spouse in a long-term care facility experienced improvements in psychological distress, physical symptoms, and cardiovascular health, relative to those caregivers continuing in-home care, likely due to reduced exposure to the chronic stress of in-home caregiving.18,19
Hospice care seeks to improve quality of life and reduce suffering at the end of life for seriously ill patients and their caregivers.20,21 Psychological and physical distress related to caring for someone with an advanced, life-threatening illness, such as Alzheimer's dementia, is an important target of hospice care. Currently, 5.4 million U.S. adults suffer from AD, which, in its final stages, is now considered a terminal illness.22,23 Care for people with AD is provided by 14.9 million caregivers, accounting for $183 billion in annual costs.23 Caregiver stress is common and costly, as well as a major source of suffering for patients and families. In this context, effective strategies to reduce the distress associated with family caregiving in AD have the potential to significantly impact quality of life and health outcomes in this large population, while reducing health care costs.
This preliminary pilot investigation examined whether hospice care may ameliorate some of the psychological and physiologic stresses associated with caregiving for a spouse suffering from AD.
Methods
Participants
Subjects were drawn from a larger, longitudinal investigation that prospectively assessed psychological and physical health outcomes for a cohort of 120 elderly spousal caregivers of people with AD, during the five-year study period from 2002 to 2006. Detailed methods for the larger study are provided elsewhere.19 Subjects had participated in this larger study at the University of California, San Diego (UCSD) Alzheimer's Disease Research Center. All participants provided in-home care for their spouse with AD, were at least 55 years of age, and were free of serious medical conditions at the time of enrollment. Participants were excluded if they were caring for a friend, a sibling, a child, or otherwise were not caring for a spouse. Additional exclusion criteria included the use of beta-blocker or anticoagulant medication, or uncontrolled hypertension, as these were potential confounders for biological outcomes assessed in the parent project. The UCSD institutional review board approved the protocol, and all participants provided written informed consent prior to enrollment.
The charts of all caregivers enrolled in the parent study (n=120) were reviewed, and participants whose spouse with AD died during the five-year study period were identified (n=32); these 32 caregivers served as the subjects in the present report. This report compares changes in pre-death to postdeath psychological and physiological outcomes for participants in the parent study who reported hospice enrollment for their spouse (n=10) as compared to those who did not use hospice services (n=22).
Procedures
In the parent longitudinal study, research staff conducted face-to-face assessments of caregivers at 12-month intervals. In addition, regular check-in phone calls were made every six months to inquire about changes in health status and transitions in caregiving (i.e., placement of the AD spouse in long-term care or death of the AD patient). After any reported transition in caregiving, an additional follow-up assessment was scheduled within six months.
Measures
A detailed description of the measures used for demographic and outcomes variables is provided elsewhere.19 Briefly, demographics included age, gender, ethnicity, years of education, and income. Dementia severity (of the person with AD) was assessed using the Clinical Dementia Rating Scale.24 The primary psychological outcomes included symptoms of depression and anxiety, as measured by the 17-item Hamilton Rating Scale for Depression (HAM-D)25,26 and the 14-item Hamilton Rating Scale for Anxiety (HAM-A).27 Modes of caregiver coping were measured using the Avoidance Coping subscale of the Ways of Coping instrument,28 since this coping strategy has been most consistently linked to psychological morbidity and decreased well-being.29 Assessments of physical health included the following: (1) an overall health outcomes score derived from a semistructured interview assessing participants' health outcomes over the prior six months; (2) resting blood pressure and heart rate; and (3) hemodynamic reactivity to stress, as measured by response of blood pressure and heart rate to a simulated stressor.30,31 Finally, caregiver sleep was evaluated using the Global Sleep Quality Score of the Pittsburgh Sleep Quality Index (PSQI).32 All instruments were administered by research staff and based on participants' self-report of symptoms.
Data analyses
Change in the dependent variables from pre-death to postdeath was analyzed using Analyses of Covariance (ANCOVAs), with postdeath scores as the dependent variable and pre-death scores as covariates, controlling for the effect of pre-death differences on outcome measures. This analysis used pre-death and postdeath measures most proximate to the spouse's death (i.e., the set of measures immediately before and immediately after the spouse's death). For heart rate and blood pressure reactivity, residualized change scores (i.e., the posttest score as a deviation from the posttest-on-pretest regression line)32,33 were created and the postdeath score was used as the dependent variable, with pre-death scores as covariates. Hospice involvement was used as the primary predictor in all analyses. Due to the small sample size, effect sizes for group mean differences (Cohen's d) were calculated for all outcome variables in this study. For statistical tests, significance was assumed at the p<0.05 level.
Results
Pre-death demographic data, scores of dementia severity, and baseline blood pressure measurements for all participants are presented in Table 1. Caregivers who utilized hospice were more highly educated (16.1±1.85 years versus 14.18±1.76 years; t(30)=2.81; p<0.01) and showed a trend toward higher incomes. No other significant baseline differences were observed, including depressive symptoms (p=0.314), anxiety symptoms (p=0.356), avoidance coping (p=0.759), health symptoms (p=0.710), SBP (p=0.702), or DBP (p=0.966).
Table 1.
Pre-Death Demographic Characteristics of Caregivers Who Did and Did Not Utilize Hospice Services
| No hospice (n=22) | Hospice (n=10) | t-value, x2 | p-value | |
|---|---|---|---|---|
| Age, mean (SD) | 73.95 (8.85) | 76.80 (8.68) | −0.85 | 0.403 |
| Monthly income, mean (SD) | $3,763.60 ($1,613.08) | $5,761.86 ($3,899.06) | −1.92 | 0.067 |
| Years of education, mean (SD) | 14.18 (1.76) | 16.10 (1.85) | −2.81 | 0.009* |
| Clinical Dementia Rating Scale score, n (%) | ||||
| Mild | 4 (18.2) | 1 (10.0) | 1.05 | 0.592 |
| Moderate | 7 (31.8) | 5 (50.0) | ||
| Severe | 11 (50.0) | 4 (40.0) | ||
| Systolic Blood Pressure | 132.90 (17.58) | 135.13 (15.07) | −0.39 | 0.702 |
| Diastolic Blood Pressure | 65.98 (9.30) | 65.94 (11.37) | 0.043 | 0.966 |
p<0.05
After controlling for differences in pre-death outcomes scores, significant group differences were found in postdeath symptoms of depression and anxiety as measured by the HAM-D and HAM-A, respectively (see Figure 1). Specifically, caregivers who utilized hospice reported lower postdeath symptoms of depression (2.2±0.55 versus 5.73±1.18; F(1,29)=6.10, p<0.05) and anxiety (3.70±1.16 versus 6.14±1.12; F(1,29)=5.71, p<0.05), compared to those who did not use hospice. No group differences were observed with use of avoidance coping, physical health measures (overall health outcomes, or blood pressure or heart rate reactivity), or sleep quality. Table 2 provides depictions of raw depressive symptoms, anxiety symptoms, and health outcomes scores (pre- and postdeath) by group, as well as Cohen's d values.
FIG. 1.
Change from pre- to postdeath by hospice and nonhospice groups±standard error for (A) depression symptoms, (B) anxiety symptoms, and (C) health outcomes. *p<0.05.
Table 2.
Comparisons of Outcome Measures for Caregivers Who Did and Did Not Utilize Hospice Services
| |
No hospice, bereaved (n=22) |
Hospice, bereaved (n=10) |
|
|
|
||
|---|---|---|---|---|---|---|---|
| Pre (SD) | Post (SD) | Pre (SD) | Post (SD) | F (group) | p-values | Cohen's d | |
| Psychological measures | |||||||
| Depressive symptoms (HAM-D) | 3.91 (3.89) | 5.73 (5.53) | 5.70 (5.89) | 2.20 (1.75) | 6.10 | 0.02* | 0.92 |
| Anxiety symptoms (HAM-A) | 4.14 (4.37) | 6.14 (5.25) | 5.80 (5.25) | 3.70 (3.68) | 5.71 | 0.02* | 0.89 |
| Physiological measures | |||||||
| Health Outcomes Score | 6.95 (8.39) | 7.59 (9.84) | 5.90 (4.12) | 4.00 (3.37) | 3.56 | 0.07 | 0.70 |
| Systolic blood pressure reactivity (n=18,9) | 20.70 (18.92) | 20.41 (15.51) | 17.20 (17.37) | 13.81 (14.06) | 0.94 | 0.34 | 0.40 |
| Heart rate reactivity (n=19,9) | 6.14 (5.57) | 7.53 (4.99) | 8.15 (6.85) | 5.41 (3.26) | 2.37 | 0.14 | 0.62 |
| Coping style | |||||||
| Avoidance coping (n=20,8) | 4.90 (3.70) | 4.68 (3.10) | 5.63 (2.62) | 3.00 (2.67) | 2.08 | 0.16 | 0.58 |
| Sleep quality | |||||||
| Sleep (global PSQI) (n=20,8) | 7.75 (4.64) | 6.95 (3.41) | 9.75 (3.20) | 5.75 (2.49) | 2.45 | 0.13 | 0.63 |
p<0.05
PSQI, Pittsburgh Sleep Quality Index.
On average, the postdeath assessment occurred 7.3 months after the death of the spouse (SD=1.3 months). Including this variable as a covariate in the analysis did not significantly predict HAM-D scores (p=0.493). Also, hospice condition remained significant (p=0.022).
Discussion
This pilot investigation was aimed at providing preliminary evidence for the relationship between hospice care and the well-being of family caregivers for patients with AD. The data reported here suggest an association between hospice enrollment and decreased psychological distress in these caregivers, specifically with reductions in symptoms of depression and anxiety. The data failed to show a relationship to several physical health outcomes, coping strategies, or sleep quality.
Caution should be used in interpreting these findings, given the small sample size and nonexperimental design of the study. Only a small number of caregivers experienced the death of their spouse during the study period, and even fewer utilized hospice care. Recruitment from a single geographic region also limits generalizability. Similarly, participants were not randomized to exposure groups, and other methodological strategies to control for baseline differences between the groups were not prospectively incorporated into the study design. For these reasons, alternative explanations for the results cannot be ruled out, such as baseline (pre-death) group differences that might account for hospice utilization and influence change in psychological distress.
Despite these limitations, these data point to potentially fruitful areas of further investigation. Larger, experimental studies are needed to validate and further characterize the relationships suggested by the results of this pilot study. For example, the effects of specific hospice care elements on psychological distress should be explored in order to inform effective strategies for caregiver support in this population. Specifically, does the location of hospice care (in-home versus inpatient, for example) influence the amelioration of psychological stress? Do specific elements of bereavement care (individual counseling versus support groups, for example) affect psychological benefits associated with hospice use? Does the duration of engagement in hospice influence psychological benefits? A larger study with more robust methods would allow an exploration of these important questions. Similarly, this data suggests a trend toward significance in health outcomes scores (p=0.07). Whether or not hospice participation may also confer some physical health benefits to caregivers deserves further study and attention in more robust trials.
Although preliminary in nature, the data from this study suggest a relationship between hospice care and caregiver psychological well-being. The consequences of unrelieved psychological distress are substantial: depressive symptoms, for example, have been shown to contribute to the development of cardiovascular disease in caregivers19 as well as to increased cardiovascular morbidity and mortality in the general population.34 Moreover, increased symptoms of depression and/or anxiety, if not detected or addressed, can increase the perceived severity of pain and other physical symptoms;35–38 affect physical health and quality of life;35,39 impair decision making; impact the relationship with a care recipient, and significantly increase the probability of morbidity, mortality,40 and suicide.41–45 Effective strategies to ameliorate psychological distress, particularly in the setting of caregiving for family members with AD, are likely to have a profound impact on the end-of-life experiences of these patients and their family members. Hospice care may serve as a model to deliver such interventions and thereby support caregivers in this final phase of caring for loved ones with AD.
Acknowledgments
The Palliative Care Psychiatry Program at San Diego Hospice and the Institute for Palliative Medicine was supported, in part, by the National Palliative Care Research Center, Award Number K23MH091176 (Dr. Scott Irwin) from the National Institute of Mental Health, and by donations from the generous benefactors of the education and research programs at San Diego Hospice and The Institute for Palliative Medicine. Other relevant support came from National Institute on Aging grants R01 AG015301 (Dr. Igor Grant), R01 AG031090 (Dr. Brent Mausbach), and R01 AG08415 (Dr. Sonia Ancoli-Israel). The authors gratefully acknowledge the contributions of JSN TANAS. RIP San Diego Hospice. ↑→
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Schulz R. O'Brien AT. Bookwala J. Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: Prevalence, correlates, and causes. Gerontologist. 1995;35:771–791. doi: 10.1093/geront/35.6.771. [DOI] [PubMed] [Google Scholar]
- 2.Dura JR. Stukenberg KW. Kiecolt-Glaser JK. Anxiety and depressive disorders in adult children caring for demented parents. Psychol Aging. 1991;6:467–473. doi: 10.1037//0882-7974.6.3.467. [DOI] [PubMed] [Google Scholar]
- 3.Gallagher D. Wrabetz A. Lovett S. Del Maestro S. Rose J. Depression and other negative affects in family caregivers. In: Light E, editor; Lebowitz BD, editor. Alzheimer's Disease Treatment and Family Stress: Directions for Research. Rockville, MD: U.S. Health & Human Services; 1989. pp. 218–244. [Google Scholar]
- 4.Rose-Rego SK. Strauss ME. Smyth KA. Differences in the perceived well-being of wives and husbands caring for persons with Alzheimer's disease. Gerontologist. 1998;38:224–230. doi: 10.1093/geront/38.2.224. [DOI] [PubMed] [Google Scholar]
- 5.McCurry SM. Logsdon RG. Teri L. Vitiello MV. Sleep disturbances in caregivers of persons with dementia: Contributing factors and treatment implications. Sleep Med Rev. 2007;11:143–153. doi: 10.1016/j.smrv.2006.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCurry SM. Gibbons LE. Logsdon RG. Vitiello MV. Teri L. Insomnia in caregivers of persons with dementia: Who is at risk and what can be done about it? Sleep Med Clin. 2009;4:519–526. doi: 10.1016/j.jsmc.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schulz R. Visintainer P. Williamson GM. Psychiatric and physical morbidity effects of caregiving. J Gerontol. 1990;45:P181–P191. doi: 10.1093/geronj/45.5.p181. [DOI] [PubMed] [Google Scholar]
- 8.Shaw WS. Patterson TL. Ziegler MG. Dimsdale JE. Semple SJ. Grant I. Accelerated risk of hypertensive blood pressure recordings among Alzheimer caregivers. J Psychosom Res. 1999;46:215–227. doi: 10.1016/s0022-3999(98)00084-1. [DOI] [PubMed] [Google Scholar]
- 9.Mausbach BT. Patterson TL. Rabinowitz YG. Grant I. Schulz R. Depression and distress predict time to cardiovascular disease in dementia caregivers. Health Psychol. 2007;26:539–544. doi: 10.1037/0278-6133.26.5.539. [DOI] [PubMed] [Google Scholar]
- 10.Lee S. Colditz GA. Berkman LF. Kawachi I. Caregiving and risk of coronary heart disease in U.S. women: A prospective study. Am J Prev Med. 2003;24:113–119. doi: 10.1016/s0749-3797(02)00582-2. [DOI] [PubMed] [Google Scholar]
- 11.Vitaliano PP. Scanlan JM. Zhang J. Savage MV. Hirsch IB. Siegler IC. A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Psychosom Med. 2002;64:418–435. doi: 10.1097/00006842-200205000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Schulz R. Beach SR. Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. JAMA. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 13.Ory MG. Hoffman RR., III Yee JL. Tennstedt S. Schulz R. Prevalence and impact of caregiving: A detailed comparison between dementia and nondementia caregivers. Gerontologist. 1999;39:177–185. doi: 10.1093/geront/39.2.177. [DOI] [PubMed] [Google Scholar]
- 14.Ford DE. Mead LA. Chang PP. Cooper-Patrick L. Wang NY. Klag MJ. Depression is a risk factor for coronary artery disease in men: The precursors study. Arch Intern Med. 1998;158:1422–1426. doi: 10.1001/archinte.158.13.1422. [DOI] [PubMed] [Google Scholar]
- 15.Musselman DL. Evans DL. Nemeroff CB. The relationship of depression to cardiovascular disease: Epidemiology, biology, and treatment. Arch Gen Psychiatry. 1998;55:580–592. doi: 10.1001/archpsyc.55.7.580. [DOI] [PubMed] [Google Scholar]
- 16.Kop WJ. Chronic and acute psychological risk factors for clinical manifestations of Coronary Artery Disease. Psychosom Med. 1999;61:476–487. doi: 10.1097/00006842-199907000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Bauer KA. Rosenberg RD. The pathophysiology of the prethrombotic state in humans: Insights gained from studies using markers of hemostatic system activation. Blood. 1987;70:343–350. [PubMed] [Google Scholar]
- 18.Grant I. Adler KA. Patterson TL. Dimsdale JE. Ziegler MG. Irwin MR. Health consequences of Alzheimer's caregiving transitions: Effects of placement and bereavement. Psychosom Med. 2002;64:477–486. doi: 10.1097/00006842-200205000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Mausbach BT. Aschbacher K. Patterson TL. von Kanel R. Dimsdale JE. Mills PJ. Ancoli-Israel S. Grant I. Effects of placement and bereavement on psychological well-being and cardiovascular risk in Alzheimer's caregivers: A longitudinal analysis. J Psychosom Res. 2007;62:439–445. doi: 10.1016/j.jpsychores.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 20.National Hospice and Palliative Care Organization. National Hospice and Palliative Care Organization; Alexandria, VA: 2011. NHPCO Facts and Figures: Hospice Care in America. [Google Scholar]
- 21.Ferris FD. Balfour HM. Bowen K. Farley J. Hardwick M. Lamontagne C. Lundy M. Syme A. West P. Ottawa, ON: Canadian Hospice Palliative Care Association; 2002. A Model to Guide Hospice Palliative Care. [PubMed] [Google Scholar]
- 22.Mitchell SL. Teno JM. Kiely DK. Shaffer ML. Jones RN. Prigerson HG. Volicer L. Givens JL. Hamel MB. The clinical course of advanced dementia. N Engl J Med. 2009;361:1529–1538. doi: 10.1056/NEJMoa0902234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alzheimer's Association. Alzheimer's Association; Chicago, IL: 2011. Alzheimer's Disease Facts and Figures. [DOI] [PubMed] [Google Scholar]
- 24.Hughes CP. Berg L. Danziger WL. Coben LA. Martin RL. A new clinical scale for the staging of dementia. Br J Psychiatry. 1982;140:566–572. doi: 10.1192/bjp.140.6.566. [DOI] [PubMed] [Google Scholar]
- 25.Hamilton M. Pichot P. Olivier-Martin R. Psychological Measurements in Psychopharmacology. Basel, Switzerland: S. Karker; 1974. General problems of psychiatric rating scales (especially depression) [Google Scholar]
- 26.Hamilton M. Standardised assessment and recording of depressive symptoms. Psychiatr Neurol Neurochir. 1969;72:201–205. [PubMed] [Google Scholar]
- 27.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 28.Lazarus RS. Folkman S. Stress, Appraisal, Coping. New York: Springer; 1984. [Google Scholar]
- 29.Penley JA. Tomaka J. Wiebe JS. The association of coping to physical and psychological health outcomes: A meta-analytic review. J Behav Med. 2002;25:551–603. doi: 10.1023/a:1020641400589. [DOI] [PubMed] [Google Scholar]
- 30.Saab PG. Llabre MM. Hurwitz BE. Frame CA. Reineke LJ. Fins AI. McCalla J. Cieply LK. Schneiderman N. Myocardial and peripheral vascular responses to behavioral challenges and their stability in black and white Americans. Psychophysiol. 1992;29:384–397. doi: 10.1111/j.1469-8986.1992.tb01712.x. [DOI] [PubMed] [Google Scholar]
- 31.Mills PJ. Dimsdale JE. The effects of acute psychologic stress on cellular adhesion molecules. J Psychosom Res. 1996;41:49–53. doi: 10.1016/0022-3999(96)00051-7. [DOI] [PubMed] [Google Scholar]
- 32.Buysse DJ. Reynolds CF., III Monk TH. Berman SR. Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 33.Cronbach LJ. Furbi L. How should we measure “change”: Or should we? Psychol Bull. 1970;74:68–80. [Google Scholar]
- 34.Nicholson A. Kuper H. Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: A meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J. 2006;27:2763–2774. doi: 10.1093/eurheartj/ehl338. [DOI] [PubMed] [Google Scholar]
- 35.Spiegel D. Bloom JR. Group therapy and hypnosis reduce metastatic breast carcinoma pain. Psychosom Med. 1983;45:333–339. doi: 10.1097/00006842-198308000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Cassem EH. Depressive disorders in the medically ill: An overview. Psychosomatics. 1995;36:S2–S10. doi: 10.1016/S0033-3182(95)71698-X. [DOI] [PubMed] [Google Scholar]
- 37.Ciaramella A. Poli P. Assessment of depression among cancer patients: The role of pain, cancer type and treatment. Psychooncology. 2001;10:156–165. doi: 10.1002/pon.505. [DOI] [PubMed] [Google Scholar]
- 38.Spiegel D. Sands S. Koopman C. Pain and depression in patients with cancer. Cancer. 1994;74:2570–2578. doi: 10.1002/1097-0142(19941101)74:9<2570::aid-cncr2820740927>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 39.Wilson KG. Chochinov HM. de Faye BJ. Breitbart W. Diagnosis and management of depression in palliative care. In: Chochinov HM, editor; Breitbart W, editor. Handbook of Psychiatry in Palliative Medicine. New York: Oxford University Press; 2000. pp. 25–50. [Google Scholar]
- 40.McDaniel JS. Brown FW. Cole SA. Assessment of depression and grief reactions in the medically ill. In: Stoudemire A, editor; Fogel BS, editor; Greenberg DB, editor. Psychiatric Care of the Medical Patient. New York: Oxford University Press; 2000. pp. 149–164. [Google Scholar]
- 41.Breitbart W. Rosenfeld B. Pessin H. Kaim M. Funesti-Esch J. Galietta M. Nelson CJ. Brescia R. Depression, hopelessness, and desire for hastened death in terminally ill patients with cancer. JAMA. 2000;284:2907–2911. doi: 10.1001/jama.284.22.2907. [DOI] [PubMed] [Google Scholar]
- 42.Conwell Y. Duberstein PR. Caine ED. Risk factors for suicide in later life. Biol Psychiatry. 2002;52:193–204. doi: 10.1016/s0006-3223(02)01347-1. [DOI] [PubMed] [Google Scholar]
- 43.Alexopoulos GS. Bruce ML. Hull J. Sirey JA. Kakuma T. Clinical determinants of suicidal ideation and behavior in geriatric depression. Arch Gen Psychiatry. 1999;56:1048–1053. doi: 10.1001/archpsyc.56.11.1048. [DOI] [PubMed] [Google Scholar]
- 44.Waern M. Rubenowitz E. Wilhelmson K. Predictors of suicide in the old elderly. Gerontology. 2003;49:328–334. doi: 10.1159/000071715. [DOI] [PubMed] [Google Scholar]
- 45.American Psychiatric Association's Work Group on Suicidal Behaviors: Practice guideline for the assessment and treatment of patients with suicidal behaviors. Am J Psychiatry. 2003;160:1–60. [PubMed] [Google Scholar]