Abstract
Purpose:
To examine the frequency and significance of visualization of popliteal nodes during lymphoscintigraphy for the investigation of lower extremity swelling.
Materials and Methods:
Technetium-99m-labeled nanocolloid was injected subcutaneously in the first web spaces of both feet of 90 patients (24 males, 66 females; age range, 4-70 years) who had clinical evidence of lower limb lymphedema and were referred for routine lymphoscintigraphy; imaging was performed 5, and 90 minutes after injection without any vigorous exercise between the injection and imaging.
Results:
According to the scan findings, patients were divided into two groups; group I included 63 patients without popliteal nodes visualization on scanning, and group II included 27 patients with positive popliteal nodes uptake. None of patients with primary lymphedema (N = 22) due to agenesis or hypoplasia showed popliteal node uptake, whereas, patients with secondary lymphedema (N = 68) had either severe (N = 23) or partial (N = 45) lymphatic obstruction. A high positive association of popliteal node uptake with the severity of lymphatic obstruction was noted. Popliteal nodes were visualized in 26 of 57 patients with dermal back flow (46%), and in only 1 of 33 patients without dermal back flow (3%). There was a strong association between skin rerouting and popliteal node visualization (P < 0.01). Skin changes were detected in 24 patients (38%) with positive popliteal node uptake.
Conclusion:
Popliteal lymph nodes uptake during lymphoscintigraphy for clinical lymphedema of the lower limb indicates lymph rerouting through the deep system and raises a diagnosis of higher severity and longer duration of lymphatic dysfunction.
Keywords: Lower limb edema, lymphoscintigraphy, popliteal lymph node
INTRODUCTION
Lymphedema is a chronic debilitating progressive disease that is frequently misdiagnosed and results from impaired lymphatic transport caused by injury to the lymphatics, infection or congenital abnormality. Lymphedema is characterized by four pathologic features: Excess tissue protein, edema, chronic inflammation and fibrosis.[1] Lymphedema is often multifactorial, it can be primary (e.g., lymphatic aplasia, hypoplasia, lymphangiectasia) but is more commonly secondary (e.g., infectious, inflammatory, traumatic, malignant, iatrogenic and irradiation induced).[2] Lymphoscintigraphy of the lower limbs is routinely performed for the investigation of a swollen limb.
Lymphoscintigraphy not only confirms lymphatic failure when abnormal, but also can provide useful information about the pathophysiology and mechanism of lymphatic failure. For example, in genetic forms of lymphedema, like milroy disease, there is a failure of initial lymphatic uptake as a result of mutations in the gene for vascular endothelial growth factor receptor 3.[3] In lymphedema distichiasis syndrome, which is caused by mutations in forkhead box protein C2 gene, the mechanism is lymph reflux due to lymphatic valve failure and the lymphoscintigraphic images are characteristic.[4]
Lymphoscintigraphy for sentinel lymph node (SLN) identification in patients with lower limb extremity melanoma has shown that popliteal nodes may take up tracer, indicating subfascial (deep) lymphatic vessel transport.[5,6]
Popliteal node visualization during lymphoscintigraphy for the investigation of a swollen lower limb after injection of the radiotracer into a web space, therefore, has come to be regarded as a normal variant.[7] However, tracer administered around the lateral foot and ankle, as given for SLN identification, may drain via the deep route, but tracer administered into the web spaces, under normal circumstances, follows an epifascial route.[5]
The aim of this study was to determine the frequency and significance of popliteal node uptake after web space injection during lymphoscintigraphy for lower limb edema.
MATERIALS AND METHODS
Patients
This study was a retrospective analysis of 90 patients (24 males, 66 females; age range, 4-70 years, mean of age = 43.4 ± 15.2 years) who had clinical evidence of lower limb lymphedema and were referred to Nuclear Medicine Unit in our institution for routine lower limb lymphoscintigraphy from the period between July 2010 and December 2012. Data collection and reviewing of images were approved by the local Institutional Ethical Committee.
Lymphoscintigraphy
An average dose of 0.5 mCi (~20 MBq) of technetium-99m-labeled nanocolloid (Nanocoll, GE Health-care) in a volume of 0.2 mL was injected using 25-gauge needle into the subcutaneous tissue of the dorsum of the first web space of the right and left foot. During injection, avoidance of intradermal introduction of the radiotracer was experienced by pinching up the skin at the injection site with careful aspiration to avoid intravascular injection as well. Anterior and posterior half-body images from the lower abdomen to the toes were obtained with a dual head gamma camera equipped with an all-purpose, low energy, parallel hole collimator covering a NaI (Tl) crystal 3/8-inch thickness, set at 140 KeV with 20% window, zoom 1.0 with 256 × 256 matrix size. Imaging began immediately after tracer injection (early image) and 90 min later (delayed image). Patients were instructed to take a short walk between the early and delayed scans without vigorous exercise.
Qualitative image interpretation included evaluation of the injection site, lymphatic vessels, collateral vessels, dermal backflow and lymph nodes (number, size and intensity of radiotracer uptake). A popliteal node was considered present when lymphoscintigraphy showed at least one discrete focus of activity at the level of the knee between the injection site and the ipsilateral draining ilioinguinal lymph nodes. Patients were divided into two groups according to the presence or absence of popliteal lymph node (PLN) uptake on scan.
Statistical methods
Data were statistically described in terms of mean and standard deviation, median and range or frequencies (number of cases) and percentages when appropriate. Comparison of numerical variables between the study groups was performed using Student's t-test for independent samples. Within group comparison of numerical variables was performed using paired t-test. P < 0.05 was considered to be statistically significant. All statistical calculations were performed using computer programs SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA) version 15 for Microsoft Windows.
RESULTS
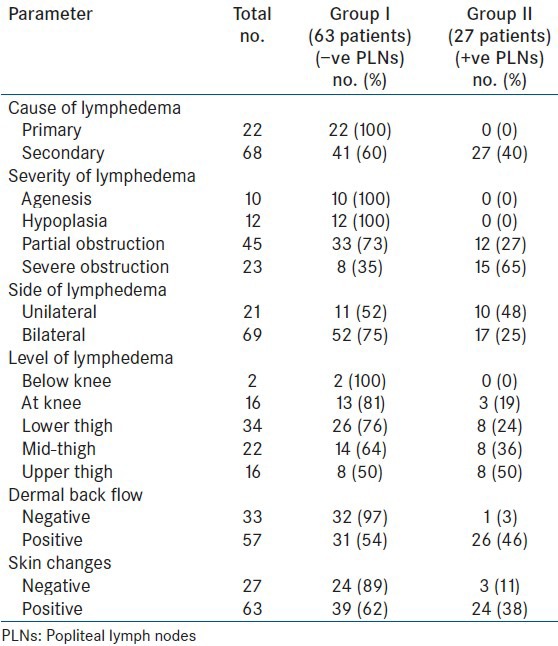
Table 1 demonstrates the details of the results and the distribution of the studied parameters within the two groups.
Table 1.
Distribution of some clinical findings and lymphoscintigraphic pattern in the patients group in relation to popliteal lymph node uptake
Patients group had clinically apparent unilateral or bilateral lower limb lymphedema due to either primary or secondary causes with clinical evidence of different levels of edema (below knee, at knee, lower thigh, mid-thigh or upper thigh) and variable severities (agenesis, hypoplasia, partial obstruction or severe obstruction).
According to the scan findings, patients were divided into two groups; Group I included 63 patients (70%) had no scintigraphic evidence of PLN visualization on scanning, their mean of age was 40.3 ± 16.8 years and Group II included 27 patients (30%) with positive PLN uptake; their mean of age was 50.6 ± 6.1 years. There was a significant statistical difference in the age between the two groups (P < 0.01).
Patients in Group II had a significant higher duration of lower limb swelling (13.4 ± 5.1 years) compared with that of patients in Group I (10.8 ± 6.5 years) (P < 0.05).
It was noted that none of patients with primary lymphedema (N = 22) due to either agenesis or hypoplasia showed popliteal node uptake. Whereas, patients with secondary lymphedema (N = 68) had either severe (N = 23) or partial lymphatic obstruction (N = 45). Positive popliteal node uptake was seen in 15/23 representing 65% of patients with severe lymphatic obstruction and in 12/45 (27%) of patients with partial lymphatic obstruction (P < 0.01 between both groups). This indicates a high positive association of popliteal node uptake with the severity of lymphatic obstruction.
The frequency of popliteal node uptake was higher among patients when the level of edema was above the knee (in 24/27 patients, 88.8%).
Dermal backflow is attributed to rerouting of lymph through the skin, was diagnosed on lymphoscintigraphy when the tracer was obviously seen in the small lymphatic vessels of the skin. Popliteal nodes were visualized in 26/57 patients (46%) with dermal back flow. In contrast, popliteal nodes were not detected in 32/33 patients (97%) without dermal back flow. There was a very strong association between skin rerouting and popliteal node visualization (P < 0.01).
Positive popliteal node uptake were detected in 24/63 patients (38%) with lymphedema associated with skin changes such as non-pitting edema, dermatosclerosis, hyperkeratosis or increased skin turgor compared with only 3/27 patients (11%) without skin changes (P < 0.01).
Figures 1 and 2 represent two patients in Group II with secondary lymphedema and positive popliteal nodes uptake.
Figure 1.
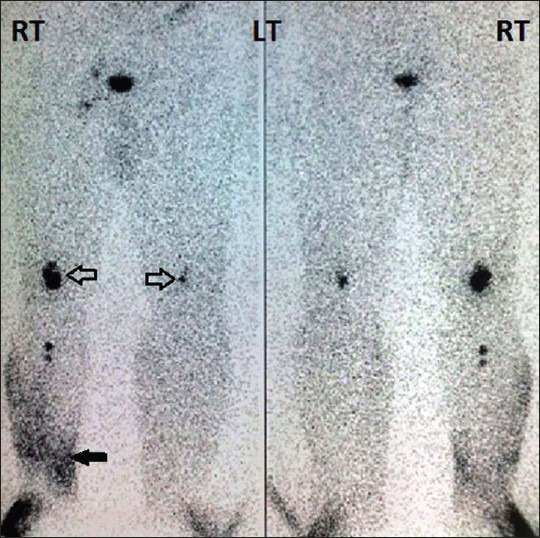
Lymphoscintigraphic findings of bilateral severe lymphatic obstruction in 47-year-old woman clinically diagnosed as bilateral lymphedema. Multiple popliteal nodes (open arrows) on the right side and single node on the left side are seen. Ilioinguinal nodal activity is less in number and activity on right and not seen on left with non-visualization of the deep lymphatic trunks on both sides. Dermal backflow of ankle and leg until below knee is seen on right (solid arrow)
Figure 2.

Lymphoscintigraphic findings of bilateral partial lymphatic obstruction in 50-year-old man clinically diagnosed as bilateral lymphedema. Image shows multiple popliteal nodes (open arrows) on both sides. Ilioinguinal nodes activity is adequately seen (black arrows). Dermal backflow until below knee on the left side and until above ankle on the right side is noted (solid arrows)
DISCUSSION
Many of patients with lymphedema in the lower limbs suffer from severe lifelong disability if they are not properly diagnosed and treated. Early diagnosis can lead to effective treatment and prevention of secondary effects, including extremity deformity, disuse atrophy and increased susceptibility to recurrent infections.[8]
Lymphoscintigraphy offers objective evidence to distinguish lymphatic pathology from non-lymphatic causes of extremity edema.[9,10] Criteria for lymphatic dysfunction include delay, asymmetric or absent visualization of regional lymph nodes and the presence of “dermal backflow.” Additional findings include asymmetric visualization of lymphatic channels, collateral lymphatic channels and interrupted vascular structures.[11]
Popliteal nodes are in lymphatic chains that accompany the deep veins and are consequently consistently seen after subfascial injection, such as into the gastrocnemius muscle. In the study by Hatta et al., all five patients in whom popliteal nodes were visualized received the primary injection into the heel and the lateral foot or malleolus, suggesting a lymph route that from those sites is diverted into the deep system. This finding is consistent with contrast-enhanced lymphography, which showed that injection into these sites accesses the deep system.[12] Subcutaneous and intradermal injections into the web spaces, in contrast, deliver tracer to the epifascial lymphatic system, which normally remains separate from and does not mix with the deep system.[13]
In the current study, we aimed to explain the significance of popliteal nodes uptake during lymphoscintigraphy for lower limb lymphedema. Our data analysis was based on a patient-by-patient basis rather than limb by limb because of the likelihood of the lymphatic dysfunction, when present, is bilateral.[14]
Popliteal nodes uptake were detected in 27/90 patients representing 30% of the studied patients, all had clinical and scintigraphic evidence of secondary lymphedematous changes suggesting the presence of an aberrant lymph drainage route to deep popliteal nodes from a superficial injection. This finding was also confirmed in the study of Burnand et al., who found a popliteal nodes uptake in 59/136 patients (43.4%) with clinical evidence of lymphedema and abnormal scintigraphy findings.[15]
Exercise after radiotracer injection results in rerouting of lymph through the deep system possibly as a result of increased blood flow, capillary filtration and lymph production and masks a potentially useful clue of lymphatic dysfunction.[7] To avoid misinterpretation of positive popliteal uptake, our subjects were told not to undertake any strenuous exercise after radiotracer injection until completion of the imaging.
Popliteal nodes were seen significantly more frequently in patients with secondary compared with primary lymphedema on scintigraphy; there was also a strong and positive association between popliteal node visualization and lymph rerouting through the skin (dermal backflow), severity of lymphedema, presence of associated skin changes as well as duration of the disease.
From the current results, the final message we can give to nuclear medicine physicians is that whenever you see PLNs, you have to be cautious and meticulous in interpretation, possibly there is secondary lymphedema or at least something abnormal probably mild interstitial lymphostasis that possibly can occur due to presence of lymphangitis and true lymphatic obstruction may take place over time.
CONCLUSION
PLNs uptake during lymphoscintigraphy for lower limb lymphedema indicates lymph rerouting through the deep system and raises a diagnosis of higher severity and longer duration of lymphatic dysfunction.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Mortimer PS, Levick JR. Chronic peripheral oedema: The critical role of the lymphatic system. Clin Med. 2004;4:448–53. doi: 10.7861/clinmedicine.4-5-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clarke D, Martinez A, Cox RS, Goffinet DR. Breast edema following staging axillary node dissection in patients with breast carcinoma treated by radical radiotherapy. Cancer. 1982;49:2295–9. doi: 10.1002/1097-0142(19820601)49:11<2295::aid-cncr2820491116>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 3.Mellor RH, Hubert CE, Stanton AW, Tate N, Akhras V, Smith A, et al. Lymphatic dysfunction, not aplasia, underlies Milroy disease. Microcirculation. 2010;17:281–96. doi: 10.1111/j.1549-8719.2010.00030.x. [DOI] [PubMed] [Google Scholar]
- 4.Mellor RH, Tate N, Stanton AW, Hubert C, Mäkinen T, Smith A, et al. Mutations in FOXC2 in humans (lymphoedema distichiasis syndrome) cause lymphatic dysfunction on dependency. J Vasc Res. 2011;48:397–407. doi: 10.1159/000323484. [DOI] [PubMed] [Google Scholar]
- 5.Sumner WE, 3rd, Ross MI, Mansfield PF, Lee JE, Prieto VG, Schacherer CW, et al. Implications of lymphatic drainage to unusual sentinel lymph node sites in patients with primary cutaneous melanoma. Cancer. 2002;95:354–60. doi: 10.1002/cncr.10664. [DOI] [PubMed] [Google Scholar]
- 6.McMasters KM, Chao C, Wong SL, Wrightson WR, Ross MI, Reintgen DS, et al. Interval sentinel lymph nodes in melanoma. Arch Surg. 2002;137:543–7. doi: 10.1001/archsurg.137.5.543. [DOI] [PubMed] [Google Scholar]
- 7.Weissleder H, Weissleder R. Lymphedema: Evaluation of qualitative and quantitative lymphoscintigraphy in 238 patients. Radiology. 1988;167:729–35. doi: 10.1148/radiology.167.3.3363131. [DOI] [PubMed] [Google Scholar]
- 8.Szuba A, Shin WS, Strauss HW, Rockson S. The third circulation: Radionuclide lymphoscintigraphy in the evaluation of lymphedema. J Nucl Med. 2003;44:43–57. [PubMed] [Google Scholar]
- 9.Cambria RA, Gloviczki P, Naessens JM, Wahner HW. Noninvasive evaluation of the lymphatic system with lymphoscintigraphy: A prospective, semiquantitative analysis in 386 extremities. J Vasc Surg. 1993;18:773–82. doi: 10.1067/mva.1993.50510. [DOI] [PubMed] [Google Scholar]
- 10.Pecking AP. Possibilities and restriction of isotopic lymphography for the assessment of therapeutic effects in lymphedema. Wien Med Wochenschr. 1999;149:105–6. [PubMed] [Google Scholar]
- 11.Witte CL, Witte MH, Unger EC, Williams WH, Bernas MJ, McNeill GC, et al. Advances in imaging of lymph flow disorders. Radiographics. 2000;20:1697–719. doi: 10.1148/radiographics.20.6.g00nv141697. [DOI] [PubMed] [Google Scholar]
- 12.Hatta N, Morita R, Yamada M, Takehara K, Ichiyanagi K, Yokoyama K. Implications of popliteal lymph node detected by sentinel lymph node biopsy. Dermatol Surg. 2005;31:327–30. doi: 10.1111/j.1524-4725.2005.31083. [DOI] [PubMed] [Google Scholar]
- 13.Browse NL, Burnand K, Mortimer PS. The normal lymphographic appearances of the lower limb and pelvis. In: Kinmonth JB, editor. The Lymphatics. London, UK: Edward Arnold; 1982. pp. 19–35. [Google Scholar]
- 14.Burnand KM, Glass DM, Mortimer PS, Peters AM. Lymphatic dysfunction in the apparently clinically normal contralateral limbs of patients with unilateral lower limb swelling. Clin Nucl Med. 2012;37:9–13. doi: 10.1097/RLU.0b013e31823931f5. [DOI] [PubMed] [Google Scholar]
- 15.Burnand KM, Glass DM, Sundaraiya S, Mortimer PS, Peters AM. Popliteal node visualization during standard pedal lymphoscintigraphy for a swollen limb indicates impaired lymph drainage. AJR Am J Roentgenol. 2011;197:1443–8. doi: 10.2214/AJR.11.6631. [DOI] [PubMed] [Google Scholar]


