Abstract
Background General practitioners often encounter patients with medically unexplained symptoms. These patients share many common features, but there is little agreement about the best diagnostic framework for describing them.
Aims This study aimed to explore how GPs make sense of medically unexplained symptoms.
Design Semi-structured interviews were conducted with 24 GPs. Each participant was asked to describe a patient with medically unexplained symptoms and discuss their assessment and management.
Setting The study was conducted among GPs from teaching practices across Australia.
Methods Participants were selected by purposive sampling and all interviews were transcribed. Iterative analysis was undertaken using constructivist grounded theory methodology.
Results GPs used a variety of frameworks to understand and manage patients with medically unexplained symptoms. They used different frameworks to reason, to help patients make sense of their suffering, and to communicate with other health professionals. GPs tried to avoid using stigmatising labels such as ‘borderline personality disorder’, which were seen to apply a ‘layer of dismissal’ to patients. They worried about missing serious physical disease, but managed the risk by deliberately attending to physical cues during some consultations, and focusing on coping with medically unexplained symptoms in others. They also used referrals to exclude serious disease, but were wary of triggering a harmful cycle of uncoordinated care.
Conclusion GPs were aware of the ethical relevance of psychiatric diagnoses, and attempted to protect their patients from stigma. They crafted helpful explanatory narratives for patients that shaped their experience of suffering. Disease surveillance remained an important role for GPs who were managing medically unexplained symptoms.
Keywords: diagnosis, general practice, mental health, somatoform disorders, uncertainty
Background
Patients with medically unexplained symptoms (MUS) have traditionally been described using psychiatric terms (somatoform disorder, somatisation), terms that refer to unexplained symptoms within a particular body system (functional disorders), or terms that suggest difficult interpersonal relationships between doctor and patient (‘heartsink patients’).
There has been extensive debate about the best way to conceptualise and assess patients with medically unexplained symptoms, particularly in general practice.
This study explores the way that GPs make sense of patients with medically unexplained symptoms, including the way that they use diagnostic frame-works to assess and manage patients in the absence of an organic diagnosis.
GPs use diagnoses to assist them in conceptualising their patient's distress, to shape the patient's understanding of their own illness, and to manage the stigma that is attached to certain psychiatric labels.
Introduction
Patients with medically unexplained symptoms are commonly managed in general practice, and the prevalence of MUS is estimated to be over 25%.1–5 Some patients have multiple symptoms and experience debilitating illness.2,6,7 Many have comorbid medical and psychiatric disorders,8–11 or abuse substances. Most are women,12 and a history of childhood trauma is common.13–15 These patients are complex and challenging to manage and are often described as ‘heartsink’16,17 or ‘difficult.’
Because these patients have a number of similar features, researchers and clinicians have tried to develop a diagnostic term to describe their symptoms. The term ‘somatoform disorders’ is used within DSM-IV18 and ICD-10,19 and ‘somatic symptom disorder’ is used in DSM-V.20 However, there are other categorical diagnoses in use, including functional disorders in the medical specialties. Other terms, including ‘heartsink patient’, describe the interpersonal challenges of managing the therapeutic relationship. However, to date there is only a limited understanding of how GPs make sense of these presentations.
Whereas biomedical disorders usually have underlying ‘first principles’, based on physiology and biochemistry, psychiatry is dependent on pattern recognition.21 In somatoform disorders, the GP is required to utilise both approaches simultaneously, excluding physical illness using first principles while undertaking pattern recognition to identify a psychiatric disorder. Because 6–10% of patients in general practice have a rare disease,22 it is understandable that GPs are concerned about the possibility of missing a serious biomedical diagnosis. Many writers describe the difficulty of excluding important physical illnesses without over-investigating and causing iatrogenic harm.23
There is also significant cross-cultural variation in the way that mental health problems are experienced and communicated.24 Communication styles and preferences vary across cultures, and this may influence the way that illness is understood by patients and clinicians.25 Shame and stigma can also prevent patients from raising mental health issues.26 The ability of clinicians to adapt their relational style to meet an individual patient's needs can therefore influence diagnosis as well as therapy.25,26
Diagnosis should give a simple characterisation of a phenomenon, so that it is possible to study it, predict behaviour and judge the efficacy of treatment.27,28 However, the single view of mental disorder provided by a categorical diagnosis has limitations. Sadler has described the importance of multiple frameworks by using the analogy of a botanist and a gardener.27 For the botanist, classification produces a taxonomy that is rigorous and reliable. For the gardener, classification informs the way that a garden is developed and nurtured in a specific context.29 Given the limitations of categorical diagnosis, clinicians need to develop other frameworks in order to understand medically unexplained symptoms holistically.
Ethnographic theory,30 grounded theory31 and phenomenological methodologies32 have been used to study medically unexplained symptoms, and have provided different ways of conceptualising illness. Such qualitative research allows evidence to emerge from complex and layered data, building a different understanding of diagnosis. However, these approaches are only beginning to build evidence for alternative diagnostic frameworks in general practice.
Psychiatric disorders also have consequences for patients, and can affect their social power and agency.33 The difficulty with somatoform disorders is that doctors can recast physical symptoms as a psychiatric disorder.
Despite these challenges, GPs somehow learn to traverse this difficult terrain and provide help for their patients.34 The purpose of this study is to examine how novice and experienced GPs make sense of medically unexplained symptoms.
Methods
This study utilised constructivist grounded theory methodology35 using semi-structured interviews as the research method. Grounded theory builds a theoretical model ‘from the ground up.’ Researchers code interviews line by line in the initial interviews, gradually clustering these codes into categories. Importantly, data collection and analysis occur concurrently, with the interviewer returning to the field to test and develop emerging categories and the relationship between them. The researcher continues interviewing until no further concepts emerge, and the analysis yields an emerging theory. At this point, the researcher is said to have reached ‘theoretical saturation.’
In this study, interviews were conducted with novice and expert general practitioners in Australia from 2009 to 2010.
Sampling
Participants were selected using purposive sampling techniques. Registrars were recruited through regional Directors of Training, who circulated a promotional flyer at an educational event in their region. Participants were informed of the aims and methods of the study, asked to give written consent, and offered a $100 book voucher to thank them for their time and expertise. As the study progressed, the Directors of Training were asked to identify and invite registrars with particular interests, educational experience, clinical contexts and personal attributes to participate in the study.
Supervisors were selected as the expert group primarily because they are recognised within the profession for both their expertise and their specific competencies in teaching. Because supervisors are often asked to articulate their clinical reasoning and clinical processes, clearly they were an ideal expert sample for this study. Supervisors were approached directly on the basis of their specific contexts, recognised expertise, clinical and educational interests and personal attributes.
In total, 8 registrars and 16 supervisors were interviewed. The characteristics of the sample are listed in Table 1.
Table 1.
Characteristics of the sample
| Characteristic | Number of participants |
|---|---|
| Role | |
| Registrar | 8 |
| Supervisor | 16 |
| Gender | |
| Female | 11 |
| Male | 13 |
| Age (years) | |
| 20–30 | 4 |
| 30–40 | 4 |
| 40–50 | 8 |
| 50–60 | 6 |
| 60 | 2 |
| Setting | |
| Urban | 12 |
| Rural | 8 |
| Remote | 3 |
| Aboriginal Medical Service | 3 |
| Correctional facilities | 1 |
| State of Australia | |
| New South Wales | 13 |
| Victoria | 3 |
| Northern Territory | 3 |
| Australian Capital Territory | 1 |
| Tasmania | 1 |
| Queensland | 3 |
| Identified interest in mental health | |
| Yes. Sets aside specific consultations for counselling | 3 |
| Yes. Incorporates counselling into their normal GP consultations | 9 |
| No. Identifies other interests (e.g. sports medicine, procedural practice) | 12 |
Interviews
Interviews were conducted face to face or by telephone and lasted for 45 to 75 minutes. Participants were asked to describe a case in which a patient had mixed emotional and physical symptoms and no diagnosis, and were then asked to describe how they made sense of the situation. Participants and their patients were de-identified when the interviews were transcribed for analysis. Each participant was identified by a pseudonym, followed by the letter R (for registrar) or S (for supervisor). Any identifying information, such as patient names, clinical locations or town names, was replaced with appropriate pseudonyms.
Analysis
The data were analysed iteratively using open inductive coding through line-by-line reading of the interview transcripts. NVivo software was utilised to code the data and develop theoretical models around the process of clinical assessment. Field notes were also utilised, using Charmaz's technique of memoing at the conclusion of each interview, and these reflections were incorporated as data. As theoretical models emerged, these were tested and refined within the subsequent interviews, and interviews continued until theoretical saturation was reached.
Ethical approval
Ethical approval was granted by the Sydney University Human Research Ethics Committee (HREC 12269).
Results
The participants identified four core strategies for crafting useful diagnostic frameworks for patients with medically unexplained symptoms.
Strategy 1: validating suffering without ‘medicalising misery’
All of the patients had physical symptoms, so there was a clear requirement for the GPs to exclude disease in the initial phases of diagnosis. However, the extent to which the GP ‘chased down’ a possible organic diagnosis was an area of debate:
That dizziness that I've been telling you about … he was a bit tachycardic … [so I] sent him off to hospital … he'd had a fractured rib which had ruptured his spleen. You have to stay in that anxious frame of going: maybe the fact that he's dizzy is that he's ruptured his spleen. [laugh] I mean that's pretty dramatic.
(Ellen R)
Most of the participants felt responsible for supporting patients who suffer significant distress and functional disability in the absence of disease:
We are the only ones who may have some hope of actually seeing that there is a physical component that we actually have to manage and at the same time being accessible, inquiring, encouraging and supportive of the psychological walk, whether or not that's with another health professional, this is the only place where the body and mind actually become one. And if that's not our job then I don't know whose job it is.
(Ian S)
However, there was some ambivalence about where that role begins and ends. In the words of one registrar:
Sometimes you don't learn that craft from your supervisors … how much they take on and where they draw the line and where they put their boundaries, and why they will see this patient at six o'clock on a Friday, but they won't see that patient at six o'clock on a Friday.
(Anna R)
All of the patients who were discussed had an initial physical symptom, and this placed the patient clearly within the role description of a primary care doctor. However, there was considerable discussion about reorienting help seeking so that a physical ‘ticket of entry’ was not required in order to access care. One doctor described an adolescent presenting with her mother, and the use of the GP as a mediator to facilitate discussions about the family dynamics. Another described a situation with a patient who had been treated by multiple services and had become alienated from the medical system. The GP from her current medical clinic described how the patient needed to escalate her symptoms in order to be ‘taken seriously’:
I think what happened when she came down to us was that she was taken seriously. She wasn't then berated when her symptoms didn't match the biological aetiology, and because we were still willing to help, she felt accepted, and it was a chance for her then to say, when I talk to you the headaches do get better. You know, I don't need [opiates], I think I could actually manage this on some ibuprofen.
(Charlotte R)
Registrars were particularly concerned about the risk of missing an important physical diagnosis:
You know, if it's anxiety … we can deal with it … but if it's a physical thing and I was to say it's anxiety and not rule out the physical thing, then that wouldn't be good. That's my sort of thinking.
(Daniel R)
Registrars also mentioned the shift from hospital to community care, and how this required them to manage patients whom they had previously discharged from tertiary care. One registrar reflected on her Accident and Emergency experience:
Well, the heart sink was never there, because if you didn't like the next person on the list then you didn't see them. [laugh] And you got to know the ones that you didn't want to see. So now I can't escape that! So it's interesting. You can't refer them back to their local doctor because it's you.
(Anna R)
Strategy 2: having a name for the illness
Despite concerns about diagnostic labels, the GPs recognised that there was a powerful value in having a name for illness and distress. They described the absence of a name as being ‘disorientating’ and ‘anxiety producing’ (Jonathan S). There was a sense that the name gave some sort of structure and framework for the patient in their suffering, and some way of thinking with the presentation, making sense of a series of seemingly unrelated symptoms. For one participant, the name ‘serves as a comforting wrap around things’ (Yvonne S), as it helps to make the distress seem more predictable, more manageable and the suffering justified. It is no longer ‘all in my head, doctor.’ A categorical diagnosis is also necessary for patients to access services in some contexts:
You know, once you've got the safety of a concrete rheumatoid arthritis diagnosis or something of that sort where either you as the practitioner or the registrar knows enough about it to make themselves comfortable, or they can find a nicely appropriate secondary care specialist to manage it all, they've got that safety valve.
(Xavier S)
Supervisors described registrars who were lost without a diagnosis at the end of the consultation, and left feeling ‘awkward’ (Kathy S). They recognised in these cases that there were often issues of language, and a paucity of descriptive terms: ‘maybe they just don't have the words’ (Kathy S).
A diagnosis provides a conclusion to the process and a justification that the doctor has done a good job. And a non-diagnosis potentially makes the registrar feel that the reason they've got a non-diagnosis is because they are fundamentally incompetent.
(Quentin S)
The pattern of best-practice care was also mentioned, with diagnosis preceding evidence-based treatment, and acting as a marker of good clinical practice. When evidence-based practice did not bring about cure, some of the registrars expressed doubt that the diagnosis was correct, and concern that their management was inadequate:
If I've given her some medication, I've tried some psychotherapy, and we're kind of a little bit better but not really better … Yeah. This patient's going to be … coming back all the time, same thing. I was thinking ‘Where am I going to take her?’ You know?
(Daniel R)
In the absence of a diagnostic label, participants used narrative to shape the patient's experience and make sense of it. They described patients as being ‘victims’ or ‘frequent attenders.’ They described them using stories, leaving the label open but discussing the language and frameworks they use to understand ‘what is going on’:
He's a very capable man who has lots of positive attributes, who's been worn down by his responsibilities [as a carer]. I mean, we're just giving him a hand.
(Leon S)
Strategy 3: avoiding diagnoses that apply a ‘layer of dismissal’
Most of the patients who were described had been diagnosed with disorders, either physical ones, such as asthma or arthritis, or psychiatric ones, such as anxiety or depression. However, there was suffering and distress that could not be fully explained by these diagnoses. The participants recognised that certain diagnoses may accurately describe the patient's illness, but in many cases they found them unhelpful and chose not to use them. Diagnoses such as borderline personality disorder, somatisation and hypochondriasis leave a ‘bad taste’ (Leon S) and also ‘carry weight’ (Jonathan S) for future care. One participant described the act of diagnosis in this context as ‘applying a layer of dismissal’ (Charlotte R):
Whether you voice it to them or not, it's not something you want to think of on their behalf easily … it does give me some negative emotions about them, about the relationship that we've had … and about my effectiveness and ability in that consult … it's almost like I've consigned them to something, you know, I've consigned them to the scrap.
(Xavier S)
It probably is the way that they relate to you … I feel more like they blame us for it … like, ‘Why can't you fix me?’ It's because … people don't seem to think of mental health issues as real diseases.
(Anna R)
The GPs described three important layers of diagnosis, namely a diagnosis that provided them with a framework of care, a diagnosis that helped the patient to make sense of their suffering, and a label that had the potential to direct future care:
If I actually give a name, I want it to be able to somehow help me … It's got to help me understand where you're coming from and what your issues are. … It's got to help me with how I manage you. … There's [also] got to be something that allows you to grow. There are some labels that, whilst it may sound helpful in understanding a process, that may give other doctors a significant misrepresentation of the person.
(Ian S)
They described this dilemma using an ethical framework. The diagnostic labels available to them in this context were unhelpful and potentially damaging to the patient. This included permission to ‘give up’ on the patient:
Personality disorder just means that we've given up … it actually gives you disutility, because it just means … I've got an excuse to give up on her and she's got an excuse to give up on herself.
(Paula S)
Another key consequence was the way the patient was seen by other health professionals as a consequence of the label, the way they ‘roll their eyes the moment the patient's name is mentioned’ (Charlotte R). The idea that you can protect a patient from future prejudice was a strong theme through-out the interviews. Participants spoke about their patients with respect, and tried to protect them from being discounted. They felt ‘reluctant for that patient to trot into casualty with [somatisation] on their notes’ (Warren S):
I think there's an ethic of us making a decision that we're not going to give them a label that's really, really sticky and stays there forever and has all sorts of negative stigma to it.
(Victoria S)
The participants were concerned that certain labels over-simplified the situation and were dangerous and misleading. They were also reluctant to use a label that their patients could not accept. They described patients who have a way of being in the world that is quite disordered, and yet felt these patients could not take the next step of accepting that they have a psychiatric disorder. One supervisor described her patient as being ‘a permanent emotional pre-contemplator, and you're trying to model a positive relationship that puts her in some position of power’ (Paula S).
Some participants expressed frustration that their patients were abandoned by the health system in the absence of a firm diagnosis:
We can treat chest pain. We can send them off to the cardiologist. We can give them a medication for it, then we can manage it, whereas I think with heart pain the patient flounders, the patient's family flounders, and it's never fixed. And it affects the patient's functionality. … They become, they become invalids. Whereas when we have a chest pain … you know, you go to out-patients, you join the cardiac support team, there are psychologists and there are dietitians and exercise physiologists, and you have a treatment path and you come out of it … you can even join a support group, survivor of you know, myocardial infarct. There is no ‘survivor of heart pain.’
(Charlotte R)
Strategy 4: managing disease surveillance
Many of the supervisors described keeping the potential for disease in focus by deliberately attending to physical cues during some consultations, and focusing on coping with chronic illness during others:
You sort of … pop your head up … you put the periscope up now and then to see if there is a way, there is an island nearby or a way out, otherwise you're just there with the patient travelling with them.
(Sarah S)
Other participants described outsourcing disease surveillance by referring the patient to a specialist. One of the registrars commented that this indicated to the patient that their concerns were being taken seriously:
If you refer them to someone they feel like you're paying attention, it's a serious problem … going up to see a special doctor was really putting the gravitas like, this is, ‘I'm really worried about you, I need you to go and see her … it's really important. You told me what you want to do, and I want to help you to get there, but you need to take it seriously.’
(Beth R)
However, several participants described Balint's collusion of anonymity,36 that is, by referring the patient to a specialist, they triggered a spiral of uncoordinated referrals to others. In doing so, they felt that the patient was being exposed to harm. This was not only the risk of iatrogenic harm, but also having their focus on physical disease cemented and the opportunities for addressing mental health issues lost.
When she becomes extremely stressed, her escape mechanism has become aberrant, and it's become a sort of pseudo-physical presentation, and because she moves from practitioner to practitioner, this level of medical chaos, there's a lack of, communication falls through, there's a lack of continuative care, and so she's over-investigated, over-admitted, and over-treated with medication.
(Charlotte R)
She saw a neurologist who, much to his credit, had just said ‘Look, I don't think there's very much organic going on here,’ and you know that in a way had reworded my approach, which she just didn't want at all and wanted a second opinion, which I sort of caved in on. But after that … it was just a sort of a spiral, it was like that cascade effect, where someone sees a specialist, and because the thing is not within the specialty for which they are trained [they] don't feel able to exclude organic pathology, and will therefore either make a referral or intimate that a referral would be required … and that led to this sort of spiral where we had two neurologists, an ophthalmologist, a neurosurgeon, a psychologist, vascular surgeon, endocrinologist, rheumatologist and cardiologist! … and I felt guilty about what was happening, but it … felt kind of out of my control. … And there was this sort of a lack of ability to say ‘Look, we need to stop now.’ And then the final straw was when she got admitted to hospital by one of the local surgeons for a leg ulcer and was in there for just months, months and months and months on end. Really, she should have come home. … So the whole medicalisation of her internal distress was really strongly embedded as a result.
(Warren S)
Several supervisors described the importance of managing the coordination of care for their patients, and their role as advocates in the complex tertiary specialist network:
‘Who is taking ownership of this case? Who is in charge?’ And the specialist smiled to himself ironically when I said it to him, and then said ‘Not me.’ And so, anyway, I said ‘Right, I'll find somebody.’ So I spent an hour and a half I think it was, jotting out a summary of the situation … it was over a page and a half of notes on the letter, and then rang up a friend of mine who was a hand surgeon … and I explained the whole scenario to him. It took me three quarters of an hour to actually go through it with him … and he said ‘Look, actually, I'll take charge. And if I can't deal with it, I'll find someone who will.’ And so he did. So then, that was a turning point.
(Jonathan S)
Discussion
Summary of main findings
GPs were very aware of the power of making psychiatric diagnoses in patients with medically unexplained symptoms. Somatoform and personality disorder diagnoses were cautiously applied, because the participants recognised the stigma and therapeutic limitations associated with these psychiatric labels. However, avoiding diagnosis altogether also carried ethical consequences. Patients without a diagnosis had difficulty accessing social support systems. Without a name for the illness, GPs and their patients struggled to make sense of their suffering. Supervisors described registrars feeling awkward or lost without a diagnostic framework. GPs managed this dilemma by constructing helpful narratives, presenting a positive view of the patient with a descriptive outline of their context, symptoms, strengths and challenges.
GPs also described the challenge of achieving a balance between the tendency to ‘medicalise misery’ by applying diagnostic labels too liberally, and ignoring suffering by not validating the patient's illness experience.
Disease surveillance was important, and GPs outlined various strategies to avoid missing serious physical disorders. These strategies included taking time to focus on disease screening, or using referral to specialist services. However, referrals had the potential to trigger a spiral of tertiary interventions. This carried the risk of iatrogenic harm, and meant that the GP lost the opportunity to manage the inherent uncertainty of the patient's illness. Many of the participants commented that uncertainty was poorly tolerated in the tertiary sector, with patients being over-investigated, over-treated and lost in a network of tertiary care. They expressed a commitment to coordinate care and provide advocacy and support.
Emerging theory
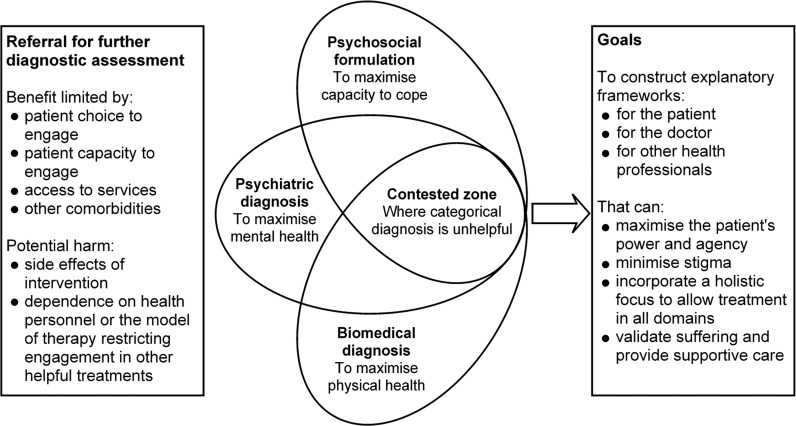
Figure 1 illustrates the emerging theory relating to assessment of medically unexplained symptoms in general practice. GPs describe diagnosing and managing three domains of patient distress, namely physical illness, psychiatric illness and psychosocial well-being. However, there are two major issues that remain after this process is complete.
Figure 1.
Constructing a helpful explanatory framework for patients with medically unexplained symptoms in general practice.
GPs need to decide how far they investigate and manage all three of these domains. Over-investigation and over-treatment are harmful. Balancing the likely therapeutic benefit with the potential for iatrogenic harm is a difficult but necessary task. In particular, GPs are concerned that patients may become ‘stuck’ in a cycle of investigation, or entrenched in treatments that are ineffective, which may prevent them from seeking more appropriate care. There is also the issue of access. Many patients are unable to afford or access investigations and treatment, or may choose not to engage with particular practitioners or therapies. Some patients may have comorbid illnesses that make some investigations or treatments inappropriate, difficult to access or harmful.
When this process is complete, these patients have significant residual symptoms that are distressing and medically unexplained. In Figure 1, this area is described as a ‘contested zone’, because there is disagreement about the most helpful categorical diagnosis to be used to describe patients. GPs may craft three explanatory frameworks in this zone, the first to help them to reason through and manage the situation, the second to help the patient to conceptualise their distress, and the third to explain their situation to other health professionals. These frame-works are often presented as stories, and are designed to validate the patient's suffering, to maximise their sense of their own power and agency, and to minimise stigma.
Strengths and limitations of the study
This study focused on the GPs of patients with medically unexplained symptoms. The interviews focused on a diverse group of patients that extended beyond categorical psychiatric disorders. The study also engaged a highly diverse group of GPs across Australia, who provided rich data. The constructivist grounded theory methodology of this study also facilitated the development of concepts and frameworks iteratively, which enriched both the data and the analysis.
Further study in this area could involve interviewing doctors and their patients over time. This approach could be used to explore differences in understanding and experience between doctors and their patients, and to highlight how diagnostic thinking develops. Observation of medical behaviour, rather than mere reflection on diagnostic thinking, would also enrich our understanding of this complex area.
The interviews revealed strong feelings among the GPs, and although this study focused on the way that the GPs made sense of the patient's presentation, further research could explore the discomfort experienced by GPs when managing situations that involve high levels of uncertainty. This was particularly interesting in relation to the GP registrars who were navigating the transition between tertiary and primary care.
A broader sampling frame may also enrich our understanding. In this study, participants were drawn from an expert sample who were experienced in reflecting on and communicating their clinical thinking and behaviour. It may be helpful to explore the attitudes of a broader range of GPs, particularly those who do not identify an interest in mental health. Conversely, there may be benefit in exploring the thinking of a range of GPs who identify an interest and competence in psychotherapy. Although grounded theory generated a rich methodological framework for this study, it would also be interesting to explore the experience of doctors and patients in this area using phenomenological or narrative perspectives.
Comparison with the existing literature
The question of where medical responsibility for suffering begins and ends is a difficult one. The patients described in this study were seriously un-well, and many of them struggled to function effectively in their social worlds. The GPs recognised this, but also discussed frankly the feeling of hopelessness and ‘heartsink’ described in the literature. For the registrars, managing the fear of ‘missing something’ was very challenging.
Although the medical profession has been criticised for ‘medicalising misery’,37,38 there has also been considerable public debate about so-called ‘contested illnesses’, where the medical profession is seen to turn its back on suffering in the absence of an accepted diagnosis.34,39,40 Balint's ‘collusion of anonymity’ is still problematic, and the GPs identified the importance of their role in coordinating care and providing advocacy and support. The concept of patient ‘ownership’ was critical, and the GPs described maintaining a central role in managing the complex network of clinical care and professional relationships. They also felt more professionally able to tolerate uncertainty than the tertiary networks of care, and felt that this minimised the risk of iatrogenic harm.
The participants agreed with the literature relating to multiple perspectives on diagnosis. Like Sadler,27 they identified that there was a role for categorical diagnosis, but also for other perspectives, including narrative. They described different diagnostic frameworks, namely the one that they held in their own thinking, the one that they shared with the patient, and often a third framework that they expressed to other health professionals.
Implications for future research or clinical practice
If young GPS are to acquire the skills that they need in order to deal with patients with mixed emotional and physical symptoms, where there is no single diagnosis, they need to learn from more experienced practitioners. GPs craft broad and sometimes idio-syncratic diagnostic frameworks41 that can be used to direct therapeutic effort. This ensures that heath care services and appropriate treatment are available to help those who are suffering, despite a lack of clarity about the diagnosis.
GP registrars would benefit from a broader discussion of the ethical implications of categorical diagnosis. The difference between an accurate diagnosis and a helpful one was a common theme in this study, and given the stigma surrounding psychiatric diagnoses, a broader discussion of the ethics of diagnosis in general practice would be helpful. This includes balancing the benefits of validating suffering by providing a diagnosis against the risk of ‘medicalising misery’ by labelling normal sadness with a disease name. Managing the ‘layer of dismissal’ associated with various diagnoses is clearly a common concern in the GP context.
Patients with undifferentiated distress commonly present to primary care services, but the role of the GP in managing this distress is contested. In this study a range of views was identified, from GPs who performed psychotherapy to those who referred patients for specialised treatment. Assuming ‘ownership’ of a distressed patient without an identified disorder raises questions about the role of the GP. For example, to what extent is it appropriate to provide support in the absence of a clinical disorder? In an environment in which healthcare is necessarily limited, and demand is increasing, there need to be discussions about the comparative value of supportive care for patients with medically unexplained symptoms in the community.
Young doctors are understandably concerned about missing a rare or serious diagnosis. This study identified clear strategies that were utilised to manage disease surveillance. Balancing the risk of iatrogenic harm against the risk of overlooking potentially serious disease was difficult, and it would be helpful for senior doctors to reflect on and communicate their strategies to registrars.
Conclusion
Managing patients with medically unexplained symptoms can be uncomfortable, and requires examination of core professional and personal values. This area would benefit from broader discussions within the profession to deepen understanding of clinical reasoning, professional values and role definitions.
ACKNOWLEDGEMENTS
This study was partly funded by the Royal Australian College of General Practitioners (RACGP) Foundation's Family Medical Care Education and Research (FMCER) grant, and their support is gratefully acknowledged. I am also grateful to General Practice Education and Training (GPET) for their support. I would like to thank my PhD supervisors and mentors Dr Claire Hooker, Associate Professor Jill Gordon and Dr Stacy Carter for their contributions to this study, and the interview participants for their time and expertise. I am particularly grateful to the academic GPs and medical educators who have enriched my understanding through discussion, reflection and their own writing in this complex area.
REFERENCES
- 1.Katon W, Ries R, Kleinman A. The prevalence of somatization in primary care. Comprehensive Psychiatry 1984;25:208–15 [DOI] [PubMed] [Google Scholar]
- 2.Katon W, Russo J. Somatic symptoms and depression. Journal of Family Practice 1989;29:65–9 [PubMed] [Google Scholar]
- 3.Barsky AJ. The paradox of health. New England Journal of Medicine 1988;318:414–18 [DOI] [PubMed] [Google Scholar]
- 4.Smith RC, Lyles JS, Gardiner JC, et al. Primary care clinicians treat patients with medically unexplained symptoms: a randomized controlled trial. Journal of General Internal Medicine 2006;21:671–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clarke DM, Piterman L, Byrne CJ, et al. Somatic symptoms, hypochondriasis and psychological distress: a study of somatisation in Australian general practice. Medical Journal of Australia 2008;189:560–4 [DOI] [PubMed] [Google Scholar]
- 6.Escobar JI, Waitzkin H, Silver R, et al. Abridged somatization: a study in primary care. Psychosomatic Medicine 1998;60:466–72 [DOI] [PubMed] [Google Scholar]
- 7.deGruy F, Crider J, Hashimi D, et al. Somatization disorder in a university hospital. Journal of Family Practice 1987;25:579–84 [PubMed] [Google Scholar]
- 8.Kroenke K. The interface between physical and psychological symptoms. Primary Care Companion to the Journal of Clinical Psychiatry 2003;5(Suppl. 7):11–18 [Google Scholar]
- 9.Brown FW, Golding JM, Smith GR. Psychiatric comorbidity in primary care somatization disorder. Psychosomatic Medicine 1990;52:445–51 [DOI] [PubMed] [Google Scholar]
- 10.Hanel G, Henningsen P, Herzog W, et al. Depression, anxiety, and somatoform disorders: vague or distinct categories in primary care? Results from a large cross-sectional study. Journal of Psychosomatic Research 2009;67:189–97 [DOI] [PubMed] [Google Scholar]
- 11.Toft T, Fink P, Oernboel E, et al. Mental disorders in primary care: prevalence and co-morbidity among disorders. Results from the Functional Illness in Primary care (FIP) study. Psychological Medicine 2005;35:1175–84 [DOI] [PubMed] [Google Scholar]
- 12.Deary I. A taxonomy of medically unexplained symptoms. Journal of Psychosomatic Research 1999;47:51–9 [DOI] [PubMed] [Google Scholar]
- 13.Fiddler M, Jackson J, Kapur N, et al. Childhood adversity and frequent medical consultations. General Hospital Psychiatry 2004;26:367–77 [DOI] [PubMed] [Google Scholar]
- 14.Resnick HS, Acierno R, Kilpatrick DG. Health impact of interpersonal violence: II. Medical and mental health outcomes. Behavioral Medicine 1997;23:65–78 [DOI] [PubMed] [Google Scholar]
- 15.Katon W, Sullivan M, Walker E. Medical symptoms without identified pathology: relationship to psychiatric disorders, childhood and adult trauma, and personality traits. Annals of Internal Medicine 2001;134(Part 2):917–25 [DOI] [PubMed] [Google Scholar]
- 16.Jewell D. I do not love thee Mr Fell … techniques for dealing with heartsink patients. British Medical Journal 1988;297:498–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosendal M, Fink P, Bro F, et al. Somatization, heartsink patients, or functional somatic symptoms? Towards a clinical useful classification in primary health care. Scandinavian Journal of Primary Health Care 2005;23:3–10 [DOI] [PubMed] [Google Scholar]
- 18.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). American Psychiatric Association, Washington, DC, 1994 [Google Scholar]
- 19.World Health Organization The ICD-10 Classification of Mental and Behavioural Disorders: clinical descriptions and diagnostic guidelines. World Health Organization: Geneva, 1992 [Google Scholar]
- 20.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). American Psychiatric Association: Washington, DC, 2013 [Google Scholar]
- 21.Feinstein AR. An analysis of diagnostic reasoning. 1. The domains and disorders of clinical macrobiology. Yale Journal of Biological Medicine 1973;46:212–32 [PMC free article] [PubMed] [Google Scholar]
- 22.Stone L. On botany and gardening: diagnosis and uncertainty in the GP consultation. Australian Family Physician 2012;41:795–8 [PubMed] [Google Scholar]
- 23.Green C, Holden J. Diagnostic uncertainty in general practice. A unique opportunity for research? European Journal of General Practice 2003;9:13–15 [DOI] [PubMed] [Google Scholar]
- 24.Kirmayer L. Culture, context and experience in psychiatric diagnosis. Psychopathology 2005;38:192–296 [DOI] [PubMed] [Google Scholar]
- 25.Mulvaney-Day NE, Earl TR, Diaz-Linhart Y, et al. Preferences for relational style with mental health clinicians: a qualitative comparison of African American, Latino and Non-Latino White patients. Journal of Clinical Psychology 2011;67:31–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beck B, Gordon C. An approach to collaborative care and consultation: interviewing, cultural competence, and enhancing rapport and adherence. The Medical Clinics of North America 2010;94:1075–88 [DOI] [PubMed] [Google Scholar]
- 27.Sadler JZ. Values and Psychiatric Diagnosis. Oxford University Press: New York, 2005 [Google Scholar]
- 28.Australian Psychological Society Evidence-Based Psychological Interventions in the Treatment of Mental Disorders: a literature review, 3rd edn. Australian Psychological Society Ltd: Melbourne, 2010 [Google Scholar]
- 29.Stone L. Being a botanist and a gardener: using diagnostic frameworks in general practice patients with medically unexplained symptoms. Australian Journal of Primary Health 2013;19:90–97 [DOI] [PubMed] [Google Scholar]
- 30.Karp DA. Illness ambiguity and the search for meaning: a case study of a self-help group for affective disorders. Journal of Contemporary Ethnography 1992;21:139–70 [Google Scholar]
- 31.Charmaz K. ‘Discovering’ chronic illness: using grounded theory. Social Science and Medicine 1990;30:1161–72 [DOI] [PubMed] [Google Scholar]
- 32.Råheim M, Håland W. Lived experience of chronic pain and fibromyalgia: women's stories from daily life. Qualitative Health Research 2006;16:741–61 [DOI] [PubMed] [Google Scholar]
- 33.Sadler JZ. Diagnosis/antidiagnosis. Radde J. (ed.) Philosophy of Psychiatry: a companion. Oxford University Press: New York, 2004. pp. 163–79 [Google Scholar]
- 34.Swoboda DA. Negotiating the diagnostic uncertainty of contested illnesses: physician practices and paradigms. Health 2008;12:453–78 [DOI] [PubMed] [Google Scholar]
- 35.Charmaz K. Constructing Grounded Theory. Sage Publications Ltd: London, 2006 [Google Scholar]
- 36.Balint M. The Doctor, his Patient and the Illness. International Universities Press, Inc.: New York, 1957 [Google Scholar]
- 37.Kleinman A. Psychiatry without context: turning sadness into disease. The Lancet 2007;370:819–20 [Google Scholar]
- 38.Ussher JM. Are we medicalizing women's misery? A critical review of women's higher rates of reported depression. Feminism and Psychology 2010;20:9–35 [Google Scholar]
- 39.Bulow PH. Sharing experiences of contested illness by storytelling. Discourse and Society 2004;15:33–53 [Google Scholar]
- 40.Fink P, Toft T, Hansen MS, et al. Symptoms and syndromes of bodily distress: an exploratory study of 978 internal medical, neurological, and primary care patients. Psychosomatic Medicine 2007;69:30–39 [DOI] [PubMed] [Google Scholar]
- 41.Heneghan C, Glasziou P, Thompson M, et al. Diagnostic strategies used in primary care. British Medical Journal 2009;338:b946. [DOI] [PMC free article] [PubMed] [Google Scholar]
CONFLICTS OF INTEREST
None.