Abstract
Purpose
Approximately 4.8 million stroke survivors are living in the community with some level of disability requiring the assistance of family caregivers. Stroke family caregivers are often unprepared for the demands required of them. The purpose of this grounded theory study was to explore the needs of stroke patients and their family caregivers as they transitioned through the stroke care continuum from acute care to inpatient rehabilitation to home.
Methods
Thirty-eight participants, 19 recovering stroke patients (11 male, 8 female), 15 primary family caregivers (14 spouses, 1 mother), and 4 adult children were interviewed during their stay at a rehabilitation facility and within 6 months of discharge. Interview questions were loosely structured and focused on the stroke experience and how patients and caregivers were managing postdischarge. Data were analyzed using dimensional and comparative analysis.
Results
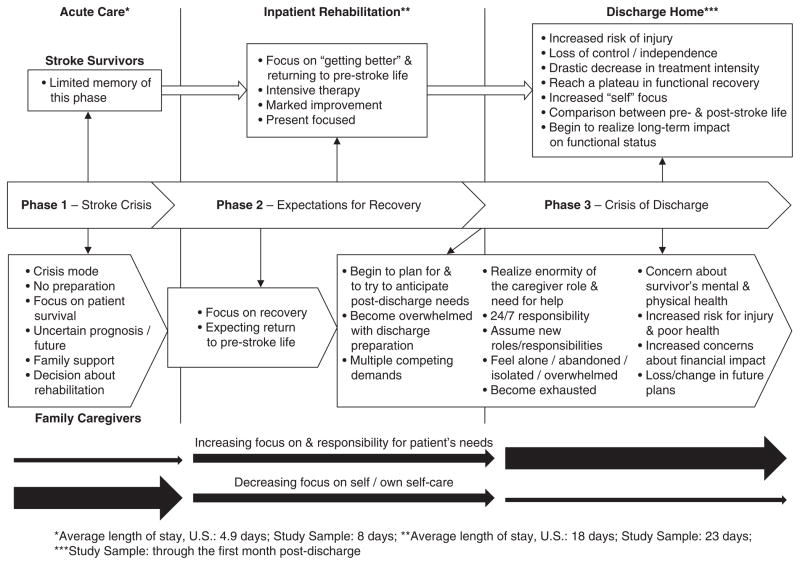
Findings were organized in a conceptual framework illustrating the trajectory of the crisis of stroke. Stroke survivors and their caregivers faced enormous challenges as they moved through 3 phases of the trajectory: the stroke crisis, expectations for recovery, and the crisis of discharge. Findings from this study suggest that as caregivers move through the phases of the trajectory, they do not have a good understanding of the role to which they are committing, and they are often underprepared to take on even the basic tasks to meet the patients’ needs on discharge.
Conclusion
Stroke survivors and their caregivers do not have adequate time to deal with the shock and crisis of the stroke event, let alone the crisis of discharge and all of the new responsibilities with which they must deal.
Keywords: caregiving, discharge planning, qualitative research, stroke
Each year, nearly 800,000 people experience a new or recurrent stroke event.1 Approximately 4.8 million stroke survivors are living in the community with some level of disability, and 50% need assistance with activities of daily living (ADLs) or instrumental activities of daily living (IADLs).2 As diagnosis and interventions for persons with stroke improve, the number of stroke survivors and, in turn, the number of familial caregivers will increase. Although stroke survivors often have significant functional limitations, the implementation of prospective payment systems for inpatient rehabilitation services in the United States has resulted in significant reductions in lengths of stay for stroke rehabilitation3,4 by as much as 8 days.5 These reductions are not new. In the 1980s, a study of more than 3,000 stroke patients showed that the length of acute care hospital stays reduced from 17.5 to 6.4 days.6 Patients with stroke thus continue to be discharged home “quicker and sicker,” resulting in increased stress on family caregivers who are typically unprepared to meet the accommodations and need for assistance with ADLs/IADLs that is required (eg, establishing wheelchair access, assisting with toileting, dispensing medications, and driving to doctor’s appointments).
In 2009, more than 65.7 million unpaid caregivers in the United States provided an average of 20 hours per week of care, with an estimated market value of $375 billion.7,8 Most were family relatives, and their efforts were not without cost. Deleterious effects on the health and well-being of these caregivers has been well documented in the literature9–13 and identified as a major public health concern.14 Approximately 3.5 million of these unpaid caregivers are family members providing care for stroke survivors.7
Needs of stroke caregivers are categorically different from those of caregivers of persons with progressive conditions such as dementia in that stroke is an unpredictable and sudden event that can be life-disrupting and does not allow family members sufficient time to prepare for the complex responsibilities of caregiving. Stroke patients with residual functional limitations typically transition from being cared for by formal caregivers in acute care and inpatient rehabilitation – 24 hours a day, 7 days a week – to relying fully on informal caregivers (most often a spouse or adult child). Even if the caregiver has had previous experience caring for individuals with disabilities, the demands and vigilance required for adequate care at home are often overwhelming and exhausting. Researchers’ findings have repeatedly demonstrated the damaging health effects of caregiving. Caregivers often describe feeling isolated, abandoned, and alone13,15,16; what frequently follows is a predictable trajectory of depression and a downward spiral of deteriorating physical health.9,10,12,13,17,18
Adverse consequences of caregiving ultimately affect the care recipient as well. Research indicates that outcomes for patients with stroke are influenced by the ability of the family caregiver to provide emotional and instrumental support as well as assistance with ADLs.14 As the caregiver’s health decreases, the patient’s health and recovery will also likely suffer, leading to premature placement in an institution. Shyu, Chen, and Lee19 found that persons with stroke who were cared for by caregivers who needed more support were 5 times as likely to be rehospitalized. So, although there is sufficient evidence that caregiving can have debilitating effects on caregivers and patients, research investigating the needs and experiences of caregivers as they move into this role is limited. This is particularly true of cases in which the transition occurs because of a sudden, life-altering event, such as stroke.
The purpose of this grounded theory study was to explore experiences of stroke patients and their family caregivers as they moved from acute care to inpatient rehabilitation to home and to identify their needs as they transitioned through the care continuum. The model developed in this study differs from findings in other studies about stroke caregiving, because it illustrates the crisis points and consequences experienced by stroke caregivers and patients as they move through the care continuum. The findings suggest that the root of long-term caregiver strain and burden may be traced back to the crisis caregivers experience as patients transition from rehabilitation to home.
Methods
After receiving approval from the institutional review board of the study facilities and university, patients experiencing their first stroke and their family caregivers were recruited by the case managers at each inpatient rehabilitation facility (IRF). Patients (when they were able) or their primary caregivers were contacted by the research team and informed about the study. Interview times were set up and consents were signed prior to the start of the first interview. Study participants were interviewed while the patients were still in rehabilitation or as close to discharge as was convenient for the caregiver. In 5 cases from 1 site, we did not receive the contact information for the caregiver until the day of discharge. These caregivers wanted to participate in the study, but they chose to delay the interview because the transition from rehabilitation to home was so overwhelming. These interviews were conducted within 4 days to 6 weeks postdischarge. The second interview was conducted within 6 months of discharge in a location convenient for the caregivers and patients (usually the home). Caregivers and patients were given the option of being interviewed together or separately. Interview questions were loosely structured. The first interview focused on patients’ and family members’ plans and needs for postdischarge care. In the second interview, participants were asked to compare their experiences of stroke recovery and caregiving to their initial expectations.
Based on the analysis of the data from the patients and caregivers, we realized we also needed to understand the perspectives of the IRF case managers regarding patients’ and caregivers’ needs and discharge concerns they identified when working with stroke patients and their families. Therefore, we conducted a group interview with 3 case managers at 1 site and an individual interview with the case manager at the other site. We used these data in our comparative analysis to understand the differences in perspectives between caregivers and case managers in terms of discharge needs.
Data analysis
Data were analyzed using dimensional analysis, a naturalistic analytic strategy developed for use with text or narrative data in qualitative studies.20–22 Based on the coding procedures set forth by Strauss23 and Strauss and Corbin,24 dimensional analysis consists of a line-by-line coding process that identifies and tracks the study participants’ constructions of the phenomenon or experience in question.20–22 Consistent with symbolic interactionism, dimensional analysis allows the researcher to identify how individuals carve out reality, in other words, what captures their attention and contributes to their understanding and experience.25 The end result is a framework that identifies “reality” as defined by the study participants using their perceptions, understanding, preferences, and logic. This framework becomes the basis for the final grounded theory.
Using constant comparative technique,23,24 comparisons were made among the narratives of stroke patients, primary caregivers, other key family members, and case managers, along with the literature about discharge decision making. NVivo 8.0 (QSR International, Melbourne, Australia) qualitative data management software26 was used to aid the research team in analyzing and managing the data and in making comparisons within and across texts. As dimensions were uncovered in the data, they were verified with other study participants as a way to substantiate their cogency with the developing conceptual framework.
A multidisciplinary research team, consisting of the study team and graduate and undergraduate students, helped to develop and revise the conceptual framework. The principal investigator and research team met weekly to discuss the ongoing analysis and wrote field notes and memos23,24 to create an ongoing audit trail to document and record study findings and to track methodological and substantive decisions made during the analysis. Several renditions of the framework were developed as the data analysis progressed. The final conceptual framework illustrates components of the stroke crisis trajectory from the perspectives of patients and family caregivers through the first month postdischarge.
Study participants
The study sample included 20 patient/family units from 2 IRFs; 6 were Black, 1 was American Indian, and 13 were White. A patient/family unit included the patient, his or her primary family caregiver (usually a spouse), and any other family members who were involved in the patient’s care. Data were collected between January 2008 and August 2009 via 2 interviews with members of these units. One patient/family unit withdrew prior to the first interview, and 3 withdrew before the second interview because they did not feel they had time to complete the interview. In all, we collected data from 38 individuals, including 19 recovering stroke patients (11 male, 8 female), 15 primary family caregivers (14 spouses, 1 mother), and 4 adult children. Three of the stroke survivors lived alone and chose not to provide contact information for their family members. Seven of our families had annual incomes lower than $20,000; 8 had incomes above $40,000. Table 1 provides average ages for participants and FIM* scores for stroke survivors.
Table 1.
Participant demographics
| Participants | Mean | Range |
|---|---|---|
| Caregivers (n = 19) | ||
| Age | 58 | 23–82 |
| Stroke survivors (n = 19) | ||
| Age | 64 | 33–84 |
| Admission FIM | ||
| Total | 49 | 28–73 |
| Motor | 26 | 12–47 |
| Cognitive | 23 | 11–32 |
| Discharge FIM | ||
| Total | 78 | 56–105 |
| Motor | 53 | 32–73 |
| Cognitive | 25 | 16–32 |
FIM™ is a trademark of Uniform Data System for Medical Rehabilitation, a division of UB Foundation Activities, Inc.
The FIM is an instrument used in rehabilitation to measure patient functional ability. It has 18 items in 6 domains related to cognitive and motor function. Total FIM scores can range from 18 (totally dependent) to 126 (totally independent).27–29 Thirteen of the stroke survivors had admission motor FIM scores below 30, indicating severe functional limitations. In a previous study, Lutz30 found that stroke patients with an admission motor FIM score below 30 were almost 3 times as likely to be discharged to a nursing home.
Results
Stroke crisis trajectory
As study participants moved through the stroke crisis trajectory from the stroke event to discharge home, they described their experiences as a series of 3 phases: the stroke crisis, expectations for recovery, and the crisis of discharge. They identified important dimensions in each phase of the trajectory that are described in the following paragraphs with representative quotes. The quotes are labeled with a [P] for patient and [C] for caregiver followed by a case number. These phases are illustrated in Figure 1.
Figure 1.
Stroke Crisis Trajectory
Phase I: Stroke crisis
Phase I occurred when the patient was diagnosed with stroke and admitted to acute care. Our findings demonstrated this as a time of high anxiety, shock, and disbelief for patients (when they are cognizant), caregivers, and other family members. During their stay in acute care, family members and stroke survivors (if they were cognizant) began to recognize what happened to them. They experienced stress, confusion, fear, and loss of control and began to wonder what would happen next. Most stroke survivors had limited memory of this phase and relied on their caregivers and family members to fill in the gaps about what happened. With the crisis of stroke, the focus was on survival and determining what steps should be taken next. Family members of patients with severe stroke were very concerned about the patient’s survival as this caregiver describes:
All the kids came. And we had some very serious discussions, and there was some debate that he wouldn’t live and what do we do now. And it was good that all of us were there, making decisions on the same thing…The second night he was there, they said, call his family and tell them to come. So I did and they came. We thought we were going to lose him, but he made it through. He made it through and in the seventh day, they transferred him to rehab. And we were so happy. [C-18]
Family caregivers typically had no preparation for the predicament in which they found themselves. Some blamed the patient, themselves, or emergency medical personnel for not immediately recognizing the stroke symptoms. In some cases, family members blamed the caregiver: “I can’t believe my mother didn’t realize that my dad was having a stroke” [C-18]. In this time of shock, disbelief, and crisis management, however, other family members and friends often rallied to provide support for the patient and the primary caregiver.
In my family, as an entirety, I felt I had lots of support. On the day of his surgery, 5 of his 6 daughters were there—plus his brother and his nephew from down south. [C-14]
Research shows that when persons are faced with crisis situations, their capacity to take in new information and make decisions is compromised. Yet during this time, caregivers may be asked to make life-changing treatment decisions for a family member with stroke.31 Because the focus at this time was on the patient’s survival, family members often requested that “everything be done” for the person with stroke. They were not yet thinking ahead, nor did they understand the challenges that lay before them or the long-term implications of stroke recovery.
The amount of time stroke survivors and caregivers had to face this crisis and make life-changing decisions was often very short. Many patients in our study moved very quickly from acute care to rehabilitation; some were discharged to the IRF straight from the intensive care unit. Our participants’ acute care lengths of stay ranged from 24 hours to 23 days, with 8 days as the average. Nationally, the average length of stay in acute care poststroke is 4.9 days.1
Phase II: Expectations for recovery
Once the patients’ health status stabilized, families and patients began to look ahead to the next step in the trajectory and focus on recovery. This was when the option of inpatient (acute) rehabilitation was presented to patients and family members, with nursing home placement or subacute rehabilitation (usually provided within a nursing home) as an alternative. For many patients and families, nursing home placement was not viewed as a suitable option. As this caregiver describes, “Being very familiar with nursing homes, no. That’s not what I wanted, I wanted more” [C-13]. Our participants viewed rehabilitation at an IRF as synonymous with recovery. The implied promise of inpatient rehabilitation was that patients would not be discharged home until they were able to return to their prestroke lives. “I wanted him to have the best chance to recover as much as possible, so he can get back to the things he enjoys doing. So that’s how we chose this [rehab] hospital” [C-17]. Therefore, committing to returning home after discharge – an important criterion for admission to an IRF – seemed realistic. Oftentimes family members did not understand the scope of the decision to which they were committing.
For patients who lived alone and were not able to identify a primary family caregiver who could provide care postdischarge, this was also a time to begin thinking about and planning for their future options. They began to try to identify possible extended family or friends who might be available for help, so they could return home. For those without these options, they viewed inpatient rehabilitation as an extension of their inpatient stay, in hopes of achieving a level of recovery and function that would allow them to return home independently. They also realized that going to inpatient rehabilitation provided them with time to figure out the next step in their recovery process.
This phase typically began near the end of the acute care stay and continued through much of the stay at the IRF. The average length of stay in the IRF for our sample was 23 days, with a range of 8 to 38 days. Nationally, the average length of stay in an IRF for patients with stroke is approximately 18 days.3
Patients came into the IRF and were assessed; plans of treatment were developed by the rehabilitation team, and therapy commenced. However, the team often could not give family members a good sense of the patient’s expected level of recovery until they had sufficient time to evaluate the patient’s ability to progress with the treatment plan.
Although family caregivers and stroke survivors began to acknowledge poststroke impairments during this phase, it was also a time of optimism and hope. Stroke survivors focused on “getting better,” and many believed they would be able to stay in the IRF until they “got better.” Their definition of improvement, however, was not always congruent with rehabilitation providers’ perceptions. Stroke survivors’ views of “getting better” meant returning to their prestroke activities and life: “I expect that I’ll go back to doing everything I did before this all happened” [P-6]. Another said, “I just wanted them to bring me in here [IRF] and teach me to walk, so I could walk out of here” [P-1]. This survivor then expressed that even if this level of recovery took some time to occur, he would “eventually…be able to walk alone, by myself, within a year.” For health care providers, “getting better” may mean a small, but notable, change in function such as improved balance, increased strength, or walking a short distance with assistance.
During this time, stroke survivors were receiving intensive therapy for 3 or more hours per day. They often noticed marked improvement and this, coupled with the encouragement and support from therapists and nurses, fueled their expectations of returning to prestroke activities. They tended to stay present-focused, working each day to improve their function, strength, and stamina. It was a time of hope and optimism.
Every day as I’m going to my therapy classes, every day, I feel that am a new person again being here. Now, I can walk on a cane, and I can move my hand a little bit better than what it was, because it was dead, you would be surprised how you can see me walking on a cane, compared to the time I came in here. [P-7]
For primary caregivers, this time was characterized by relief that the patient survived the stroke and by hope for a return to prestroke activity and life. They typically assumed the stroke survivor would be able to stay in the IRF until he or she was able to at least assist with most ADLs and IADLs and be able to be alone at least for short periods of time.
But I, I really feel like that by the time we go home, he is going to be able to do enough that I can assist him. [C-1]
Phase III: Crisis of discharge
Discharge home was typically a highly anticipated event for stroke survivors and caregivers. They believed that when they got home, things would return to normal and life could resume its previous routine, with few or minor changes. However, at some point during the rehabilitation process, family caregivers began to realize the stroke survivors were going to be discharged even if they had not met their functional goals and that they (the caregivers) needed to prepare for the stroke survivors’ postdischarge limitations and resulting needs. For some, this realization did not come until a day or 2 prior to discharge, and the discharge date, itself, often surprised caregivers. “It was quick, when they went to release him. It was real quick” [C-2].
This created another crisis. Caregivers were required to determine what needed to be done and who could do it to accommodate the survivor postdischarge. For example, would the house need to be remodeled, carpeting removed, a ramp added, a bathroom or bedroom reconfigured? What kinds of equipment would they need? Should they rent it or buy it? What kinds of support would be needed (eg, personal care assistance)? Could they afford it and, if not, would their insurance pay for it? Who would help if they could not afford paid assistance? What would they do about their jobs? Would they be able to keep working? If not, what would they do for income? Did they qualify for social services like Social Security disability and food stamps? How would they get these things? Who should they talk to? The list seemed endless and overwhelming. Although case managers could assist with tasks related to the patients’ needs by providing a list of phone numbers or ordering equipment, the caregivers had to schedule, complete necessary paperwork, and coordinate and be available for appointments and deliveries.
Moreover, caregivers were expected to be at the IRF to receive training to care for the stroke survivor at home. In fact, IRF staff viewed attendance and attention at rehabilitation training sessions by family members as a measure of how well the patient and family would fare at home. As this case manager describes:
And the daughter took him home to her house to provide care, and she said that from day 1, when I did my assessment, ‘Oh, don’t worry about me, I’ll be fine’. And she was one of those family members who was here daily, who was hands-on, not afraid to get in there and you know, provide some nursing care and some continence help. So, I wasn’t terrified about her going home at all.
The amount of preparation and training required made most caregivers feel overwhelmed and exhausted before the patients ever got home.
It was really, really stressful because we were moving in [to a new apartment], we [caregiver and adult daughter] didn’t have a chance [to unpack]. We wanted to have everything ready so at least there could have been walkways [in the hallways] for him to walk. [C-12]
Bringing the survivor home prompted mixed feelings. Most patients wanted to go home, but their caregivers were understandably concerned if rehabilitation goals were not met and they felt they had inadequate time to prepare. Patients, themselves, were also alarmed if they felt they were dismissed prematurely. Being home also meant a drastic reduction in therapy, from 3 hours per day to a few hours 1 or 2 days a week. Often, the therapy did not start for a week or more postdischarge. This was typically accompanied by a plateau or regression in recovery that survivors and caregivers attributed to the reduction in therapy and/or a change in therapists. Both survivors and caregivers were also required to develop relationships with new therapists and nurses.
Once home, stroke survivors realized they had to depend on others for things they took for granted their whole lives. They were beset with feelings of frustration, anger, sadness, loss, grief, and/or depression, as this quote illustrates:
You know, it’s very humiliating to have to call somebody so you can go to the damn bathroom in the middle of the night. Just to go to the bathroom. Yeah, that’s when you know you’re really screwed up, when you have to call somebody to help you out with something that simple, something you take for granted your whole life. [P-13]
When patients did come home, their caregivers began to realize the enormity of the tasks before them. They were now responsible for providing care for 24 hours a day, 7 days a week. “It was a day from hell, the day he was discharged. It was horrible. I mean, you know, a terrible, terrible experience” [C-4]. These caregivers began to realize the skills they learned during inpatient rehabilitation did not always translate well at home. For example, the bathroom door at home may not be wide enough for a wheelchair or for 2 people to walk through together. Transfers were far more difficult in the home than in rehabilitation, and caregivers were often required to do as many as 8 to 10 transfers each day.
The transfers in [the IRF] were not realistic to the transfers in real life. The transfers were off of one of those gym tables cranked to just the ideal height to match the chair to transfer from the chair to the table or back…Home is totally different; things are different heights. We had to take the wheels off of the hospital bed and put coasters on there, because the hospital bed was too high up, even at its lowest position for me to sling [transfer] him to the wheel chair….[C-20]
Providing care in the home environment, especially transfers and medication administration, without the support of rehabilitation staff, resulted in safety concerns for caregivers and patients. Ten of the patient participants had fallen at home, and often caregivers either fell with them or were injured trying to help the patients get up. Falls generally occurred when caregivers were helping the patients transfer to and from the bed or wheelchair or when the patients lost their balance or tried to transfer without assistance. These quotes from 3 participants illustrate the issue of falling at home:
He doesn’t remember a lot, but he’s, he’s had 5 falls since we brought him home. He fell against me and sent me back into that corner. And I knew that ottoman was there, and I was like, “Oh, if I go over that ottoman I’m going to hurt myself,” and so I’m trying to catch myself, and so I managed to get myself righted…He got a bruise on his head. [C-14]
I fell off the walker; I don’t remember falling. I broke my ankle in 2 places. [P-8]
I was sitting on the potty chair, and I reached down to pick up something and it was on the floor and I wound up on the floor and he had to pick me up. And he does not need to do things like that. He just doesn’t because he gets so short of breath. [P-19]
Taking on the responsibility of administering multiple medications at various times throughout the day also presented safety concerns.
I came across 2 medications the other day that were so similar, one was the littlest bit more yellowy and the other was the littlest bit more blush looking. And I said I’m scared to do this because I was afraid I was going to give him the wrong thing. [C-1]
Medication administration was especially problematic when the caregiver was overwhelmed and exhausted as this caregiver describes:
I’m terrified that I’ll mix up a med. I’ve got them in a little pill container, so I just have to dump them out, but I’m just terrified that I’ll give him the wrong pill at the wrong time because I’m disoriented. [C-20]
Nighttime behaviors and financial burdens also presented serious challenges for many caregivers. Stroke survivors who woke at night and called for help or tried to get up unassisted caused caregivers to experience generalized worry that often resulted in insomnia and exhaustion, as described by this caregiver:
I continue to have not enough sleep and he continues to be sleep deprived, one or both of us is going to end up seriously injured, because we’re going to fall doing the transfers. [C-13]
Financial difficulties added to mounting burdens. Lost income from patients and/or caregivers who were working prior to the stroke and the depletion of retirement savings to cover the costs of medications, equipment, and services that were not covered by insurance were all a source of concern, as this couple describes:
She’s [the caregiver] doing all these big things, like getting the house ready for the market [to sell]. I’m not working, so I don’t have an income stream so I can’t pay my car payment. So, goodbye car. They came and got that [P-4].
I’ve had to deal with all his bills….[C-4]
All my creditors. [P-4]
… to try to renegotiate the bills. All the doctors, the hospitals, the credit cards, you know, who else can do it? [C-4]
Caregivers not only worried and were inundated with providing daily care for the stroke survivors, they also had to pick up the tasks that were done by the survivors before the stroke. This included maintaining the household, paying bills, doing laundry, preparing meals, and lawn care. Additionally, they had the added responsibility of keeping track of and getting the patients to multiple appointments and managing medications. “My thing now is to try to regulate her medicine intake, try to get her to therapy, try to engage with a few exercises with her” [C-9]. Over the course of the trajectory, caregivers found that they were expected to take on increasing responsibility for meeting patients’ needs and concerns. This resulted in decreased focus on themselves and their own health over time. Self-care is often the last item on caregivers’ list of daily tasks.
You balance it the best you can. You have to accommodate him before yourself. It’s an ongoing process—trying to find balance, trying to find time for me, even 5 minutes. [C-13]
Even caregivers who had previously worked with disabled, elderly populations expressed feelings of being overwhelmed, abandoned, and isolated: “I felt like I was a little old Eskimo woman that they put on this ice block, chopped it off and sailed it out in the middle of the ocean” [C-17]. They were totally exhausted, as these quotes from 2 of the caregivers indicate:
The first 3 weeks were the 3 weeks from hell. Because both of us are tired and he’s not able to do the things he was doing [in inpatient rehabilitation]. [C-13]
I can probably even stand the not sleeping. But I can’t work 18-hour shifts and have no sleep. ….I really haven’t had any time to grieve; it’s been nonstop from the minute he went into [the hospital]. I was there every breathing minute, in ICU to the 33 days in rehab, to [40-mile] drive to [the IRF]…it’s just been nonstop. There has been no break. None. [C-20]
Conditions that influenced the crisis of discharge
There were several conditions described by caregivers and patients that influenced their abilities to manage the transition from the IRF to home. The degree to which the caregivers’ capacity to provide care (ie, their experience, skill, physical stamina, proximity) matched with the patients’ level of need (ie, their functional status, need for assistance with ADLs and IADLs) impacted how well the patient and caregiver were able to make the transition home. This has been supported in the previous research.30,32 However, for some caregivers, having a high capacity to provide care was equated with expectations from themselves and others of taking on all of the care and needing little or no help that resulted in increased strain.
Protective factors identified by caregivers that helped to minimize the discharge crisis included self-awareness (ie, recognizing their limitations) and a strong sense of self-advocacy. These caregivers were able to identify what care they could and could not provide and indicate these limitations to the case managers and therapists. They typically had a physical condition, such as a previous back injury or heart condition, which limited their capacity to provide physical care. However, when advocating for themselves in this way, they had conflicted feelings of guilt for limiting their role. These feelings were increased when health care providers and other family members questioned them about why they were not going to assume the total care for the stroke survivor, as described here:
It was a surprise, and it was scary and one of the therapists—oh, she made me felt so bad. “Mrs. [caregiver’s name], you mean to tell me you are not taking him home?” I said, “I cannot; I live by myself, just my husband and me. I cannot provide 24-hour coverage for him…” Oh, I just felt so bad. I said, “Lord have mercy.” I was [also] battling his two older sisters who were having a fit that he was going to nursing home care, and never mind the fact that they weren’t going to come and help with his care, oh Lord. [C-17]
In our study, only 3 caregivers described this strategy of self-advocacy; the rest took on the role despite misgivings and even when they felt ill-prepared to do so.
Finally, financial resources and informal support networks also influenced the crisis of discharge. Those caregivers who could afford to pay for assistance or who had family members to help them were not as overwhelmed and exhausted as those caregivers who were left to manage the transition home alone.
Options for stroke survivors who lived alone were limited if they did not have the support of family and/or friends for postdischarge care. In this study, there were 3 participants, all female, who lived alone prior to their stroke. One participant decided early in the process that she would need to spend time in a nursing home after her stay at the IRF and prior to moving back home because the only available family caregiver was her daughter-in-law, who was caring for 3 young children alone while her husband was deployed overseas in the military. This participant received some instrumental support from her daughter-in-law but did not want to ask her to help with personal care or daily activities.
You know there’s just too much going on there. She would have to be worrying about me every time she went out, whether I was okay or not, and I don’t want to put that on them [P-3].
The other 2 participants expected that family members (adult daughter or daughter-in-law) would be available to provide the care. However, this did not work out as expected. In our last contact with them, they were considering other options, such as nursing home placement.
Discussion
Stroke patients and their family caregivers in the United States are faced with enormous challenges as they move through the stroke care continuum – from acute care to inpatient rehabilitation to home. Findings from this study provide compelling evidence that as caregivers move through the phases of the trajectory they do not have a good understanding of the role to which they are committing, and they are often underprepared to assume even the basic tasks to meet the patients’ needs on discharge. They do not have adequate time to deal with the shock and crisis of the stroke event, let alone the crisis of discharge and all of the new responsibilities with which they must deal.
To stroke survivors and their families, the expectation of rehabilitation is that the survivors will be functional on discharge, perhaps not back to prestroke levels, but at least able to attend to the basic ADLs, particularly toileting and hygiene. Shortened lengths of stay, especially for those with significant functional limitations, are often inadequate for both the logistical and emotional preparation that many family caregivers must undertake to achieve the tasks of preparing the home and marshalling resources for discharge – all the while doing their best to be emotionally and physically available to the survivor. They do not have the time to adjust to the idea that recovery might not be complete, to arrange home modifications, and to learn strategies to deal with functional limitations that may persist after discharge. Additionally, there is inadequate time to deal with the grief of the loss they are suffering in the aftermath of stroke.
Other authors have identified support needs and gaps in care for patients and caregivers as they transition through the care continuum.33–35 Our stroke crisis trajectory adds to this literature by vividly illustrating the consequences of these gaps as caregivers accompanied stroke survivors in the transfer from acute care to rehabilitation to home. Much of the time when caregivers are expected to make decisions about the patients’ welfare and prepare for and implement newly learned tasks and skills, they are in crisis and are overwhelmed. The crisis of discharge is where caregivers in our study became totally overwhelmed and realized they were not ready to assume the tasks and responsibilities of caring for and managing daily physical, instrumental, and emotional needs of the stroke survivor. They had neither the time nor the resources to deal with their own needs for emotional and instrumental support. These phases impacted the support and information needs of caregivers and patients and their abilities to successfully navigate their way through the stroke care continuum.
Our findings suggest that these caregivers face excessive burdens, and many of them are the sole caregivers for stroke patients. The trajectory presented here demonstrates that as patients are physically transferred through the care continuum from acute care, to IRF, and to home, caregivers are often not ready to transition to the next level of care and take on the added responsibilities of caregiving. This was particularly problematic during the time when patients were discharged home. As a result, caregivers not only are at risk for serious physical and emotional problems, but also feel a sense of abandonment and loss of support from the current health system.
Implications for practice
The findings suggest implications for practice as patients and caregivers transition through rehabilitation to home. Rehabilitation staff should be cognizant of and sensitive to the needs of caregivers as they are dealing with the overwhelming life changes that result from the disabling experiences of stroke. Several authors have developed interventions for caregivers of stroke patients postdischarge.36–38 These interventions provide problem solving and educational information to help caregivers cope with the new role in which they find themselves. Because of the crisis points that caregivers face prior to patients’ discharge, our findings suggest caregivers may need more intensive interventions while the patients are still in the IRF and as they make the transition home, especially in the first month postdischarge. These transitional interventions should begin with an in-depth, systematic assessment of the caregiver’s needs and ability to take on the caregiving role and awareness of the potential for poor outcomes. Assessment of the caregivers’ understanding of and capacity to take on the caregiving role as the patients move from acute care to rehabilitation is a key piece usually missing from a patient-focused assessment on admission to rehabilitation and has been recommended by researchers and caregiver advocates for several years.39–41
Additionally, caregivers and patients, if they are able, may benefit from regularly scheduled family counseling to help them better manage the multiple losses that they are suffering and to adapt to the major life changes they are facing poststroke. However, this type of counseling is generally not recommended to caregivers and patients during inpatient rehabilitation or postdischarge. None of the caregivers in our study were referred to family counseling to help them deal with these life changes.
When caregivers indicate that they may be unable to care for the patient at home, rehabilitation staff must work with caregivers to identify suitable options for care. This finding also suggests the need for changes in health care policy with more flexible payment systems allowing for the right services to be delivered at the right time to meet the needs of the patient and the family caregiver. These services may include inpatient rehabilitation and follow-up subacute care to allow caregivers the time they need to prepare for the long-term role of caregiving.
Conclusion
Our society values and applauds caregivers who decide to bring their family members with stroke home to advance their recovery and provide for a high quality of life. Not only is this viewed as being socially desirable, the right thing to do, and preferable to nursing home placement, it saves billions of dollars in formal health care services every year.8 These savings, however, seem to be at the expense of the physical and emotional well-being of the caregivers who make such a commitment. In the current US health care system, transfers of care from one level to the next are fragmented, poorly coordinated,33,34 and do not take into account the capacity of the caregivers or the emotional and support needs of the patient/caregiver dyad. Transfer and discharge decisions are based on insurance policy directives and prospective payment systems and not on the needs or well-being of caregivers and care recipients. Caregivers in our study felt isolated, abandoned, and alone and told us they felt like they “had been pushed off a cliff” when they were discharged home without the requisite support services or assistance.
Because of funding policies, the current system focuses on the needs of patients and views family caregivers as resources for patients. The needs of caregivers are marginalized and eclipsed. The caregiving capacity of family members is not systematically assessed prior to discharge, and there are limited, if any, transitional services available to stroke survivor/caregiver dyads as they move home, which leaves them to cobble resources and assistance together the best they can. The need for better transitions of care, care coordination, and patient and family engagement in care decisions has finally been recognized as a national health care priority in the United States.42 We need to conduct additional research on appropriate intervention strategies that provide seamless, cost-effective, transitional care with a focus on meeting the needs of caregivers and patients as they move through the stroke recovery trajectory. These strategies will increase the likelihood of caregivers and patients adapting to the life-changing event of stroke and reducing injury, preventing poor health outcomes, and decreasing unnecessary hospitalizations for both patients and their caregivers.
Acknowledgments
We gratefully acknowledge the study participants for sharing their experiences with us, the contract grant sponsor, National Institutes of Health (NIH)/National Institute of Nursing Research, grant number R15NR009800 (PI: Barbara Lutz, PhD, RN), and Dr. Kathleen Jett and Ms. Pam Selby for their careful review of this manuscript. This work was also partially supported by grant 1UL1RR029890 from the National Institute of Research Resources, NIH.
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 2010;121(7):e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.American Heart Association. [Accessed January 22, 2006];Heart Disease and Stroke Statistics—2006 Update. http://www.americanheart.org/downloadable/heart/1105390918119HDSStats2005Update.pdf.
- 3.Dobrez D, Heinemann AW, Deutsch A, Manheim L, Mallinson T. Impact of Medicare’s prospective payment system for inpatient rehabilitation facilities on stroke patient outcomes. Am J Phys Med Rehabil. 2010;89(3):198–204. doi: 10.1097/PHM.0b013e3181c9fb40. [DOI] [PubMed] [Google Scholar]
- 4.O’Brien SR. Trends in inpatient rehablitation stroke outcomes before and after advent of the prospective payment system: a systematic review. J Neurol Phys Ther. 2010;34:17–23. doi: 10.1097/NPT.0b013e3181cfd3ac. [DOI] [PubMed] [Google Scholar]
- 5.Gillen R, Tennen H, McKee T. The impact of the inpatient rehabilitation facility prospective payment system on stroke program outcomes. Am J Phys Med Rehabil. 2007;86(5):356–363. doi: 10.1097/PHM.0b013e31804a7e2f. [DOI] [PubMed] [Google Scholar]
- 6.Schmidt SM, Guo L, Scheer SJ. Changes in the status of hospitalized stroke patients since inception of the prospective payment system in 1983. Arch Phys Med Rehabil. 2002;83(7):894–898. doi: 10.1053/apmr.2002.33219. [DOI] [PubMed] [Google Scholar]
- 7.National Alliance for Caregiving, AARP. [Accessed July 15, 2010];Caregiving in the US. 2009 http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf.
- 8.National Alliance for Caregiving, Evercare. [Accessed July 15, 2010];The Evercare survey of the economic downturn and its impact on family caregiving. 2009 http://www.caregiving.org/data/EVC_Caregivers_Economy_Report%20FINAL_4-28-09.pdf.
- 9.Chumbler NR, Rittman M, Van Puymbroeck M, Vogel WB, Qin H. The sense of coherence, burden, and depressive symptoms in informal caregivers during the first month after stroke. Int J Geriatr Psychiatry. 2004;19(10):944–953. doi: 10.1002/gps.1187. [DOI] [PubMed] [Google Scholar]
- 10.Greenwood N, Mackenzie A, Cloud GC, Wilson N. Informal carers of stroke survivors—factors influencing carers: a systematic review of quantitative studies. Disabil Rehabil. 2008;30(18):1329–1349. doi: 10.1080/09638280701602178. [DOI] [PubMed] [Google Scholar]
- 11.Lutz BJ, Young ME. Rethinking intervention strategies in stroke family caregiving. Rehabil Nurs. 2010;35(4):152–160. doi: 10.1002/j.2048-7940.2010.tb00041.x. [DOI] [PubMed] [Google Scholar]
- 12.Perrin PB, Heesacker M, Hinojosa MS, Uthe CE, Rittman MR. Identifying at-risk, ethnically diverse stroke caregivers for counseling: a longitudinal study of mental health. Rehabil Psychol. 2009;54(2):138–149. doi: 10.1037/a0015964. [DOI] [PubMed] [Google Scholar]
- 13.van Exel NJ, Koopmanschap MA, van den Berg B, Brouwer WB, van den Bos GA. Burden of informal caregiving for stroke patients. Identification of caregivers at risk of adverse health effects. Cerebrovasc Dis. 2005;19(1):11–17. doi: 10.1159/000081906. [DOI] [PubMed] [Google Scholar]
- 14.Talley RC, Crews JE. Framing the public health of caregiving. Am J Public Health. 2007;97(2):224–228. doi: 10.2105/AJPH.2004.059337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brereton L, Nolan M. You do know he’s had a stroke, don’t you?” Preparation for family caregiving—the neglected dimension. J Clin Nurs. 2000;9(4):498–506. doi: 10.1046/j.1365-2702.2000.00396.x. [DOI] [PubMed] [Google Scholar]
- 16.van Exel NJ, Scholte op Reimer WJ, Brouwer WB, van den Berg B, Koopmanschap MA, van den Bos GA. Instruments for assessing the burden of informal caregiving for stroke patients in clinical practice: a comparison of CSI, CRA, SCQ and self-rated burden. Clin Rehabil. 2004;18(2):203–214. doi: 10.1191/0269215504cr723oa. [DOI] [PubMed] [Google Scholar]
- 17.van Exel NJ, Brouwer WB, van den Berg B, Koopmanschap MA, van den Bos GA. What really matters: an inquiry into the relative importance of dimensions of informal caregiver burden. Clin Rehabil. 2004;18(6):683–693. doi: 10.1191/0269215504cr743oa. [DOI] [PubMed] [Google Scholar]
- 18.McCullagh E, Brigstocke G, Donaldson N, Kalra L. Determinants of caregiving burden and quality of life in caregivers of stroke patients. Stroke. 2005;36(10):2181–2186. doi: 10.1161/01.STR.0000181755.23914.53. [DOI] [PubMed] [Google Scholar]
- 19.Shyu YI, Chen MC, Lee HC. Caregiver’s needs as predictors of hospital readmission for the elderly in Taiwan. Soc Sci Med. 2003;58(2004):1395–1403. doi: 10.1016/S0277-9536(03)00334-4. [DOI] [PubMed] [Google Scholar]
- 20.Bowers B, Schatzman L. Dimensional analysis. In: Morse JM, Stern PN, Corbin JM, Charmaz KC, Bowers B, Clarke AE, editors. Developing Grounded Theory: The Second Generation. Walnut Creek, CA: Left Coast Press; 2009. pp. 86–121. [Google Scholar]
- 21.Caron CD, Bowers BJ. Methods and application of dimensional analysis: a contribution to concept and knowledge development in nursing. In: Rodgers BL, Knafl KA, editors. Concept Development in Nursing: Foundatons, Techniques, and Applications. 2. Philadelphia: WB Saunders; 2000. pp. 285–319. [Google Scholar]
- 22.Schatzman L. Dimensional analysis: notes on an alternative approach to the grounding of theory in qualitative research. In: Maines DR, editor. Social Organization and Social Process Essays in Honor of Anselm Strauss. New York: Aldine De Gruyter; 1991. pp. 303–314. [Google Scholar]
- 23.Strauss AL. Qualitative Analysis for Social Scientists. New York: Cambridge University Press; 1987. [Google Scholar]
- 24.Strauss A, Corbin J. Basics of Qualitative Research. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 25.Shalin DN. Pragmatism and social interactionism. Am Sociol Rev. 1986;51:9–29. [Google Scholar]
- 26.NVivo Qualitative Data Analysis Program [computer program] Melbourne, Australia: 2008. Version 8.0. [Google Scholar]
- 27.Dodds TA, Martin DP, Stolov WC, Deyo RA. A validation of the Functional Independence Measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil. 1993;74:531–536. doi: 10.1016/0003-9993(93)90119-u. [DOI] [PubMed] [Google Scholar]
- 28.Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: a new tool for rehabilitation. In: Eisenberg MG, Grezesiak RC, editors. Advances in Clinical Rehabilitation. New York: Springer; 1987. pp. 6–18. [PubMed] [Google Scholar]
- 29.Oczkowski WJ, Barreca S. The functional independence measure: its use to identify rehabilitation needs in stroke survivors. Arch Phys Med Rehabil. 1993;74(12):1291–1294. doi: 10.1016/0003-9993(93)90081-k. [DOI] [PubMed] [Google Scholar]
- 30.Lutz BJ. Determinants of discharge destination for stroke patients. Rehabil Nurs. 2004;29(5):154–163. doi: 10.1002/j.2048-7940.2004.tb00338.x. [DOI] [PubMed] [Google Scholar]
- 31.Palmer S, Glass TA, Palmer JB, Loo S, Wegener ST. Crisis intervention with individuals and their families following stroke: a model for psychosocial service during inpatient rehabilitation. Rehabil Psychol. 2004;49(4):338–343. [Google Scholar]
- 32.Lutz BJ, Chumbler NR, Roland K. Care coordination/home-telehealth for veterans with stroke and their caregivers: addressing an unmet need. Top Stroke Rehabil. 2007;14(2):32–42. doi: 10.1310/tsr1402-32. [DOI] [PubMed] [Google Scholar]
- 33.National Quality Forum. Care Coordination. Washington, DC: Oct, 2010. [Google Scholar]
- 34.National Quality Forum. Preferred Practices and Performance Measures for Measuring and Reporting Care Coordination: A Consensus Report. Washington, DC: NQF; 2010. [Google Scholar]
- 35.Cameron JI, Gignac MA. “Timing It Right”: a conceptual framework for addressing the support needs of family caregivers to stroke survivors from the hospital to the home. Patient Educ Couns. 2008;70(3):305–314. doi: 10.1016/j.pec.2007.10.020. [DOI] [PubMed] [Google Scholar]
- 36.Bakas T, Farran CJ, Austin JK, Given BA, Johnson EA, Williams LS. Stroke caregiver outcomes from the Telephone Assessment and Skill-Building Kit (TASK) Top Stroke Rehabil. 2009;16(2):105–121. doi: 10.1310/tsr1602-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grant JS, Elliott TR, Weaver M, Bartolucci AA, Giger JN. Telephone intervention with family caregivers of stroke survivors after rehabilitation. Stroke. 2002;33(8):2060–2065. doi: 10.1161/01.str.0000020711.38824.e3. [DOI] [PubMed] [Google Scholar]
- 38.Hartke RJ, King RB. Telephone group intervention for older stroke caregivers. Top Stroke Rehabil. 2003;9(4):65–81. doi: 10.1310/RX0A-6E2Y-BU8J-W0VL. [DOI] [PubMed] [Google Scholar]
- 39. [Accessed July 27, 2009];Family Caregiver Alliance: Caregiving National Center on Cargiving. 2008 http://www.caregiver.org/caregiver/jsp/content_node.jsp?nodeid=2313.
- 40.Feinberg LF. The state of the art of caregiver assessment. Generations. 2003;27(4):24–31. [Google Scholar]
- 41.Family Caregiver Alliance. Caregivers Count Too! A Toolkit to Help Practitioners Assess the Needs of Family Caregivers. San Francisco: Author; 2006. [Google Scholar]
- 42.National Quality Forum. [Accessed November 25, 2010];Addressing national priorities. 2010 http://www.qualityforum.org/Setting_Priorities/Addressing_National_Priorities.aspx.