Abstract
Hydrogen sulfide (H2S) and nitric oxide (NO) are major gasotransmitters produced in endothelial cells (ECs), contributing to the regulation of vascular contractility and structural integrity. Their interaction at different levels would have a profound impact on angiogenesis. Here, we showed that H2S and NO stimulated the formation of new microvessels. Incubation of human umbilical vein endothelial cells (HUVECs-926) with NaHS (a H2S donor) stimulated the phosphorylation of endothelial NO synthase (eNOS) and enhanced NO production. H2S had little effect on eNOS protein expression in ECs. L-cysteine, a precursor of H2S, stimulated NO production whereas blockage of the activity of H2S-generating enzyme, cystathionine gamma-lyase (CSE), inhibited this action. CSE knockdown inhibited, but CSE overexpression increased, NO production as well as EC proliferation. LY294002 (Akt/PI3-K inhibitor) or SB203580 (p38 MAPK inhibitor) abolished the effects of H2S on eNOS phosphorylation, NO production, cell proliferation and tube formation. Blockade of NO production by eNOS-specific siRNA or nitro-L-arginine methyl ester (L-NAME) reversed, but eNOS overexpression potentiated, the proliferative effect of H2S on ECs. Our results suggest that H2S stimulates the phosphorylation of eNOS through a p38 MAPK and Akt-dependent pathway, thus increasing NO production in ECs and vascular tissues and contributing to H2S-induced angiogenesis.
Keywords: Hydrogen sulfide, Nitric oxide, Endothelial cells, eNOS, CSE, Cystathionine gamma-lyase
Introduction
Hydrogen sulfide and NO are known gasotransmitters that contribute to many physiological functions 1. These gaseous messengers can be produced endogenously to respond to diverse physiological and pathophysiological stimuli 1. In ECs, H2S can be generated from L-cysteine by the enzymatic action of CSE (EC 4.4.1.22) 2. Hydrogen sulfide-induced relaxation of vascular tissue was partially reduced by the removal of the vascular endothelium or in the presence of L-NAME (an inhibitor of NO synthase) 3. Nitric oxide can be generated in ECs from L-arginine by eNOS (EC 1.14.13.39) 4. Being a homodimeric protein, the activation of eNOS is dependent on intracellular calcium (Ca2+) level and other cofactors like nicotinamide adenine dinucleotide phosphate (NADPH), tetrahydrobiopterin (BH4), flavin adenine dinucleotide (FAD) and flavin mononucleotide (FMN) 5. The activity of eNOS is affected by many post-translational modification mechanisms, such as phosphorylation on multiple amino acids like Ser-1179/1177 (bovine/human) and Thr-495 residues 6, 7, whereas eNOS protein can be self-inhibited by high concentrations of NO through S-nitrosylation 8. Due to its reducing capability, H2S may reduce NO to form a thiol-sensitive molecule S-nitrothiols (RSNO) 9. Conversely, H2S has been found to reduce RSNO to release NO from GSNO (S-Nitrosoglutathione) 10. Moreover, H2S and NO interact on each other's catalysing enzymes; NO donor increases the expression and activity of CSE in cultured aortic smooth muscle cells (SMCs) 3. In rat vascular SMCs, H2S had no direct effect on NO production, but it augmented interleukin-induced NO production, and this effect was related to increased iNOS expression (inducible NOS) 11. NaHS (a H2S donor) treatment reduced eNOS activity and expression but not of nNOS (neuronal NOS) and iNOS in isolated rat aortas and HUVECs 12. NaHS inhibited eNOS-catalysed conversion of [3H]-arginine to [3H]-citrulline 13. NaHS also inhibited iNOS expression and NO production in macrophage cells (RAW264.7) 14. Na2S selectively augmented NO production in chronically ischaemic tissues, by influencing iNOS and nNOS expression and stimulating nitrite reduction to NO via xanthine oxidase (XO) under hypoxic condition 15.
The angiogenic crosstalk between H2S and NO in ECs has been unclear. Our present study showed that the pro-angiogenic effect of H2S appears to be regulated by both a NO-dependent and an independent mechanism, whereas NO effect on angiogenesis is partially dependent on H2S. We demonstrated that H2S stimulated NO release by increasing eNOS phosphorylation via a p38 MAPK and Akt-dependent mechanism, which contributes to the stimulatory effect of H2S on EC proliferation and angiogenesis.
Materials and methods
Cell culture and chemicals
Human umbilical vein endothelial cells-derived EA.hy 926 cells were kindly provided by Dr. Cora-Jean S. Edgell 16 (University of North Carolina, USA). The cells were cultured in Dulbecco's modified eagles medium (DMEM) without ferric nitrate (Sigma-Aldrich, Oakville, ON, Canada), containing penicillin (100 U/ml), streptomycin (100 μg/ml) and 10% (v/v) foetal bovine serum. The primary aortic ECs were isolated from the aorta of 10- to 12-week-old C57BL/6J/129 mice, as previously described 17. Aortic ECs were cultured in a medium containing 20% FBS, 100 U/ml penicillin-G, 100 μg/ml streptomycin, 2 mM L-glutamine, 25 mM HEPES (pH 7-7.6), 100 μg/ml heparin, 100 μg/ml endothelial cell growth supplement (ECGS) and DMEM (Sigma-Aldrich). The nature of ECs was confirmed using endothelial-specific markers CD31 (Santa Cruz Biotechnology, Santa Cruz, CA, USA) and eNOS (Cell Signaling Technologies, Beverly, MA, USA) by Western blot, and endothelial tube formation using Matrigel assay (BD Biosciences, Mississauga, ON, Canada; data not shown). The culture medium was changed every 2 days and ECs between passages 3 and 5 were used.
Measurement of NO production
Total nitrate/nitrite concentrations were measured by conversion of nitrate to nitrite after incubating supernatants with nitrate reductase (10 U/ml) and NADPH (5 mM) for 1 hr at 37°C. The total nitrite was measured with a Griess assay kit (Promega, Madison, WI, USA) using a reference sodium nitrate standard curve 18. The results obtained with the Griess assay have also been validated by the diaminofluorescein fluorophore system (DAF-FM), which can be deacetylated by intracellular esterases and further reacts with NO to form a fluorescent benzotriazole (DAF fluorescence; Invitrogen, Burlington, ON, Canada). Endothelial cells were incubated with 5 μM DAF-FM for 30 min. at 37°C. The cells were washed to remove excess dye, replaced with fresh medium and observed under a fluorescent microscope as previously described 19. To detect the production of NO in aortic tissues, isolated aortas were incubated with DAF-FM (5 μM) at 37°C in Kreb's buffer and then rapidly removed and frozen at −20°C. Aortic tissue samples were embedded in optimal cutting temperature (OCT) compound until frozen, and sectioned using Leica CM1850 UV microtome-cryostat (Leica Biosystems, Concord, ON, Canada). The tissue blocks were cut into 10-μm thick sections and observed under a fluorescent microscope 20.
Gene knockdown and overexpression
Endothelial cells were seeded in 6-well plates and cultured until they reached 70–80% confluence. The cells were then transfected with specific siRNA to knockdown CSE or eNOS gene (50 nM). Negative siRNA was used as transfection control (50 nM), using Lipofectamine™ RNAi-MAX transfection reagent according to the manufacturer's instruction (Invitrogen). Overexpression experiments were carried out with plasmid DNA containing CSE cDNA (pIRES2-EGFP, 4.0 μg) or eNOS cDNA (pcDNA 3.1 eNOS-GFP, 4.0 μg). Mock empty vector was used as transfection control (Addgene, Cambridge, MA, USA) 21–23 using Lipofectamine™ 2000. Forty-eight hours after transfection, the cells or media were collected and evaluated by Western blot or Griess assay analysis.
Western blot analysis
Cultured cells were collected and incubated in a lysis buffer containing 0.5 M EDTA, 1 M Tris-Cl (pH 7.4), 0.3 M sucrose and a protease inhibitors mixture (Sigma-Aldrich). The cell extracts were sonicated three times (5–10 sec./each) on ice using a cell sonicator (Sonic Dismemrator Model 100, Fisher Scientific, Ottawa, ON, Canada) 23. Cellular extracts were separated by centrifugation at 14,000 × g for 15 min. at 4°C. Supernatants were collected, and the same amounts of proteins were separated on 10% SDS-polyacrylamide gels and blotted onto nitrocellulose membranes (Pall Corporation, Pensacola, FL, USA). All primary antibody incubations were performed at 4°C overnight. The antibody dilution for phospho-eNOS (Ser1177), eNOS, phospho-ERK, ERK, phospho-p38 MAPK, p38 MAPK, phospho-Akt (S473) and Akt was at 1:1000 (Cell Signaling Technologies). Anti-CSE antibody was used at 1:5000 (Proteintech Group, Chicago, IL, USA), and anti-β-actin antibody was at 1:10000 (Sigma-Aldrich). The membranes were stripped using a buffer containing 100 mM β-mercaptoethanol, 2% SDS and 62.5 mM Tris-HCl (pH 6.8) at 50°C for 30 min. Membranes were visualized using enhanced chemiluminescence Western blotting system (GE Healthcare, Piscataway, NJ, USA). Densitometric quantification was performed using Alpha Digi Doctor Software (Richardson, TX, USA). The protein bands were quantified and normalized against either β-actin or total form levels of the target protein, and expressed as a percentage relative to the controls (equals 100%). The phosphorylation level is defined as the ratio between the phosphorylated target proteins and their total forms and expressed in the summarized bar graphs as the percentage of the untreated controls.
Capillary-like tube formation assay
The Matrigel matrix gel was thawed overnight at 4°C on ice and then added to pre-chilled culture dishes and allowed to polymerize at 37°C for 1 hr. Endothelial cells (2 × 104 cells) were incubated with different agents in 500 μl DMEM and then seeded onto the surface of Matrigel (BD Biosciences). After 12 hrs, the formation of capillary-like structure was imaged by light microscope. The total lengths of tube-like structures per field were measured using image analysis software (NIH Image software- Image J).
Cell proliferation assay
Cells were counted using automated cell counter TC10™ from BioRad (Mississauga, ON, Canada) and seeded into 96-well plates (1 × 104 cells/well). After 24 hrs of initial seeding, cells were incubated with DMEM serum-free medium for overnight 23. The proliferation rates were evaluated by 5-bromo-2′-deoxyuridine (BrdU) incorporation assay according to the manufacturer's instructions (EMD Biosciences, San Diego, CA, USA).
Microvessel formation assay
Cystathionine gamma-lyase knockout (KO) mice were generated as described previously 2. Eight-week-old male CSE-KO and wild-type (WT) mice were sacrificed, and aorta were rapidly cleaned off adipose tissues and blood. Aorta were cut into rings (length, ∼3 mm) and implanted in a fibrin gel obtained by adding 400 μl of a fibrinogen solution (3 mg/ml) and thrombin (1.5 U/ml); (Sigma-Aldrich). The fibrin gels were given 30 minutes to solidify before different treatments were applied. As a control, the effect of medium alone was assayed, and quantitative evaluation of new microvessels was carried out after 72 hrs 24. All animal experiments were conducted according to the Care and Use of Laboratory Animals Guide (NIH Publication No. 85-23, revised 1996) and approved by Lakehead University Animal Care Committee, Canada.
Statistical analysis
All data were expressed as mean ± SEM. Each data point represented at least three to four independent experiments. Statistical comparisons were evaluated using Student's t-test. Values of P < 0.05 were considered statistically significant.
Results
H2S-induced NO production in ECs
Stimulation of ECs with NaHS for 30 min. increased NO production over a concentration range from 10 to 100 μM (Fig. 1A). The effect of NaHS on NO production was blocked when cells were pre-treated with NOS inhibitor Nω-L-NAME (Fig. 1B). NaHS-induced increase in NO production was further confirmed in primarily cultured mouse ECs (Figure S1). Nitro-L-arginine methyl ester treatment also significantly reduced NO production. We next determined the effect of L-cysteine (H2S precursor) on NO production. L-cysteine pre-treatment stimulated NO production in ECs (Fig. 1B). However, blocking of CSE activity by PPG reversed L-cysteine effect (Fig. 1B). Cystathionine gamma-lyase knockdown using CSE-specific siRNA significantly reduced CSE protein level and attenuated NO production in comparison with the cells transfected with negative siRNA. Moreover, CSE overexpression significantly elevated CSE expression level and resulted in an increase in NO level (Fig. 1C and D). Nitric oxide data was further confirmed by DAF-FM fluorescence dye showing that NaHS treatment stimulated NO release in aortic tissues and ECs (Fig. 1E and F).
Fig. 1.
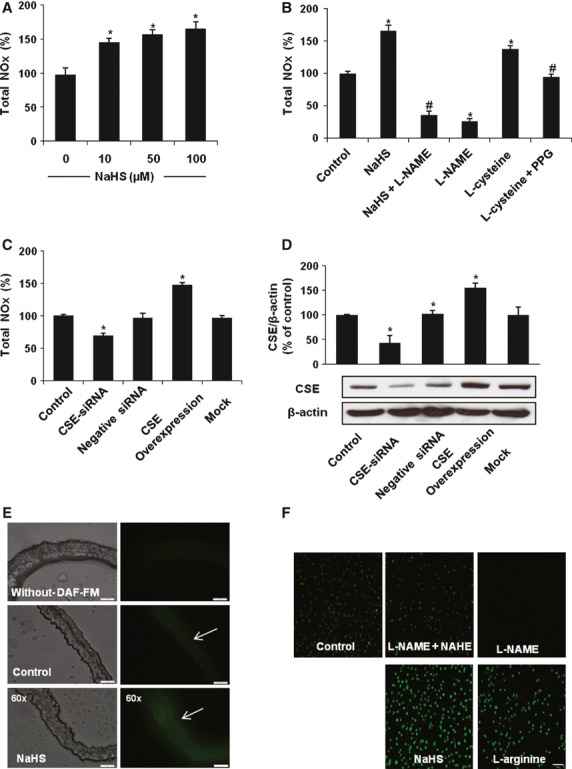
H2S stimulated NO production in endothelial cells (ECs) and aortic tissues. (A) The effect of NaHS on NO production in ECs detected by Griess assay, n = 4, *P < 0.05 versus control. (B) The effects of NO synthase (NOS) inhibitor L-NAME (200 μM, 1 hr), cystathionine gamma-lyase (CSE) inhibitor PPG (10 mM, 4 hrs), NaHS (100 μM, 30 min) and L-cysteine (6 mM, 30 min.) on NO production detected by the Griess assay, n = 3–4, *P < 0.05 versus control, #P < 0.05 versus NaHS or L-cysteine-treated groups. (C) The effects of CSE knockdown or overexpression on NO production assessed by the Griess assay. (D) The efficiency of CSE knockdown or overexpression, determined by Western blot, n = 3–4, *P < 0.05 versus control. The effect of NaHS (100 μM) and L-arginine (1 mM) treatment on NO production in isolated aortic tissues (scale bar: 50 μm) (E) and cultured ECs (F) using diaminofluorescein fluorophore system (DAF-FM) fluorescent probe (scale bar: 200 μm), n = 3–4.
NaHS (50 and 100 μM) treatment markedly increased the phosphorylation of eNOS in ECs (Fig. 2A). The stimulatory effect of NaHS on eNOS phosphorylation was time dependent, and the increase in phosphorylated eNOS appeared at 10 min., peaked at 30 min., and gradually declined to baseline over the period of 1-hr NaHS exposure (Fig. 2B). NaHS treatment up to 36 hrs had no significant effect on eNOS expression level (Fig. 2C).
Fig. 2.
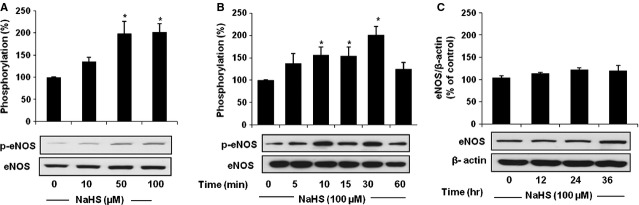
H2S stimulated the phosphorylation of endothelial NO synthase (eNOS) in endothelial cells (ECs). (A) The effect of NaHS treatment on eNOS phosphorylation. ECs were starved in Dulbecco's modified eagles medium (DMEM) medium free of serum for 24 hrs and treated with different concentrations of NaHS for 30 min. Western blot analysis was conducted using anti-phospho-eNOS and anti-total eNOS antibody, n = 3–4, *P < 0.05 versus control. (B) Time-dependent effect of NaHS treatment on the phosphorylation of eNOS. ECs were treated with NaHS (100 μM) for different periods (0–60 min.). At the end of each time-point, cells were collected and proteins lysates were analysed by Western blot, n = 3–4, *P < 0.05 versus control. (C) The effect of NaHS treatment on eNOS expression level in ECs. The ECs were treated with NaHS (100 μM) for 12–36 hrs, and then cells were collected and proteins were subjected to Western blot analysis. n = 3–4, *P < 0.05 versus control.
The role of p38 MAPK/Akt in H2S-induced eNOS phosphorylation and NO production
Diverse kinases such as Akt, p38-MAPK kinase and ERK are important for NO production and signalling activation 25–27. To elucidate the signalling pathways involved in H2S-induced eNOS phosphorylation and the NO production, we examined the roles of Akt, ERK and p38 MAPK in H2S-stimulated NO production. Treatment with NaHS at 100 μM enhanced the phosphorylation of p38 MAPK, Akt and ERK to different levels (Fig. 3). SB202190 (a p38 MAPK inhibitor) and LY294002 (a PI3K/Akt inhibitor), but not U0126 (an inhibitor of ERK), significantly reduced H2S-induced phosphorylation of eNOS (Fig. 4). We further found that the stimulatory effect of NaHS on NO production was decreased by the same treatments (SB202190 or LY294002), and neither SB202190 nor LY294002 alone had any detectable effect on NO production (Fig. 5A). In addition, p38 MAPK inhibition by SB202190 attenuated the NaHS-induced phosphorylation of Akt (Fig. 5B), indicating that p38 MAPK might regulate the upstream signalling cascade that leads to Akt activation. These results suggest that p38 MAPK and Akt are required for NO activation by H2S.
Fig. 3.
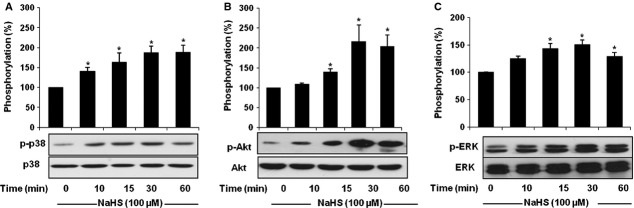
H2S-induced phosphorylation of p38 MAPK, Akt and ERK. Endothelial cells (ECs) were treated with NaHS (100 μM) for different times (0–60 min.). At the end of each time-point, cells were collected and proteins lysates were analysed by Western blot, using antibodies specific for the phosphorylated and total forms of (A) p38 MAPK, (B) Akt, and (C) ERK. Data were normalized to total protein level, n = 3–4, *P < 0.05 versus control.
Fig. 4.
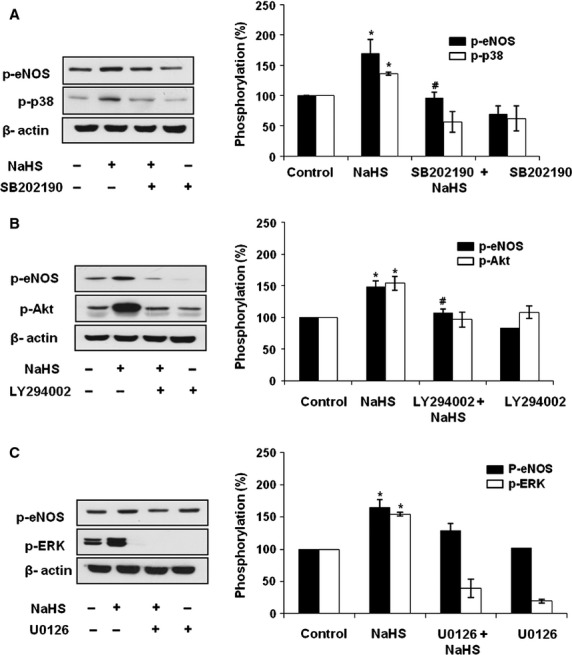
H2S-stimulated endothelial NO synthase (eNOS) phosphorylation is dependent on p38 MAPK and Akt. Endothelial cells (ECs) were pre-treated with (A) SB203580 (10 μM), (B) LY294002 (10 μM), and (C) U0126 (10 μM) for 1 hr and then treated with NaHS (100 μM) for 30 min. Cell lysates were harvested and the level of phosphorylated forms of p38 MAPK, Akt, ERK and eNOS were measured by Western blot. n = 3, *P < 0.05 versus control, #P < 0.05 versus NaHS-treated group.
Fig. 5.
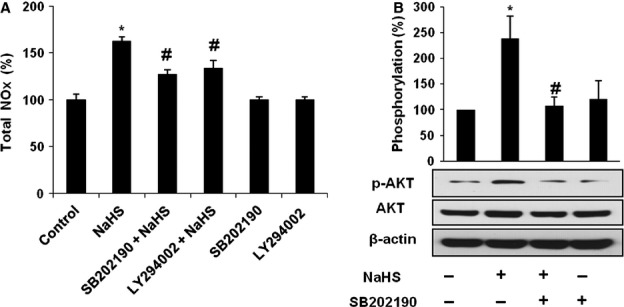
Crosstalk between p38 MAPK and Akt in H2S-induced NO production. The p38 MAPK inhibitor inhibited Akt and NO production induced by H2S. (A) Endothelial cells (ECs) were pre-treated with either SB203580 (10 μM) or LY294002 (10 μM) for 1 hr, and then treated with NaHS (100 μM) for 30 min. At the indicated time-point, the NOx generation was assessed by Griess assay, n = 3–4, *P < 0.05 versus control, #P < 0.05 versus NaHS. (B) The phosphorylated Akt was measured by Western blot after pre-treatment with SB203580 (10 μM) for 1 hr and NaHS (100 μM) treatment for 30 min., *P < 0.05 versus control, n = 3–4.
The role of NO in H2S-induced EC proliferation and angiogenesis
NaHS significantly induced EC proliferation (Fig. 6A). To show the effect of endogenously produced H2S, CSE knockdown with a siRNA approach attenuated cell proliferation. The knockdown of CSE significantly attenuated the proliferation of EC by about 25% compared with the control group (Fig. 6B). We also found that CSE knockdown significantly decreased, but NaHS induced a similar and comparable increase, in the proliferation of primarily cultured mouse ECs (Figure S2). The CSE overexpression stimulated EC proliferation (Fig. 6B). Next, we study the effect of NO on proliferation. The overexpression of eNOS stimulated cell proliferation, which was strengthened by NaHS treatment (Fig. 6C and D).
Fig. 6.
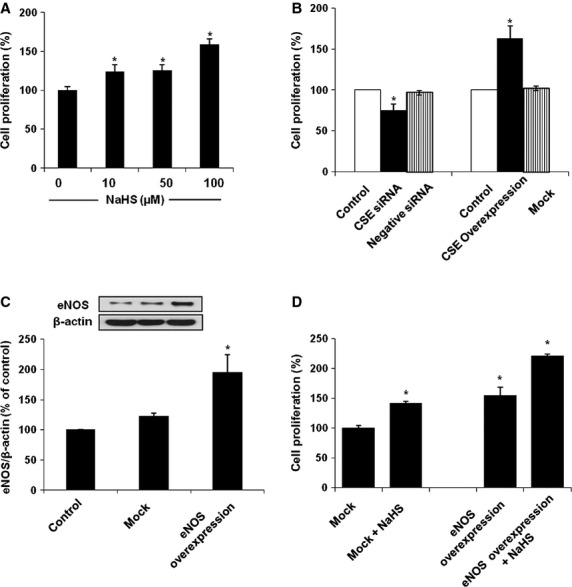
H2S-stimulated endothelial cell (EC) proliferation. (A) The effects of NaHS treatment on EC proliferation assessed using BrdU proliferation assay. n = 3, *P < 0.05 versus control. (B) The effects of cystathionine gamma-lyase (CSE) knockdown or overexpression on EC proliferation. n = 3, *P < 0.05 versus control. (C) The efficiency of endothelial NO synthase (eNOS) overexpression in ECs detected by Western blot, n = 3, *P < 0.05 versus Mock. (D) The effect of eNOS overexpression on EC proliferation. n = 3, *P < 0.05 versus Mock.
We then determined whether H2S and NO can interact to regulate angiogenesis. Hydrogen sulfide-induced EC proliferation was attenuated by eNOS knockdown (Fig. 7A and B), whereas treatment with NO precursor L-arginine (1 mM) or NaHS (100 μM) alone significantly increased EC proliferation (Fig. 7B). Furthermore, NaHS (100 μM) treatment significantly increased the capillary-like tube formation of EC compared with the untreated cells (Fig. 7C). NaHS-induced increase in tube formation was significantly attenuated by co-treatment with L-NAME (200 μM), whereas L-NAME treatment alone had no significant effect on tube formation (Fig. 7C). The aortic tissues from CSE-KO mice showed a markedly decreased formation of new microvessels compared with WT mice. After treating the embedded aortic rings with NaHS, the sporting of vascular neogenesis was significantly increased in both CSE-KO and WT mice with markedly higher levels in CSE-KO mice (Fig. 7D). Similar to the effect of NaHS, L-arginine (a NO precursor) stimulated vascular neogenesis in both CSE-KO and WT mice (Fig. 7D). Furthermore, the pro-angiogenic effects of H2S on aortic rings from both CSE-KO and WT mice were inhibited by L-NAME treatment (Fig. 7D). Nitro-L-arginine methyl ester treatment inhibited new vessel formation from WT aortic rings, but not that from CSE-KO aortic rings (Fig. 7D). Treatment of EC with NaHS (100 μM) increased the capillary-like tube formation, and co-treatment with a p38 or Akt inhibitor (SB202190 or LY294002) significantly reduced the H2S effect (Fig. 7E). However, treatment of EC with LY294002 or SB202190 alone had no significant effect on tube formation (Fig. 7E). LY294002 or SB202190 blocked the proliferation induced by H2S, and neither LY294002 nor SB202190 alone had any detectable effect (Fig. 7F), demonstrating that p38 MAPK and Akt are responsible for H2S-induced EC proliferation and angiogenesis.
Fig. 7.
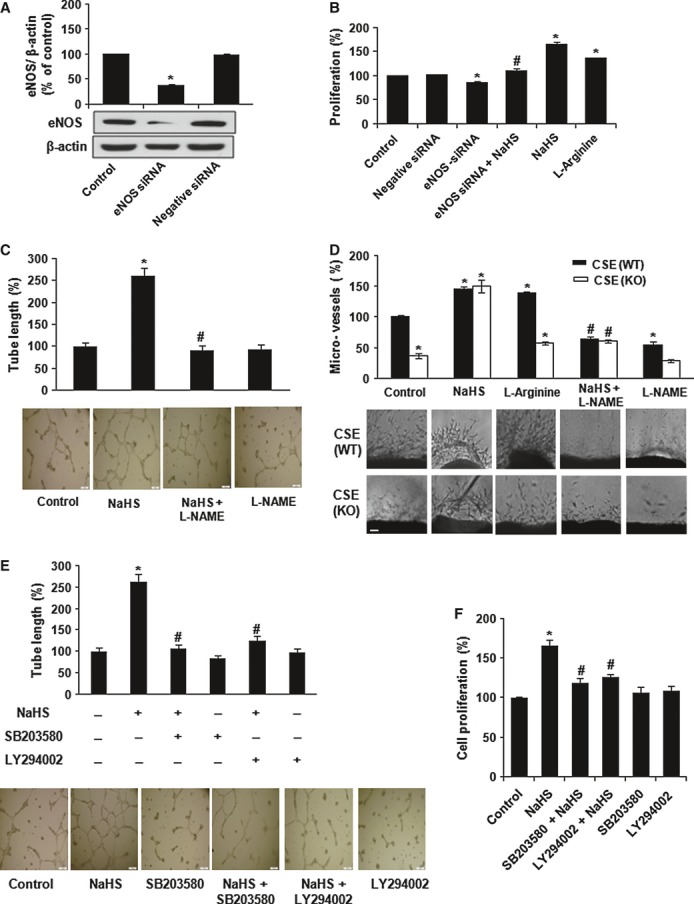
H2S interacts with NO to stimulate endothelial cell (EC) proliferation and angiogenesis. (A) The efficiency of endothelial NO synthase (eNOS) knockdown transfection in EC detected by Western blot. n = 3-4, *P < 0.05 versus control. (B) The effects of eNOS-knockdown (eNOS siRNA, 50 nM), NaHS (100 μM), and L-arginine (1 mM) treatments on EC proliferation evaluated by BrdU assay. n = 3-4, *P < 0.05 versus control, #P < 0.05 versus NaHS-treated group. (C) H2S-NO interaction on EC tube formation. The effects of NaHS (100 μM) and L-NAME (200 μM) on tube formation of ECs (Scale Bar: 500 μm). (D) The effects of L-NAME (200 μM), L-arginine (1 mM) and NaHS (100 μM) on angiogenesis (scale bar: 200 μm), n = 3–4 mice for each group, *P < 0.05 versus control, #P < 0.05 versus NaHS-treated group. (E) The involvements of p38 MAPK and Akt in EC proliferation and tube formation. ECs were pre-treated with p38 MAPK inhibitor SB202190 (10 μM) and Akt inhibitor LY294002 (10 μM) for 1 hr, and treated with NaHS (100 μM) for 30 min. Cells (2 × 104 cells) were seeded on Martigel for 12 hrs to assist the formation of capillary-like structure (scale bar, 500 μm). (F) Cells were pre-treated with LY294002 or SB202190 and NaHS. The cells were cultured for 24 hrs for measurement of proliferation rate using BrdU proliferation assay. n = 3–4, *P < 0.05 versus control.
Discussion
Gasotransmitters play important roles in angiogenesis 28–30. Angiogenesis is important for the development of the cardiovascular system and sustaining blood supplies, wound healing and fetus development 31–35. In our present study, we found that H2S can interact with NO to induce angiogenesis of both cloned EC line and freshly isolated primary mouse ECs. The mechanisms for H2S action are mainly ascribed to the stimulation of the p38 MAPK/Akt and eNOS phosphorylation, which was followed by increased NO production.
Phosphorylation activates eNOS 30. In our study, the phosphorylation of p38 MAPK precedes the phosphorylation of Akt in the H2S signalling cascade, which was confirmed when inhibition of p38 MAPK abolished H2S-induced phosphorylation of Akt. We also found that H2S activated ERK phosphorylation with a time course similar to that for p38 MAPK activation. However, the inhibition of ERK did not affect H2S-stimulated NO production. By altering the phosphorylation of eNOS, H2S regulated NO production in ECs. Our observation is consistent with another recent finding by Predmore et al. 36 who demonstrated that Na2S (150 μM) treatment stimulated NO production in bovine arterial ECs. While these authors illustrated the H2S-dependent Akt mechanism that stimulates NO production, the involvement of other kinases, like p38 MAPK, or the synergistic partnership between H2S and NO in angiogenesis were not addressed. Conversely, it has been reported that a high concentration of NaHS (300–3000 μM) significantly inhibited the activity of recombinant bovine eNOS 13. It is worthy noted here that NaHS at this high concentration range unlikely bears physiological relevance.
We explored the possible interaction between H2S and NO in angiogenesis regulation. Ex vivo aortic explants isolated from CSE-KO mice showed a remarkable decrease in vascular neogenesis when compared to WT mice. L-arginine treatment stimulated angiogenesis in the WT mice and to a lesser extent, in the CSE-KO mice. On the other hand, L-NAME treatment reduced new vessel formation in WT mice, and this inhibitory effect was not significant in CSE-KO mice, suggesting that the angiogenic effect of NO might be mediated through H2S biosynthesis. Cystathionine gamma-lyase overexpression stimulated EC proliferation, whereas CSE knockdown reversed this effect. Interestingly, we found that the pro-angiogenic effect of H2S was partially attenuated in the presence of eNOS inhibitor L-NAME, or after eNOS knockdown using siRNA. Taken together, our results suggest that both gasotransmitters are required for optimal angiogenic activity, yet angiogenesis still proceeds in the presence of either H2S or NO alone albeit to a reduced degree. Previous studies had reported that H2S and NO can mediate angiogenesis without much knowledge about the H2S–NO interaction on angiogenesis 24, 37. Recently, one study reported that a mutually dependent relationship between H2S and NO is important for physiological control of different vascular function 38. Our study used different angiogenesis model (CSE-KO mice versus rat) and experimental conditions, and we found that H2S and NO, alone or combined, can cause angiogenesis. Hydrogen sulfide-stimulated angiogenesis was partially but not completely inhibited by NO blockage, whereas in CSE-KO mice, NO treatment stimulated angiogenesis but to a reduced level. The exact molecular mechanism underlying H2S-mediated NO pro-angiogenic response is not clear.
In summary, our studies demonstrate that H2S promotes NO production in ECs via the activation of a cascade of phosphorylation events, starting from p38 MAPK, Akt to eNOS. Hydrogen sulfide promotes EC tube formation, proliferation and angiogenesis by NO-dependent and independent mechanisms as outlined in Figure 8. Thus, H2S may be a key regulator for angiogenic signalling pathways, whether they required NO or not. The elucidation of the H2S–NO relationship in the vascular biology would improve our understanding of the pathogenic mechanisms for cardiovascular disease in general and angiogenic-related diseases in particular.
Fig. 8.
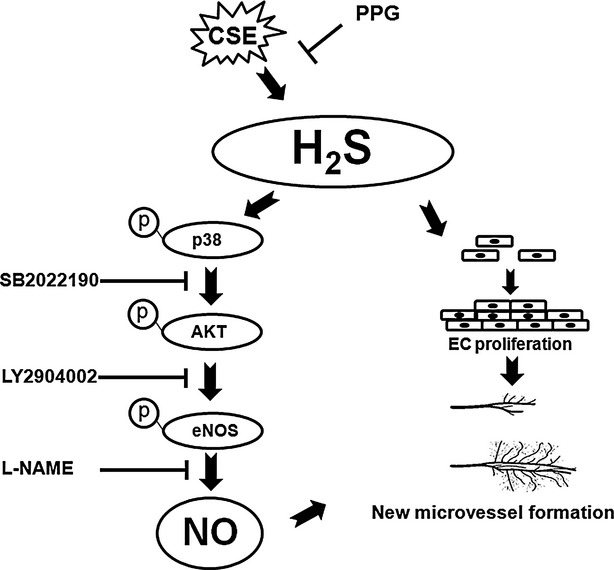
Schematic representation of proposed pathways of H2S-induced NO production and angiogenesis.
Acknowledgments
This study has been supported by an operating grant from Canadian Institutes of Health Research to RW. GY is a New Investigator award recipient from Heart and Stroke Foundation of Canada.
Conflict of interest
There is no conflict of interest of any kind with any of the authors.
Supporting information
Additional Supporting Information may be found in the online version of this article:
Figure S1 The effect of H2S on NO production in primarily cultured mouse aortic endothelial cells. (A) The effects of CSE siRNA knockdown and NaHS treatment on NO production detected by Griess assay, n = 3, *P < 0.05 versus control, #P < 0.05 versus NaHS-treated group. (B) The effects of NaHS and L-NAME treatment on NO production detected by diaminofluorescein diacetate–based probes (DAF-FM), scale bars: 200 μm.
Figure S2 The pro-proliferative effects of H2S and NO on primarily cultured mouse aortic endothelial cells. (A) The effects of CSE siRNA, eNOS siRNA and NaHS treatments on EC proliferation assessed using BrdU proliferation assay, n = 3, *P < 0.05 versus control, #P < 0.05 versus NaHS-treated group (B) The efficiency of CSE siRNA and eNOS siRNA in ECs detected by Western blot.
References
- 1.Wang R. Two's company, three's a crowd – Can H2S be the third endogenous gaseous transmitter? FASEB J. 2002;13:1792–8. doi: 10.1096/fj.02-0211hyp. [DOI] [PubMed] [Google Scholar]
- 2.Yang G, Wu L, Jiang B, et al. H2S as a physiologic vasorelaxant: hypertension in mice with deletion of cystathionine gamma-lyase. Science. 2008;322:587–90. doi: 10.1126/science.1162667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhao W, Zhang J, Lu Y, et al. The vasorelaxant effect of H2S as a novel endogenous gaseous KATP channel opener. EMBO J. 2001;20:6008–16. doi: 10.1093/emboj/20.21.6008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murad F. Cellular signaling with nitric oxide and cyclic GMP. Braz J Med Biol Res. 1999;32:1317–27. doi: 10.1590/s0100-879x1999001100001. [DOI] [PubMed] [Google Scholar]
- 5.Klatt P, Schmidt K, Uray G, et al. Multiple catalytic functions of brain nitric oxide synthase. Biochemical characterization, cofactor-requirement, and the role of N omega-hydroxy-L-arginine as an intermediate. J Biol Chem. 1993;268:14781–7. [PubMed] [Google Scholar]
- 6.Boo YC, Sorescu G, Boyd N, et al. Shear stress stimulates phosphorylation of endothelial nitric-oxide synthase at Ser1179 by Akt-independent mechanisms: role of protein kinase A. J Biol Chem. 2002;277:3388–96. doi: 10.1074/jbc.M108789200. [DOI] [PubMed] [Google Scholar]
- 7.Lin MI, Fulton D, Babbitt R, et al. Phosphorylation of threonine 497 in endothelial nitric-oxide synthase coordinates the coupling of L-arginine metabolism to efficient nitric oxide production. J Biol Chem. 2003;278:44719–26. doi: 10.1074/jbc.M302836200. [DOI] [PubMed] [Google Scholar]
- 8.Ravi K, Brennan AL, Levic S, et al. S-nitrosylation of endothelial nitric oxide synthase is associated with monomerization and decreased enzyme activity. Proc Natl Acad Sci USA. 2004;24:2619–24. doi: 10.1073/pnas.0300464101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whiteman M, Li L, Kostetski I, et al. Evidence for the formation of a novel nitrosothiol from the gaseous mediators nitric oxide and hydrogen sulphide. Biochem Biophys Res Commun. 2006;343:303–10. doi: 10.1016/j.bbrc.2006.02.154. [DOI] [PubMed] [Google Scholar]
- 10.Teng X, Isbell TS, Crawford JH, et al. Novel method for measuring S-nitrosothiols using hydrogen sulfide. Methods Enzymol. 2008;441:161–72. doi: 10.1016/S0076-6879(08)01209-3. [DOI] [PubMed] [Google Scholar]
- 11.Jeong SO, Pae HO, Oh GS, et al. Hydrogen sulfide potentiates interleukin-1beta-induced nitric oxide production via enhancement of extracellular signal-regulated kinase activation in rat vascular smooth muscle cells. Biochem Biophys Res Commun. 2006;345:938–44. doi: 10.1016/j.bbrc.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 12.Geng B, Cui Y, Zhao J, et al. Hydrogen sulfide downregulates the aortic L-arginine/nitric oxide pathway in rats. Am J Physiol Regul Integr Comp Physiol. 2007;293:1608–18. doi: 10.1152/ajpregu.00207.2006. [DOI] [PubMed] [Google Scholar]
- 13.Kubo S, Doe I, Kurokawa Y, et al. Direct inhibition of endothelial nitric oxide synthase by hydrogen sulfide: contribution to dual modulation of vascular tension. Toxicology. 2007;232:138–46. doi: 10.1016/j.tox.2006.12.023. [DOI] [PubMed] [Google Scholar]
- 14.Oh GS, Pae HO, Lee BS, et al. Hydrogen sulfide inhibits nitric oxide production and nuclear factor-kappaB via heme oxygenase-1 expression in RAW264.7 macrophages stimulated with lipopolysaccharide. Free Radic Biol Med. 2006;41:106–19. doi: 10.1016/j.freeradbiomed.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 15.Bir SC, Kolluru GK, McCarthy P, et al. Hydrogen sulfide stimulates ischemic vascular remodeling through nitric oxide synthase and nitrite reduction activity regulating hypoxia-inducible factor-1α and vascular endothelial growth factor–dependent angiogenesis. J Am Heart Assoc. 2012;1:e004093. doi: 10.1161/JAHA.112.004093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Edgell CJ, McDonald CC, Graham JB. Permanent cell line expressing human factor VIII-related antigen established by hybridization. Proc Natl Acad Sci USA. 1983;80:3734–7. doi: 10.1073/pnas.80.12.3734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kobayashi M, Inoue K, Warabi E, et al. A simple method of isolating mouse aortic endothelial cells. J Atheroscler Thromb. 2005;12:138–42. doi: 10.5551/jat.12.138. [DOI] [PubMed] [Google Scholar]
- 18.Babaei S, Teichert-Kuliszewska K, Monge JC, et al. Role of nitric oxide in the angiogenic response in vitro to basic fibroblast growth factor. Circ Res. 1998;82:1007–15. doi: 10.1161/01.res.82.9.1007. [DOI] [PubMed] [Google Scholar]
- 19.Choi YS, Choi HJ, Min JK, et al. Interleukin-33 induces angiogenesis and vascular permeability through ST2/TRAF6-mediated endothelial nitric oxide production. Blood. 2009;114:3117–26. doi: 10.1182/blood-2009-02-203372. [DOI] [PubMed] [Google Scholar]
- 20.Wang X, Chang T, Jiang B, et al. Attenuation of hypertension development by aminoguanidine in spontaneously hypertensive rats: role of methylglyoxal. Am J Hypertens. 2007;20:629–36. doi: 10.1016/j.amjhyper.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 21.Fulton D, Gratton JP, McCabe TJ, et al. Regulation of endothelium-derived nitric oxide production by the protein kinase Akt. Nature. 1999;399:597–601. doi: 10.1038/21218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sowa G, Liu J, Papapetropoulos A, et al. Trafficking of endothelial nitric-oxide synthase in living cells. Quantitative evidence supporting the role of palmitoylation as a kinetic trapping mechanism limiting membrane diffusion. J Biol Chem. 1990;274:22524–31. doi: 10.1074/jbc.274.32.22524. [DOI] [PubMed] [Google Scholar]
- 23.Yang G, Wu L, Bryan S, et al. Cystathionine gamma-lyase deficiency and overproliferation of smooth muscle cells. Cardiovasc Res. 2010;86:487–95. doi: 10.1093/cvr/cvp420. [DOI] [PubMed] [Google Scholar]
- 24.Papapetropoulos A, Pyriochou A, Altaany Z, et al. Hydrogen sulfide is an endogenous stimulator of angiogenesis. Proc Natl Acad Sci USA. 2009;106:21972–7. doi: 10.1073/pnas.0908047106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dimmeler S, Dernbach E, Zeiher AM. Phosphorylation of the endothelial nitric oxide synthase at ser-1177 is required for VEGF-induced endothelial cell migration. FEBS Lett. 2000;477:258–62. doi: 10.1016/s0014-5793(00)01657-4. [DOI] [PubMed] [Google Scholar]
- 26.Thors B, Halldorsson H, Thorgeirsson G. Thrombin and histamine stimulate endothelial nitric-oxide synthase phosphorylation at Ser1177 via an AMPK mediated pathway independent of PI3K-Akt. FEBS Lett. 2004;573:175–80. doi: 10.1016/j.febslet.2004.07.078. [DOI] [PubMed] [Google Scholar]
- 27.Zheng J, Wen Y, Chen DB, et al. Angiotensin II elevates nitric oxide synthase 3 expression and nitric oxide production via a mitogen-activated protein kinase cascade in ovine fetoplacental artery endothelial cells. Biol Reprod. 2005;72:1421–8. doi: 10.1095/biolreprod.104.039172. [DOI] [PubMed] [Google Scholar]
- 28.Ziche M, Morbidelli L, Masini E, et al. Nitric oxide mediates angiogenesis in vivo and endothelial cell growth and migration in vitro promoted by substance P. J Clin Invest. 2003;94:2036–44. doi: 10.1172/JCI117557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li Volti G, Sacerdoti D, Sangras B, et al. Carbon monoxide signaling in promoting angiogenesis in human microvessel endothelial cells. Antioxid Redox Signal. 2005;7:704–10. doi: 10.1089/ars.2005.7.704. [DOI] [PubMed] [Google Scholar]
- 30.McCabe TJ, Fulton D, Roman LJ. Sessa W.C. Enhanced electron flux and reduced calmodulin dissociation may explain “calcium-independent” eNOS activation by phosphorylation. J Biol Chem. 2000;275:6123–8. doi: 10.1074/jbc.275.9.6123. [DOI] [PubMed] [Google Scholar]
- 31.Smith SK. Angiogenesis and reproduction. BJOG. 2001;108:777–83. doi: 10.1111/j.1471-0528.2001.00211.x. [DOI] [PubMed] [Google Scholar]
- 32.Burri PH, Hlushchuk R, Djonov V. Intussusceptive angiogenesis: its emergence, its characteristics, and its significance. Dev Dyn. 2004;231:474–88. doi: 10.1002/dvdy.20184. [DOI] [PubMed] [Google Scholar]
- 33.Folkman J, Klagsbrun M. Angiogenic factors. Science. 1987;235:442–7. doi: 10.1126/science.2432664. [DOI] [PubMed] [Google Scholar]
- 34.Bergers G, Benjamin LE. Tumorigenesis and the angiogenic switch. Nat Rev Cancer. 2003;3:401–10. doi: 10.1038/nrc1093. [DOI] [PubMed] [Google Scholar]
- 35.Liekens S, De Clercq E, Neyts J. Angiogenesis: regulators and clinical applications. Biochem Pharmacol. 2001;61:253–70. doi: 10.1016/s0006-2952(00)00529-3. [DOI] [PubMed] [Google Scholar]
- 36.Predmore BL, Julian D, Cardounel AJ. Hydrogen sulfide increases nitric oxide production from endothelial cells by an Akt-dependent mechanism. Front Physiol. 2011;2:1–5. doi: 10.3389/fphys.2011.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cai WJ, Wang MJ, Moore PK, et al. The novel proangiogenic effect of hydrogen sulfide is dependent on Akt phosphorylation. Cardiovasc Res. 2007;76:29–40. doi: 10.1016/j.cardiores.2007.05.026. [DOI] [PubMed] [Google Scholar]
- 38.Coletta C, Papapetropoulos A, Erdelyi K, et al. Hydrogen sulfide and nitric oxide are mutually dependent in the regulation of angiogenesis and endothelium-dependent vasorelaxation. Proc Natl Acad Sci USA. 2012;109:9161–6. doi: 10.1073/pnas.1202916109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


