Abstract
Self-reported cigarettes per day (CPD) is a very common screening, as well as dependent or independent, measure in clinical and non-clinical research on smoking, but consistency of CPD across days in dependent smokers is uncertain. Adult dependent smokers (N=357; 170 men, 187 women) retrospectively reported “usual” CPD at screening and then prospectively self-monitored CPD on 3 consecutive days of one week during an ad libitum baseline period. Participants were those recruited for later tests of brief medication effects in those with high (n=170) versus low (n=187) interest in quitting smoking soon (within 3 months). Consistency was determined by intraclass correlation (ICC). Prospective daily CPD was generally consistent (ICC = 0.78, 95% CI of 0.74–0.81), but CPD changed (increase or decrease) by 5 cigarettes/day or more in 40% of participants and by at least 10/day in 10%. Consistency in CPD was greater in higher dependent smokers and in women with low (vs. high) quit interest, but consistency tended to be greater in men with high (vs. low) quit interest. Although retrospectively reported CPD at screening was consistent with the overall mean for prospectively monitored daily CPD, 15% of participants differed by at least 5/day between methods, and digit bias was twice as likely with retrospective versus prospective CPD, which was at chance levels. Understanding variability in CPD may improve knowledge of dependence and factors that foster or discourage daily smoking amount, but precise assessment of daily CPD likely requires prospective monitoring.
Keywords: smoking behavior, cigarettes per day, dependence, sex differences
A smoker’s daily cigarette intake is an important factor in many studies assessing level of dependence or various consequences of smoking exposure. Self-reported cigarettes per day (CPD) has been used to define “heavy” dependence (Alpert, Connolly, & Biener, 2012), “hardcore” smokers (Augustson & Marcus, 2004), and as part of the inclusion/exclusion criteria for study recruitment (e.g., Hughes, Lesmes, Hatsukami, Richmond, Lichtenstein, Jorenby, et al., 1999). Moreover, the initial screening of potential participants sometimes uses CPD for assignment of subjects to study conditions, such as cessation medication dosing regimen (Burns, Tong & Levinson, 2010; Sonderskov, Olsen, Sabroe, Meillier, & Overvad, 1997). CPD also has been proposed as a criterion for diagnosing tobacco dependence in DSM-5 (Baker, Breslau, Covey, & Shiffman, 2012).
Careful assessment of CPD over time may increase our understanding of dependence and other factors that promote or discourage a persistent level of daily smoking consumption. For example, CPD is associated with biochemical indices of smoke exposure (Klesges, Debon, & Ray, 1995), genetic factors (Chen, Baker, Grucza, Wang, Johnson, Breslau, et al., 2011), and subsequent quitting success (Borland, Yong, O’Connor, Hyland, & Thompson, 2010). Multiple assessments of CPD across weeks, months, or years have been used to gauge trajectories of smoking escalation during onset of dependence in teens (e.g., Tan, Dierker, Rose, & Li, 2011; Weinstein, Mermelstein, Shiffman, & Flay, 2008) and changes in smoking behavior as a result of harm reduction efforts (Hoeppner, Goodwin, Velicer, Mooney, & Hatsukami, 2007) or among those unwilling or unable to quit (Yong, Borland, Thrasher, & Thompson, 2012).
However, the strength of these associations and screening methods depends on the consistency and reliability of self-reported CPD, which may be unclear (e.g., Shiffman, 2009). Prior research has assessed the consistency of self-report measures of CPD in smokers who were actively engaged in preparing to quit (Gariti, Alterman, Ehrman, & Pettinati, 1998; Toll, Cooney, McKee, & O’Malley, 2005) or otherwise participating in a treatment trial, such as for other substance abuse (Fals-Stewart, O’Farrell, Freitas, McFarlin, & Rutigliano, 2000) or for smoking harm reduction (Hoeppner, et al., 2007). Nevertheless, we are unaware of published studies prospectively assessing such consistency in CPD across temporally proximal periods (e.g. within a few weeks) among adult dependent smokers who were not actively engaged in treatment of some kind. Other studies have examined daily variability in abstinence status or smoking reduction (Peters & Hughes, 2009) and the temporal patterns of smoking within a day (Chandra, Shiffman, Scharf, Dang, & Shadel, 2007) in smokers preparing to quit, as well as consistency of acute smoking topography in smokers not trying to quit (e.g., Perkins, Karelitz, Giedgowd, & Conklin, 2012). Yet, this research did not specifically assess the consistency of day-to-day ad libitum cigarette consumption of dependent smokers.
Moreover, wide variability across days in cigarette intake may question the reliability of a single reported “usual” CPD and suggest the need for careful, prospective assessments, both to detect such variability and avoid under- or over-counting the actual number consumed per day. Reliability of recall for even recent CPD can be lower in retrospective self-reports of smoking, compared to prospective assessment, such as via electronic diaries (e.g., Shiffman, Hufford, Hickox, Paty, Gnys, & Kassel, 1997). Similarly, another commonly identified problem with smoker estimates of their “usual” number of CPD is “digit bias,” in which their estimates are observed to be values that are even multiples of 5 cigarettes (e.g. 15/day, 20/day, 25/day) more often than would be expected by chance (Klesges, et al., 1995). In a study using a method aimed at gaining a more precise CPD estimate, the retrospective Time Line Follow Back (TLFB) procedure, digit bias in reports of CPD was about five times more likely than expected (Shiffman, 2009).
The current analysis examined the consistency of prospectively self-monitored daily cigarette intake (i.e., CPD) in 357 dependent adult smokers across three consecutive days of one week. We also examined individual differences in the consistency of this CPD due to gender, level of dependence, menthol brand preference, and high or low interest in making a permanent quit smoking attempt in the next 3 months. We did not relate CPD to biochemical measures of expired-air CO or cotinine; neither could be assessed at the end of each 24-hr period of day-today CPD self-monitoring (midnight) and both were sensitive to variability that intentionally was not controlled (e.g. hours since last cigarette; Benowitz, Jacob, Ahijevich, Jarvis, Hall, LeHouzec, et al. 2002). Finally, CPD amounts were also compared with a one-time retrospective measure of “usual” CPD (i.e. “global”; Shiffman, 2009), obtained from the participant at an initial screening session in the manner CPD is typically assessed (e.g., Borland, et al., 2010). The objective there was to examine how well such commonly obtained retrospective single estimates predict subsequent prospectively monitored daily cigarette intake.
Methods
Participants
Participants were 357 adult smokers (170 men, 187 women) providing data from the initial screening session and baseline week of three very similar studies. All were required to meet DSM-IV nicotine dependence criteria (adapted from the measure reported by Breslau, Kilbey, & Andreski, 1994), smoke ≥ 10 cigarettes per day for ≥ 1 year, and provide a CO of at least 10 ppm. They self-identified mostly as Caucasian (76.5%), with 12.3% as African-American, 3.1% as Asian, less than 1% as Hispanic or Other, and 7% More than one ethnicity. These studies were each aimed at assessing short-term ability to quit smoking due to week-long placebo or medication conditions (see Perkins, Lerman, Stitzer, Fonte, Briski, Scott, & Chengappa, 2008; Perkins, Lerman, Fonte, Mercincavage, Stitzer, Chengappa, & Jain, 2010). However, only smoking behavior during the baseline ad libitum smoking week, prior to any medication, is analyzed here. There were no differences in participant characteristics across the three studies.
Recruitment ads sought smokers who were, or were not, interested in quitting smoking “soon” (i.e. at the end of the specific study, which was within the next 3 months). Those intending to quit within 3 months were labeled “high” in quit interest, while those stating no intention of quitting within the next 6 months were labeled “low” in quit interest. Only those who consistently indicated high or low interest in quitting during both a phone screen and then an in-person screening session were eligible. (Those wanting to quit immediately and those intending to quit within 3–6 months were excluded and referred to local treatment programs.) Assessment and validation of quit interest is described in more detail elsewhere (Perkins et al., 2008; 2010). Demographic and smoking characteristics, assessed during the initial screening session, are presented in Table 1 by groups divided on high versus low quit interest.
Table 1.
Demographic and smoking characteristics assessed during the initial screening session, by low and high current quit smoking interest.
| Current Quit Interest | ||||||
|---|---|---|---|---|---|---|
| Low (n = 187) | High (n = 170) | Total (N = 357) | ||||
| Mean | S.D. | Mean | S.D. | Mean | S.D. | |
| Characteristics | ||||||
| Age | 30.1 | 11.7 | 33.7 | 11.5 | 31.8 | 11.7 |
| Gender (% male) | 48.70% | 46.50% | 47.60% | |||
| Smoking History | ||||||
| Cigarettes/day | 17.0 | 5.5 | 16.6 | 4.9 | 16.8 | 5.2 |
| FTND (0–10) | 4.6 | 1.5 | 4.7 | 1.6 | 4.7 | 1.5 |
| Years smoking | 12.5 | 10.8 | 14.9 | 10.4 | 13.6 | 10.7 |
| Menthol (% yes) | 41.40% | 44.71% | 42.98% | |||
Procedure
These studies were from a project aimed at assessing the number of days a participant (high or low in quit interest) was able to stop smoking for at least 24 hrs during week-long simulated quit attempts while taking active medication versus placebo. Following the smoking data examined in the current research, the three within-subjects studies compared days quit during week-long medication conditions involving 21 mg nicotine patch (N=205), varenicline (N=111), or bupropion (N=41), in comparison with a week-long placebo condition. (As noted, these medication conditions were not relevant here since only daily ad libitum smoking data from the initial baseline week, prior to starting any medication, is included in analyses.) These studies were approved by the University of Pittsburgh Institutional Review Board, and all participants provided written informed consent for participation after the nature and consequences of the relevant study was explained.
Each study began with a screening session to verify study eligibility, including smoking characteristics of self-reported usual CPD ≥ 10, and CO ≥ 10 ppm, although none was informed of eligibility requirements. Retrospective CPD at screening was determined by asking, “How many cigarettes per day do you smoke?” They also reported their preferred brand (and menthol) and completed the Fagerstrom Test of Nicotine Dependence, or FTND (Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991).
After study entry, the participant came to the lab for three brief visits during Mon-Fri of the first study week (“baseline”), which began an average of 11.4 days after the screening session. The purpose was to assess ad libitum smoking prior to the start of a medication condition the second study week. During the first lab visit of the baseline week, participants were given three tally cards to use in self-monitoring their smoking on each of the subsequent three consecutive days, beginning at midnight (i.e., the next day). Baseline week visits began on Mon or Tues, and so the 3 self-monitoring days were Tues, Wed, and Thurs, or Wed, Thurs, and Fri. Each tally was turned in at the next scheduled weekday session following the day they were to self-monitor smoking. The rows of each tally card listed the individual hours of the day (e.g. “12 noon–1:00 pm”) starting at midnight, with a space to mark tallies. Participants were instructed to place a tally mark every time they smoked a cigarette at that time. (The size and shape of the card was intentionally designed to fit inside the cellophane wrapper of a pack of cigarettes, to facilitate compliance.) To encourage compliance, they received $5 for turning in the cigarette tally card for the prior day’s smoking. (Twenty other potential participants were excluded from these analyses due to missing tally data.) This method has been shown to be valid and reliable in assessments of amount of daily nicotine spray medication use (Perkins, Grobe, D’Amico, Fonte, Wilson, & Stiller, 1996).
Data Analyses
Consistency of CPD across the three days during the baseline week was determined primarily by intraclass correlation (ICC). Type A ICC values were examined to determine similarity of absolute CPD amounts (i.e., agreement; McGraw & Wong, 1996), the more relevant measure. (The typically higher Type C ICC values provide only a relative ranking of CPD and so were not of interest because they ignore potential systematic differences across days). Individual differences in consistency were determined by non-overlapping 95% confidence intervals (CI) of the ICC’s between subgroups differing on dichotomous characteristics of subject sex, quit interest (high/low), FTND (high/low, determined by scores of 5 or greater vs. 4 or lower, respectively), or menthol brand preference (yes/no; one participant did not indicate clear brand preference, leaving N=356 for this analysis). We also examined the prevalence of smokers who varied their individual daily intake by at least 5 cigarettes/day (the standard deviation for the entire sample of usual CPD assessed at screening; see Table 1); this approach is similar to other research on smoking consistency across days (John Hughes, personal communication). To illustrate differences in consistency between the subgroup that did (“variable”) versus did not (“consistent”) vary intake by at least 5/day, we presented CPD for each of the 3 baseline days among individual participants from a random sample of 10% within each subgroup. Randomization was performed via the SPSS Random sample of cases method (Brace, Kemp, & Snelgar, 2003). Finally, we used t-test and multiple regression analyses to examine the association of the initial screening assessment of retrospective CPD with prospective self-monitored daily CPD during the 3 baseline days.
Results
Mean (SD) prospectively assessed CPD (i.e. daily tallies) for all 357 participants was 16.8 ± 6.4, 16.5 ± 6.4, and 17.2 ± 6.8 for the three consecutive days of the baseline week. More importantly, individual daily CPD consistency was evidenced by ICC=0.78 (95% CI=0.74–0.81; Cronbach’s alpha = 0.91). As expected, these values did not differ between subsamples recruited for the three studies, with respective ICC (95% CI) results of 0.77 (0.72–0.81), 0.78 (0.72–0.84), and 0.82 (0.71–0.89), and so results were collapsed across studies.
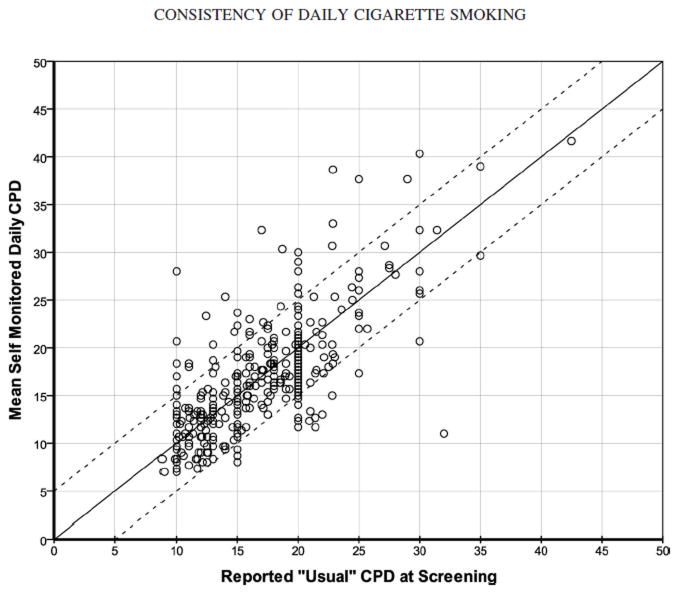
When consistency in self-monitoring of CPD was examined further for each individual participant, we found that the change between the three days (i.e. from day 1 to day 2, or day 1 to day 3, or day 2 to day 3) increased or decreased by at least 5/day in 146 of the 357 participants (40.9%). Day-to-day change in CPD was at least 10/day in 37 of these participants (10.4% of the entire sample). Thus, for two-fifths of these dependent adult smokers, CPD varied by at least 5/day, although these results also indicate that more than half of the smokers varied their daily intake by less than 5/day. These two subgroups were labeled “variable” and “consistent,” respectively, and are illustrated in Figure 1 by the day-to-day CPD for randomly selected 10% subsamples of each subgroup. (Retrospective screening CPD is also presented, for visual comparison.) We also examined the potential for digit bias in this self-monitoring by assessing the number of daily tallies that were evenly divisible by 5 (i.e. 10, 15, 20, 25, etc. cigarettes per day). Frequency of CPD values divisible by 5 was no more likely than expected (20%), as such values were observed in 17.9%, 20.7%, and 16.8% of the tallies on days 1, 2, and 3, respectively.
Figure 1.
Individual cigarettes per day (CPD) assessed retrospectively at the screening session (“usual”) and then prospectively during each of three consecutive days during ad libitum baseline. Shown are representative 10% subsamples of those whose prospective CPD did (“variable”, n=15) or did not (“consistent”, n=19) vary between these baseline days by at least 5/day. The screening session was an average of 11.4 days prior to Day 1 of baseline (shown by dashed lines).
Individual differences in consistency
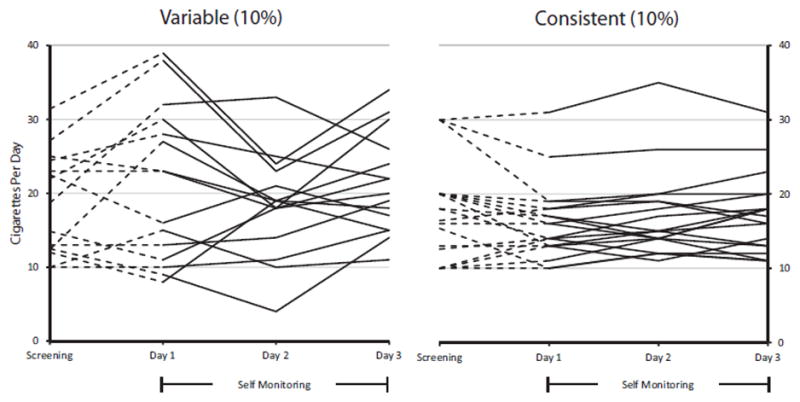
Regarding individual differences, the consistency of self-monitored CPD was greater in the 169 participants with higher FTND (≥5) vs. the 188 with lower FTND (≤4), as the non-overlapping ICC’s (CI’s) were 0.81 (0.76–0.85) vs 0.67 (0.60–0.73), respectively. Although consistency did not differ between women and men overall, 0.81 (0.77–0.85) vs 0.74 (0.68–0.79), respectively, the difference in ICC due to higher versus lower FTND was more apparent in women compared to men, as indicated in Figure 2.
Figure 2.
Intraclass correlations (ICC) and bars to show 95% confidence intervals (CI) in self-monitored cigarettes per day across the three days of the baseline week. Results are presented separately for women and men, by low (≤ 4; 96 F, 92 M) and high (≥ 5; 91 F, 78 M) FTND score and by low (96 F, 91 M) and high (91 F, 79 M) quit smoking interest. CI’s presented in the bars do not overlap between the subgroups of women, indicating subgroup differences in consistency, but do overlap between the subgroups of men.
Unexpectedly, moreover, the consistency in CPD due to high versus low quit smoking interest tended to differ in opposite directions for women compared to men. As also shown in Figure 2, consistency was greater due to low versus high quit interest among women, while consistency tended to be greater due to high versus low quit interest among men, based on the comparison of overlap in CI’s between quit interest subgroups for each sex. As a result, consistency was virtually identical overall between those who were high versus low in quit interest, 0.78 (0.72–0.82) vs 0.78 (0.73–0.82), respectively, masking the apparent interaction of sex by quit interest on consistency in CPD. However, when examining individual differences in the 146 whose CPD tallies varied by at least 5/day, men were more likely to be “variable” across these baseline days (82 of 170 men, 48.2%) compared to women (64 of 187 women, 34.2%), χ2(1)=7.23, p<.01. No other differences were significant, as ICC results also showed that consistency was similar between those whose preferred brand was menthol (n=153) or non-menthol (n=203), 0.81 (0.76–0.85) vs 0.76 (0.70–0.80), respectively, and there was no menthol difference by sex.
Retrospective CPD at screening versus prospective self-monitoring of CPD
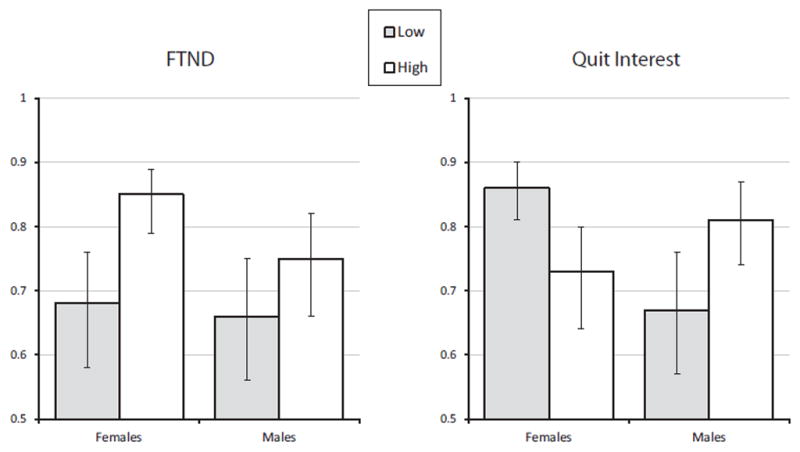
For the group as a whole, the mean (SD) retrospective report of usual CPD at the screening session (Table 1) was virtually identical to that for the subsequent prospectively self-monitored tallies of CPD, 16.8 ± 5.2 vs. 16.8 ± 6.0, respectively, t(356)= 0.06, ns (paired t-test). For individual participants, the association of retrospective usual CPD at screening with the mean prospective daily tallies of CPD during baseline is presented in the scatterplot in Figure 3. Regression showed that the initial screening report of CPD was highly related to the mean of the CPD tallies, B(SE)=0.78 ± 0.05, t (352)=16.91, p<.001, controlling for FTND, quit interest, and gender (i.e. characteristics that showed some association with daily consistency, above). The R2 was 0.563. Because of the association of high/low FTND with CPD consistency by sex (above), we compared daily CPD consistency by high/low screening reports of usual CPD. The ICC for consistency of daily CPD was similar between those reporting a usual CPD intake at screening of at least 20/day (n=124) versus less than 20/day (n=233) among women, 0.75 (0.64–0.83) vs 0.74 (0.68–0.80), respectively, and among men, 0.72 (0.61–0.80) vs 0.59 (0.49–0.69).
Figure 3.
Scatterplot of the association between reported retrospective “usual” CPD at screening with the mean of the prospective CPD during the baseline week for all 357 subjects. Diagonal lines indicate the degree of similarity between the two measures (continuous line), or self-monitored CPD values that were 5/day higher or lower than the screening reports of CPD (dashed lines). Digit bias at screening is suggested by the high frequency of screening CPD numbers evenly divisible by 5.
However, the retrospective screening measure of CPD was at least 5/day less than mean self-monitored CPD during the baseline week in 10.1% of participants, including at least 10/day less in 3.1%. By comparison, the screening measure of CPD was at least 5/day more than mean self-monitored CPD in half as many participants, 5.3%, including at least 10/day more in just 0.3% (1 smoker). Therefore, although relatively few in number, smokers were twice as likely to potentially under-state as over-state their typical CPD during the one-time retrospective screening assessment of cigarettes per day, compared to their subsequent prospective daily tallies of CPD. In addition, digit bias was much more apparent with these retrospective screening reports of CPD, about twice as often as expected (20%), as values evenly divisible by 5 were observed in 41.2% of such reports (binomial z = 9.94, p<.001; see Figure 3).
Discussion
Our results suggested that prospective self-monitoring of CPD in 357 adult dependent smokers not currently engaged in treatment showed similar daily means during a week of ad lib smoking, when considered for the entire sample. However, examination of day-to-day variability in CPD for each individual indicated that 40% of them increased or decreased CPD by at least 5/day, and 10% changed by at least 10/day. Therefore, research may only detect such variability with careful monitoring of prospective CPD (e.g., as a dependent measure in harm reduction). The validity of our self-monitored tallies of CPD was indirectly supported by the comparability between the means for the daily tallies versus retrospective CPD at screening and by lack of evidence for digit bias in daily tallies, as such bias was no more common than chance.
Among individual differences warranting further study, consistency of CPD was greater among more dependent smokers, as assessed by higher versus lower FTND, especially for women (Figure 2). These results may be consistent with the notion that heavily dependent smokers are more invariant in their smoking, perhaps reflecting greater dependence on nicotine per se, while the smoking of less dependent smokers may be more responsive to environmental or other factors that can vary day by day (e.g., Shiffman & Paty, 2006). Consistency in daily CPD also was related to near-term interest in quitting smoking in opposite fashion between women and men. Consistency was greater in women with low quit interest but tended to be greater in men with high quit interest (Figure 2). It is conceivable, if speculative, that women and men may differentially change their daily smoking frequency in anticipation of a near-term attempt to quit. However, although no main effect of sex was apparent for consistency of CPD, men were more likely than women to be among those whose daily CPD varied by at least 5/day. Research is needed to replicate these differences in daily CPD consistency due to characteristics of women versus men. Finally, menthol preference was not related to CPD consistency.
Similar to the results for day-to-day consistency in CPD, the retrospective screening assessment of usual CPD produced values that appeared to be comparable to the mean for self-monitored daily CPD when the sample was considered as a whole. Yet, when considered on an individual basis, the mean prospective CPD tallies differed from the retrospective screening CPD by at least 5/day (lower or higher) in 15% of the participants. This suggests that one-time reports of “usual” CPD may not closely predict subsequent actual daily CPD in some smokers (see Figures 1 and 3), consistent with other research (e.g., Shiffman, 2009). Although smokers may estimate their average daily CPD when asked how many cigarettes per day they smoke, twice as many of these participants (10%) reported lower as higher CPD amounts during retrospective screening versus the prospective daily tallies. Therefore, smokers may be twice as likely to retrospectively under-report as over-report their actual CPD.
Limitations of this research include self-monitoring of CPD via simple daily “tallies” (i.e., a mark for each cigarette), which itself can influence smoking behavior, rather than with real-time electronic responses (e.g., Shiffman, 2009). Although participants were monetarily reinforced for completing and turning in such daily monitoring tallies, we could not validate each cigarette consumption. Nevertheless, there was little evidence of under-reporting their CPD via the prospective daily self-monitoring forms, which tended to be similar to, or occasionally greater than, the retrospective screening report of CPD (Figures 1 and 3). Also, lack of digit bias in the self-monitoring forms, compared to a doubling of expected digit bias in the screening CPD report, suggests reasonably accurate assessment of daily CPD in these participants.
We also assessed daily CPD over just 3 consecutive weekdays of one week, and longer duration, inclusion of the weekend, or a longer interval between assessments of daily CPD may reveal greater (or lesser) variability in the frequency of daily cigarette intake (e.g., Cooper, Borland, Yong, Hyland, & Cummings, 2012). Yet, to facilitate comparison between the methods of assessing CPD, we wanted to conduct the retrospective screening and prospective daily self-monitoring assessments in close temporal proximity (mean of about 2 weeks between screening and end of self-monitoring assessments). Our research also assessed primarily young adult dependent smokers (see Table 1), and consistency of CPD may be different for older adults or adolescent smokers, especially those who are not dependent and/or smoke fewer than 10 cigarettes/day (Harris, Golbeck, Cronk, Catley, Conway, & Williams, 2009). As suggested, consistency of CPD may also differ sharply depending on the particular situational factors across days experienced by participants (e.g. Hatsukami, Morgan, Pickens, & Champagne, 1990; Chandra, et al., 2007), and we did not assess the presence of such factors.
Strengths of the research include the possibility that this is the first direct test of consistency in CPD across several consecutive days of ad libitum smoking among a fairly large sample of adult dependent smokers not actively engaged in a clinical trial. This large sample also allowed us to explore potential individual differences in daily consistency due to characteristics that could be relevant when conducting clinical trials or other research on amount of smoking behavior. Specifically, comparison of smokers differing in FTND and explicitly recruited for high versus low quit smoking interest allowed us to determine whether level of dependence or planning to quit in a few months might alter consistency in CPD. Our sample size also enabled us to determine that no such differences in CPD consistency were found due to menthol preference or between men and women overall.
In conclusion, short-term CPD may vary across days in nearly half of adult smokers, especially those who are less dependent. Consistency in daily CPD due to an interest in quitting smoking may not vary overall but could differ in opposite ways between men and women. Although a traditional one-time assessment of retrospective CPD may generally predict prospective monitoring of daily CPD in most smokers, it may not in many others because it fails to detect day-to-day variability, and digit bias may be twice as likely. Better knowledge of variability in CPD could increase our understanding of individual differences in dependence and factors that may alter daily smoking behavior.
Acknowledgments
Funding
This research was supported by NIH Grants CA143187 and DA031218.
The authors thank John Hughes for his helpful comments about assessing cigarettes per day, as well as Carolyn Fonte, Melissa Mercincavage, and Jessica Briski for their assistance in these studies.
Footnotes
Declaration of Interests
No authors have any disclosures.
References
- Alpert HR, Connolly GN, Biener L. A prospective cohort study challenging the effectiveness of population-based medical intervention for smoking cessation. Tobacco Control. 2012 doi: 10.1136/tobaccocontrol-2011-050129. in press. Downloaded from TC Online First. [DOI] [PubMed] [Google Scholar]
- Augustson EM, Marcus SE. Use of the Current Population Survey to characterize subpopulations of continued smokers: a national perspective on the “hardcore” smoker phenomenon. Nicotine & Tobacco Research. 2004;6:621–629. doi: 10.1080/14622200410001727876. [DOI] [PubMed] [Google Scholar]
- Baker TB, Breslau N, Covey L, Shiffman S. DSM criteria for tobacco use disorder and tobacco withdrawal: a critique and proposed revisions for DSM-5. Addiction. 2012;107:263–275. doi: 10.1111/j.1360-0443.2011.03657.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland R, Yong HH, O’Connor RJ, Hyland A, Thompson ME. The reliability and predictive validity of the Heaviness of Smoking Index and its two components: Findings from the International Tobacco Control Four Country study. Nicotine & Tobacco Research. 2010;12(suppl 1):S45–S50. doi: 10.1093/ntr/ntq038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brace N, Kemp R, Snelgar R. SPSS for Psychologists. 2. Mahwah NJ: Lawrence Erlbaum Assoc; 2003. [Google Scholar]
- Breslau N, Kilbey MM, Andreski P. DSM-IIIR nicotine dependence in young adults: prevalence, correlates and associated psychiatric disorders. Addiction. 1994;89:743–754. doi: 10.1111/j.1360-0443.1994.tb00960.x. [DOI] [PubMed] [Google Scholar]
- Burns EK, Tong S, Levinson AH. Reduced NRT supplies through a quitline: smoking cessation differences. Nicotine & Tobacco Research. 2010;12:845–849. doi: 10.1093/ntr/ntq094. [DOI] [PubMed] [Google Scholar]
- Chandra S, Shiffman S, Scharf S, Dang Q, Shadel WG. Daily smoking patterns, their determinants, and implications for quitting. Experimental and Clinical Psychopharmacology. 2007;15:67–80. doi: 10.1037/1064-1297. [DOI] [PubMed] [Google Scholar]
- Chen LS, Baker TB, Grucza R, Wang JC, Johnson EC, Breslau N, et al. Dissection of the phenotypic and genotypic associations with nicotinic dependence. Nicotine & Tobacco Research. 2011;14:425–433. doi: 10.1093/ntr/ntr231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper J, Borland R, Yong H-H, Hyland A, Cummings KM. Variations in daily cigarette consumption on work days compared with nonwork days and associations with quitting: Findings from the International Tobacco Control Four-Country survey. Nicotine & Tobacco Research. 2012 doi: 10.1093/ntr/ntr110. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fals-Stewart W, O’Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. Journal of Consulting and Clinical Psychology. 2000;68:134–144. doi: 10.1037/0022-006X.68.1.134. [DOI] [PubMed] [Google Scholar]
- Gariti PW, Alterman AI, Ehrman RN, Pettinati HM. Reliability and validity of the aggregate method of determining number of cigarettes smoked per day. American Journal on Addictions. 1998;7:283–287. [PubMed] [Google Scholar]
- Harris KJ, Golbeck AL, Cronk NJ, Catley D, Conway K, Williams KB. Timeline follow-back versus global self-reports of tobacco smoking: a comparison of findings with nondaily smokers. Psychology of Addictive Behaviors. 2009;23:368–372. doi: 10.1037/a0015270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatsukami DK, Morgan SF, Pickens RW, Champagne SE. Situational factors in cigarette smoking. Addictive Behaviors. 1990;15:1–12. doi: 10.1016/0306-4603(90)90002-F. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hoeppner BB, Goodwin MS, Velicer WF, Mooney ME, Hatsukami DK. Detecting longitudinal patterns of daily smoking following drastic cigarette reduction. Addictive Behaviors. 2007;33:623–639. doi: 10.1016/j.addbeh.2007.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Lesmes GR, Hatsukami DK, Richmond RL, Lichtenstein R, Jorenby DE, et al. Are higher doses of nicotine replacement more effective for smoking cessation? Nicotine & Tobacco Research. 1999;1:169–174. doi: 10.1080/14622299050011281. [DOI] [PubMed] [Google Scholar]
- Klesges RC, Debon M, Ray JW. Are self-reports of smoking rate biased? Evidence from the second National Health and Nutrition Examination Survey. Journal of Clinical Epidemiology. 1995;48:1225–1233. doi: 10.1016/0895-4356(95)00020-5. [DOI] [PubMed] [Google Scholar]
- McGraw KO, Wong SP. Forming inferences about some intraclass correlation coefficients. Psychological Methods. 1996;1:30–46. Retrieved from http://ft.csa.com/ids70. [Google Scholar]
- Perkins KA, Grobe JE, D’Amico D, Fonte C, Wilson A, Stiller RL. Low-dose nicotine nasal spray use and effects during initial smoking cessation. Experimental and Clinical Psychopharmacology. 1996;4:157–165. doi: 10.1037/1064-1297.4.2.157. [DOI] [Google Scholar]
- Perkins KA, Karelitz JL, Giedgowd GE, Conklin CA. The reliability of puff topography and subjective responses during ad lib smoking of a single cigarette. Nicotine & Tobacco Research. 2012;14:490–494. doi: 10.1093/ntr/ntr150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins KA, Lerman C, Fonte C, Mercincavage M, Stitzer ML, Chengappa KRN, Jain A. Cross-validation of a new procedure for early screening of smoking cessation medications in humans. Clinical Pharmacology and Therapeutics. 2010;88:109–114. doi: 10.1038/clpt.2010.65. [DOI] [PubMed] [Google Scholar]
- Perkins KA, Lerman C, Stitzer ML, Fonte CA, Briski JL, Scott JA, Chengappa KNR. Development of procedures for early screening of smoking cessation medications in humans. Clinical Pharmacology and Therapeutics. 2008;84:216–221. doi: 10.1038/clpt2008.30. [DOI] [PubMed] [Google Scholar]
- Peters EN, Hughes JR. The day-to-day process of stopping or reducing smoking: A prospective study of self-changes. Nicotine & Tobacco Research. 2009;11:1083–1092. doi: 10.1093/ntr/ntp105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S. How many cigarettes did you smoke? Assessing cigarette consumption by global report, time-line follow-back, and ecological momentary assessment. Health Psychology. 2009;28:519–526. doi: 10.1037/a0015197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Paty J. Smoking patterns and dependence: contrasting chippers and heavy smokers. Journal of Abnormal Psychology. 2006;115:509–523. doi: 10.1037/0021-843X.115.3.509. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Hufford M, Hickox M, Paty JA, Gnys M, Kassel JD. Remember that?: A comparison of real-time versus retrospective recall of smoking lapses. Journal of Consulting and Clinical Psychology. 1997;65:292–300. doi: 10.1037/0022-006X.65.2.292.a. [DOI] [PubMed] [Google Scholar]
- Sonderskov J, Olsen J, Sabroe S, Meillier L, Overvad K. Nicotine patches in smoking cessation: a randomized trial among over-the-counter customers in Denmark. American Journal of Epidemiology. 1997;145:309–318. doi: 10.1093/oxfordjournals.aje.a009107. [DOI] [PubMed] [Google Scholar]
- Tan XM, Dierker L, Rose J, Li RZ. How spacing of data collection may impact estimates of substance use trajectories. Substance Use & Misuse. 2011;46:758–768. doi: 10.3109/10826084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toll BA, Cooney NL, McKee SA, O’Malley SS. Do daily interactive voice response reports of smoking behavior correspond with retrospective reports? Psychology of Addictive Behaviors. 2005;19:291–295. doi: 10.1037/0893-164X.19.3.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein SA, Mermelstein R, Shiffman S, Flay B. Mood variability and cigarette smoking escalation among adolescents. Psychology of Addictive Behaviors. 2008;22:504–513. doi: 10.1037/0893-164X.22.4.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yong HH, Borland R, Thrasher JF, Thompson ME. Stability of cigarette consumption over time among continuing smokers: a latent growth curve analysis. Nicotine & Tobacco Research. 2012;14:531–539. doi: 10.1093/ntr/ntr242. [DOI] [PMC free article] [PubMed] [Google Scholar]