Abstract
The timing of the umbilical cord clamping at birth is still controversial. In the modern era of medicine, the cord has been clamped early to facilitate resuscitation and stabilization of infants. However, recently delayed cord clamping has been supported by physicians because it allows for the physiological transfer of blood from the placenta to the infant. Many clinical studies have revealed that the delayed cord clamping elevates blood volume and haemoglobin and prevents anaemia in infants. Moreover, since it was known that umbilical cord blood contains various valuable stem cells such as haematopoietic stem cells, endothelial cell precursors, mesenchymal progenitors and multipotent/pluripotent lineage stem cells, the merit of delayed cord clamping has been magnified. In this review, we discuss the advantages and disadvantages of delayed cord clamping at birth. We highlight the importance of delayed cord clamping in realizing mankind’s first stem cell transfer and propose that it should be encouraged in normal births.
Keywords: umbilical cord blood, stem cells, delayed cord clamping, birth, anaemia, preterm
Introduction
For decades, the timing of the umbilical cord clamping at birth has been the focus of controversies and intense discussions among practitioners [1, 2]. Although without clear benefit and no rationale to support it, early cord clamping remains the most common practice among obstetricians and midwives in the western hemisphere [3, 4]. In a recent Cochrane review [5], early cord clamping is defined as covering a wide range from immediately to less than 1 min. from birth, whereas delayed cord clamping is defined as greater than 1 min. to until the cord stops pulsating. Normal cord clamping time can be construed as between 30 sec. to 1 min. after birth. These definitions are used within this review unless otherwise stated. It is however, worth noting that there are some inconsistencies among studies with respect to this, since the earlier (but recently reprinted in 2009) Cochrane review by Rabe et al.[6] defined delayed as more than 30 sec. Historically, birthing included the mother squatting with gravity being a contributing factor to both delivery and draining of the blood from the umbilical cord (Fig. 1). In the era of modern medicine, the cord has been clamped early to facilitate resuscitation and stabilization of infants and because of concerns that delayed clamping could have adverse effects [7]. Moreover, in this period of cord blood banking, the umbilical cord is often clamped early in order to harvest a large amount of blood since the success of cord blood transplantation relates to the volume and number of cells transplanted [8–10]. However, there have been accumulating clinical and meta-analytical studies suggesting that delayed clamping increases blood volume and prevents anaemia in infants without severe adverse effects. In this review, we focus on the importance of delayed cord clamping in terms of the existence of stem cells in the umbilical cord blood (UCB) at birth.
Fig 1.
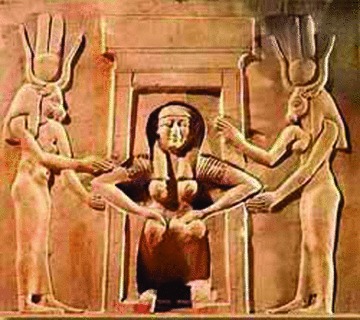
A relief from the Temple of Hathor at Dendera, depicting a squatting woman giving birth. She is assisted by two goddesses Hathor and Taweret. Cairo, Egyptian Museum.
Early haematopoiesis in foetus
To understand the relationship between cord clamping time and stem cells, it is first necessary to comprehend the early haematopoiesis during the human perinatal period [6]. At 2 weeks of human embryogenesis, foetal haematopoiesis begins from stromal cells in the yolk sac. Liver haematopoiesis occurs at 6 weeks in pluripotent stem cells migrating from the yolk sac, but yolk sac haematopoiesis continues until 10 weeks. The liver is the main source of the foetal blood components until 20 weeks when medullary sites in axial bones start haematopoiesis with pluripotent stem cells migrating from the liver. Although haematopoiesis in foetal liver begins to slow following initiation of bone marrow (BM) haematopoiesis, liver haematopoiesis still continues until birth [11]. Haematopoiesis shifts completely from liver to BM after delivery [12]. Therefore, the migration of pluripotent stem cells to BM is still in progress until delivery, suggesting that pluripotent stem cells should exist in the foetal circulation including UCB at this time. With the significant presence of stem cells in the foetal circulation, the issue of cord clamping timing is noteworthy.
Early versus late clamping of the umbilical cord
Delaying the clamping of the umbilical cord at birth allows the physiological transfer of blood from the placenta to the infant. This placental transfusion can increase the infant’s blood volume up to 30 ml/kg of body weight depending on several factors, including timing of clamping, initiation of first breath and cry, the effect of gravity, mode of delivery and intensity of uterine contractions at the end of the second stage of labour [13–17]. Increased blood volume is particularly important for preterm infants because they have less foetal-placenta blood volume than term infants, increasing the risk of relative hypoperfusion if immediate clamping occurs [18, 19]. Hypoperfusion may disrupt the autoregulation that is essential to stabilize cerebral blood flow and prevent a pressure-passive circulation [20].
Several randomized controlled trials, systematic reviews and meta-analyses have compared the effects of late versus early clamping of the umbilical cord. In preterm infants, delaying the clamping of the cord for at least 30 sec. reduced the incidences of intraventricular haemorrhage, late-onset sepsis and anaemia, and decreased the need for blood transfusions [6, 21]. A 1-min. delay in cord clamping resulted in remarkably elevated red blood cell volume/mass and weekly haematocrit compared to early clamping in neonates of 30–36 weeks’ gestation [22]. Furthermore, delayed cord clamping improves cerebral oxygenation in preterm infants in the first 24 hrs of life [23]. A recent study concluded that late clamping is safe and does not compromise the preterm infant in the initial post-partum adaptation phase [24]. In term infants, delaying cord clamping for at least 2 min. reduced the incidence of anaemia in the neonatal period, prevented anaemia over the first 3 months of life and enriched iron stores and ferritin levels for as long as 6 months [25]. This is of particular importance for patients in developing countries where anaemia during infancy and childhood is highly prevalent [26–31]. In contrast to the belief of most practitioners, the risk of some of the potential adverse effects of late cord clamping such as tachypnea or grunting, hyperbilirubinemia, polycythemia and hyperviscosity are not clinically significant and represent part of the physiological compensatory mechanism [25–31].
Another potential benefit of delayed cord clamping is to ensure that the baby can receive the complete retinue of clotting factors necessary at birth since the actual birthing experience has been shown to switch on both the mother’s and baby’s clotting and fibrinolytical systems [32]. It could be suggested that the latter effect facilitates maintenance of umbilical cord flow to the baby.
Of course, there are still many supporters of early cord clamping, or at least for not delaying cord clamping, especially among researchers or physicians who are associated with cord blood banking or transplantation. The residual placental blood volume following normal or delayed cord clamping is probably insufficient for banking and donation [33, 34]. Therefore, harvesters of cord blood may make an attempt to clamp as early as possible to force a larger placental residual volume even though such practice is thought to be ethically inappropriate [35].
There are additional reasons that support early clamping, in particular, the advancement of cord blood banking [12]. First, cord blood harvest is considered a physiological event beyond the preterm, in that consequences extend to full term and healthy newborns’ matter. At term birth, generally the newborn has excessive haemoglobin to compensate for the hypoxic prenatal environment, and subsequently experiences transient physiological anaemia following exposure to the more oxygenated extrauterine environment [12]. A baby with a normal diet has no difficulty in recovering from this natural lack in red blood cells. Therefore, the healthy baby can tolerate considerable decreases in haemoglobin without deleterious adverse effects, even if early clamping was performed for the blood collection [12]. Second, even a normal cord clamping time provides appropriate blood volume for future transplantation [12]. If clamping is delayed unnecessarily in healthy term babies and subsequently cord blood is not collected, invaluable stem cells in the cord blood will be discarded. Thus a concerted effort must be rendered against any intent to waste the opportunity for stem cell collection, especially in view of the lack of evidence demonstrating a relation between cord blood banking and consequent anaemia [12]. Third, although delayed cord clamping seems to increase haematocrit and red blood cell volume, there is no significant difference in clinical outcome such as Apgar scores and requirements for mechanical ventilation even in preterm groups [22]. In addition, clinical benefit from delayed clamping such as fewer intraventricular haemorrhage and blood transfusions is still controversial [22].
Stem cells in human umbilical cord blood
Cellular composition
As mentioned above, the current debate over cord clamping time has been intense due to the value of cord blood for stem cell transplantation, beyond the simple issue of infantile anaemia. The transfusion of blood from the placenta to the infant not only gives the infant extra blood volume to stabilize the circulatory system and enrich the iron stores, it also provides important cellular components such as the haematopoietic stem cells contained in the mononuclear fraction of the umbilical cord blood. UCB has been known to contain enough haematopoietic stem cells to be used for transplantation, but there has been accumulating evidence about the value of other types of UCB-derived stem cells for cell-based therapy. Human UCB plays a significant role as a reservoir of pluripotent stem cells to provide a variety of stem cells such as haematopoietic stem cells, endothelial cell precursors, mesenchymal progenitors and pluripotent/ multipotent lineage stem cells [36–38].
Haematopoietic stem cells from human UCB are not only the most primitive but are also able to repopulate blood lineages over a long period [39–41]. In vitro, human UCB-derived haematopoietic progenitors can proliferate in long-term cultures with various growth factors and possess longer telomeres [42] as well as have a higher colony-forming capability compared to adult stem cells [43]. Therefore, transplantation of human UCB recovers the host reservoir of haematopoietic progenitor cells to a greater degree compared to adult BM stem cells [44]. Even a single human UCB sample can provide enough haematopoietic stem cells for both short- and long-term engraftment [45].
The mononuclear fraction of human UCB is primarily composed of lymphocytes and monocytes [46]. Human UCB lymphocytes are close to the B-cell population but have a lesser absolute T-cell (CD3+) count and a higher CD4+/CD8+ ratio compared to adult peripheral blood [46, 47]. Moreover, UCB-derived B-cell precursors are more immature than adult blood derivatives with comparison of the properties of B-cell differentiation in vitro from CD34+ haematopoietic progenitors [48]. Human UCB possess higher numbers of immature T cells, but lower numbers of mature memory [47, 49] and CD56+ cytotoxic T cells [49] compared to other adult sources. In addition, cord blood lymphocytes express less pro-inflammatory cytokines and their receptors such as interleukin (IL)-2, IL-6, IL-7, tumour necrosis factor (TNF)-α, and interferon-γ[50, 51]. By contrast, they produce higher levels of IL-10 (anti-inflammatory) than lymphocytes in adult blood [51, 52], which down-regulates CD86 expression on dendritic cells (DCs). Consequently, these reactions appear to inhibit the beginning of the T-cell mediated immune reaction [53]. Besides, increased levels of IL-10 probably activate regulatory T cells, which subsequently, redouble inhibition of antigen-specific immune responses [54].
Monocytes and DCs in human UCB are also immature. UCB monocytes do not respond to hepatocyte growth factor (HGF) by which adult monocytes are stimulated [55]. Subsequently, they cannot induce specific adhesion molecules, which are critical for antigen presenting [55]. UCB monocytes also have less expression of the human leucocyte antigen-DR, which subsequently decreases their cytotoxic capacity compared to adult cells [56]. Furthermore, UCB monocytes have difficulty in differentiating into mature DCs to activate naïve T cells, even with special stimulatory cytokines [57]. Unlike adult blood, DCs in cord blood have a lymphoid character that is more likely to be responsible for colonizing neonatal tissue [58]. The lymphoid DCs promote anti-inflammatory T-helper 2 cell reactions, which presumably down-regulate the immune and inflammatory responses along with the naïve T cells [58, 59]. Of interest, natural killer (NK) cells which are able to inhibit T-cell proliferation and decrease TNF-α production [60] highly exist in cord blood [49]. By contrast, cytotoxicity of UCB natural killer cells is much lower compared to adult blood [61].
There are two different subpopulations of mononuclear human UCB cells, namely adherent and floating cells [62]. A significant number of stem cell antigens as well as neural cell markers were detected in the floating population, whereas the adherent cell population mainly contained lymphocytes (∼53%) expressing haematopoietic antigens. These findings suggest not only the existence of a non-haematopoietic subpopulation within mononuclear UCB cells but also their potential to differentiate into cells of other diverse lineages.
Mesenchymal stem cells (MSCs) and MSC-like progenitors can be isolated from amniotic fluid, placenta and Wharton’s jelly [63]. The MSC has also been found as a small fraction of UCB cells [63–65]. Wharton’s Jelly and human umbilical vein endothelial cells, which are closely associated with the umbilical cord, also exhibit stem cell-like properties and may possess equally robust haematopoietic and mesenchymal cell populations distinct from UCB. It is unclear whether any cells apart from those in the UCB are likely to enter the baby at birth and therefore their potential contribution to the child warrants investigation. Consequently the widespread availability of these cells from Wharton’s Jelly and human umbilical vein endothelial cells even after the cord blood is drained should not necessarily act against delayed cord clamping until the interplay between these other non-UCB-derived cells and the baby are known.
MSCs from human UCB have shown outstanding plasticity including the capability for differentiation into cells of the three germ-line derivatives [65–67]. Under specific growth conditions, UCB-MSCs could differentiate into osteogenic and chondrogenic cells [68]. After incubation in neural differentiation medium, human UCB-MSCs expressed a number of neural cell antigens such as glial fibrillary acidic protein (astrocyte marker) and TuJ-1 (neural progenitor marker) as well as intermediate filament proteins reflecting neural differentiation such as vimentin and nestin [69].
Usefulness of umbilical cord blood stem cells
In virtue of the unique and immature features of cord blood, since the first human UCB transplantation to treat a 16-year-old male with acute lymphoblastic leukaemia in 1972 [70], human UCB stem cells have been successfully transplanted to treat a variety of paediatric genetic, haematological, immunological, metabolical and oncological disorders [71–82]. Their ability to differentiate in vitro into non-haematopoietic cells, has led scientists to investigate other potential clinical uses of these cells.
As mentioned above, UCB cells have distinctive properties such as outstanding pluripotency, great proliferative capability, high self-renewal ability, unique T-cell immaturity, diminished capacity for antigen presentation and inflammatory stimulation, extended telomere length, and anti-inflammatory function [12, 83]. Most of all, the innate immaturity of cord blood cells including their immune naïveté may result in the optimal effects of these cells for haematopoietic and somatic organ transplantation compared to other adult stem cells such as BM-derived MSCs. These immature properties contribute to a lower incidence of immune rejection including graft-versus-host disease (GvHD) and/or inhibition of deleterious inflammatory reaction after transplantation even though they come from an allogeneic donor. Consequently, these characteristics could allow for relatively flexible donor-recipient matching requirements, hence leading to a shorter preparatory period for treatment [83]. Rocha et al.[84] revealed that GvHD incidence was significantly lower in children receiving human UCB transplants compared to BM recipients, when both sources were from an HLA-identical sibling. Furthermore, even unrelated HLA-mismatched UCB recipients have a lower GvHD incidence than HLA-identical BM recipients [85].
Encouraging results have been observed when human umbilical cord stem cells were infused intravenously following an ischemic stroke in an experimental animal model. Reductions in infarct volume and restoration of motor impairments were observed and were dependent on the time of administration of the cells and on the cell dose [86–88]. The neuroprotective effect of human UCB stem cells in stroke [89] seems to be related to the induction of the release of neurotrophic growth factors [90] and/or angiogenic factors [91] and a reduction of inflammation [92] rather than to cell replacement.
Human UCB stem cells have also been explored for the treatment of congenital metabolic diseases. For example, Sanfilippo syndrome type B (mucopolysaccharidosis type III B) is an autosomal recessive disorder caused by a deficiency of α-N-acetylglucosaminidase enzyme. Clinical symptoms appear after 2 years of normal development and then progressive cerebral and systemic multiple organ abnormalites are seen. There have been accumulating data supporting the potential of UCB cells for transplantation in this devastating disease in vitro and in vivo[93–95]. Furthermore, in a neonatal rat model of perinatal hypoxic-ischemic brain injury, intraperitoneal transplantation of human cord blood mononuclear cells resulted in incorporation of these cells into the damaged brain and alleviation of the neurological effects of cerebral palsy [96].
First stem cell transplantation at birth
Nature’s first stem cell transplant occurs at birth when the placenta and umbilical cord start contracting and pumping blood toward the newborn. After the blood equilibrates in both compartments, the cord becomes pulseless and the blood flow stops. This phenomenon occurs in most placental mammals and this transfusion of blood is allowed to end physiologically in most species except in human beings. Human beings manipulate the transition from foetal to neonatal life by early clamping of the umbilical cord, meaning that nature’s first stem cell transplant is curtailed, thus depriving infants of additional stem cells.
Regardless, stem cells play an essential role in the development and maturity of many organ systems including the central nervous, respiratory, cardiovascular, haematologic, immunologic and endocrine systems long before birth [97–102]. The aetiology of many diseases of the newborn is related to delayed development and immaturity. In addition, the maturation of every organ system continues after the neonatal period; thus the artificial loss of stem cells at birth could potentially impact later development and predispose infants to diseases such as chronic lung disease, asthma, diabetes, epilepsy, cerebral palsy, Parkinson’s disease, infection and neoplasm.
In particular, the postnatal transfer of UCB cells may be important in preterm infants since the UCB of infants born between 24 to 31 weeks gestation contains a higher concentration of primitive haematopoietic progenitor cells and long-term culture-initiating cells compared with cord blood of infants born closer to term [103]. Therefore, the timing of the clamping of the umbilical cord may be more critical for the transfer of those stem cells to the newborn infant, especially in the preterms, and late clamping of the umbilical cord is a physiologic, safe and inexpensive practice that can avoid the loss of such important cells if harvesting is not planned. Avoiding stem cell loss by the simple practice of delayed cord clamping could potentially decrease the morbidity and mortality associated with many newborn conditions (Table 1).
Table 1.
Common disorders of the newborn related to immaturity of organ systems. There is evidence for benefit from delayed clamping for the first five listed disorders. Only one reference is shown. The remaining five have yet to be conclusively shown to be altered by delayed clamping. Note that the benefit for periventricular leukomalacia has so far only been shown in sheep
| Disorder [Ref.] |
| •Respiratory distress syndrome [13] |
| •Anaemia of prematurity [22] |
| •Intraventricular haemorrhage [24] |
| •Sepsis [104] |
| •Periventricular leukomalacia [105] |
| To be confirmed |
| •Chronic lung disease |
| •Apneas of prematurity |
| •Retinopathy of prematurity |
| •Necrotizing enterocolitis |
| •Patent ductus arteriosus |
One important point to consider is the long-term effects of delayed cord clamping. The present authors are unaware of any studies in either animals or human beings that followed the organism to adulthood. In human beings the longest studies go to 6–7 months and some benefits can still be observed with respect to iron status [27] and motor disability [106]. It is crucial to perform long-term follow-up studies to determine whether the reported benefits of delayed cord clamping are long term, or whether additional benefits may become apparent.
Conclusions
There is no consensus among scientists and clinicians about adequate timing for cord clamping and proper cord blood collection. However, delayed cord clamping and stem cell banking are not mutually exclusive activities, as some authors have suggested [8]. By contrast, the most important thing is how to avoid the loss of valuable stem cells during delivery. First of all, delayed cord clamping should be recommended to populations that have limited access to health care and presumed poor nutrition and those that choose not to bank cord blood for financial or other reasons. Cord clamping also should be delayed appropriately for preterm babies to provide enough blood volume and stem cells except in those who need immediate resuscitation. Unnecessary excessive delayed clamping should be precluded in healthy term cord blood donors. Until now, there has been no consensus about the optimal stem cell amount that newborns need for normal development during the perinatal period. Nonetheless, if cord clamping is performed at the normal time, it would not prevent the adequate stem cell migration that is responsible for newborn babies’ health. In addition, even normal cord clamping would be enough to prevent postnatal anaemia and collect the adequate blood volume for banking in healthy term babies. Nevertheless, if UCB yields a finite number of mononuclear cells at normal time or delayed clamping, newer methods of isolation, preservation and expansion of stem cells derived from UCB and other tissues such as umbilical cord tissue and placenta will decrease dependence on cord blood as a source of stem cells. In the future, residual placental blood volume that remains after delayed cord clamping may yield a sufficient number of stem cells that can be expanded and banked for transplantation. This practice would maintain the physiological benefits of delayed clamping for the infant, yet still yield stem cells for future transplantation use.
In summary, autologous transplantation of stem cells naturally occurs in nature at birth in mammals via the umbilical cord. A delay in the cord blood clamping may increase the stem cell supply to the baby, thereby allowing an innate stem cell therapy that can promote acute benefits in the case of neonatal disease, as well as long-term benefits against age-related diseases. We therefore propose based on the current literature that delayed cord blood clamping should be strongly considered in all healthy babies and when safe to do so in preterm babies. At the same time, we do not wish to discourage the collection of UCB and hope that future studies will show that delayed cord clamping and cord blood collection do not have to be mutually exclusive.
Acknowledgments
No competing financial interests exist. CVB is a consultant for and PRS is cofounder and Chairman of Saneron CCEL Therapeutics, Inc. (SCTI, Tampa, FL, USA). SCTI is a University of South Florida start-up company, which is developing UCB-derived treatments for neurodegenerative and cardiovascular disorders.
References
- 1.Peltonen T. Placental transfusion – advantage an disadvantage. Eur J Pediatr. 1981;137:141–6. doi: 10.1007/BF00441306. [DOI] [PubMed] [Google Scholar]
- 2.Mercer JS. Current best evidence: a review of the literature on umbilical cord clamping. J Midwifery Womens Health. 2001;46:402–14. doi: 10.1016/s1526-9523(01)00196-9. [DOI] [PubMed] [Google Scholar]
- 3.McClausland AM, Holmes F, Schumann WR. Management of cord and placental blood and its effect upon the newborn. Part II. West J Surg Obstet Gynecol. 1950;58:591–608. [PubMed] [Google Scholar]
- 4.Mercer JS, Nelson CC, Skovgaard RL. Umbilical cord clamping: beliefs and practices of American nurse-midwives. J Midwifery Womens Health. 2000;45:58–66. doi: 10.1016/s1526-9523(99)00004-5. [DOI] [PubMed] [Google Scholar]
- 5.McDonald SJ, Middleton P. Effect of timing of umbilical cord clamping of term infants on matenal and neonatal outcomes. Cochrane Database Syst Rev. 2008:CD004074. doi: 10.1002/14651858.CD004074.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Rabe H, Reynolds G, Diaz-Rossello J. Early versus delayed umbilical cord clamping in preterm infants. Cochrane Database Syst Rev. 2004:CD003248. doi: 10.1002/14651858.CD003248.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Capasso L, Raimondi F, Capasso A, et al. Early cord clamping protects at-risk neonates from polycythemia. Biol Neonate. 2003;83:197–200. doi: 10.1159/000068933. [DOI] [PubMed] [Google Scholar]
- 8.Diaz-Rossello JL. Early umbilical cord clamping and cord-blood banking. Lancet. 2006;368:840. doi: 10.1016/S0140-6736(06)69323-9. [DOI] [PubMed] [Google Scholar]
- 9.Hutchon DJ. Commercial cord blood banking: immediate cord clamping is not safe. BMJ. 2006;333:919. doi: 10.1136/bmj.333.7574.919-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levy T, Blickstein I. Timing of cord clamping revisited. J Perinat Med. 2006;34:293–7. doi: 10.1515/JPM.2006.056. [DOI] [PubMed] [Google Scholar]
- 11.Glader BE. Red blood cell aplasias in children. Pediatr Ann. 1990;19:168–9. doi: 10.3928/0090-4481-19900301-05. [DOI] [PubMed] [Google Scholar]
- 12.Schiffman JD. The benefits of cord blood collection. Neoreviews. 2006;7:e564–6. [Google Scholar]
- 13.Usher RH, Saigal S, O’Neil A, et al. Estimation of red blood cell volume in premature infants with and without respiratory distress syndrome. Biol Neonate. 1975;26:241–8. doi: 10.1159/000240735. [DOI] [PubMed] [Google Scholar]
- 14.Yao AC, Wist A, Lind J. The blood volume of the newborn infant delivered by caesarean section. Acta Paediatr Scand. 1967;56:585–92. doi: 10.1111/j.1651-2227.1967.tb15984.x. [DOI] [PubMed] [Google Scholar]
- 15.Yao AC, Lind J. Effect of gravity on placental transfusion. Lancet. 1969;2:505–8. doi: 10.1016/s0140-6736(69)90213-x. [DOI] [PubMed] [Google Scholar]
- 16.Yao AC, Hirvensalo M, Lind J. Placental transfusion-rate and uterine contraction. Lancet. 1968;1:380–3. doi: 10.1016/s0140-6736(68)91352-4. [DOI] [PubMed] [Google Scholar]
- 17.Aladangady N, McHugh S, Aitchison TC, et al. Infants’ blood volume in a controlled trial of placental transfusion at preterm delivery. Pediatrics. 2006;117:93–8. doi: 10.1542/peds.2004-1773. [DOI] [PubMed] [Google Scholar]
- 18.Linderkamp O. Placental transfusion: determinants and effects. Clin Perinatol. 1982;9:559–92. [PubMed] [Google Scholar]
- 19.Nelle M, Zilow EP, Bastert G, et al. Effect of Leboyer childbirth on cardiac output, cerebral and gastrointestinal blood flow velocities in full-term neonates. Am J Perinatol. 1995;12:212–6. doi: 10.1055/s-2007-994455. [DOI] [PubMed] [Google Scholar]
- 20.Papile LA, Rudolph AM, Heymann MA. Autoregulation of cerebral blood flow in the preterm fetal lamb. Pediatr Res. 1985;19:159–61. doi: 10.1203/00006450-198502000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Mercer J, Erickson-Owens D. Delayed cord clamping increases infants’ iron stores. Lancet. 2006;367:1956–8. doi: 10.1016/S0140-6736(06)68858-2. [DOI] [PubMed] [Google Scholar]
- 22.Strauss RG, Mock DM, Johnson KJ, et al. A randomized clinical trial comparing immediate versus delayed clamping of the umbilical cord in preterm infants: short-term clinical and laboratory endpoints. Transfusion. 2008;48:658–65. doi: 10.1111/j.1537-2995.2007.01589.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baenziger O, Stolkin F, Keel M, et al. The influence of the timing of cord clamping on postnatal cerebral oxygenation in preterm neonates: a randomized, controlled trial. Pediatrics. 2007;119:455–9. doi: 10.1542/peds.2006-2725. [DOI] [PubMed] [Google Scholar]
- 24.Rabe H, Reynolds G, Diaz-Rossello J. A systematic review and meta-analysis of a brief delay in clamping the umbilical cord of preterm infants. Neonatology. 2008;93:138–44. doi: 10.1159/000108764. [DOI] [PubMed] [Google Scholar]
- 25.Hutton EK, Hassan ES. Late vs early clamping of the umbilical cord in full-term neonates: systematic review and meta-analysis of controlled trials. Jama. 2007;297:1241–52. doi: 10.1001/jama.297.11.1241. [DOI] [PubMed] [Google Scholar]
- 26.Ceriani Cernadas JM, Carroli G, Pellegrini L, et al. The effect of timing of cord clamping on neonatal venous hematocrit values and clinical outcome at term: a randomized, controlled trial. Pediatrics. 2006;117:e779–86. doi: 10.1542/peds.2005-1156. [DOI] [PubMed] [Google Scholar]
- 27.Chaparro CM, Neufeld LM, Tena Alavez G, et al. Effect of timing of umbilical cord clamping on iron status in Mexican infants: a randomised controlled trial. Lancet. 2006;367:1997–2004. doi: 10.1016/S0140-6736(06)68889-2. [DOI] [PubMed] [Google Scholar]
- 28.Emhamed MO, Van Rheenen P, Brabin BJ. The early effects of delayed cord clamping in term infants born to Libyan mothers. Trop Doct. 2004;34:218–22. doi: 10.1177/004947550403400410. [DOI] [PubMed] [Google Scholar]
- 29.Gupta R, Ramji S. Effect of delayed cord clamping on iron stores in infants born to anemic mothers: a randomized controlled trial. Indian Pediatr. 2002;39:130–5. [PubMed] [Google Scholar]
- 30.Grajeda R, Perez-Escamilla R, Dewey KG. Delayed clamping of the umbilical cord improves hematologic status of Guatemalan infants at 2 mo of age. Am J Clin Nutr. 1997;65:425–31. doi: 10.1093/ajcn/65.2.425. [DOI] [PubMed] [Google Scholar]
- 31.Van Rheenen P, Brabin BJ. Late umbilical cord-clamping as an intervention for reducing iron deficiency anaemia in term infants in developing and industrialised countries: a systematic review. Ann Trop Paediatr. 2004;24:3–16. doi: 10.1179/027249304225013286. [DOI] [PubMed] [Google Scholar]
- 32.Bonnar J, McNicol GP, Douglas AS. The blood coagulation and fibrinolytic systems in the newborn and the mother at birth. J Obstet Gynaecol Br Commonw. 1971;78:355–60. doi: 10.1111/j.1471-0528.1971.tb00285.x. [DOI] [PubMed] [Google Scholar]
- 33.Yao AC, Moinian M, Lind J. Distribution of blood between infant and placenta after birth. Lancet. 1969;2:871–3. doi: 10.1016/s0140-6736(69)92328-9. [DOI] [PubMed] [Google Scholar]
- 34.Wall DA. Issues in the quality of umbilical cord blood stem cells for transplantation: challenges in cord blood banking quality management. Transfusion. 2005;45:826–8. doi: 10.1111/j.1537-2995.2005.05116.x. [DOI] [PubMed] [Google Scholar]
- 35.Diaz-Rossello JL. International perspectives: cord clamping for stem cell donation: medical facts and ethics. Neoreviews. 2006;7:e557–63. [Google Scholar]
- 36.Erices A, Conget P, Minguell JJ. Mesenchymal progenitor cells in human umbilical cord blood. Br J Haematol. 2000;109:235–42. doi: 10.1046/j.1365-2141.2000.01986.x. [DOI] [PubMed] [Google Scholar]
- 37.Berger MJ, Adams SD, Tigges BM, et al. Differentiation of umbilical cord blood-derived multilineage progenitor cells into respiratory epithelial cells. Cytotherapy. 2006;8:480–7. doi: 10.1080/14653240600941549. [DOI] [PubMed] [Google Scholar]
- 38.Kim JW, Kim SY, Park SY, et al. Mesenchymal progenitor cells in the human umbilical cord. Ann Hematol. 2004;83:733–8. doi: 10.1007/s00277-004-0918-z. [DOI] [PubMed] [Google Scholar]
- 39.Todaro AM, Pafumi C, Pernicone G, et al. Haematopoietic progenitors from umbilical cord blood. Blood Purif. 2000;18:144–7. doi: 10.1159/000014438. [DOI] [PubMed] [Google Scholar]
- 40.Nayar B, Raju GM, Deka D. Hematopoietic stem/progenitor cell harvesting from umbilical cord blood. Int J Gynaecol Obstet. 2002;79:31–2. doi: 10.1016/s0020-7292(02)00187-x. [DOI] [PubMed] [Google Scholar]
- 41.Broxmeyer HE, Hangoc G, Cooper S, et al. Growth characteristics and expansion of human umbilical cord blood and estimation of its potential for transplantation in adults. Proc Natl Acad Sci USA. 1992;89:4109–13. doi: 10.1073/pnas.89.9.4109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vaziri H, Dragowska W, Allsopp RC, et al. Evidence for a mitotic clock in human hematopoietic stem cells: loss of telomeric DNA with age. Proc Natl Acad Sci USA. 1994;91:9857–60. doi: 10.1073/pnas.91.21.9857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nakahata T, Ogawa M. Hemopoietic colony-forming cells in umbilical cord blood with extensive capability to generate mono- and multipotential hemopoietic progenitors. J Clin Invest. 1982;70:1324–8. doi: 10.1172/JCI110734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Frassoni F, Podesta M, Maccario R, et al. Cord blood transplantation provides better reconstitution of hematopoietic reservoir compared with bone marrow transplantation. Blood. 2003;102:1138–41. doi: 10.1182/blood-2003-03-0720. [DOI] [PubMed] [Google Scholar]
- 45.Sirchia G, Rebulla P. Placental/umbilical cord blood transplantation. Haematologica. 1999;84:738–47. [PubMed] [Google Scholar]
- 46.Pranke P, Failace RR, Allebrandt WF, et al. Hematologic and immunophenotypic characterization of human umbilical cord blood. Acta Haematol. 2001;105:71–6. doi: 10.1159/000046537. [DOI] [PubMed] [Google Scholar]
- 47.Harris DT, Schumacher MJ, Locascio J, et al. Phenotypic and functional immaturity of human umbilical cord blood T lymphocytes. Proc Natl Acad Sci USA. 1992;89:10006–10. doi: 10.1073/pnas.89.21.10006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hirose Y, Kiyoi H, Itoh K, et al. B-cell precursors differentiated from cord blood CD34+ cells are more immature than those derived from granulocyte colony-stimulating factor-mobilized peripheral blood CD34+ cells. Immunology. 2001;104:410–7. doi: 10.1046/j.1365-2567.2001.01336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.D’Arena G, Musto P, Cascavilla N, et al. Flow cytometric characterization of human umbilical cord blood lymphocytes: immunophenotypic features. Haematologica. 1998;83:197–203. [PubMed] [Google Scholar]
- 50.Zola H, Fusco M, Macardle PJ, et al. Expression of cytokine receptors by human cord blood lymphocytes: comparison with adult blood lymphocytes. Pediatr Res. 1995;38:397–403. doi: 10.1203/00006450-199509000-00021. [DOI] [PubMed] [Google Scholar]
- 51.Gluckman E, Rocha V. History of the clinical use of umbilical cord blood hematopoietic cells. Cytotherapy. 2005;7:219–27. doi: 10.1080/14653240510027136. [DOI] [PubMed] [Google Scholar]
- 52.Rainsford E, Reen DJ. Interleukin 10, produced in abundance by human newborn T cells, may be the regulator of increased tolerance associated with cord blood stem cell transplantation. Br J Haematol. 2002;116:702–9. doi: 10.1046/j.0007-1048.2001.03321.x. [DOI] [PubMed] [Google Scholar]
- 53.Buelens C, Willems F, Delvaux A, et al. Interleukin-10 differentially regulates B7–1 (CD80) and B7–2 (CD86) expression on human peripheral blood dendritic cells. Eur J Immunol. 1995;25:2668–72. doi: 10.1002/eji.1830250940. [DOI] [PubMed] [Google Scholar]
- 54.Asseman C, Powrie F. Interleukin 10 is a growth factor for a population of regulatory T cells. Gut. 1998;42:157–8. doi: 10.1136/gut.42.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jiang Q, Azuma E, Hirayama M, et al. Functional immaturity of cord blood monocytes as detected by impaired response to hepatocyte growth factor. Pediatr Int. 2001;43:334–9. doi: 10.1046/j.1442-200x.2001.01420.x. [DOI] [PubMed] [Google Scholar]
- 56.Theilgaard-Monch K, Raaschou-Jensen K, Palm H, et al. Flow cytometric assessment of lymphocyte subsets, lymphoid progenitors, and hematopoietic stem cells in allogeneic stem cell grafts. Bone Marrow Transplant. 2001;28:1073–82. doi: 10.1038/sj.bmt.1703270. [DOI] [PubMed] [Google Scholar]
- 57.Liu E, Tu W, Law HK, et al. Decreased yield, phenotypic expression and function of immature monocyte-derived dendritic cells in cord blood. Br J Haematol. 2001;113:240–6. doi: 10.1046/j.1365-2141.2001.02720.x. [DOI] [PubMed] [Google Scholar]
- 58.Willing AE, Eve DJ, Sanberg PR. Umbilical cord blood transfusions for prevention of progressive brain injury and induction of neural recovery: an immunological perspective. Regen Med. 2007;2:457–64. doi: 10.2217/17460751.2.4.457. [DOI] [PubMed] [Google Scholar]
- 59.Arpinati M, Green CL, Heimfeld S, et al. Granulocytecolony stimulating factor mobilizes T helper 2-inducing dendritic cells. Blood. 2000;95:2484–90. [PubMed] [Google Scholar]
- 60.El Marsafy S, Dosquet C, Coudert MC, et al. Study of cord blood natural killer cell suppressor activity. Eur J Haematol. 2001;66:215–20. doi: 10.1034/j.1600-0609.2001.066004215.x. [DOI] [PubMed] [Google Scholar]
- 61.Dalle JH, Menezes J, Wagner E, et al. Characterization of cord blood natural killer cells: implications for transplantation and neonatal infections. Pediatr Res. 2005;57:649–55. doi: 10.1203/01.PDR.0000156501.55431.20. [DOI] [PubMed] [Google Scholar]
- 62.Chen N, Hudson JE, Walczak P, et al. Human umbilical cord blood progenitors: the potential of these hematopoietic cells to become neural. Stem Cells. 2005;23:1560–70. doi: 10.1634/stemcells.2004-0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ding DC, Shyu WC, Chiang MF, et al. Enhancement of neuroplasticity through upregulation of beta1-integrin in human umbilical cord-derived stromal cell implanted stroke model. Neurobiol Dis. 2007;27:339–53. doi: 10.1016/j.nbd.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 64.Goodwin HS, Bicknese AR, Chien SN, et al. Multilineage differentiation activity by cells isolated from umbilical cord blood: expression of bone, fat, and neural markers. Biol Blood Marrow Transplant. 2001;7:581–8. doi: 10.1053/bbmt.2001.v7.pm11760145. [DOI] [PubMed] [Google Scholar]
- 65.Yang SE, Ha CW, Jung M, et al. Mesenchymal stem/progenitor cells developed in cultures from UC blood. Cytotherapy. 2004;6:476–86. doi: 10.1080/14653240410005041. [DOI] [PubMed] [Google Scholar]
- 66.Jeong JA, Gang EJ, Hong SH, et al. Rapid neural differentiation of human cord blood-derived mesenchymal stem cells. Neuroreport. 2004;15:1731–4. doi: 10.1097/01.wnr.0000134846.79002.5c. [DOI] [PubMed] [Google Scholar]
- 67.Lee KD, Kuo TK, Whang-Peng J, et al. In vitro hepatic differentiation of human mesenchymal stem cells. Hepatology. 2004;40:1275–84. doi: 10.1002/hep.20469. [DOI] [PubMed] [Google Scholar]
- 68.Kosmacheva SM, Volk MV, Yeustratenka TA, et al. In vitro growth of human umbilical blood mesenchymal stem cells and their differentiation into chondrocytes and osteoblasts. Bull Exp Biol Med. 2008;145:141–5. doi: 10.1007/s10517-008-0028-3. [DOI] [PubMed] [Google Scholar]
- 69.El-Badri NS, Hakki A, Saporta S, et al. Cord blood mesenchymal stem cells: potential use in neurological disorders. Stem Cells Dev. 2006;15:497–506. doi: 10.1089/scd.2006.15.497. [DOI] [PubMed] [Google Scholar]
- 70.Ende M, Ende N. Hematopoietic transplantation by means of fetal (cord) blood. Virginia Med Mon. 1972;99:276–80. [PubMed] [Google Scholar]
- 71.Gluckman E, Broxmeyer HA, Auerbach AD, et al. Hematopoietic reconstitution in a patient with Fanconi’s anemia by means of umbilical-cord blood from an HLA-identical sibling. N Engl J Med. 1989;321:1174–8. doi: 10.1056/NEJM198910263211707. [DOI] [PubMed] [Google Scholar]
- 72.Escolar ML, Poe MD, Provenzale JM, et al. Transplantation of umbilical-cord blood in babies with infantile Krabbe’s disease. N Engl J Med. 2005;352:2069–81. doi: 10.1056/NEJMoa042604. [DOI] [PubMed] [Google Scholar]
- 73.Hall JG, Martin PL, Wood S, et al. Unrelated umbilical cord blood transplantation for an infant with beta-thalassemia major. J Pediatr Hematol Oncol. 2004;26:382–5. doi: 10.1097/00043426-200406000-00010. [DOI] [PubMed] [Google Scholar]
- 74.Kelly P, Kurtzberg J, Vichinsky E, et al. Umbilical cord blood stem cells: application for the treatment of patients with hemoglobinopathies. J Pediatr. 1997;130:695–703. doi: 10.1016/s0022-3476(97)80009-1. [DOI] [PubMed] [Google Scholar]
- 75.Krivit W, Shapiro EG, Peters C, et al. Hematopoietic stem-cell transplantation in globoid-cell leukodystrophy. N Engl J Med. 1998;338:1119–27. doi: 10.1056/NEJM199804163381605. [DOI] [PubMed] [Google Scholar]
- 76.Locatelli F, Rocha V, Reed W, et al. Related umbilical cord blood transplantation in patients with thalassemia and sickle cell disease. Blood. 2003;101:2137–43. doi: 10.1182/blood-2002-07-2090. [DOI] [PubMed] [Google Scholar]
- 77.Myers LA, Hershfield MS, Neale WT, et al. Purine nucleoside phosphorylase deficiency (PNP-def) presenting with lymphopenia and developmental delay: successful correction with umbilical cord blood transplantation. J Pediatr. 2004;145:710–2. doi: 10.1016/j.jpeds.2004.06.075. [DOI] [PubMed] [Google Scholar]
- 78.Staba SL, Escolar ML, Poe M, et al. Cord-blood transplants from unrelated donors in patients with Hurler’s syndrome. N Engl J Med. 2004;350:1960–9. doi: 10.1056/NEJMoa032613. [DOI] [PubMed] [Google Scholar]
- 79.Fruchtman SM, Hurlet A, Dracker R, et al. The successful treatment of severe aplastic anemia with autologous cord blood transplantation. Biol Blood Marrow Transplant. 2004;10:741–2. doi: 10.1016/j.bbmt.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 80.Rocha V, Cornish J, Sievers EL, et al. Comparison of outcomes of unrelated bone marrow and umbilical cord blood transplants in children with acute leukemia. Blood. 2001;97:2962–71. doi: 10.1182/blood.v97.10.2962. [DOI] [PubMed] [Google Scholar]
- 81.Rocha V, Labopin M, Sanz G, et al. Transplants of umbilical-cord blood or bone marrow from unrelated donors in adults with acute leukemia. N Engl J Med. 2004;351:2276–85. doi: 10.1056/NEJMoa041469. [DOI] [PubMed] [Google Scholar]
- 82.Wall DA, Carter SL, Kernan NA, et al. Busulfan/melphalan/antithymocyte globulin followed by unrelated donor cord blood transplantation for treatment of infant leukemia and leukemia in young children: the Cord Blood Transplantation study (COBLT) experience. Biol Blood Marrow Transplant. 2005;11:637–46. doi: 10.1016/j.bbmt.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 83.Newcomb JD, Sanberg PR, Klasko SK, et al. Umbilical cord blood research: current and future perspectives. Cell Transplant. 2007;16:151–8. [PMC free article] [PubMed] [Google Scholar]
- 84.Rocha V, Wagner JE, Jr, Sobocinski KA, et al. Graft-versus-host disease in children who have received a cord-blood or bone marrow transplant from an HLA-identical sibling. Eurocord and International Bone Marrow Transplant Registry Working Committee on Alternative Donor and Stem Cell Sources. N Engl J Med. 2000;342:1846–54. doi: 10.1056/NEJM200006223422501. [DOI] [PubMed] [Google Scholar]
- 85.Rocha V, Cornish J, Sievers EL, et al. Comparison of outcomes of unrelated bone marrow and umbilical cord blood transplants in children with acute leukemia. Blood. 2001;97:2962–71. doi: 10.1182/blood.v97.10.2962. [DOI] [PubMed] [Google Scholar]
- 86.Vendrame M, Cassady J, Newcomb J, et al. Infusion of human umbilical cord blood cells in a rat model of stroke dose-dependently rescues behavioral deficits and reduces infarct volume. Stroke. 2004;35:2390–5. doi: 10.1161/01.STR.0000141681.06735.9b. [DOI] [PubMed] [Google Scholar]
- 87.Newcomb JD, Ajmo CT, Jr, Sanberg CD, et al. Timing of cord blood treatment after experimental stroke determines therapeutic efficacy. Cell Transplant. 2006;15:213–23. doi: 10.3727/000000006783982043. [DOI] [PubMed] [Google Scholar]
- 88.Newman MB, Willing AE, Manresa JJ, et al. Stroke-induced migration of human umbilical cord blood cells: time course and cytokines. Stem Cells Dev. 2005;14:576–86. doi: 10.1089/scd.2005.14.576. [DOI] [PubMed] [Google Scholar]
- 89.Park DH, Borlongan CV, Willing AE, et al. Human umbilical cord blood cell grafts for brain ischemia. Cell Transplant. 2009;18:985–98. doi: 10.3727/096368909X471279. [DOI] [PubMed] [Google Scholar]
- 90.Newman MB, Willing AE, Manresa JJ, et al. Cytokines produced by cultured human umbilical cord blood (HUCB) cells: implications for brain repair. Exp Neurol. 2006;199:201–8. doi: 10.1016/j.expneurol.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 91.Taguchi A, Soma T, Tanaka H, et al. Administration of CD34+ cells after stroke enhances neurogenesis via angiogenesis in a mouse model. J Clin Invest. 2004;114:330–8. doi: 10.1172/JCI20622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Vendrame M, Gemma C, De Mesquita D, et al. Anti-inflammatory effects of human cord blood cells in a rat model of stroke. Stem Cells Dev. 2005;14:595–604. doi: 10.1089/scd.2005.14.595. [DOI] [PubMed] [Google Scholar]
- 93.Garbuzova-Davis S, Gografe SJ, Sanberg CD, et al. Maternal transplantation of human umbilical cord blood cells provides prenatal therapy in Sanfilippo type B mouse model. FASEB J. 2006;20:485–7. doi: 10.1096/fj.05-4684fje. [DOI] [PubMed] [Google Scholar]
- 94.Garbuzova-Davis S, Willing AE, Desjarlais T, et al. Transplantation of human umbilical cord blood cells benefits an animal model of Sanfilippo syndrome type B. Stem Cells Dev. 2005;14:384–94. doi: 10.1089/scd.2005.14.384. [DOI] [PubMed] [Google Scholar]
- 95.Garbuzova-Davis S, Xie Y, Zayko O, et al. Human umbilical cord blood cells in treatment of Sanfilippo syndrome type B. Cell Transplant. 2009;18:214–5. doi: 10.3727/096368914X676916. [DOI] [PubMed] [Google Scholar]
- 96.Meier C, Middelanis J, Wasielewski B, et al. Spastic paresis after perinatal brain damage in rats is reduced by human cord blood mononuclear cells. Pediatr Res. 2006;59:244–9. doi: 10.1203/01.pdr.0000197309.08852.f5. [DOI] [PubMed] [Google Scholar]
- 97.Merkle FT, Alvarez-Buylla A. Neural stem cells in mammalian development. Curr Opin Cell Biol. 2006;18:704–9. doi: 10.1016/j.ceb.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 98.Borok Z, Li C, Liebler J, et al. Developmental pathways and specification of intrapulmonary stem cells. Pediatr Res. 2006;59:84R–93R. doi: 10.1203/01.pdr.0000203563.37626.77. [DOI] [PubMed] [Google Scholar]
- 99.Garry DJ, Olson EN. A common progenitor at the heart of development. Cell. 2006;127:1101–4. doi: 10.1016/j.cell.2006.11.031. [DOI] [PubMed] [Google Scholar]
- 100.Dieterlen-Lievre F. Emergence of haematopoietic stem cells during development. C R Biol. 2007;330:504–9. doi: 10.1016/j.crvi.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 101.Bhandoola A, Von Boehmer H, Petrie HT, et al. Commitment and developmental potential of extrathymic and intrathymic T cell precursors: plenty to choose from. Immunity. 2007;26:678–89. doi: 10.1016/j.immuni.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 102.Murtaugh LC. Pancreas and beta-cell development: from the actual to the possible. Development. 2007;134:427–38. doi: 10.1242/dev.02770. [DOI] [PubMed] [Google Scholar]
- 103.Haneline LS, Marshall KP, Clapp DW. The highest concentration of primitive hematopoietic progenitor cells in cord blood is found in extremely premature infants. Pediatr Res. 1996;39:820–5. doi: 10.1203/00006450-199605000-00013. [DOI] [PubMed] [Google Scholar]
- 104.Mercer JS, Vohr BR, McGrath MM, et al. Delayed cord clamping in very preterm infants reduces the incidence of intraventricular hemorrhage and late-onset sepsis: a randomized, controlled trial. Pediatrics. 2006;117:1235–42. doi: 10.1542/peds.2005-1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Marumo G, Kozuma S, Ohyu J, et al. Generation of periventricular leukomalacia by repeated umbilical cord occlusion in near-term fetal sheep and its possible pathogenetical mechanisms. Biol Neonate. 2001;79:39–45. doi: 10.1159/000047064. [DOI] [PubMed] [Google Scholar]
- 106.Mercer JS, Vohr BR, Erickson-Owens DA, et al. Seven-month developmental outcomes of very low birth weight infants enrolled in a randomized controlled trial of delayed versus immediate cord clamping. J Perinatol. 2010;30:11–6. doi: 10.1038/jp.2009.170. [DOI] [PMC free article] [PubMed] [Google Scholar]


