Abstract
Few community-based HIV interventions exist for Black men at heterosexual risk for HIV. None focus on structural HIV risks such as unemployment and unstable housing. This study involved a pilot evaluation of the MEN [Making Employment Needs] Count HIV intervention, a three session peer counselor-delivered program of HIV risk reduction and gender equity counseling, and employment and housing case management. A single-arm intervention trial of MEN Count was conducted with Black men recruited from a community men’s clinic and social services program. Eligible men were those who reported 2 or more sex partners in the past 6 months and current unemployment and/or recent homelessness. Most participants (68%) had a history of incarceration. Participants (N=50) were surveyed on outcomes at baseline (Time 1), posttest (Time 2; 60–90 days after baseline), and 2 month follow-up (Time 3). The majority of participants were retained in the program (86%) and the final follow-up survey (76%). McNemar tests revealed significant reductions in past 30 day unprotected sex from Time 1 (74%) to Time 2 (47%) and to Time 3 (47%), and in homelessness from Time 1 (58%) to Time 3 (32%). Significant increases in employment from Time 1 (8%) to Time 2 (29%) and Time 3 (32%) were also seen. Participants completed a brief participant satisfaction survey at posttest. Most (n=28, 65%) rated the program as excellent, and an additional 10 (23%) rated it as good. Although there was no significant reduction in multiple sex partners, a trend was observed from Time 1 (56%) to Times 2 (44%) and 3 (42%). Findings suggest that the MEN Count model is a feasible and promising HIV prevention program for Black men at heterosexual risk for HIV. Larger scale implementation and more rigorous evaluation of MEN Count are needed to confirm study findings.
Keywords: HIV/AIDS, Black men, heterosexual risk, structural interventions, behavioral interventions
Introduction
Epidemiologic data indicate that one in 16 Black men in the US is likely to become HIV-infected in his lifetime (Hall, An, Hutchinson, Sansom, 2008). Although most Black men in the US are infected via sexual contact with a male partner, approximately 1 in 5 newly-infected Black men acquired HIV via heterosexual contact (CDC, 2012a). However, there remains a paucity of HIV interventions for Black men at heterosexual risk for HIV (CDC, 2009; Raj & Bowleg, 2012; Henny, Crepaz, Lyles, Marshall, Aupont, Jacobs et al., 2012; Crosby, DiClemente, Charnigo, Snow, Troutman, 2009). To address this gap in the field, the MEN (Making Employment Needs) Count HIV intervention was developed for Black men in urban community clinic or social service (e.g., job placement) agency settings. This paper presents findings from the MEN Count pilot evaluation study.
MEN Count was developed based on both the empirical literature and a theoretical framework comprised of Social Cognitive Theory (SCT; Bandura 1977) and Theory of Gender and Power (TGP; Connell 1987). SCT posits that HIV risk behaviors for heterosexual Black men are affected by social cognitive factors, including peer norms related to condom use and multiple sex partners, HIV risk perceptions, substance use and depression as “triggers” of behavioral risk, and sexual risk reduction self-efficacy (e.g., Noar & Morokoff, 2002; Raj, Reed, Decker, Rothman, Silverman, 2007; Raj, Reed, Santana, Walley, Welles, Horsburgh, Flores, Silverman, 2009; Whitehead, 1997). To better account for social-structural HIV risks, TGP (Connell 1987) was also included. TGP has been used in multiple interventions with heterosexual Black females (see CDC, 2012b for review), suggesting its importance for this male population.
TGP (Connell, 1987) posits three constructs affecting health behavior- 1. Sexual division of labor (gender-based labor imbalances), 2. Sexual division of power (greater male control in heterosexual couples), and 3. Structure of cathexis (traditional gender role ideologies). Numerous studies with heterosexual Black men document associations between HIV sex risk behaviors (non-use of condoms, multiple and concurrent sex partnering) and the latter two constructs. Specifically, sex risk is associated with male partner violence perpetration and male control over condoms or sexual decision-making [division of power], as well as traditional gender role and relationship ideologies such as beliefs regarding male hypersexuality, sexual jealousy, and acceptability and norms of partner violence [cathexis] (e.g., Bowleg et al., 2011; Raj et al., 2007; Raj, Reed, Welles, Santana, Horsburgh, Silverman, 2008; Santana, Raj, Decker, LaMarche, Silverman, 2006). The division of labor construct is predicated on an assumption of greater economic opportunity for males relative to females (Connell, 1987). However, disproportionate risk for incarceration persists for Black men, compromising their equal access to employment and housing. Thus, they may not have greater economic autonomy than women and thus may choose to exert their masculinity through other means such as violence or hypersexuality (Whitehead, 1997). Research documents that the structural factors destabilizing these men’s economic autonomy (i.e., history of incarceration, unemployment, homelessness) are linked to both risky sex and partner violence perpetration (e.g., Adimora, Schoenbach, Martinson, 2006; Adimora, Schoenbach, Doherty, 2006; Raj, Reed, Santana, Welles, Horsburgh, Flores, Silverman, 2008; Lane, Rubinstein, Keefe, Levandowski, Freedman, Rosenthal, Cibula, Czerwinski, 2004; Whitehead, 1997).
The SCT approach was integrated with application of TGP for MEN Count to address traditional gendered risks of TGP (partner violence, masculinity norms) and to provide support against structural TGP risks (unemployment, homelessness). [See Figure 1.] Prior HIV intervention research with heterosexual men in South Africa (Jewkes, Nduna, Levin, Jama, Dunkie, Puren, Duvvury, 2008) and Black heterosexual men in the US (Frye, Henny, Bonner, Williams, Bond, Hoover, et al., 2012) documents the utility of a gendered prevention approach, though neither of these evaluated programs included focus on structural factors. Interventions to affect structural risks of housing and employment have proved useful with Black men being released from prison (Wolitski, et al., 2006) though this intervention did not included gendered risk considerations. MEN Count considers behavioral, gender and structural HIV risks for use with Black heterosexual men. [See Figure 1.] This study involves pilot testing of MEN Count in terms of its short-term impact on risky sex and feasibility of implementation.
Figure 1. Application of Social Cognitive Theory (SCT) and Theory of Gender and Power (TGP) to Understand Black Heterosexual Men’s Risk for HIV.
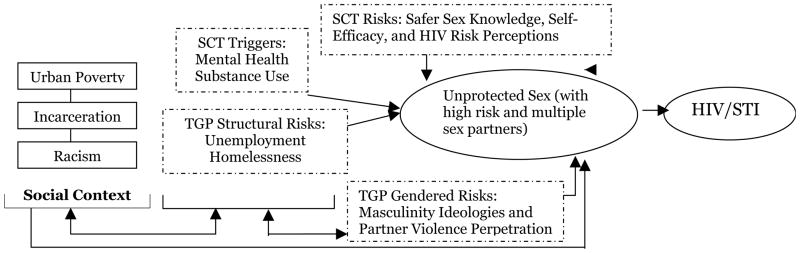
*Dashed Line around box indicates factors targeted by MEN Count Intervention
Methods
A single-armed intervention design was used to evaluate the MEN Count intervention, using baseline, posttest and follow-up assessments over a 5 month timeframe. Participants were recruited over 6 months in 2009–10 from an urban community health center (UCHC) in a large northeastern city. This UCHC is known for its men’s health and social service program operating in a community disproportionately affected by HIV, poverty and unemployment (BPHC, 2010). Participants were recruited sequentially from primary care waiting rooms by project staff. Recruitment hours and days varied to reduce biases in recruitment. Those indicating interest met with research staff for private eligibility screening. Eligibility criteria were adult age (18 years or older), reporting 2+ female sex partners and any unprotected vaginal sex in the past 6 months, and reporting no full time employment or any days homeless in the past 6 months. Eighty-five men were screened for participation; 68 were eligible, and 50 agreed to participate.
Consent and Study Procedure
Informed consent was obtained from those eligible and willing to participate. For those agreeing to the STI/HIV testing as part of the study, a Health Insurance Portability and Accountability Act of 1996 (HIPAA) authorization was obtained to allow for medical record review. A federal Certificate of Confidentiality was also obtained, as illicit activities were assessed on the survey.
Following acquisition of informed consent and HIPAA authorization, HIV/STI (Chlamydia, gonorrhea and syphilis) testing was conducted by UCHC staff, and survey assessments were conducted by the research team. [NOTE: For those tested and found to be STI+, notification and treatment was conducted in accordance with UCHC clinic protocols. No one was found to be HIV+ in this study.] The computerized survey was conducted in a private room and assessed demographics, sex risk behaviors, and theory-generated predictors of sex risk (see Figure 1). Participants were provided with a $25 gift card incentive payment for their baseline survey participation and escorted to the MEN Count Peer Counselor to schedule their first intervention session.
Following completion of the intervention, 2–2.5 months after baseline assessment, a posttest computerized survey was conducted on all study outcomes. At posttest, participants were also asked to complete a brief survey on their perceptions of the MEN Count intervention; this served as the participant satisfaction survey. They were again given a $25 gift card incentive payment for survey participation. Of the 50 participants, 34 (68%) were retained for posttest.
Two months following posttest (4–5 months post-baseline), participants were again asked to participate in a computerized survey which used the same items as those used in posttest, and HIV/STI testing was again conducted if HIPPA was obtained. Finally, a brief open-ended interview was conducted by research staff for feedback on how they felt the intervention affected their housing, employment, and sexual relationships with women. Participants not retained at posttest were also asked to complete the participant satisfaction survey at final follow-up survey. For this final assessment, they received a $35 gift card incentive payment. Of the 50 participants, 38 (76%) were retained for the 2 month follow-up assessment; 29 participants provided data for posttest and follow-up.
All data were labeled by a unique identifier to link participant data across assessment times and to HIV/STI tests without use of names. These procedures were approved by the institutional review board of Boston University Medical Campus.
The MEN Count Model
MEN Count integrates a) HIV risk reduction and gender-equity counseling, inclusive of considerations of how gender inequities and masculinity ideologies impede sexual risk reduction practices, with b) employment and housing case management, to promote HIV risk reduction behaviors among Black men at heterosexual risk for HIV. The program was delivered by a trained Peer Counselor via 3 60 minute sessions, with 1–2 brief (10 minute) check-in meetings between the sessions, over a 60–90 day timeframe. HIV risk behavior assessments were conducted with participants at each session (10–20 minutes), but with consideration of healthy relationship dynamics and stability of life context. To provide greater focus on gendered risks for HIV, sessions 2 and 3 also included a 10–15 minute discussion of the nature of participants’ relationships with women with regard to trust and respect. Emphasis was placed on the importance of respecting a sex partner as you want to be respected, emotionally, physically and sexually. Strategies for averting physical and sexual violence were noted (e.g., walking away, confirming sexual consent). Each session also included a 15–20 minute assessment of the participant’s current housing and employment situations. Case managers processed with participants the pros and cons of these situations and supported them in problem solving solutions for stabilizing their existing situation (e.g., not walking away from a safe job or housing situation) or to identify a better situation. Action plans developed by participants at the end of each session focused on action steps for procuring or maintaining stable housing and employment, and healthy sexual relationships. Men seeking employment were linked to services to develop and refine resumes and develop interview skills. All men completing the program were offered a letter that documented their responsible participation and completion of the MEN Count intervention, for use with employers, landlords and the criminal justice system. [See Table 1 for details.]
Table 1.
Overview of Approaches Undertaken in MEN Count Intervention Intensive Sessions and Check In Sessions
| Individual Sessions | Check-In Sessions |
|---|---|
|
Sequentially and Briefly-
|
| NOTE: Sessions are repetitive to build participant skills to conduct their own personalized risk assessment, problem solving and action plan development so they can continue this approach in their lives subsequent to program completion. All elements described above were included in every session, but the risk assessment had greater focus in Session 1 and relationship violence was not assessed until Session 2 to ensure rapport was established with the participant first. | NOTE: Check-ins offer a supportive and resiliency focused approach to maintain participants’ perceptions regarding their capacity to create change in their lives in the face of social disparities. |
Survey Measures
Single item measures were used to assess age, income, education, employment, housing and relationship/family characteristics. Items on participants’ past 30 day binge alcohol use (5 or more drinks in a day), marijuana use, and cocaine use were used to assess substance use. Violence items included yes/no assessments of childhood victimization, witnessing violent crime in the community, and partner violence perpetration. History of incarceration was assessed using ever and past year items. To create the unprotected sex with a woman outcome measure, number of unprotected anal of vaginal sex episodes with a woman in the past 30 days was calculated and dichotomized as any versus no unprotected sex. Those reporting more than one sex partner in the past 30 days were defined as having multiple female sex partners. HIV/STI results were obtained from participant medical records, for those agreeing.
Process Evaluation and Quality Assurance Component
To ensure high quality implementation of program and adherence to curriculum, the Peer Counselor maintained case notes on points discussed, action plans created, and referrals provided for each client session. These were monitored and weekly meetings were conducted with the Peer Counselor to review cases. Attendance records were maintained by the Peer Counselor. A brief participant satisfaction survey was conducted which included four open-ended questions were conducted by research staff to assess participants’ perceptions of changes in key outcomes (safer sex, employment, housing and relationships with women) as a consequence of the program. Triangulation of quantitative outcome findings with these qualitative outcome data helped validate observed intervention effects.
Data Analysis
Quantitative outcome data were analyzed via McNemar tests to determine whether changes in outcome variables were significant from Time 1 to Time 2 and from Time 1 to Time 3. Significance was set at p<.05. Attrition analyses were also conducted to determine if there were significant differences between participants who were retained or not retained in the study on study outcomes and age. No differences were identified. All quantitative analyses were conducted using SPSS version 19.0. Open-ended responses from the perceptions data were analyzed qualitatively by listing quoted responses by question. Two coders independently reviewed quotes by question to determine themes; themes identified focused on intervention effects on HIV risk, employment, homelessness, and relationships with women. Example quotes were selected by coders to reflect identified themes.
Results
Demographic Profile
Participants were aged 18–54 years. Few reported employment or housing (n=4, 8%, respectively). [See Table 2.] Half of the men (n=25, 50%) had at least one child under age 18 years. Only 5 of these resided with this child, though 18 reported contributing financially to their support. Most participants (n=33, 66%) reported current involvement in a steady relationship with a female partner.
Table 2.
Demographic Profile of MEN Count Pilot Participants (N=50)
| n (%) | |
|---|---|
|
| |
| US Born | 47 (94%) |
|
| |
| Education | |
| Less than High School | 20 (40%) |
| GED/High School Diploma | 17 (34%) |
| Some College/College Degree | 13 (26%) |
|
| |
| Legally Employed | |
| Full-Time Employed | 2 (4%) |
| Part-Time Employed | 2 (4%) |
| Income, Not Via Legal Employment | 6 (12%) |
| No Income | 40 (80%) |
|
| |
| Predominant Living Situation, Past 90 Days | |
| Renting House or Apartment | 4 (8%) |
| Residing with Family or Friends | 22 (44%) |
| Homeless on the Streets or in Shelter | 23 (46%) |
Substance Use, Incarceration, Sex Risk and STI
Almost half of participants reported binge alcohol use (5+ drinks in one day) (n=21; 42%) and marijuana use (n=23, 46%), in the past 30 days. More than half (n=34, 68%) had a history of incarceration. Half (n=28, 56%) reported two or more partners in the past 30 days. Most (n= 37, 74%) reported unprotected sex in this same timeframe. Of the 32 men tested for STI at baseline, 4 (13%) were positive.
Pilot Evaluation Findings
Unprotected sex significantly decreased from Time 1 to Time 2 (p=.02) and from Time 1 to Time 3 (p=.04). [See Table 3.] Reports of multiple sex partnering did not significantly reduce over time, though a trend of reduction was observed. Employment significantly increased from Time 1 to Time 2 (p=.01) and from Time 1 to Time 3 (p=.01). Homelessness did not significantly decrease from Time 1 to Time 2, but did from Time 1 to Time 3 (p=.04). Corresponding with these quantitative findings, in the brief open-ended items on these issues at post-test, participants described how MEN Count helped them to consider their sex risk more carefully and helped them to procure or maintain stable employment and housing. [See quotes in Table 3.] Quantitative analysis of reductions in partner violence were not able to be conducted due to the small number of men reporting past 30 day partner violence at baseline (n=5). However, in open-ended responses, participants did describe how the program heightened their consideration of their female partners and provided tools for them to avoid relationship violence.
Table 3.
MEN Count Pilot Evaluation Findings: Change Over Time in Unprotected Sex, Employment, and Homelessness
| Time 1 (T1) N=50 n (%) | Time 2 (T2) n=34 n (%) | Time 3 (T3) n=38 n (%) | p-value (T1–T2); p-value (T1–T3) | Quotes from participants at post-test on their perceptions of the program’s utility on study outcomes. | |
|---|---|---|---|---|---|
| Unprotected Sex, Past 30 Days | 37 (74%) | 16 (47%) | 18 (47%) | .02 .04 |
[The Program] showed me that living on the edge, it’s kids’ stuff. It’s time to grow up. I don’t want my son to come to my funeral after I died from AIDS. I use condoms now. I have one relationship now, and it’s because of this program. |
| Multiple Sex Partners, Past 30 Days | 28 (56%) | 15 (44%) | 16 (42%) | NS NS |
|
| Currently Employed | 4 (8%) | 10 (29%) | 12 (32%) | .01 .01 |
Overall the program really got me confident again about the workforce… helped me with my resume. [The Program] helped with my needing to maintain my job…, despite other people or issues at the job. |
| Any Homeless Days, Past 30 Days | 29 (58%) | 16 (47%) | 12 (32%) | NS .04 |
[The Program] gave me a drive to want to do more. [I] went downtown to apply for housing… I want my kids to come see me and have rooms of their own. [The Program] helped [me] realize I can’t go [from] place-to-place… I have to take care of myself. I don’t have a lot of homeless days now. Some days I stay at my parents’ place. I am pushing to get my own place- maybe with my twin brother. |
| Intimate Partner Violence Perpetration, Past 30 Days* | - | - | - | - |
[The program] opened up a sense of the threat of [relationship] violence. It mentioned how you can channel this anger into something non-harmful and what kinds of steps can be taken to avoid this [violence]. [The program] made me aware of females’ feelings… I have, like, an intervention of how to treat them, treat them like an equal. |
Quantitative analysis of reductions in partner violence were not able to be conducted due to the small number of men reporting past 30 day partner violence at baseline (n=5). However, open-ended responses from participants were recorded on how the intervention affected relation dynamics and intimate partner violence.
Program Retention and Participant Satisfaction
All 50 study participants completed Session 1; 38 participated in Session 2, and 42 were retained for Session 3. Review of case notes across participants revealed good adherence to curriculum in sessions. Of those providing participant satisfaction data (n=43), the majority (n=28, 65%) rated the program as excellent. An additional 10 (23%) rated it as good. (See Table 4.)
Table 4.
Participant Satisfaction with MEN Count Program (n=43)
| Excellent | Good | Fair | Poor | |
|---|---|---|---|---|
| Overall, how would you rate the MEN Count program? | 28 (61%) | 10 (22%) | 4 (9%) | 1 (2%) |
| How much did the program meet your HIV and sexual health concerns? | 20 (47%) | 12 (28%) | 11 (26%) | 0 (0%) |
| How much did the program meet your employment concerns? | 12 (28%) | 9 (21%) | 15 (35%) | 7 (16%) |
| How much did the program meet your housing concerns? | 10 (23%) | 9 (21%) | 14 (33%) | 10 (23%) |
| Was the peer counselor knowledgeable about topics discussed in your meetings? | 22 (51%) | 10 (23%) | 10 (23%) | 1 (2%) |
| How useful were your action plans in helping you to achieve your program goals? | 12 (28%) | 14 (33%) | 14 (33%) | 3 (7%) |
| Definitely Yes | Probably Yes | Not Sure | No | |
| Has this program helped you have lasting positive changes in your life? | 20 (47%) | 12 (28%) | 10 (23%) | 1 (2%) |
| Do you think this program should be continued at the Health Center? | 31 (67%) | 7 (15%) | 5 (11%) | 0 (0%) |
Discussion
Findings from the current study suggest the potential effectiveness of this community-based MEN Count model in addressing behavioral and structural risks for HIV among Black heterosexual men. Further, study findings document good response to and retention in this multisession 2–3 month program without incentives for program participation. Consistent with previous effective HIV interventions for Black men, this intervention involved linkage to medical services, male program staff, and shorter-term follow-up periods (Henny et al., 2012). Building upon previous work, this study documents the utility of including a combination of behavioral, gender equity and structural risks for HIV prevention with Black men, in accordance with an SCT-TGP framework. While the study was too small to test whether observed effects of the intervention were attributable to changes in SCT and TGP constructs, intervention content related to these constructs did appear to be meaningful to men’s perceptions of their HIV risk. Overall, these findings indicate that the MEN Count model can support the President’s National HIV/AIDS strategy which prioritizes community-based HIV prevention (the White House, 2010).
Significant increases in housing and employment as a consequence of MEN Count participation were a goal but nonetheless were surprising in a very difficult economic environment- 2009/10 a period with rapidly increasing unemployment rates. The Peer Counselor’s provision of social support and linkage to job opportunities appeared to assist men in retaining existing if not optimal housing and employment, as well as in attempting to acquire new housing and employment. Such attempts appear to have been more successful for employment than housing. Subsidized housing programs prioritize women with children. Fathers not residing with their minor-aged children have low likelihood of procuring their own subsidized housing, especially if they had a history of incarceration (Johnson, 2010). These findings indicate that, while structural interventions such as housing placement may be useful to support HIV prevention among Black men (Blankenship, Friedman, Dworkin, Mantell, 2006), they are unlikely to occur unless policies inhibiting Black men’s access to such opportunities change. Greater support for stabilization of men’s housing, as done in MEN Count, may be required but in the absence of policy change may be limited in utility. Nonetheless, we would recommend retaining the approach, as supportive retention of dependent housing did appear to reduce number of homeless days for participants. Additionally, participants viewed the program as centered on HIV, possibly because of the clinical setting and limited support for housing or employment in the clinical context. The intervention may be better-suited for placement in a community program focused on employment or job training for men, and HIV counseling and testing could then be included in MEN Count as part of the community-based program. This approach would be in line with President’s National HIV/AIDS strategy which encourages placement of HIV testing in non-traditional community settings (the White House, 2010).
Study limitations include lack of a control condition, which could result in observed findings being attributable to factors other than the MEN Count program (e.g., testing effects). However, qualitative data support quantitative findings attributing observed changes to program involvement, though qualitative data were limited in scope. Fourteen percent loss of study participants at final follow-up may have resulted in a bias toward retaining individuals most amenable to change. However, 43/50 participants (86%) were able to be reached for assessment over our two survey time points. The sample size was small and likely limited in generalizability. Small sample size prohibited our ability to conduct dose analyses or analyses inclusive of all three assessment time points simultaneously. Outcomes are solely based on self-report, and are thus subject to social desirability and recall biases. Lack of audiotaping of qualitative interviews and counseling sessions impeded gathering of quotes and real time quality assurance of program delivery. Audiotaping was not possible as it is viewed as invasive in this population. Further research is needed to test MEN Count with a larger sample and more rigorous evaluation. Nonetheless, given the paucity of community-based interventions for Black men at heterosexual risk for HIV, MEN Count offers a promising approach to help address the generalized epidemic of HIV in urban Black communities in the US.
Acknowledgments
We would like to thank the staff and patients of Whittier Street Health Center for supporting this study, as well as our MEN Count participants for providing their time and insight into the project. We would also like to acknowledge the contributions of Elizabeth Reed, Lisa Bowleg and Wanda Allen in helping us interpret and disseminate study findings within the communities in which this research occurred. This study was funded by the National Institute of Mental Health grant R21MH085614 (PI: Anita Raj); additional support for authors’ time to develop this paper also came from the National Institute of Mental Health Grant R01MH096657 (PI: Anita Raj).
References
- Adimora AA, Schoenbach VJ, Martinson FE, Coyne-Beasley T, Doherty I, Stancil TR, Fullilove RE. Heterosexually transmitted HIV infection among African Americans in North Carolina. Journal of Acquired Immune Deficiency Syndrome. 2006;41(5):616–23. doi: 10.1097/01.qai.0000191382.62070.a5. [DOI] [PubMed] [Google Scholar]
- Adimora AA, Schoenbach VJ, Doherty IA. HIV and African Americans in the southern United States: Sexual networks and social context. Sexually Transmitted Diseases. 2006;33(suppl 7):S39–45. doi: 10.1097/01.olq.0000228298.07826.68. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-Efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Blankenship KM, Friedman SR, Dworkin S, Mantell JE. Structural interventions: Concepts, challenges and opportunities for research. Journal of Urban Health. 2006;83(1):59–72. doi: 10.1007/s11524-005-9007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boston Public Health Commission (BPHC) Health of Boston 2010. 2010 [cited 2012 November 16]. Retrieved from http://www.bphc.org/about/research/hob2010/Pages/Home.aspx.
- Bowleg L, Teti M, Massie JS, Patel A, Malebranche DJ, Tschann JM. “What does it take to be a man? What is a real man?”: ideologies of masculinity and HIV sexual risk among Black heterosexual man. Culture, Health and Sexuality. 2011;13(5):545–59. doi: 10.1080/13691058.2011.556201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDCa) Diagnoses of HIV Infection and AIDS in the United States and Dependent Areas, 2010. HIV Surveillance Report. 2012a;22 [cited 2012 November 16]. Retrieved from: http://www.cdc.gov/hiv/surveillance/resources/reports/2010report/index.htm. [Google Scholar]
- Centers for Disease Control and Prevention (CDCb) Best-Evidence Interventions. HIV Prevention Research Synthesis Project. 2012b [cited 2012 November 16]. Retrieved from: http://www.cdc.gov/hiv/topics/research/prs/RRcomplete-list.htm.
- Centers for Disease Control and Prevention (CDC) Characteristics Associated with HIV Infection among Heterosexuals in Urban Areas with High AIDS Prevalence --- 24 Cities, United States, 2006—2007. Morbidity and Mortality Weekly Report (MMWR) 2011;60(31):1045–1049. [PubMed] [Google Scholar]
- Connell RW. Gender and Power: Society, the Person, and Sexual Politics. Stanford (CA): Stanford University Press; 1987. [Google Scholar]
- Crosby R, DiClemente RJ, Charnigo R, Snow G, Troutman A. A brief, clinic-based, safer sex intervention for heterosexual African American men newly diagnosed with an STD: A randomized controlled trial. American Journal of Public Health. 2009;99:S96–S103. doi: 10.2105/AJPH.2007.123893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye V, Henny K, Bonner S, Williams K, Bond KT, Hoover DR, Lucy D, Greene E, Koblin BA & the Straight Talk Study Team. “Straight Talk” for African American heterosexual men: Results of a single-arm behavioral intervention trial. AIDS Care. 2012 doi: 10.1080/09540121.2012.722605. [cited 2012 November 16]. Retrieved from: http://dx.doi.org/10.1080/09540121.2012.722605. [DOI] [PMC free article] [PubMed]
- Henny KD, Crepaz N, Lyles CM, Marshall KJ, Aupont LW, Jacobs ED, Liau A, Rama S, Kay LS, Willis LA, Charania MR. Efficacy of HIV/STI behavioral interventions for heterosexual African American men in the United States: a meta-analysis. AIDS and Behavior. 2012;16(5):1092–114. doi: 10.1007/s10461-011-0100-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane SD, Keefe RH, Rubinstein RA, Levandowski BA, Freedman M, Rosenthal A, Cibula DA, Czerwinski M. Marriage promotion and missing men: African American women in a demographic double bind. Medical Anthropology Quarterly. 2004;18(4):405–428. doi: 10.1525/maq.2004.18.4.405. [DOI] [PubMed] [Google Scholar]
- Jewkes R, Nduna M, Levin J, Jama N, Dunkie K, Puren A, Duvvury N. Impact of Stepping Stones on incidence of HIV and HSV-2 and sexual behaviour in rural South Africa: cluster randomised controlled trial. British Medical Journal. 2008;337:a506. doi: 10.1136/bmj.a506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson WE, editor. Social Work With African American Males Health, Mental Health, and Social Policy. Oxford University Press; 2010. [Google Scholar]
- Noar SM, Morokoff PJ. The relationship between masculinity ideology, condom attitudes, and condom use stage of change: A structural equation modeling approach. International Journal of Men’s Health. 2002;1(1):43–58. [Google Scholar]
- Raj A, Bowleg L. Heterosexual risk for HIV among Black men in the United States - a call to action against a neglected crisis in black communities. American Journal of Men’s Health. 2012;6(3):178–81. doi: 10.1177/1557988311416496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raj A, Reed E, Decker MR, Rothman EF, Silverman JG. The contexts of condom use and non-use among adolescent male perpetrators of dating violence. AIDS Care. 2007;19(8):970–3. doi: 10.1080/09540120701335246. [DOI] [PubMed] [Google Scholar]
- Raj A, Reed E, Santana MC, Walley AY, Welles SL, Horsburgh CR, Flores SA, Silverman JG. Associations of binge alcohol use with HIV/STI risk and diagnosis among African American men who have sex with women. Drug and Alcohol Dependence. 2009;101(1–2):101–6. doi: 10.1016/j.drugalcdep.2008.11.008. [DOI] [PubMed] [Google Scholar]
- Raj A, Reed E, Santana MC, Welles SL, Horsburgh CR, Flores SA, Silverman JG. History of incarceration and gang involvement are associated with recent STD/HIV diagnosis in African American men. Journal of the Acquired Immune Deficiency Syndrome. 2008;47(1):131–4. doi: 10.1097/QAI.0b013e31815a5731. [DOI] [PubMed] [Google Scholar]
- Raj A, Reed E, Welles SL, Santana MC, Horsburgh CR, Silverman JG. Intimate partner violence perpetration, risky sexual behavior and STI/HIV diagnosis among heterosexual African American men. American Journal of Men’s Health. 2008;2(3):291–5. doi: 10.1177/1557988308320269. [DOI] [PubMed] [Google Scholar]
- Santana MC, Raj A, Decker MR, LaMarche A, Silverman JG. Masculine gender roles associated with increased sexual risk and intimate partner violence perpetration among young adult men. Journal of Urban Health. 2006;83(4):575–85. doi: 10.1007/s11524-006-9061-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead TL. Urban low-income African American men, HIV/AIDS, and gender identity. Medical Anthropology Quarterly. 1997;11(4):411–47. doi: 10.1525/maq.1997.11.4.411. [DOI] [PubMed] [Google Scholar]
- The White House. National HIV/AIDS strategy for the United States. Washington, DC: Office on National AIDS Policy; 2010. [cited 2012 November 16]. Retrieved from: http://www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf. [Google Scholar]
- Wolitski RJ The Project START study group. Relative efficacy of a multisession sexual risk reduction intervention for young men released from prison in 4 states. American Journal Public Health. 2006;96(10):1845–1861. doi: 10.2105/AJPH.2004.056044. [DOI] [PMC free article] [PubMed] [Google Scholar]


