Abstract
Background
Day case surgery services are increasing all over the world. The prevalence of postoperative pain after day surgery is found to be high. Little is known about the prevalence of postoperative pain, in Kenya, after day case surgeries.
Objective
To investigate the prevalence of postoperative pain after day surgery at Aga Khan University Hospital (AKUH), Nairobi, to determine the severity/intensity of postoperative pain following day case surgery
Methods
Consecutive sampling was carried out until sample size of one hundred and fifty patients was achieved. The purpose and nature of the study was explained to patients before informed consent was obtained. They were shown how to score their pain using a visual analogue scale prior to the surgical procedure. A questionnaire was used to collect data from the patients. Follow up information was obtained through telephone interviews at 24 and 48 hours, after discharge from the day surgery unit.
Results
The prevalence of postoperative pain after day care surgery was found to be 58% within 30minutes postoperatively, 55.3% after 24 hours, and 34.7% after 48 hours following surgery. The prevalence of moderate to severe postoperative pain was 13% after 24 hours, and 11.7% after 48 hours.
Conclusion
The overall prevalence of postoperative pain after day surgery at the Aga Khan University Hospital, Nairobi was noted to be different from what has been reported in the literature. The prevalence of moderate and severe pain however, is less than reported in the literature.
Keywords: Day case surgery, postoperative pain
Introduction
Pain is one of the most common, unpleasant and frightening symptoms associated with surgery. It has been postulated that the unpleasantness and the fear of pain may lead to chronic pain even when few or no organic findings exist to explain the patient's degree of stress1,2,3. This association between fear of pain and chronic pain can be demonstrated by the “Fear avoidance model”. This model, based on these three studies, proposes that several ways through which pain-related fear might lead to disability through catastrophic thinking, escape and avoidance behaviours4,5,6. However, the patients fear may be due to pessimism (that of long-term consequences of the operation, association with more pain, poor global recovery, and worse quality of life later), whereas optimism is associated with better recovery and higher quality of life7. This makes pain control one of the key factors determining a successful day surgery service8, 9.
Persistent postoperative pain is an unpleasant sensory and emotional experience following surgery. It is thought to be caused by nerve injury10, 11, and neuroplastic change in the central nervous system induced by high-intensity pain in the first days following surgery12. Currently pain literature supports the concept that even a brief experience of moderate to severe acute pain can lead to reorganization of neurons in the higher centre13,14,15.
Several reports have shown that persistent or uncontrolled pain is associated with increased incidence of postoperative nausea and delirium16, 17, prolonged post-anaesthesia care unit (PACU) stay and delayed discharge from an ambulatory facility 18. Inadequate pain control may delay resumption of normal activities7, 19.
Postoperative patient satisfaction has been shown to be related to the level of pain control8. Therefore availability of adequate postoperative pain control preferably using oral analgesics which are effective, safe, and easily managed by patients at home, is one of the criteria for a surgical procedure to be performed as a day surgery case 20, 21.
This study aimed at investigating the prevalence of postoperative pain following day surgery in the first 48 hours at Aga Khan University Hospital, Nairobi.
Rationale of the study
Literature review suggests that postoperative pain following day surgery remains a challenge in the developed and developing world. The overall prevalence of moderate to severe postoperative pain reported in the literature is 17% to 40%, with one study revealing an incidence of up to 60% in the first 24 hours23. Many complicated surgical procedures are being performed on day care basis 23, 28, 30. This continues to pose a problem of pain management at home after surgery. Very little information can be found about the magnitude of this problem in the developing world.
At Aga Khan University hospital, Nairobi, the day surgery services began in 2005 and over the years the number of day cases has increased to about 100 patients operated per month30. Despite this increase in day case surgeries performed, there is no data investigating postoperative pain or any other postoperative complication after day surgery. It is imperative that such information is gathered in order to manage patient's pain adequately.
We hypothesized that 10% of the patients undergoing day surgery procedures at Aga Khan University hospital would have moderate to severe pain (score 4–10 on the VAS) after the surgical procedure within the first 48 hours. This presumed lower prevalence would be due to the tendency that although we generally use analgesics similar to the centres described above, similar complex day-case surgical procedures are not yet performed at Aga Khan University Hospital, Nairobi.
There is no data on the prevalence of postoperative pain in Kenya and East Africa. There is also paucity of data regarding the management of post operative pain following day surgery and the types of surgical procedures that can be performed as day care surgery at the Aga Khan University hospital. The study therefore will assist us in improving our facilities for this steadily growing service.
Methods
After obtaining approval from the Aga Khan University research and research ethics committee in January 2009 and written informed consent from the patients, data collection was conducted between March and June 2009, both months inclusive.
This was a prospective cross-sectional survey that was determining the prevalence of postoperative pain, following day surgery in the first 48 hours at Aga Khan University Hospital, Nairobi. Patients were seen in the surgical outpatient clinics or in the Accident & Emergency department and scheduled for day surgery procedures. The procedures were performed in theatre, they recovered in the PACU and were discharged from the day surgery unit (DSU) to go back home. Patients were told about the study, its purpose and the need to contact them through their cell phones or home telephones for follow up. Consent was sought after these explanations. Patients were shown how to score pain using a Visual Analogue Score (VAS) scale (0=no pain, 1–3=mild pain, 4–6=moderate pain, 7–10=severe pain) before they went for the surgical procedure, then asked to score pain once they were back in the DSU. The type of anaesthesia administered was not regulated by this study. The choice of technique and agents to be used was left to the individual anaesthetist. After surgery, the patients stayed in the recovery room and vital signs were taken and postoperative pain was managed according to what the anaesthetist in charge of that individual patient recommended. When the patients sufficiently recovered, they were transferred to the day surgery unit for complete recovery. Further postoperative pain therapy was given if required during this time in the day surgery unit, as per patients' treatment sheet. Before discharge, the patients were provided with discharge medication according to what the anaesthetist or surgeon had prescribed.
Postoperatively, in the DSU, pain was scored on arrival, after 30minutes, one hour, two hours and at discharge from the recovery room. Patients were asked about their pain intensity at arrival and at discharge from the recovery room. Postoperative telephone calls to the patients were made after 24 and 48 hours and they were asked to give a report of the progress of the postoperative pain while at home.
The patients included in the study were all adult patients from ages of 18 to 68 years who were scheduled for day surgical procedures at Aga Khan University hospital, Nairobi.
The patients excluded from the study were patients under the age of 18 years as well as patients with mental and psychological problems, with whom communication would be a problem.
Participant flow diagram is shown in figure 1
Figure 1.
Participant flow chart
Data was analysed using STATA version 10 (StataCorp, Texas). ANOVA was used to determine if differences in the means of the vital signs were statistically significant amongst the different intensities of pain. Fisher's test was used to determine the relation between vital signs and pain intensity in the recovery room and DSU. A p-value of <0.05 was considered statistically significant.
Results
In this study, 154 patients were eligible to participate, of which four patients declined to participate. Data was analysed for 150 patients; 3 patients could not be reached by phone postoperatively and were not included in the analysis at 24 and 48 hours.
This study has shown an overall prevalence of postoperative pain of 55.3% at 24 hours and 34.7% at 48 hours. In this study the prevalence of moderate to severe postoperative pain was 13% at 24 hours, and 11.7% at 48 hours. Mild pain was reported to be 44.6% at 24 hours and 22.9% at 48 hours.
Patient characteristics are shown in table 1. Female patients were more than male patients (76% vs 24%). Majority of the patients were between the ages of 25 to 44 years (72.67%). General surgery was the most frequent type of surgery performed (41.3%) followed by gynaecology (34%). The least performed type of surgery was ear nose and throat (ENT) with 1 case (0.7%). Most of these cases were done under general anaesthesia (55.3%) and 40.7% was done under local anaesthesia. Monitored anaesthesia care was administered to 4% of the participants. Two patients were in day care for diagnostic and therapeutic median branch block under the pain management unit.
Table 1.
Patients' characteristics
| N | % | |
| Age (years) | ||
| <25 | 14 | |
| 9.3 | ||
| 25 -–4 | 49 | 32.6 |
| 35– 44 | 60 | 40 |
| 45 – 54 | 20 | 13.3 |
| e” 55 | 7 | 4.6 |
| Sex | ||
| Male | 36 | 24 |
| Female | 114 | 76 |
| Type of Anaesthesia | ||
| Local anaesthesia | 61 | 40.7 |
| General anaesthesia | 83 | 55.3 |
| Regional anaesthesia | 3 | 2 |
| Monitored anaesthesia care | 3 | 2 |
| ASA | ||
| 1 | 131 | 87.3 |
| 2 | 18 | 12 |
| 3 | 1 | 0.6 |
| Type of Surgery | ||
| General Surgery | 62 | 41.3 |
| Gynaecology | 51 | 34 |
| Urology | 12 | 8 |
| Ophthalmology | 10 | 6.6 |
| Orthopaedics | 8 | 5.3 |
| Maxillofacial | 4 | 2.6 |
| Pain Management | 2 | 1.3 |
| Ear Nose and Throat | 1 | 0.6 |
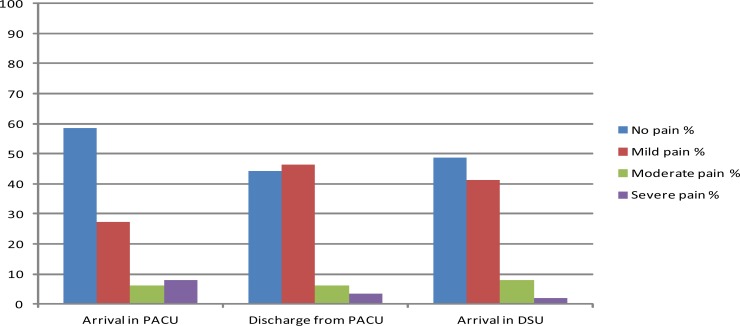
The majority of the patients arriving in the PACU (table 2 and figure 2) reported no pain (58.6%), 27.3% had mild pain, 6.0% had moderate pain and 8.0% had severe pain. At discharge from the PACU the number of patients with mild pain had increased from 27.3% at time of arrival to 46.3% at discharge. The number of patients who reported no pain (58.6%) had fallen to 44.3%. In general, the total number of patients with no pain and mild pain had increased, from the time of arrival to the PACU, compared to the number of patients with severe pain which had fallen to 3.4%. At arrival in the DSU severe pain had reduced from 8% to 2%.
Table 2.
Postoperative pain distribution in the recovery room and at arrival in DSU
| Pain intensity | No pain% | Mild pain % | Moderate pain% | Severe pain% |
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | |
| Arrival in PACU | 58.6 (50.7–66.6) | 27.3 (20.1–34.5) | 6.0 (2.2–9.8) | 8.0 (3.6–12.4) |
| Discharge from | 44.3 (36.2–52.4) | 46.3 (38.2–54.4) | 6.0 (2.2–9.9) | 3.4 (0.4–6.3) |
| PACU | ||||
| Arrival in DSU | 48.7 (40.6–56.8) | 41.3 (33.4–49.3) | 8.0 (2.2–12.4) | 2.0 (0.3–4.3) |
Figure 2.
Postoperative pain distribution in the recovery room and at arrival in DSU
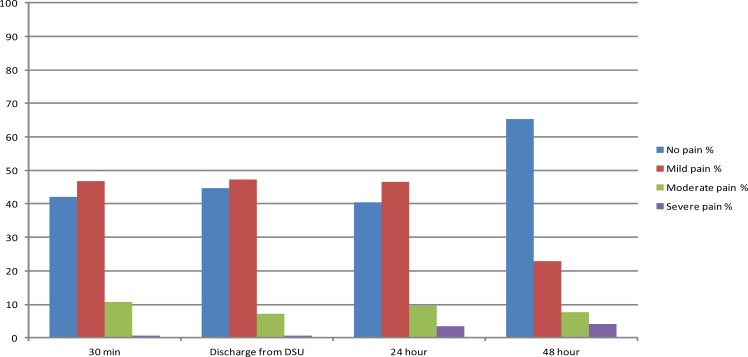
In table 3 and figure 3, after 30minutes in the DSU, pain continued to improve with 10.7% of the patients having moderate pain as compared to the time they had been admitted to DSU. On discharge from DSU, only 0.7% of all patients had severe pain and 7.3% had moderate postoperative pain. Severe pain after 24 and 48 hours was 3.4% and 4.1% respectively. Approximately 87% of patients reported no pain to mild pain after 24 hours; 88.2% of the patients reported no pain or mild pain, 48 hours after discharge.
Table 3.
Postoperative pain distribution in DSU at 24 and 48 hours after discharge
| Pain intensity | No pain% | Mild pain % | Moderate pain% | Severe pain% |
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | |
| 30 minutes | 42.0 (34.0–49.9) | 46.7 (38.6–54.7) | 10.7 (5.7–15.7) | 0.7 (0.6–1.9) |
| Discharge from DSU | 44.7 (36.6–52.7) | 47.3 (39.2–55.4) | 7.3 (3.1–11.5) | 0.7 (0.6–1.9) |
| 24 hours | 40.4 (32.4–48.5) | 46.6 (38.4–54.8) | 9.6 (4.8–14.4) | 3.4 (0.4–6.4) |
| 48 hours | 65.3 (57.4–73.1) | 22.9 (15.9–29.8) | 7.6 (3.2–12.0) | 4.1 (0.9–7.5) |
Figure 3.
Postoperative pain distribution in DSU at 24 and 48 hours after discharge
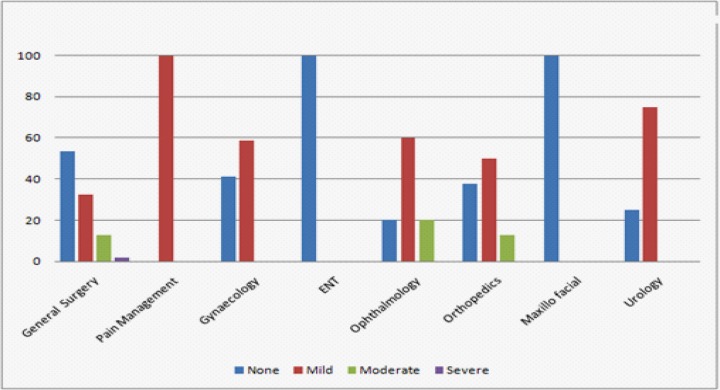
General surgical patients reported severe postoperative pain (figure 4), while ophthalmology patients scored highest (20%) for moderate postoperative pain. Patients who underwent ENT and maxillofacial procedures reported no pain both 24 and 48 hours later (3.3% of the total population). Figure 4 shows the relationship between type of surgery and postoperative pain intensity. It revealed that at the time of discharge from DSU only patients who had undergone minor surgery had moderate to severe postoperative pain. This was the same finding 48 hours later when only the group that complained of moderate to severe pain was found to have had minor surgery. After 24 hours, only 14.3% of the patients that had moderate postoperative pain had undergone intermediate surgery. This indicates that postoperative pain is a common complaint even in minor surgeries.
Figure 4.
Severity of pain in relation to the type of procedure performed
Postoperative follow up on patient's pain report - A total of 24 patients, those who were successfully contacted through their phones, reported moderate to severe pain. Of these, 16 patients had moderate pain and 8 patients had severe pain. Of these patients who reported severe pain, 5 patients had severe pain only in the first 24 hours following discharge. Three patients had moderate pain in the first 24 hours which later developed to severe pain 48 hours later.
Among the patients who had severe postoperative pain at 24 hours, there was only one patient who had been discharged without analgesics. In the group that had moderate pain, 3 patients were discharged without analgesics, and 13 patients were discharged with analgesics. A total of 16.7% of patients who developed moderate and severe postoperative pain had been discharged without analgesics. The group of patients who reported mild postoperative pain was 64 and of these 3 patients (4.7%) were discharged without medication.
None of the differences was statistically significant (table 2). The statistically significant difference in mean of pulse rates, 30minutess after the patients' arrival in DSU, may be attributed to one case, which had an unusually high pulse rate (102 beats/ min).
After discharge from hospital, patients were asked about symptoms that they suffered at home (table 4). Less than 11% complained of having one or more of the following symptoms: nausea, vomiting, headache, feeling sleepy, feeling faint and weakness. Nausea and vomiting had an incidence of 6.85% and 2.05% at 24 hours but after 48 hours both symptoms had resolved. Those patients who had to go back to ER (6.25%) had to have their eye patches or their dressings to be changed.
Table 4.
Patients symptoms after 24 hours and 48 hours (%)
| Symptoms | 24 hours | 48 hours | ||
| Yes | No | Yes | No | |
| Nausea | 6.85 | 93.15 | 0 | 100 |
| Vomiting | 2.05 | 97.95 | 0 | 100 |
| Headache | 10.96 | 89.04 | 2.24 | 97.76 |
| Sleepy | 7.53 | 92.47 | 2.24 | 97.76 |
| Faint | 5.56 | 94.44 | 0.75 | 99.25 |
| Weakness | 6.94 | 93.06 | 2.99 | 97.01 |
| Go back to ER | 6.25 | 93.75 | 2.24 | 97.76 |
| Called doctor | 0.69 | 99.31 | 1.49 | 98.51 |
Discussion
In the recovery room, immediately after surgery, 8.0% of the patients reported to have severe pain, and by the time they were discharged from the recovery room only 3.4% of the patients reported to have severe pain. This was a significant difference compared to the findings of McHugh et al. 22 who studied patients of whom 17% reported to have had severe postoperative pain immediately after surgery. These patients 22 had undergone day-case surgical procedures that were almost similar to the procedures in this study but with a few being complex procedures (dental extractions and arthroscopy). These patients who had dental extractions or arthroscopies performed on them probably had preoperative pain that could have influenced their pain scores postoperatively. The drop in the severity of postoperative pain while in the recovery room could have been caused by the analgesics given at the end of surgery taking effect or the ones that were given during the time they were in the recovery room.
This study has shown that patients have experienced less pain in the recovery room and DSU compared to after discharge. In this study, moderate to severe pain was reported by 10.7% and 0.7% of the patients respectively, after they had spent 30mins in the DSU. At discharge from DSU, 7.3% had moderate pain and 0.7% had severe pain. Both moderate and severe pain had increased after 24 hours (table 3; 9.6% and 3.4%) but after 48 hours severe pain had increased to 4.1% while moderate pain had declined to 7.6%. This could probably be due to the effects of analgesic drugs given in theatre or in the recovery room. A similar pattern has been reported by Pavlin et al, study 23. However, they performed more complex surgeries like knee arthroscopy and transvaginal surgery which may have given a higher incidence of pain 60% (>3/10) 23.
The increase in the pain intensity while at home could have stemmed from the ambulatory setting of our services where patients compliance concerning the use of analgesics during the postoperative period at home is very difficult to control. Gramke and co-workers found in their study that, patients had a low postoperative use of analgesics24. A point of criticism might be that despite these findings by Gramke and co-workers, our study disclosed that some patients were being discharged without analgesics. It was also revealed that moderate to severe postoperative pain was reported mostly by the patients who had under gone minor surgery. This can be interpreted in one way, as it might be thought that patients who undergo minor surgical procedures would not require a lot of analgesics, and probably some of them don't need any analgesics. This might account for those patients who suffered moderate to severe postoperative pain and who had not received pain killers to take home at discharge.
Acute postoperative pain is a complex physiologic reaction to tissue injury, visceral distension, or disease. It is manifested by autonomic, psychological, and behavioural responses that result in patient-specific unpleasant, unwanted sensory and subjective emotional experience.
In many countries day care surgeries account for more than 50% of all the elective surgeries25. Rescue analgesia should be offered if the prescribed analgesic is not effective. It has been shown that the use of pre-packaged take-home analgesics specific to the type of surgery and breakthrough medication can lead to improved pain control, mobility, and sleep13.
The development of pain alleviating-regimens which allow early ambulation, techniques to reduce nausea, vomiting and ileus, realization that early enteral nutrition is important for recovery and reduction of infective complications and the use of well established antithrombotic and antimicrobial regimens therefore represent the basis for a global approach to perioperative care26.
Day surgery care is a cost-effective, quality approach to surgery that has grown rapidly in recent years. The success of day-case surgery depends on effective control of postoperative pain27. Poor pain control can counteract many of the beneficial effects of day care surgery and leads to the development of chronic pain 12, 28. In developed countries prevalence of postoperative pain following day care surgery is variable ranging from 30–40%.
Limitations
The limitation of this study included the fact that the type of surgeries performed at the Aga Khan University Hospital, as a day care basis, are mostly of minor and intermediate complexity. We were not able to complete the postoperative follow up of 3 patients after discharge from day care. They might have either been in a lot of pain and they were not able to answer the phones; or they were totally pain free and found it unnecessary to be disturbed by answering the phone. We did not score our patients using a modified Brief Pain Inventory. Lastly, our survey covered a relatively small sample size.
Conclusion
The overall prevalence of postoperative pain after day care surgery was found to be 58% within 30mins postoperatively, 55.3% after 24 hours, and 34.7% after 48 hours following surgery. The prevalence of postoperative pain is low but with increase in the number of patients and the scope of surgeries to be done as day case surgeries this prevalence is likely to increase.
Acknowledgement
We thank the staff of the Aga Khan University Hospital, Nairobi, for the support they gave us during the conduct of this study
References
- 1.Peters M, Vlaeyen J, Weber W. The joint contribution of physical pathology, pain-related fear and catastrophizing to chronic back pain disability. Pain. 2005;113:45–50. doi: 10.1016/j.pain.2004.09.033. [DOI] [PubMed] [Google Scholar]
- 2.Von Korff M, Balderson B, Saunders K. A trial of an activating intervention for chronic back pain in primary care and physical therapy settings. Pain. 2005;113(3):323–330. doi: 10.1016/j.pain.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 3.Vlaeyen J, Linton S. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317–332. doi: 10.1016/S0304-3959(99)00242-0. [DOI] [PubMed] [Google Scholar]
- 4.Lethem J, Slade P, Troup J, Bentley G. Outline of a fear-avoidance model of exaggerated pain perception-I. Behavioural Research and Therapy. 1983;21(4):401–408. doi: 10.1016/0005-7967(83)90009-8. [DOI] [PubMed] [Google Scholar]
- 5.Philips H. Avoidance behaviour and its role in sustaining chronic pain. Behavioural Research and Therapy. 1987;25(4):273–279. doi: 10.1016/0005-7967(87)90005-2. [DOI] [PubMed] [Google Scholar]
- 6.Waddell G, Newton M, Henderson I, Somerville D, Main C. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 7.Peters M, Sommer M, de Rijke J, Kessels F, Heineman E, Patijn J, et al. Somatic and Psychologic Predictors of Long Term Unfavorable Outcome After Surgical Intervention. Annals of Surgery. 2007;245:487–494. doi: 10.1097/01.sla.0000245495.79781.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Girish P. Pain management after ambulatory surgery. Ambulatory Surgery. 1999;7(1):3–12. [Google Scholar]
- 9.White P. Ambulatory anesthesia in the 21st century. Current Opinion in Anesthesiology. 1998;11(6):593–594. doi: 10.1097/00001503-199811000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Bruce J, Drury N, Poobalan A, Jeffrey R, Smith W, Chambers W. The prevalence of chronic chest and leg pain following cardiac surgery: a historical cohort study. Pain. 2003;104:265–273. doi: 10.1016/s0304-3959(03)00017-4. [DOI] [PubMed] [Google Scholar]
- 11.Smith W, Bourne D, Squair J, Phillips D, Chambers W. A Retrospective cohort study of post mastectomy pain syndrome. Pain. 1999;83(1):91–95. doi: 10.1016/s0304-3959(99)00076-7. [DOI] [PubMed] [Google Scholar]
- 12.Coderre T, Katz J, Vaccarino A, Melzack R. Contribution of central neuroplasticity to pathological pain: review of clinical and experimental evidence. Pain. 1993;52(3):259–285. doi: 10.1016/0304-3959(93)90161-H. [DOI] [PubMed] [Google Scholar]
- 13.Katz W, Rothenberg R. Section 3: The nature of pain: pathophysiology. Journal of Clinical Rheumatology. 2005;11(2):S6–S10. doi: 10.1097/01.rhu.0000158686.43637.af. [DOI] [PubMed] [Google Scholar]
- 14.Kehlet H, Jensen T, Woolf C. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367(9522):1618–1625. doi: 10.1016/S0140-6736(06)68700-X. [DOI] [PubMed] [Google Scholar]
- 15.Serpell M, Makin A, Harvey A. Acute pain physiology and pharmacological targets: the present and future. Acute Pain. 1998;1(3):31–47. [Google Scholar]
- 16.Scholz J, Steinfath M, Tonner P. Postoperative nausea and vomiting. Current Opinion in Anesthesiology. 1999;12(6):657–661. doi: 10.1097/00001503-199912000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Vaurio L, Sands L, Wang Y, Mullen E, Leung J. Postoperative Delirium: The Importance of Pain and Pain Management. Anesthesia & Analgesia. 2006;102(4):1267–1273. doi: 10.1213/01.ane.0000199156.59226.af. [DOI] [PubMed] [Google Scholar]
- 18.Chung F, Mezei G. Factors Contributing to a Prolonged Stay After Ambulatory Surgery. Anesthesia & Analgesia. 1999;89(6):1352–1359. doi: 10.1097/00000539-199912000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Stephens J, Laskin B, Pashos C, Pen B, Wong J. The Burden of acute postoperative pain and the potential role of the COX-2-specific inhibitors. Rheumatology. 2003;42(Suppl. 3):iii40–iii52. doi: 10.1093/rheumatology/keg497. [DOI] [PubMed] [Google Scholar]
- 20.Rawal N. Analgesia for day-case surgery. British Journal of Anaesthesia. 2001;87(1):73–87. doi: 10.1093/bja/87.1.73. [DOI] [PubMed] [Google Scholar]
- 21.Meridy H. Criteria for selection of ambulatory surgical patients and guidelines for anesthetic management: a retrospective study of 1553 cases. Anesthesia & Analgesia. 1982;61:921–926. [PubMed] [Google Scholar]
- 22.McHugh G, Thoms G. The management of pain following day-case. Anaesthesia. 2002;57:270–275. doi: 10.1046/j.1365-2044.2002.2366_2.x. [DOI] [PubMed] [Google Scholar]
- 23.Pavlin D, Chen C, Penaloza D, Buckley F. A survey of pain and other symptoms that affect the recovery process after discharge from an ambulatory surgery unit. Journal of Clinical Anesthesia. 2004;16(3):200–206. doi: 10.1016/j.jclinane.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 24.Gramke H, de Rijke J, van Kleef M, Raps F, Kessels A, Peters M, et al. The prevalence of Postoperative Pain in a Cross-sectional Group of Patients After Day-case Surgery in a University Hospital. Clinical Journal of Pain. 2007;23:543–548. doi: 10.1097/AJP.0b013e318074c970. [DOI] [PubMed] [Google Scholar]
- 25.Mitchell A, van Zanten S, Inglis K, Porter G. A randomized controlled trial comparing acetaminophen plus ibuprofen versus acetaminophen plus codeine plus caffeine after outpatient general surgery. Journal of American College of Surgeons. 2008;206(3):472–479. doi: 10.1016/j.jamcollsurg.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 26.Rowbotham D, Smith G. Postoperative nausea and vomiting. British Journal of Anaesthesia. 1992;69:1–68. doi: 10.1093/bja/69.supplement_1.46s. [DOI] [PubMed] [Google Scholar]
- 27.Rawal N. Postoperative pain treatment for ambulatory surgery. Best Practice & Research Clinical Anaesthesiology. 2007;21(1):129–148. doi: 10.1016/j.bpa.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 28.McGrath B, Elgendy H, Chung F, Kamming D, Curti B, King S. Thirty percent of patients have moderate to severe pain 24hr after ambulatory surgery: a survey of 5,703 patients. Canadian Journal of Anesthesia. 2004;51(9):886–891. doi: 10.1007/BF03018885. [DOI] [PubMed] [Google Scholar]
- 29.Mattila K, Toivonen J, Janhunen L, Rosenberg P, Hynynen M. Postdischarge symptoms after ambulatory surgery: first-week incidence, intensity, and risk factors. Anesthesia & Analgesia. 2005;101(6):1643–1650. doi: 10.1213/01.ANE.0000184189.79572.28. [DOI] [PubMed] [Google Scholar]
- 30.Aga Khan University hospital N, Kenya, author. Official records at the medical records of Aga Khan University hospital Nairobi. Kenya: Aga Khan University hospital; 2008. [Google Scholar]