Abstract
Background
Mortality of mothers and newborns is an important public health problem in low-income countries. In the rural setting, implementation of community based education and mobilization are strategies that have sought to reduce these mortalities. Frequently such approaches rely on volunteers within each community.
Objective
To assess the perceptions of the community volunteers in rural Kenya as they implemented the EmONC program and to identify the incentives that could result in their sustained engagement in the project.
Method
A community-based cross sectional survey was administered to all volunteers involved in the study. Data were collected using a self-administered supervision tool from all the 881 volunteers.
Results
881 surveys were completed. 769 respondents requested some form of incentive; 200 (26%) were for monetary allowance, 149 (19.4%) were for a bicycle to be used for transportation, 119 (15.5%) were for uniforms for identification, 88 (11.4%) were for provision of training materials, 81(10.5%) were for training in Home based Life Saving Skills (HBLSS), 57(7.4%) were for provision of first AID kits, and 39(5%) were for provision of training more facilitators, 36(4.7%) were for provision of free medication.
Conclusion
Monetary allowances, improved transportation and some sort of identification are the main incentives cited by the respondents in this context.
Keywords: Incentives, motivation, community health workers, community implementation, community participation, Emergency Obstetric and Neonatal Care
Introduction
While the health sectors of developing countries recognize the need for paid Community Health Workers (CHWs) as recommended by World Health Organization (WHO), only a few, such as India, have in place this cadre of workers. The majority of countries in Africa, including Kenya, use volunteers from the communities for implementing community based programs. There is sufficient experience with CHWs as implementers of pre-designed programs, and their incentives have been categorized. This cadre of community volunteers are motivated by recognition, provision of tools, monetary payments and training. Long term retention of volunteers in these positions has been difficult. The use of incentives for retention of volunteer health workers in low income settings remains controversial at all levels of the healthcare including the community level health programs1–6, In addition, publications on incentives for volunteers, whose activities included mobilizing communities in a process of leveraging community owned resource to implement maternal and newborn health interventions, are few in the literature.
The Global Network for Women's and Children's Health Research (GNWCHR) is a multi-country, multi-site research network that seeks to understand the causes of perinatal morbidity and mortality. This research network was undertaking studies for reduced maternal and neonatal mortality, through increasing and improving the quality of obstetric and neonatal care in communities7. They had two independent but interlinked on-going studies. First, the Maternal and Neonatal Birth (MNH) Registry registered all pregnancies, births and deaths of mothers and neonates within the defined geographic area of the study. The second is the Emergency Obstetric and Neonatal Care (EmONC) study.
The EmONC study had volunteer-based teams, working within these geographic clusters to address the linkage between the community and the health facility (Health System) in the care for mothers and their newborns. These volunteers were villagers, nominated by fellow villagers, through a process led by the local administrators. They were to lead the community in finding home-grown solutions to the Maternal and Newborn Health problems. The cluster study team of EmONC supported these nominees by training them on how to facilitate dialogue in the community for planning, acting and evaluating their activities. In addition, they trained them on Home Based Life Saving Skills (HBLSS). The countries participating in this study included Kenya, Zambia, Guatemala, Argentina, Pakistan, India, and others. When retaining volunteers became difficult to do in Kenya, the country study team sought to find the context specific incentives to use to reduce attrition. This paper is based on anonymous retrospective review of this routine data. The protocol and related processes for the parent study was published8 and a summary has been included in the methods section of this article.
Methods
EMONC Study design and process
The EMONC study comprised of three interventions:
Home Based Life Saving Skills (HBLSS) aimed at training community birth attendants (skilled and unskilled) to recognize problems, stabilize and refer pregnant women and their newborns to appropriate health care facilities
Community Mobilization (CM), aimed to educate and mobilize the local community to identify resources and solutions within the community to improve maternal and neonatal mortality, with special emphasis on pregnant women and their families
Health Facility Improvement (HFI) aimed at ensuring that once a pregnant woman and her newborn reached the referral facility, appropriate services were available.
Implementation of the first and second arms relied upon lay personnel, most of whom were volunteers, while the third arm relied upon health-care professionals. The first two arms were designed to be done through leveraging each community's own human and material resources. Thus the cadre of community volunteers was the main human resource implementing these components. These volunteers joined cluster committees, village committees and core groups as described in the study protocol process publication8.
The cluster committees held regular planning meetings. Their activities included formation of the village committees and support of their subsequent activities, facilitation of lay persons on the discussion of newborn and maternal mortality events (mortality audits), support of the activities of volunteer facilitators and overseeing community mobilization activities. Those who were most affected and interested in maternal and newborn health in the villages joined core groups. The Village Health Committees provided support to all the core group activities. To build capacity for their activities, these volunteers received training on Home Based Life Saving Skills (HBLSS) to recognize danger signs and stabilize the mothers and newborn and refer them to the health facility. They also receive training on Community Action Cycle (CAC) for community mobilization activities9–12. The activities in the CAC included preparing to mobilize, exploring, planning, acting and evaluating action plans. The core groups were formed by community members committed to EmONC activities, and used the CAC to mobilize the village community members to participate effectively in EmONC activities.
The third arm relied upon obstetricians and nurses, trained using a standardized curriculum, providing training in the health facilities to the health care providers. This was meant to improve the quality of service. To standardize the facilities ability to provide services, the study provided basic equipment including thermometers, blood pressure sphygmomanometers and magnesium sulphate to the health facilities. The EmONC study was thus designed to introduce maternal and newborn survival interventions that can be sustained by the community.
Within the first year of implementing the protocol in Kenya, 40% of the initial members of the Cluster Committees and volunteer facilitators had dropped out. It then became obvious to all that attrition of the lay volunteers was a major contributor to delays in completing the full CAC. Even the study investigators, who had to train the new workers, had higher than anticipated cost for training new volunteers. In order to address this challenge, and as part of the CAC, the potential locally available, feasible and applicable incentives were sought.
Study site
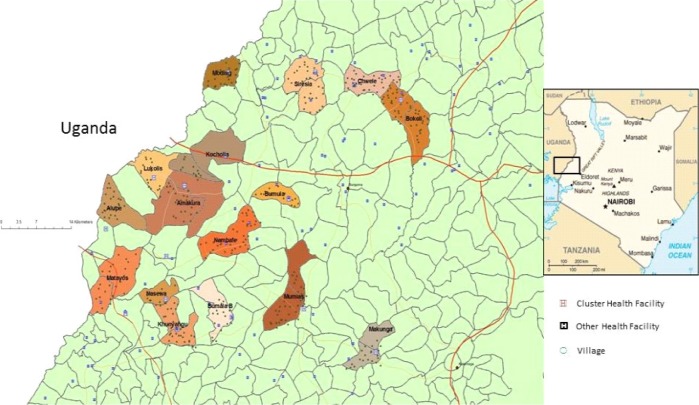
The Kenya EmONC study area was located in the western Kenya districts of Busia, Bungoma, Mumias and Teso (figure 1). This region of western Kenya is rural agrarian and has 50% of the population being in the last 2 levels of the index for household durable goods, making it among the poorest rural area in Kenya17. Most families relied upon subsistence farming. Each cluster was served by one government health facility capable of conducting deliveries, as well as several lower level health facilities or dispensaries. In addition there are a few mission hospitals also providing delivery service.
Figure 1.
Map of the EmONC area. The area is located in western Kenya, adjacent to the Uganda border
Study population on incentives
The participants in this survey were volunteers in the EmONC program. They were volunteers in the various community-based cluster committees. They participated either as high-up management members (Cluster Committee Members), or as village-based management members (Village Committee Members) or core group leadership (Volunteer Facilitators). All respondents had received training on HBLSS and CAC to guide their organizing the community for action, through the preparing to mobilize, exploring, planning, acting and evaluating action plans components. All respondents could read and write in English and Kiswahili.
All respondents were aware of the issue of lack of incentives and the accruing attrition since it had come up in many of CAC meetings in which they participated. After consensus was built in these meetings to address the problem, they proposed answering a self-administered questionnaire, to determine the nature of incentives they considered appropriate in their context.
Data collection on incentives
The questionnaire was designed by the Kenya EMONC investigators limiting the content to what the lay volunteers determined as acceptable including a few open-ended questions. The volunteers were given the questionnaires to complete and returned the completed questionnaires after 3 months (November 2009 and January 2010).
Data analysis
To extract this data, tables were constructed for each of the closed ended questions. Themes in the open ended answers were developed after being evaluated for relevance by the investigators. The data was entered into the Epidata program (EpiData Software, EpiData Association, Odense Denmark) and analysed using frequencies and cross tabulations.
Results
Based on the number of volunteers in the study area, 881 questionnaires were distributed and all were filled and returned. There were a total of 881 participants, 64% were females and 36% males. The age of the respondents ranged from 20 to over 50 years, 70% being below 40 years of age as indicated in table 1. The largest majority (98% of the respondents) had a secondary education or less as shown in table 2. Younger volunteers were more highly educated than older volunteers.
Table 1.
Gender distribution in the various age groups
| Age of participants (years) N (%) * | |||||
| 20–30 | 31–40 | 41–50 | >51 | Total | |
| Male | 52(16) | 133(42) | 85(27) | 50(16) | 320 |
| Female | 233(2) | 199(36) | 93(17) | 32(6) | 557 |
| Total | 285 | 332 | 178 | 82 | 877 |
Age group of 4 respondents was missing.
Table 2.
Education levels of the volunteers
| Years of education | 0–8 | 9–12 | >12 | Total |
| 141 | 132 | 12 | 285 | |
| 132 | 191 | 7 | 330 | |
| 88 | 88 | 2 | 178 | |
| 43 | 39 | 0 | 82 | |
| Total | 881 |
Did not respond to years of education question 6
Note that the percentages in the table are as follows: The middle rows add up to 100% for each gender
The respondents' opinions were sought on how the EmONC program has been useful to the community (table 3). Five hundred and ninety nine responses (55.1%) cited improved level of understanding (health education) through HBLSS activities, 197 (16.5%) cited reduction in mortality, 128 (10.7%) cited health facility improvement, and 205 (17.2%) cited other outcomes.
Table 3.
Responses to the question: How the EmONC program has been useful to the community
| Response | N(%) |
| Mothers health education | 599(55) |
| (HBLSS related activities) | |
| Improved health facility obstetric | 128(11) |
| care | |
| Emergency delivery materials | 68(6) |
| Education (Family planning) | 43(4) |
| Reduced mortality (mothers, | 197(17) |
| babies) | |
| Reduction of home deliveries | 61(5) |
| Increased ANC Attendance | 33(3) |
The volunteer facilitators' opinions on which incentives they wished to be provided were varied. 26% mentioned a monetary allowance as their preferred motivation or incentive. Others preferred different incentives including provision of a bicycle (19.4%), provision of uniform and identification badge (15.5%), supply of training materials (11.4%), training in Home Based Life Saving Skills (10.5%), provision of first aid kit (7.4%), training of more facilitators (5%) and supply of free medicines (4.7%) table 4.
Table 4.
Incentives requested by facilitators
| Response | N(%) |
| Personal incentives | |
| Monetary Allowance | 200(26) |
| Bicycles | 149(20) |
| Uniform | 119(16) |
| Training materials | 88(11) |
| HBLSS training | 81(11) |
| First AID Kits | 57(7) |
| Free medication | 36(5) |
| More Facilitators | 39(5) |
| Community incentives | |
| Increase in primary health | 301(30) |
| facilities. | |
| Ambulances | 147(15) |
| Emergency delivery materials | 80(8) |
| Subsidized Medication | 52(5) |
| Continued Health Education | 255(26) |
| Food Rations to the poor | 43(4) |
| Mobile Antenatal Clinics | 99(10) |
About 20.9% of the responses from the facilitators indicated a need for more primary health facilities, 18.8% desired more health education, 15% desired an ambulance, 10.1% desired mobile antenatal clinic, 10% desired maternity wards to be constructed and 25% had varied needs (table 4).
When analysis by age group (5 year intervals) was done, there was significant variation in response based on age category and were as follows as shown in table 5.
Table 5.
Positive responses (desire for) by age, showing the number of respondents and their respective percentages
| Age in years | 20–25 | 26–30 | 31–35 | 36–40 | 41–45 | 46–50 | > 51 | **P-value |
| n | 125 | 152 | 174 | 133 | 98 | 71 | 74 | |
| Allowances | 12% | 18.4% | 28.7% | 28.6% | 24.5% | 35.7% | 27.0% | 0.001 |
| Uniforms | 12.8% | 12.5% | 16.7% | 18% | 15.3% | 12.% | 9.5% | 0.606 |
| bicycles | 11.2% | 16.4% | 20.7% | 21.1% | 18.4% | 22.9% | 16.2% | 0.310 |
| Desire HBLSS |
8% | 9.2% | 10.3% | 13.5% | 8.2% | 12.9% | 14.9% | 0.572 |
| First AID Kit | 5.6% | 2% | 8.6% | 7.5% | 5.1% | 10% | 13.5% | 0.034 |
| Free Medicines | 4% | 0.7% | 4.6% | 6% | 4.1% | 5.7% | 8.1% | 0.184 |
| More HBLSS facilitators |
3.2% | 4% | 4% | 6% | 2% | 4.3% | 10.8% | 0.169 |
| Ambulance services during delivery |
11.8% | 18.1% | 19.6% | 19.9% | 12.4% | 23.9% | 11.1% | 0.108 |
| Emergency provision during delivery |
7.1% | 9.7% | 8.8% | 9.6% | 9.5% | 4.2% | 16% | 0.283 |
| Subsidized medicines and mosquito nets |
7.1% | 3.2% | 4.9% | 6.8% | 2.4% | 45.6% | 14.8% | 0.014 |
| Mobile Clinics | 13.4% | 12.9% | 11.5% | 8.2% | 17.1% | 7% | 11.4% | 0.214 |
| Health Education and Capacity building |
19.7% | 12.9% | 19.8% | 26% | 21.9% | 21.1% | 133.3% | 0.014 |
| Food rations to the poor |
7.9% | 1.9% | 4.9% | 4.8% | 3.8% | 1.4% | 11.1% | 0.029 |
| Training Centres | 9.4% | 7.1% | 9.3% | 8.2% | 8.5% | 8.5% | 11.1% | 0.03 |
Allowances, p value 0.001, range 12% to 35%, highest cited in the age category 31–50 years compared to both younger and older age groups. First aid kit, p value 0.034, range 2% to 13.5%, highest cited in age group >51 years and lowest in the 26–30 years. Subsidized medicines and nets, p value 0.014, range 2.9% to 14.8%, highest cited in age group 41–45 years and lowest in the 20–25 years.
Health education and capacity building, p value 0.014, range 19.7% to 33.3%, highest in >51 years and lowest in 20–25 years.
Provision of food rations, p value 0.03, range from one out of seventy one responses to 11.1%, highest in >51 years and lowest in 46–50 years. There were no age based difference for desire for uniforms, bicycles, HBLSS training, free medicines, training more facilitators, ambulance services, emergency delivery materials, mobile clinics and training centres. When analysis by gender as shown in table 6 was done, the findings with statistical difference (there was significant variation in response based on age category) were as follows:
Table 6.
Positive responses (desire for) by gender. Showing the number of respondent* and their respective percentages
| Gender | Males | Females | P value |
| Allowances | 79/294 (26.9%) | 121/534(22.7%) | 0.203 |
| Uniforms | 46/294(15.6%) | 75/534(14%) | 0.539 |
| Bicycles | 65/294(22.1%) | 84/534(15.7%) | 0.24 |
| Desire to learn more HBLSS | 29/294(9.9%) | 52/534(9.7%) | 1.0 |
| First AID Kit | 23/294(7.8%) | 34/534(6.4%) | 0.474 |
| Free Medicines | 16/294(5.4%) | 20/534(3.7%) | 0.166 |
| More HBLSS facilitators | 19/294(6.5%) | 20/514(3.7%) | 0.057 |
| Ambulance services during delivery | 51/318 (16%) | 96/551 (17.4%) | 0.639 |
| Emergency provision during delivery | 34/318(10.7%) | 47/551 (8.5%) | 0.333 |
| Subsidized medicines and Mosquito nets | 29/318(9.1%) | 23/551(4.2%) | 0.004 |
| Mobile clinics | 36/318(11.3%) | 64/551(11.6%) | 0.913 |
| Health Education and Capacity building | 89/318(28%) | 95/551(28%) | <0.0001 |
| Food rations to the poor | 23/318(7.2%) | 29/551(4.9%) | 0.023 |
| Training Centres | 30/318(9.4%) | 42/551(7.4%) |
Bicycles, P value 0.05, Males 22.1% and Females 15.7%.
Field Materials. P value 0.003, Males 15.0% and 8.2%. More primary health facilities, P value 0.029, Males 27.8% and Females 21.2% Food ratios, P-value 0.018. Males 7.2% and Females 3.6%
There was no gender based difference for allowances, uniform, first aid kit, HBLSS training, free medicines, more facilitators, more facilitators, ambulance and transport, maternity wards, delivery materials, mobile clinics and training centres.
Discussion
Allowances, bicycles, identification badges and training were cited as the most desired incentives for the volunteers in the EmONC study. While these key incentives were generally similar to those reported in other studies1, 16, these were specific to the context of the program and population. Though usually unsustainable, monetary incentives were the most cited (26%) by the respondents. Bicycle transport was cited by 19.4%, followed by some form of identification (15.5%), and more training (11.4%). The high rating of bicycle transport might be due to the fact that the EmONC study implementation is associated with significant movement within the villages. Bicycle transport was the main mode of short distance travel in the study area.
There is lack of a single incentive that is cited by more than 50% of the respondents including monetary incentives. In the parent study, the issue of incentives had been debated and there had been significant buy-in among those who were responding. It is therefore possible that more would have shown desire for incentive, had the questions been asked at the beginning of the implementation of the parent study, or applied to a group of potential volunteers. On the other hand, this type of incentives cited, might still have remained the same as shown in this study. The usefulness of the program was looked at from the volunteer's perception of the value of three EmONC components, that is, HBLSS training, community mobilization, and health facility improvement. The volunteers were informed that the potential outcomes of the program include reduction in deaths of mothers and their newborns, increased antenatal clinic attendance and increased numbers of deliveries within the health facility conducted by skilled birth attendants. The volunteers therefore agreed that one of the benefits of the program would be education of the community regarding maternal and newborn health. This is evidenced by the finding that 55.1% of their responses cited this as a possible benefit. Furthermore they observed that the HBLSS was useful as the communities formulate birth plans for pregnant women within their villages and encouraged them to deliver within a health facility.
These findings agree with the conclusions in the systematic review by Bhattacharyya et al, where it was noted that there is no incentive package for CHW that is universally applicable and recommended13. On the other hand, many factors were found to influence motivation of CHWs. Being part of the larger cultural and political environment, their motivation is influenced by who they are within the community including their inherent characteristics such as age, gender, ethnicity and perceived economic status. When given a large number of tasks they could become overwhelmed. Complex tasks need training and practice with less time to implement. When the area they cover is large, time requirements and lack of adequate transportation became prohibitive. The same review found that incentives are critical. These included supportive supervision, appropriate training, small items like badges that increase a sense of pride and status in their communities, appropriate job aids, such as counselling cards, peer support achieved through working in groups and worker associations. However, the most critical was the relationship with their communities. The EmONC study provided an opportunity for a strong relationship between the volunteers and their communities. Implementation of the community mobilization component was purely community owned. It is unclear why the strong relationship did not result in volunteer retention in this program.
Allowances, some aspects of free medicines, health education and food rations seemed to be cited more by the older population compared to the younger. This may be an indication that incentives vary with age, and the older age group had their own unique preferences while the younger ones were more flexible.
Males desired bicycles, durable health care structures and food rations, compared to the females. Females did not desire any incentive cited significantly more compared to the male volunteers. This may in part be a reflection of their decision making position in terms of capital investment in the community.
Conclusion
Recognition of the positive contribution of the program to a community alone does not seem to create desire by volunteers to remain actively engaged in a community program. When continuous attrition of volunteers from community programs occurs, replacement, retraining and service disruptions are unsustainably expensive. On the other hand, each community is unique and the challenges as well as opportunities it provides are thus community specific. Incentives are context specific14, and each community's background needs to be studied to identify and apply the acceptable ones for the given community. By exploring attitudes towards small incentives in a given context, it is possible to identify those that can be applicable and relevant. In Western Kenya, age and the gender specific incentives are were found.
Recommendations
Due to the varied incentives cited, some varying with age and gender, it is important that a program considering use of volunteers, discussed the alternative non-monetary incentives for retaining them. This discussion should involve the community, especially the potential volunteers before or during recruitment.
Identification of specific needed incentives in a community should be done before any are introduced in community based programs.
Acknowledgment
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number U01 HD058326 and U01 HD040636. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Perez F, Ba H, Dastagire SG, Altmann M. The role of community health workers in improving child health programmes in Mali. BMC Int Health Hum Rights. 2009;9:28. doi: 10.1186/1472-698X-9-28. Epub 2009/11/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iipinge S, Dambisya YM, Loewenson R, Chimbari M, Ndetei D, Munga M, Sibandze S, Lugina H. Policies and incentives for health worker retention in east and southern Africa: Learning from country research. Harare: University of Namibia, Training and Research Support Centre, University of Limpopo, EQUINET, ECSAHC, EQUINET Discussion Paper 78 EQUINET; 2009. [Google Scholar]
- 3.Rahman SM, Ali NA, Jennings L, Seraji MH, Mannan I, Shah R, et al. Factors affecting recruitment and retention of community health workers in a newborn care intervention in Bangladesh. Hum Resour Health. 2010;8:12. doi: 10.1186/1478-4491-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nkowane AM, Boualam L, Haithami S, El Sayed el TA, Mutambo H. The role of nurses and midwives in polio eradication and measles control activities: a survey in Sudan and Zambia. Hum Resour Health. 2009;7:78. doi: 10.1186/1478-4491-7-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ridde V, Diarra A. A process evaluation of user fees abolition for pregnant women and children under five years in two districts in Niger (West Africa) BMC Health Serv Res. 2009;9:89. doi: 10.1186/1472-6963-9-89. Epub 2009/06/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buykx P, Humphreys J, Wakerman J, Pashen D. Systematic review of effective retention incentives for health workers in rural and remote areas: towards evidence-based policy. Aust J Rural Health. 2010;18(3):102–109. doi: 10.1111/j.1440-1584.2010.01139.x. Epub 2010/06/29. [DOI] [PubMed] [Google Scholar]
- 7.McClure EM, Wright LL, Goldenberg RL, Goudar SS, Parida SN, Jehan I, et al. The global network: a prospective study of stillbirths in developing countries. Am J Obstet Gynecol. 2007;197(3):247. doi: 10.1016/j.ajog.2007.07.004. e1-5. Epub 2007/09/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pasha O, Goldenberg RL, McClure EM, Saleem S, Goudar SS, Althabe F, et al. Communities, birth attendants and health facilities: a continuum of emergency maternal and newborn care (the global network's EmONC trial) BMC Pregnancy and Childbirth. 2010;10(1):82. doi: 10.1186/1471-2393-10-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sibley L, Buffington ST, Tedessa L, Sr, McNatt K. Home-Based Life Saving Skills in Ethiopia: an update on the second phase of field testing. Journal of midwifery & women's health. 2006;51(4):284–291. doi: 10.1016/j.jmwh.2005.10.015. Epub 2006/07/04. [DOI] [PubMed] [Google Scholar]
- 10.Sibley L, Buffington ST, Haileyesus D. The American College of Nurse-Midwives' home-based lifesaving skills program: a review of the Ethiopia field test. Journal of midwifery & women's health. 2004;49(4):320–328. doi: 10.1016/j.jmwh.2004.03.013. Epub 2004/07/09. [DOI] [PubMed] [Google Scholar]
- 11.Sibley L, Buffington ST, Beck D, Armbruster D. Home based life saving skills: promoting safe motherhood through innovative community-based interventions. Journal of midwifery & women's health. 2001;46(4):258–266. doi: 10.1016/s1526-9523(01)00139-8. Epub 2001/10/18. [DOI] [PubMed] [Google Scholar]
- 12.Dynes M, Rahman A, Beck D, Moran A, Pervin J, Yunus M, et al. Home-based life saving skills in Matlab, Bangladesh: a process evaluation of a community-based maternal child health programme. Midwifery. 2011;27(1):15–22. doi: 10.1016/j.midw.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 13.Bhattacharyya K, Winch P, LeBan K, Tien M. Community Health Worker Incentives and Disincentives: How They Affect Motivation, Retention, and Sustainability. 2001:1–68. [Google Scholar]
- 14.Dieleman M, Gerretsen B, van der Wilt GJ. Human resource management interventions to improve health workers' performance in low and middle income countries: a realist review. Health Res Policy Syst. 2009;7:7. doi: 10.1186/1478-4505-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.WHO, author. Making pregnancy safer : the critical role of the skilled attendant : a joint statement by WHO, ICM and FIGO. Geneva: 2004. [Google Scholar]
- 16.Willis-Shattuck M, Bidwell P, Thomas S, Wyness L, Blaauw D, Ditlopo P. Motivation and retention of health workers in developing countries: a systematic review. BMC Health Serv Res. 2008;8:247. doi: 10.1186/1472-6963-8-247. Epub 2008/12/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kenya National Bureau of Statistics (KNBS) and ICF Macro, author. Kenya National Demographic and Health Survey 2008-09. Maryland: KNBS and ICF Macro; 2010. p. 25. [Google Scholar]