Abstract
Peripheral ossifying fibroma (POF) is most often a self-limiting, sessile or pedunculated, gingival nodule that is believed to be a reactive rather than neoplastic pathologic process. The lesion is typically <2cm, however it has been recognized that some examples may grow quite large and may displace teeth. The mass-like clinical presentation and radiographic appearance of soft tissue calcification may lead to misclassification; however the histologic appearance is diagnostic. Giant POFs (GPOF) have been referred to in the literature by several other names (large, atypical, huge, gigantiform). The distinguishing characteristics of GPOFs and the factors that contribute to their growth have primarily been explored through case reports. We present a new case of POF that was giant and review 10 previously reported giant lesions, with focus on the clinical presentation, radiographic features, and outcome to explore the possibility that this represents a distinct clinical subset of lesion, with a unique set of features that warrant recognition for accurate diagnosis.
Keywords: Giant, Differential diagnosis, Gingival neoplasms, Gingival growths, Ossifying fibroma
Introduction
Peripheral ossifying fibroma (POF) is most often a gingival nodule that is believed to be a reactive rather than neoplastic pathologic process [1]. It is a pedunculated or sessile nodule that occurs exclusively on the gingiva and is therefore believed to arise from the periodontal ligament. The lesion is typically self-limiting and <2 cm, however it has been recognized that some examples may grow quite large and may displace teeth [2]. The mass-like clinical presentation and radiographic appearance of soft tissue densities may lead to misinterpretation of lesions larger than 2 cm, however the histologic appearance is diagnostic. Giant POFs (GPOF) have been referred to in the literature by several other names (large, atypical, huge, gigantiform) [3–12]. The distinguishing characteristics of GPOFs and the factors that contribute to their growth have primarily been explored through case reports. Although large case series on hyperplastic fibrous lesions of the gingiva may have included examples that were larger than 2 cm, critical information about the clinical, radiographic and histologic correlations were not available and therefore were excluded from this review [13–15]. We present a new case of POF that was giant and review previously reported giant lesions, with focus on the clinical presentation, radiographic features, and outcome to explore the possibility that this represents a distinct clinical subset of lesion, with a unique set of features that warrant recognition for accurate diagnosis.
Report of Case
A 54 year old African American male reported to the emergency dental clinic with a chief complaint “my gums are really, really bad; protruding and pushing my teeth out of the way.” The patient denied any pain in the area. The patient reported that he “noticed a small lesion on his gums” about 6 years ago, which continued to grow. The patient also reported that the lesion caused some discomfort for about the first 3 years. The lesion was expansile and displaced the adjacent teeth. The patient had not seen a dentist in over 7 years.
The patient’s medical history revealed that he was not currently under the care of a physician, had no known medical problems and was not currently taking any medications. He reported that he smoked marijuana occasionally and drank beer socially. He indicated that he had lost 30+ pounds in the past 2 years, following the loss of his job. About 2 weeks prior, the patient visited a primary care physician out of concern for his weight loss, but reported no significant findings. The BP was recorded as 114/75 mmHg and the pulse rate was 97 bpm.
Extra-oral examination was unremarkable.
Intraoral examination revealed an asymptomatic, pedunculated, mass measuring 4.5 × 3 × 3 cm in size, covered by normal mucosa, non ulcerated, with focal areas of acute inflammation where associated teeth exhibited periodontal disease. The mass was mobile, firm to palpation and extended from the alveolar mucosa, spanning teeth #22 through 27 (Fig. 1). The mass was pedunculated. The patient had generalized advanced periodontitis, multiple caries and poor oral hygiene also noted.
Fig. 1.

Intraoral view revealing an exophytic mass with normal overlying mucosa filling the right anterior mandibular vestibule
Occlusal radiograph (Fig. 2) revealed a poorly defined, facially expansile lesion with the appearance of soft tissue opacification in the anterior right mandible and displacement of the mandibular incisor teeth. There was no root resorption.
Fig. 2.
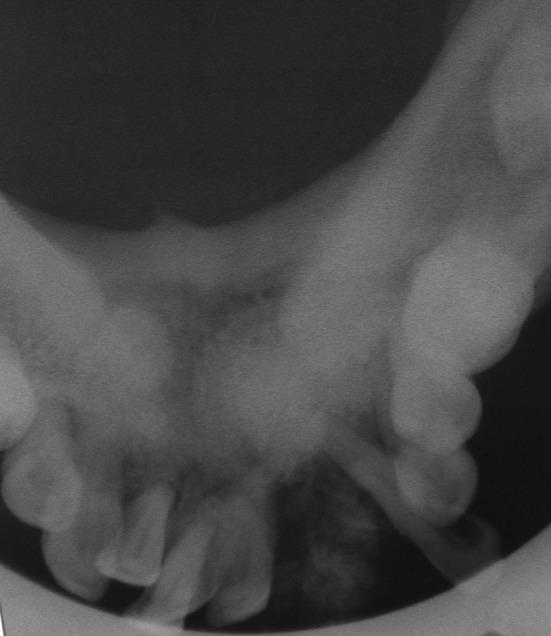
Occlusal film reveals a poorly defined, facially expansile lesion with the appearance of central radiating opaque spicules and displacement of involved teeth
After consultation with oral surgery and oral pathology, the patient was referred for biopsy. The excisional biopsy was submitted for histopathologic examination (Fig. 3). The lesion was diagnosed as POF (Fig. 4). The calcified material was viewed under polarized light and demonstrated an admixture of lamellar and woven bone, approximately 60 % woven and 40 % lamellar (Fig. 5). The patient was followed for 7 months and demonstrated excellent healing without evidence of recurrence (Fig. 6). He was then referred for comprehensive dental care.
Fig. 3.
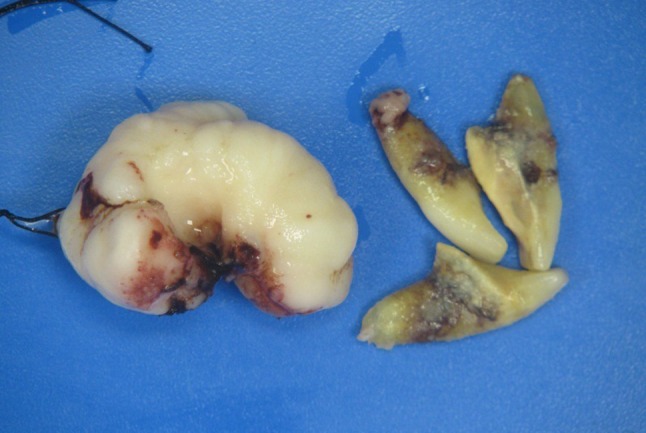
Involved teeth were removed along with soft tissue mass and submitted for histologic examination and definitive diagnosis. Note small base of lesion relative to greatest diameter
Fig. 4.
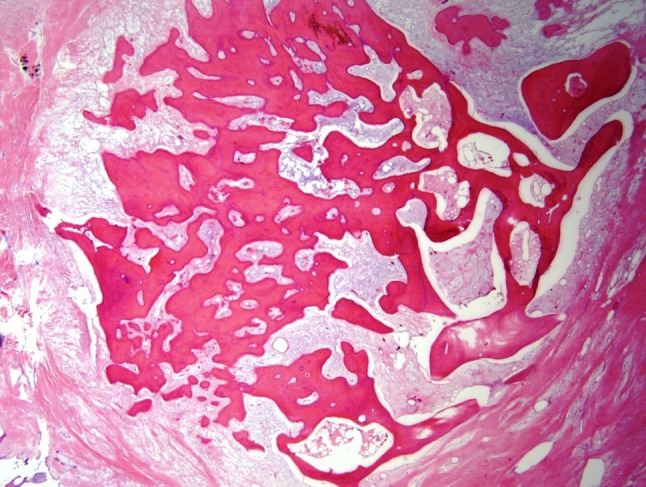
An area of calcification surrounded by fibrous stroma seen throughout the lesion, typical of peripheral ossifying fibroma. (×20 magnification)
Fig. 5.
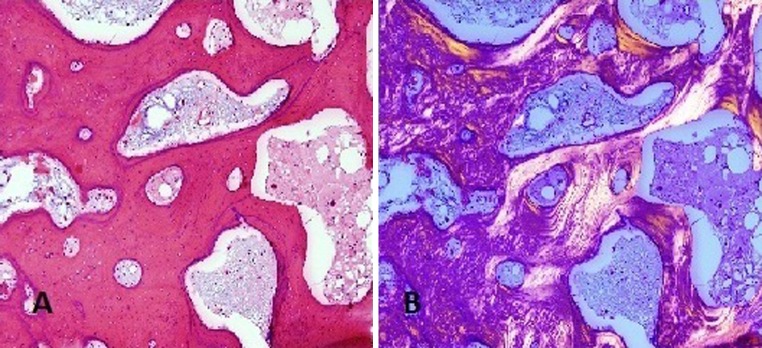
Photomicrograph of H and E stain (a), and polarized view (b) showing the mix of woven and lamellar bone typical of the calcified material in the lesion. (×100 magnification)
Fig. 6.

Patient healed post-surgical excision
Discussion
Although most reviews of POF establish the lesion to be <2 cm in diameter, we found 10 reports of larger lesions (Table 1). The lesions ranged in size from 2.5 to 9 cm in greatest dimension. The base of the lesion was pedunculated in 9 cases, 1 was described as gingival, and in 1 case the base was described as “well demarcated.” Two patients were edentulous. No cases described root resorption. Documented duration ranged from 1 month to 6 years, with 2 cases cited as unknown and 2 simply given as long duration. Patient age ranged from 7.6 to 70 years. The dental condition was poor in 3 cases, edentulous in 2 case, good in 1 case and not noted in 5 cases. Recurrence was noted in 1 case at 2 months. Including our case, 6 cases were without recurrence at the time reported and the follow up ranged from 2 to 120 months. There was no follow up in 4 cases. Facial asymmetry was noted in 5 cases and displacement of vital structures was seen on MRI in 1 case. These clinical findings differ from conventional POF.
Table 1.
Clinical, radiographic and histological features of giant peripheral ossifying fibroma
| Bodner and Dayan | Poon et al. | Kendrick and Waggoner | Moon et al. | Thierbach et al. | Kim and Kim | Poonacha | Chaudhari and Umarji | Trasad | Sacks et al. | Childers et al. | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Terminology | Large | Giant | Large | Large | Atypical | Huge | Large | Large | Large | Gigantiform | Giant |
| Clinical | |||||||||||
| Greatest dimension (cm) | 6 | 9 | 2.7 | 3.5 | 3 | 8 | 2.5 | 5.9 | 6 | 10.5 | 4.5 |
| Base | Pedunculated | Gingival | Pedunculated | Pedunculated | Pedunculated | Pedunculated | Pedunculated | Pedunculated | Well demarcated | Pedunculated | Pedunculated |
| Tooth displacement | Yes | Yes | No | Unk | No | Edentulous | Yes | Unk | Yes | Edentulous | Yes |
| Root resorption | No | No | No | Unk | No | N/A | No | Unk | No | NA | No |
| Duration | Long | 5 years | Unk | 5 month | Long | 5 years | 1 month | 6 month | 3 months | Unk | 6 years |
| Patient age (years) | 70 | 32 | 7.6 | 12 | 23 | 66 | 12 | 55 | 10 | 52 | 54 |
| Dental condition/hygiene | Poor | Unk | Good | Unk | Unk | Edentulous | Unk | Poor | Unk | Edentulous | Poor |
| Location | Mandible | Maxilla posterior and pharynx | Mandible posterior | Maxillary anterior | Mandibular posterior | Mandible posterior | Maxillary posterior | Mandibular posterior | Maxillary posterior | Mandible posterior | Mandible anterior |
| Follow up | Unk | NED 33 months | NED 6 months | NED 20 months | Unk | NED 120 months | Unk | Unk | Recurrence 2 months | NED 6 months | NED 7 months |
| Comment | Facial asymmetry | Facial asymmetry | Displaced zygomatic muscle and artery | Facial asymmetry with displaced ala of nose | Facial asymmetry with distorted labial commissure | Facial asymmetry | |||||
| Histologic | |||||||||||
| Ossification | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Stroma | Fibrocellular | Fibromyxoid | Fibrovascular | Fibroblastic | Fibrous | Fibrous | Fibroblastic | Fibroblastic | Fibrous | Fibromyxoid | Fibrous |
| Odontogenic epithelium | No | No | No | No | No | No | No | No | No | No | No |
| Radiographic | |||||||||||
| Calcification visible | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes |
| Focal bone resorption | No | Yes | Yes | No | No | Yes | No | No | No | Yes | No |
Unk unknown, NED no evidence of disease
Conventional POF is reported to remain <2 cm in greatest dimension [13, 14, 16]. Although some large case series mention cases with large size, clinicopathologic details of the individual cases were insufficient to include for the purpose of this study [13–15]. The lack of standard nomenclature hampers investigation into “giant” lesions. Without recognized terminology, controlled vocabulary (MeSH) terms cannot assist in the search. We propose the term “giant” because it has already been used in previous reports and because it is already a controlled vocabulary (MeSH) term.
Radiographic imaging in 9 cases of GPOF had radiopaque features consistent with calcification visible, 2 cases did not. Focal bone resorption was described in 4 cases. The radiographic images in some cases caused consideration of malignant neoplasms. In our case, the radiating appearance of the opacity was reminiscent of the soft tissue ossification sometimes seen in osteosarcoma. This finding is not typical for POF. Further investigation of this feature might provide a better radiographic profile of GPOF.
The histopathology in all cases of GPOF showed ossified material in a fibrous to fibromyxoid stroma. No odontogenic epithelium was noted. These findings are consistent with conventional POF.
Differential diagnosis of the 9 reports of GPOF showed consideration of both benign and malignant differentials. Our case had worrisome radiographic features with spicules of radiating opacification into less dense areas representing soft tissue, but the clinical presentation of a pedunculated, mobile mass mitigated against a malignant bone lesion. However, the size of the mass, focal bone resorption and the displacement of teeth are features that warrant consideration of an aggressive process. Recognition of GPOF characteristics may be helpful in clinical differential diagnosis.
Although 1 case of GPOF recurred at 2 months, there are too few cases to establish recurrence rate. Similarly, while it is well accepted that POF is most likely a reactive rather than neoplastic process, too few cases of GPOF are known to clearly establish the pathologic process. More studies of GPOF may clarify recurrence, pathologic process and establish whether GPOF has sufficiently distinct characteristics from POF.
Recognition of the features of this subset of POF may facilitate more accurate clinical diagnosis and subsequent treatment. We suggest adding the adjective “giant” to the diagnosis because it is a controlled vocabulary, searchable, MeSH term and standardized usage will facilitate future studies. Additional reports will enable better definition of clinical, radiographic and prognostic features. Further studies of this question will assist the clinician and the pathologist in recognition, diagnosis and appropriate treatment.
Conclusion
GPOF is a rare subset of POF with distinctive clinical and radiographic features.
Diagnosis is based on the conventional clinical and histologic features of POF in conjunction with size over 2.5 cm.
Limited follow up suggests excellent prognosis when managed by complete surgical excision.
References
- 1.Buchner A, Shnaiderman-Shapiro A, Vered M. Relative frequency of localized reactive hyperplastic lesions of the gingiva: a retrospective study of 1675 cases from Israel. J Oral Pathol Med. 2010;39(8):631–638. doi: 10.1111/j.1600-0714.2010.00895.x. [DOI] [PubMed] [Google Scholar]
- 2.Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology. 3rd ed. St. Louis, MO: Saunders Elsevier; 2009. p. 521–2.
- 3.Bodner L, Dayan D. Growth potential of peripheral ossifying fibroma. J Clin Periodontol. 1987;14(9):551–554. doi: 10.1111/j.1600-051X.1987.tb00998.x. [DOI] [PubMed] [Google Scholar]
- 4.Poon CK, Kwan PC, Chao SY. Giant peripheral ossifying fibroma of the maxilla: report of a case. J Oral Maxillofac Surg. 1995;53(6):695–698. doi: 10.1016/0278-2391(95)90174-4. [DOI] [PubMed] [Google Scholar]
- 5.Kim J, Kim ES. Huge peripheral ossifying fibroma of the lower posterior edentulous ridge. J Korean Assoc Maxillofac Plast Reconstr Surg. 2009;31(5):435–439. [Google Scholar]
- 6.Poonacha KS, Shigli AL, Shirol D. Peripheral ossifying fibroma: a clinical report. Contemp Clin Dent. 2010;1(1):54–56. doi: 10.4103/0976-237X.62520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chaudhari S, Umarji HR. Peripheral ossifying fibroma in the oral cavity: MRI findings. Case Rep Dent. 2011;2011:190592. doi: 10.1155/2011/190592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trasad VA, Devarsa GM, Subba Reddy VV, Shashikiran ND. Peripheral ossifying fibroma in the maxillary arch. J Indian Soc Pedod Prev Dent. 2011;29(3):255–259. doi: 10.4103/0970-4388.85837. [DOI] [PubMed] [Google Scholar]
- 9.Sacks HG, Amrani S, Anderson K. “Gigantiform” peripheral ossifying fibroma: report of a Case. J Oral Maxillofac Surg. 2012 doi: 10.1016/j.joms.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 10.Moon WJ, Choi SY, Chung EC, Kwon KH, Chae SW. Peripheral ossifying fibroma in the oral cavity: CT and MR findings. Dentomaxillofac Radiol. 2007;36(3):180–182. doi: 10.1259/dmfr/59377498. [DOI] [PubMed] [Google Scholar]
- 11.Thierbach V, Quarcoo S, Orlian AI. A typical peripheral ossifying fibroma. A case report. N Y State Dent J. 2000;66(8):26–28. [PubMed] [Google Scholar]
- 12.Kendrick F, Waggoner WF. Managing a peripheral ossifying fibroma. ASDC J Dent Child. 1996;63(2):135–138. [PubMed] [Google Scholar]
- 13.Salum FG, Yurgel LS, Cherubini K, De Figueiredo MA, Medeiros IC, Nicola FS. Pyogenic granuloma, peripheral giant cell granuloma and peripheral ossifying fibroma: retrospective analysis of 138 cases. Minerva Stomatol. 2008;57(5):227–232. [PubMed] [Google Scholar]
- 14.Zhang W, Chen Y, An Z, Geng N, Bao D. Reactive gingival lesions: a retrospective study of 2,439 cases. Quintessence Int. 2007;38(2):103–110. [PubMed] [Google Scholar]
- 15.Bhaskar SN, Jacoway JR. Peripheral fibroma and peripheral fibroma with calcification: report of 376 cases. J Am Dent Assoc. 1966;73:1312–1320. doi: 10.14219/jada.archive.1966.0375. [DOI] [PubMed] [Google Scholar]
- 16.Kfir Y, Buchner A, Hansen LS. Reactive lesions of the gingiva. A clinicopathological study of 741 cases. J Periodontol. 1980;51(11):655–661. doi: 10.1902/jop.1980.51.11.655. [DOI] [PubMed] [Google Scholar]


