Abstract
Around 1 % of oral cancers are metastases from distant sites. Tumor metastases to the jaw bones are uncommon and are most likely to arise from primary lung, breast, prostate or kidney tumors. Jaw bone metastases from a primary esophageal adenocarcinoma are especially rare, with only 7 reports published in the literature. Here, we describe a case of a 69 year-old male patient where 7 years elapsed between the diagnosis and successful treatment of a poorly differentiated, stage pT2N0 primary esophageal adenocarcinoma and re-presentation with jaw pain due to a metastatic mandibular deposit. The morphological appearance of the metastasis and immunohistochemical positivity with CK20, CK7 and CDX2 strongly supported an adenocarcinoma of upper gastrointestinal tract origin. This case is of particular interest as there is an unusually long time between the detection of the primary esophageal adenocarcinoma and diagnosis of metastatic disease. The longest period of time we have found for this in the literature is 9 months, although it is also reported that some oral metastases may appear more than 10 years following the primary tumor diagnosis.
Keywords: Maxillofacial, Metastasis, Esophagus, Adenocarcinoma, Mandible
Introduction
A review of the literature shows that there have been 7 reports describing esophageal adenocarcinoma metastatic to the jaw bones, which are summarized in Table 1. In 2 of these cases, the time elapsing between the original diagnosis of esophageal adenocarcinoma and re-presentation with jaw metastasis was 4 and 9 months, in 3 of the cases, the first presentation was with metastatic disease, and in 2 cases the time between the presentation with the esophageal primary and jaw metastasis was unavailable. Here, we present a case where there was a 7-year interval between detection of the primary esophageal adenocarcinoma and development of metastasis to the mandible.
Table 1.
Reports in the literature of esophageal adenocarcinoma metastases to the jaw bones
| Authors | Time between primary tumor diagnosis and detection of metastasis | Location of metastasis | Age and sex |
|---|---|---|---|
| Lawes et al. (current article) | 7 Years | Left mandible | 69 Male |
| Anderson and Peeples [1] | Concurrent | Left mandibular body and ramus | 61 Male |
| Fontaine et al. [2] | Concurrent | Right mandible | 55 Male |
| Jham and Salama [3] | Unavailable | Mandible | 67 Female |
| Sánchez-Jiménez et al. [4] | 4 Months | Upper left maxilla | 63 Male |
| Tamiolakis et al. [5] | Unavailable | Mandible | Unavailable |
| Tideman et al. [6] | Esophageal tumor diagnosed 4 weeks after jaw metastasis | Left posterior maxilla | 59 Male |
| Willard et al. [7] | 9 Months | Left posterior maxilla | 41 Male |
Case Report
A 69-year-old male was referred urgently by his Dentist to the Maxillofacial Surgery Department with left jaw pain, an inability to open the mouth beyond 20 mm, and gradual swelling of the left mandible of 8 weeks duration. He had a past medical history of bronchiectasis and asbestosis, was an ex-smoker of 30 years with a 10 year pack history, and drank around 45–80 units of alcohol per week. Examination demonstrated a palpable mass lesion involving the left angle and body of the mandible, with numbness of the left lower and upper lip. An orthopantomogram revealed a ‘moth-eaten’ appearance of the bone from the lower left 6 to the mid-ramus (Fig. 1). Biopsies were taken as the differential diagnoses included a primary or secondary neoplasm, or a purely infective process.
Fig. 1.

Orthopantomogram demonstrating a ‘moth-eaten’ appearance of the mandible from the left lower 6 to mid-ramus
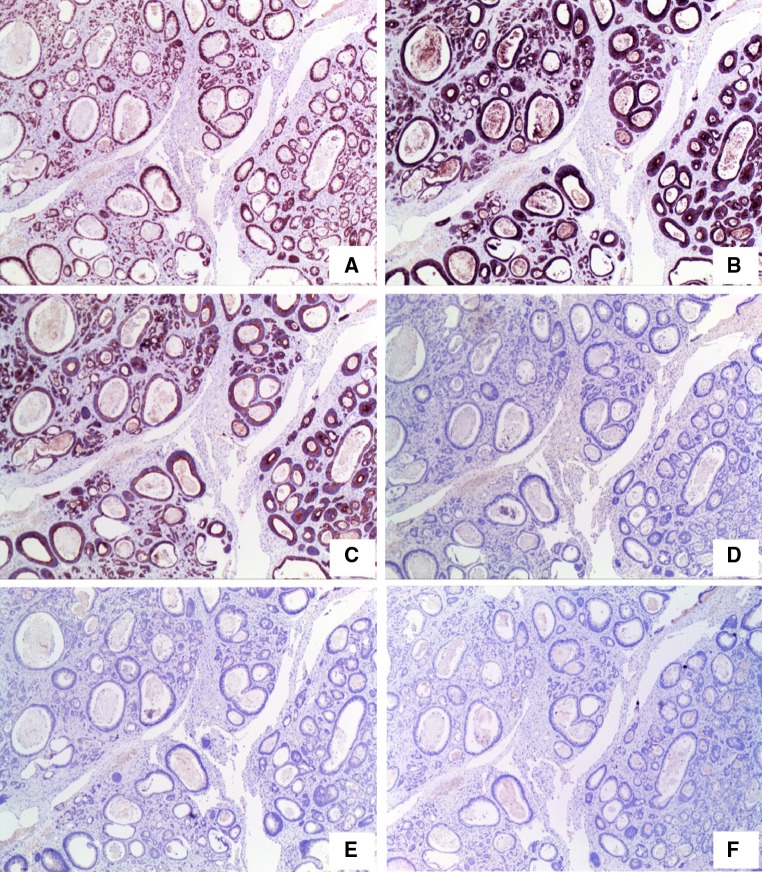
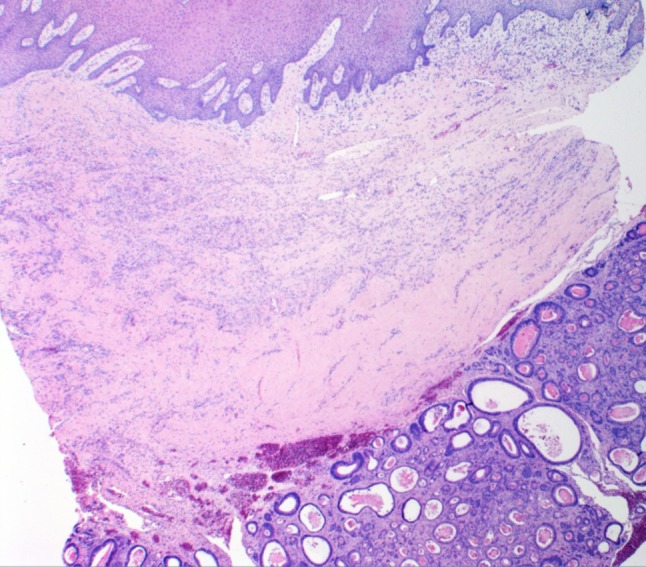
The left retromolar and lower left 8 socket biopsies showed squamous mucosa with underlying corium and a deep-seated tumor composed of ducts with some cystic dilatation, and cytologically atypical, mitotically active cells (Fig. 2). These gave strong immunohistochemical positivity for CK20, CK7 and CDX2 and were negative for PSA, TTF1 and CK5/6 (Fig. 3). This pattern favoured metastatic adenocarcinoma consistent with gastrointestinal tract origin, including the pancreatic and hepatobiliary tract, although a primary intraosseous adenocarcinoma of the mandible could not be completely excluded. Additional clinical information was obtained that 7 years previously, the patient had a 35 × 25 mm pT2N0 moderately to poorly differentiated adenocarcinoma confined to the esophagus at 30 cm (Fig. 4). A review of the slides showed that the esophageal tumor was morphologically similar on microscopy (Fig. 5) to the mandibular metastasis (Fig. 2). The esophageal primary tumor had been successfully treated with two cycles of neo-adjuvant cisplatin followed by esophago-gastrectomy. There had been no recurrence seen on imaging or endoscopic follow-up.
Fig. 2.
Left retromolar biopsy showing metastatic adenocarcinoma
Fig. 3.
Left retromolar biopsy showing metastatic esophageal adenocarcinoma with immunohistochemical positivity for CDX-2 (a), CK20 (b) and CK7 (c) and negativity for PSA (d), TTF1 (e) and CK5/6 (f)
Fig. 4.
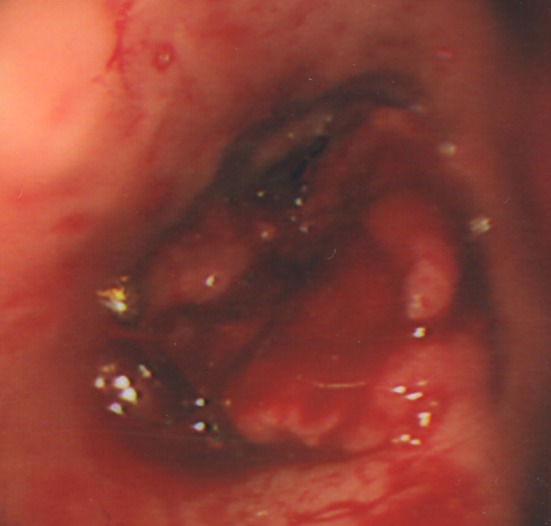
Endoscopic image of primary esopghageal adenocarcinoma at 30 cm
Fig. 5.
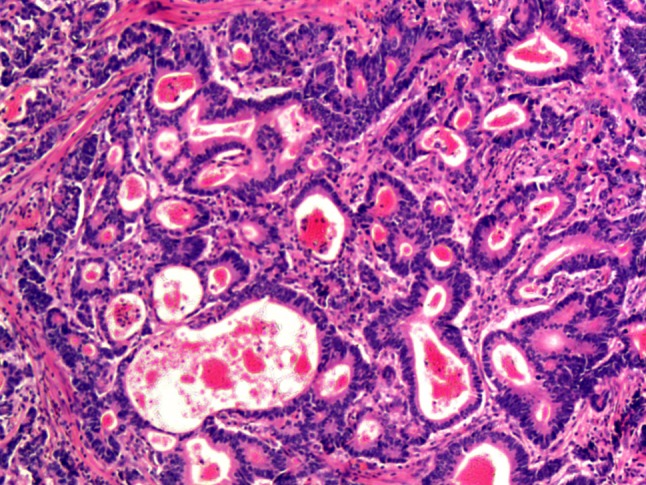
Moderate to poorly differentiated primary esophageal adenocarcinoma with similar morphology to the mandibular metastasis (Fig. 2)
Further to the histological diagnosis, computer and positron emission tomography revealed a 40 mm expansile destructive lesion arising from the left angle of the mandible (Fig. 6), with additional metastases to the right humerus, pelvis and both proximal femora (Fig. 7). The patient received palliative radiotherapy.
Fig. 6.
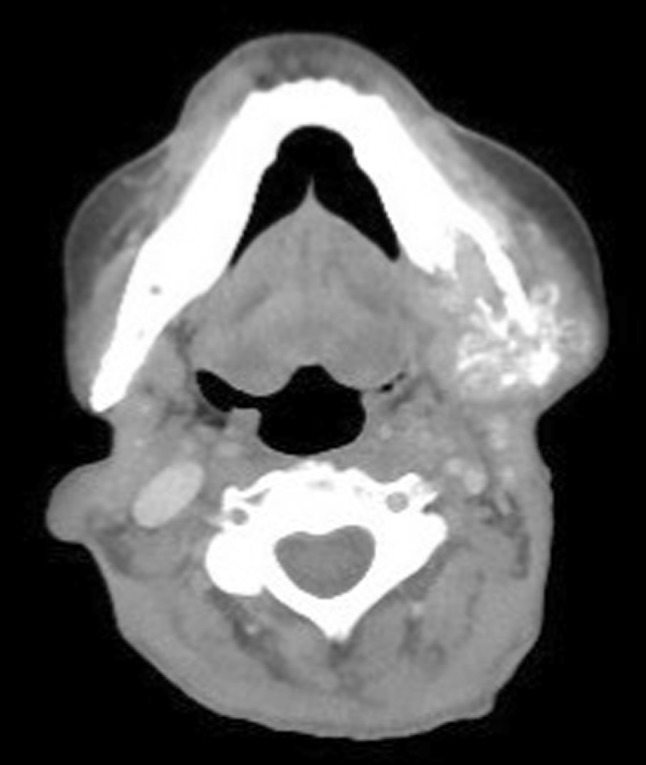
CT image showing the expansile destructive metastasis arising from the left angle of the mandible
Fig. 7.

Positron emission tomography image demonstrating metastatic deposits in the left mandible, right humerus, pelvis and both proximal femora
Discussion
The case showed strikingly similar histological morphology between the primary esophageal tumor and mandibular metastasis (Figs. 2, 5), supported by immunohistochemistry (Fig. 3). Clausen and Poulsen [8] defined strict criteria for diagnosis of true jaw metastasis, in that there should be histological similarity between the primary tumor and metastasis, with intervening healthy tissue between. The presence of jawbone deposits usually indicates late-stage disease with multiple metastases and a poor prognosis [9]. In our case, once the histological diagnosis of a metastasis was established, positron emission tomography was performed which showed widespread bony involvement. The age of our patient was 69, which is typical for presentation with jaw metastases, usually being between the 5th and 7th decades [10]. The patient’s smoking and alcohol history, along with advancing age would be major risk factors for the development of carcinoma [9]. There was a long interval of 7 years between the initial detection of the primary esophageal adenocarcinoma and diagnosis of jaw metastasis. The average time between the diagnosis of a primary tumor and jaw metastases is 40 months, although some cases have been noted to be over 10 years [10].
Metastases to the jawbones are rare. Hirshberg et al. [10] found that the most common metastases to the jaws in men were lung, prostate, liver and kidney, and in women were breast, adrenal, female genital organs and colo-rectum. The prevalence of oral metastases has been linked to the incidence of the primary cancer occurring in a given population [11]. Jawbone metastases are considered to occur through hematogenous spread with the mandible more frequently affected than the maxilla, which is thought to be due to the greater presence of hematopoietic cells in the mandible [3, 9, 12]. The literature shows that oral trauma including tooth extraction may be associated with metastatic disease. In many of these cases the underlying tumor is likely to be present prior to surgery, while in others, the inflammation and vascular changes may be a promoting factor in establishing deposits [9, 10].
D’Silva et al. [13] state that it is important for Dentists investigating patients with apparent dental-related pain and a history of malignancy to consider the possibility of metastatic disease. Hirshberg et al. [10] also note that rapid swelling, pain and paraesthesia can be cardinal symptoms of jaw metastases, as in our case where the patient also presented with an inability to open the mouth fully.
In conclusion, we present a rare case of primary esophageal adenocarcinoma and mandibular metastasis with an unusual length of time, 7 years, between initial diagnosis and detection of metastatic disease. This case emphasizes the importance for dentists, clinicians and diagnostic histopathologists examining the oral region to be aware of a prior clinical history regarding cancer.
References
- 1.Anderson RS, Peeples WJ. Mandibular osseous metastasis from esophageal carcinoma: a case report and review of the literature. J Oral Maxillofac Surg. 1990;48:188–192. doi: 10.1016/S0278-2391(10)80208-3. [DOI] [PubMed] [Google Scholar]
- 2.Fontaine R, Warter P, Lang G. Apropos of a case of the lower thoracic esophagus, until then latent, revealed by an osseous metastasis in a condyle of the inferior maxilla. Arch Mal Appar Dig Mal Nutr. 1961;50:1050–1056. [PubMed] [Google Scholar]
- 3.Jham BC, Salama AR, McClure SA, et al. Metastatic tumors to the oral cavity: a clinical study of 18 cases. Head Neck Pathol. 2011;5:355–358. doi: 10.1007/s12105-011-0286-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sánchez-Jiménez J, Acebal-Blanco F, Arévalo-Arévalo RE, et al. Metastatic tumours in upper maxillary bone of esophageal adenocarcinoma. A case report. Med Oral Patol Oral Cir Bucal. 2005;10:252–257. [PubMed] [Google Scholar]
- 5.Tamiolakis D, Tsamis I, Thomaidis V, et al. Jaw bone metastases: four cases. Acta Dermatovenerol Alp Panonica Adriat. 2007;16:21–25. [PubMed] [Google Scholar]
- 6.Tideman H, Arvier JF, Bosanquet AG, et al. Esophageal adenocarcinoma metastatic to the maxilla. Oral Surg Oral Med Oral Pathol. 1986;62:564–568. doi: 10.1016/0030-4220(86)90322-1. [DOI] [PubMed] [Google Scholar]
- 7.Willard CC, Weber CR, Buche W. Metastatic esophageal adenocarcinoma involving the maxilla. J Oral Maxillofac Surg. 2002;60:1496–1499. doi: 10.1053/joms.2002.36137. [DOI] [PubMed] [Google Scholar]
- 8.Clausen F, Poulsen H. Metastatic carcinoma of the jaws. Acta Pathol Microbiol Scand. 1963;57:361–374. doi: 10.1111/j.1699-0463.1963.tb05105.x. [DOI] [PubMed] [Google Scholar]
- 9.Muttagi SS, Chaturvedi P, D’Cruz A, et al. Metastatic tumors to the jaw bones: retrospective analysis from an Indian tertiary referral center. Indian J Cancer. 2011;48:234–239. doi: 10.4103/0019-509X.82894. [DOI] [PubMed] [Google Scholar]
- 10.Hirshberg A, Shnaiderman-Shapiro A, Kaplan I, et al. Metastatic tumours to the oral cavity—pathogenesis and analysis of 673 cases. Oral Oncol. 2008;44:743–752. doi: 10.1016/j.oraloncology.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 11.Daley T, Darling MR. Metastases to the mouth and jaws: a contemporary Canadian experience. J Can Dent Assoc. 2011;77:b67. [PubMed] [Google Scholar]
- 12.Hirshberg A, Buchner A. Metastatic tumours to the oral region. An overview. Eur J Cancer B Oral Oncol. 1995;31B:355–360. doi: 10.1016/0964-1955(95)00031-3. [DOI] [PubMed] [Google Scholar]
- 13.D’Silva NJ, Summerlin DJ, Cordell KG, et al. Metastatic tumors in the jaws: a retrospective study of 114 cases. J Am Dent Assoc. 2006;137:1667–1672. doi: 10.14219/jada.archive.2006.0112. [DOI] [PubMed] [Google Scholar]