Abstract
Purpose
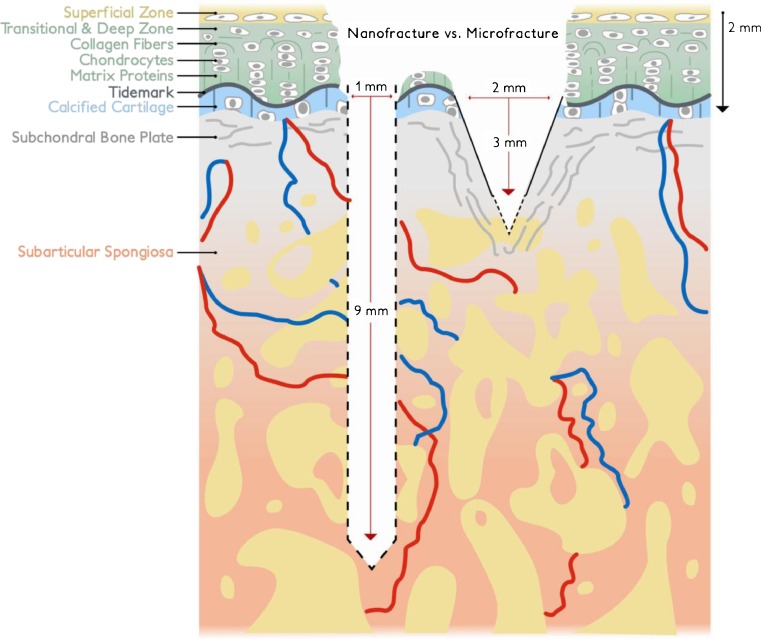
The potential of subchondral mesenchymal stem cell stimulation (MSS) for cartilage repair has led to the widespread use of microfracture as a first line treatment for full thickness articular cartilage defects. Recent focus on the effects of subchondral bone during cartilage injury and repair has expanded the understanding of the strengths and limitations in MSS and opened new pathways for potential improvement. Comparative studies have shown that bone marrow access has positive implications for pluripotential cell recruitment, repair quality and quantity, i.e. deeper channels elicited better cartilage fill, more hyaline cartilage character with higher type II collagen content and lower type I collagen content compared to shallow marrow access.
Methods
A subchondral needling procedure using standardised and thin subchondral perforations deep into the subarticular bone marrow making the MSS more consistent with the latest developments in subchondral cartilage remodelling is proposed.
Results
As this is a novel method clinical studies have been initiated to evaluate the procedure especially compared to microfracturing. However, the first case studies and follow-ups indicate that specific drills facilitate reaching the subchondral bone marrow while the needle size makes perforation of the subchondral bone easier and more predictable. Clinical results of the first group of patients seem to compare well to microfracturing.
Conclusion
The authors suggest a new method for a standardised procedure using a new perforating device. Advances in MSS by subchondral bone marrow perforation are discussed. It remains to be determined by clinical studies how this method compares to microfracturing. The subchondral needling offers the surgeon and the investigator a method that facilitates comparison studies because of its defined depth of subchondral penetration and needle size.
Keywords: Mesenchymal stem cell stimulation, Full thickness cartilage defect repair, Comparison with microfracture, New harvesting device
Introduction
The potential of mesenchymal stem cell stimulation (MSS) for cartilage repair has been recognised since the 1950s and was first introduced by Pridie [1]. Further development, particularly by Steadman et al. since the 1990s [2], has led to widespread use of microfracture as a primary procedure for full thickness cartilage defects due its low cost, ease of operation, and positive results especially in the younger patient population [3–7]. Microfracture induced pluripotential cell recruitment and migration to the joint surface followed by cell differentiation in chondrogenic and other cell lineages has been demonstrated in previous studies [4, 8, 9]. However, a consensus regarding a standardised application (e.g. diameter and depth of perforations, pattern, and spacing) of microfracture has not been reported. There is also no unity on the devices used to perform microfracture (drill, chondropick, manual or mechanical application). Renewed attention to the effects of subchondral bone in cartilage repair has opened new pathways for potential improvement in particular as they relate to channel formation and depth, cell recruitment, and the ensuing cartilage quantity and quality [10, 11]. The authors introduce a new subchondral needling procedure (Nanofracture®, Arthrosurface, MA, USA) recently cleared by the US Food and Drug Administration, with a device and technique that standardises and further develops the application of microfracture, whereby the needle diameter is thinner compared to microfracture and the depth of subchondral bone perforation is deeper and defined thus following the latest findings in MSS. This system includes a cannulated pick with a 15° angled tip to facilitate access to the defect site (Fig. 1). Subchondral bone perforations are carried out with a one millimetre thick needle (nitinol) that is advanced through the cannulated pick (Fig. 2) to a precise depth of nine millimetres. The nitinol needle underwent testing according to ASTM to conform to industry manufacturing standards of medical devices. No breakages have been reported to date.
Fig. 1.
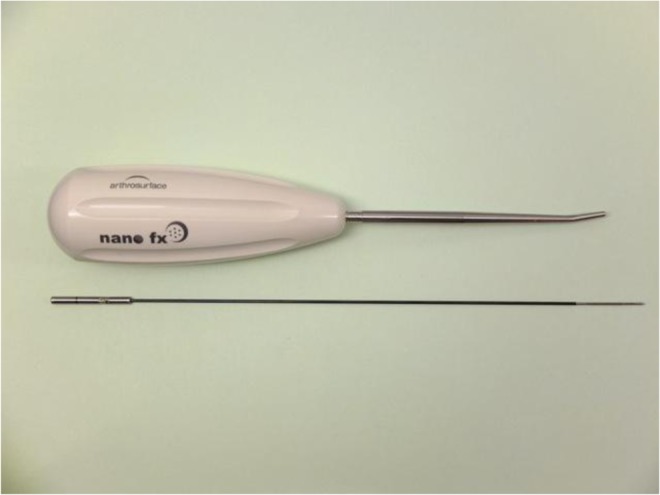
Nanofracture© 15° angled, cannulated pick and needle
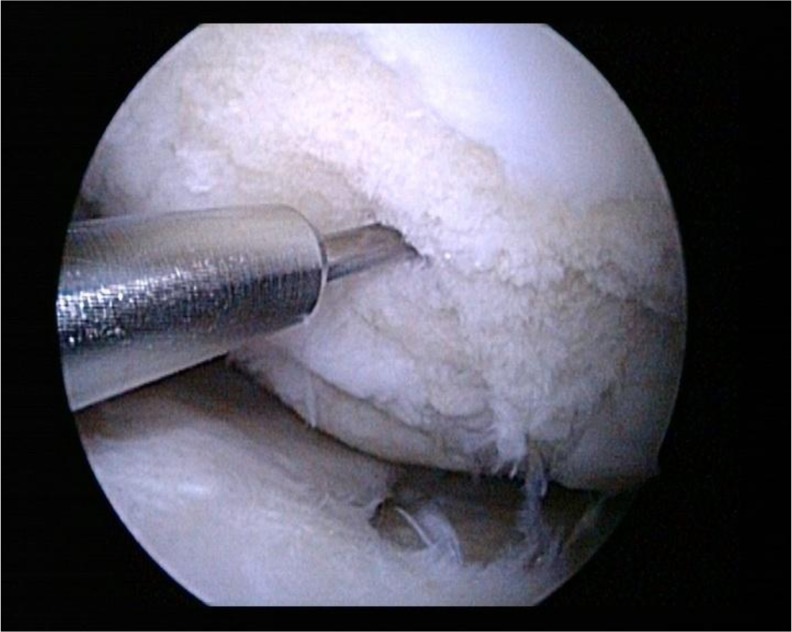
Fig. 2.
Tip of Nanofracture© needle after insertion into an ICRS grade IV cartilage defect
Penetration depth is suggested at a defined length of nine millimetres. This was established after cadaver studies showed that a longer needle would have a higher risk of wire fracture without necessarily offering any advantage. However, the exact length of subchondral penetration remains to be determined and is not as yet defined in the literature. Chen [11] sees a dependency of depth of penetration and bone marrow stimulation, i.e. the deeper the penetration, the better the bone marrow seems to be stimulated.
Indications, outcome predictors and contraindications
After failed conservative management, patients with clear symptomatology and adequate cartilage lesion(s) on pre-operative magnetic resonance imaging (MRI) should be considered for surgery. The final decision is made during knee arthroscopy and depends on lesion characteristics and general joint status. Symptomatic full-thickness chondral defects, without extensive subchondral bony deficiency and a lesion size of up to 2 × 2 cm have shown more consistent results [12–14]. Defects with depths of five to ten mm have limited indications and lesions greater than ten mm deep should not be considered for MSS [12]. Every patient presents with a unique set of parameters (Table 1) and while the perfect patient rarely exists, the compounding effects of multiple factors should be taken into consideration when creating a patient profile and discussing treatment options and patient expectations (Table 1).
Table 1.
Indications and outcome predictors in subchondral cartilage stimulating surgery
| Factors | Better results with: |
|---|---|
| Age [15] | <40 years |
| Duration of symptoms [15] | <12 months |
| Lesion size [15] | up to 2 × 2 cm |
| Lesion depth [15] | <5 mm |
| Body mass index [15] | <30 kg/m2 |
| Preoperative activity level Tegner score [15] | >4 |
| Previous surgery [15] | Primary microfracture |
| Repair cartilage volume [15] | Good defect fill (>66 %) |
| Mechanical alignment [16] | Normal |
| Joint anatomy [16] | Normal |
| Joint stability [16] | Ligamentously stable with adequate muscle strength |
| Meniscus [17] | Without loss of meniscal tissue |
| Kissing lesion | Monopolar |
Mechanical malalignment and joint instability may lead to or aggravate cartilage defects and joint degeneration in particular when they both occur within the same joint [18, 19] and should be addressed at the same time as cartilage repair surgery. A corrective osteotomy to re-establish neutral mechanical axis should be performed in conjunction with the cartilage procedure in varus malalignment in the knee. Similarly, patella maltracking should be simultaneously corrected if addressing patello-femoral cartilage lesions. General contraindications include patients who are unwilling or unable to follow rehabilitation requirements, inability to use the opposite leg for weight bearing, partial thickness defects, widespread articular and joint degeneration and possibly kissing lesions [20].
Patient profiling and quality control
All patients present with a unique combination of joint status, injury mechanism, defect location, size and grade, comorbidities, activity requirements, and a distinctive set of outcome predictors. Algorithmic treatment recommendations based on averaged results rarely do justice to the complex interaction between patient profile, intraoperative findings and treatment, and postoperative remodelling. Individual treatment and management of patient expectations therefore is paramount for success in the level of treatment effect, and the durability of MSC (Table 1). Bone marrow stimulation (BMS) is an arthroscopic procedure where the treatment effect is triggered intra-operatively, but the actual repair occurs during the postoperative recovery phase. The biphasic regimen places challenges on quality control and reproducibility of the results. Subchondral needling offers an advantage over microfracture because perforation depth and diameter are consistent and reproducible (Fig. 3). The procedure may also be applied in cartilage defects type ICRS 2 and 3 where stabilised remaining cartilage is preserved as a matrix for the newly developing cartilage tissue. In conventional microfracture, however, depending on how much force is exerted upon the microfracture awl, the depth of subchondral bone perforations remains inconsistent along with the surface diameter of each perforation due to the V-shaped tip. This may negatively impact the validation and comparison among different patient cohorts, anatomical locations, and defect sizes. The pick has a stop-controlled perforation depth of nine millimetres at a consistent diameter of one millimetre. The smaller diameter causes less trauma to the subchondral bone surface and may provide a greater perforation density compared to the much larger 2.5-mm microfracture awl when the reported bone bridge distance of two to four millimetre is maintained [3, 21, 22]. However, cell recruitment has to be quantified before final recommendations for needle spacing and pattern density can be made.
Fig. 3.
Demonstrating the difference between the deeper Nanofracture© (left) which reaches the subchondral bone plate more regularly, in a consistent cylindrical shape and at a more defined depth than microfracture (right)
Surgical technique
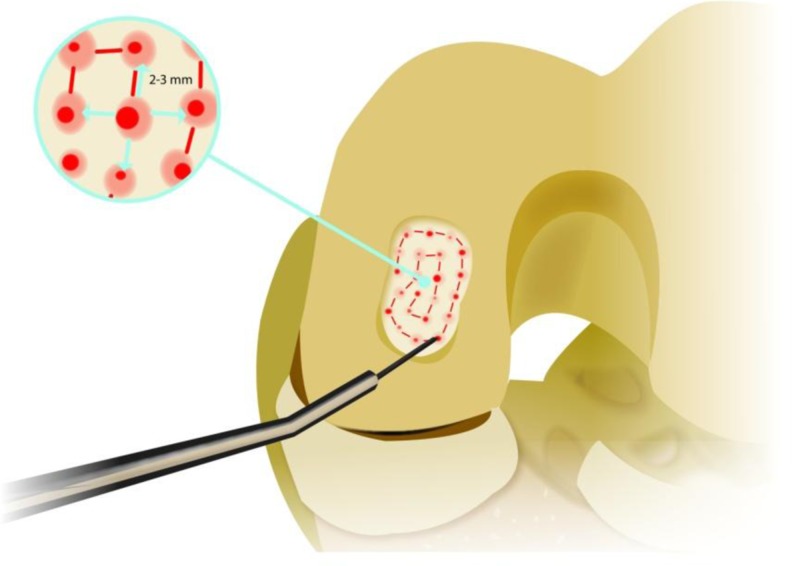
Debridement of unstable cartilage is carried out until healthy margins and vertical walls are created. In lesions graded ICRS 2 and 3, fixed cartilage may be left as a matrix for regeneration. Upon completion of the defect preparation, subchondral needling is performed in a systematic, spiral fashion starting from the periphery of the lesion. The one millimetre needle is inserted into the lumen of the pick. The tip of the pick is placed onto the prepared defect bed and slight hammer strikes on the proximal end of the needle advance the tip into the subchondral bone at a consistent, stop-controlled depth of nine millimetres with no thermal damage to the tissue. The needle is removed and consecutive subchondral bone channels are placed throughout the defect bed in a defined pattern (Fig. 4). Each perforation is placed about three millimetres apart to give an even distribution. Adequate bone bridges between each channel should be maintained to protect the mechanical stability of subchondral bone during postoperative remodelling. A joint lavage concludes the procedure to remove loose bony particles and cartilage debris. Intra-articular drains should not be used to avoid interference with marrow clot formation, cell recruitment and differentiation.
Fig. 4.
Bone perforation pattern with a 3–4 mm bone bridge distance
Postoperative rehabilitation
Clinical studies [17, 23] give mixed recommendations about postoperative weight bearing restrictions. However, limited weight-bearing is not only important for articular cartilage repair, but also for protection of subchondral bone remodelling after microfracture. Osteoarticular remodelling and maturation during this phase continues beyond three to six months after surgery and should be considered when discussing treatment options with patients. Premature weight bearing may lead to displacement of the repair clot, inferior tissue integration, and may also damage the subchondral bone integrity and tissue response to load bearing stimuli during the healing phase. Patient and therapist compliance is therefore critical [21].
Discussion
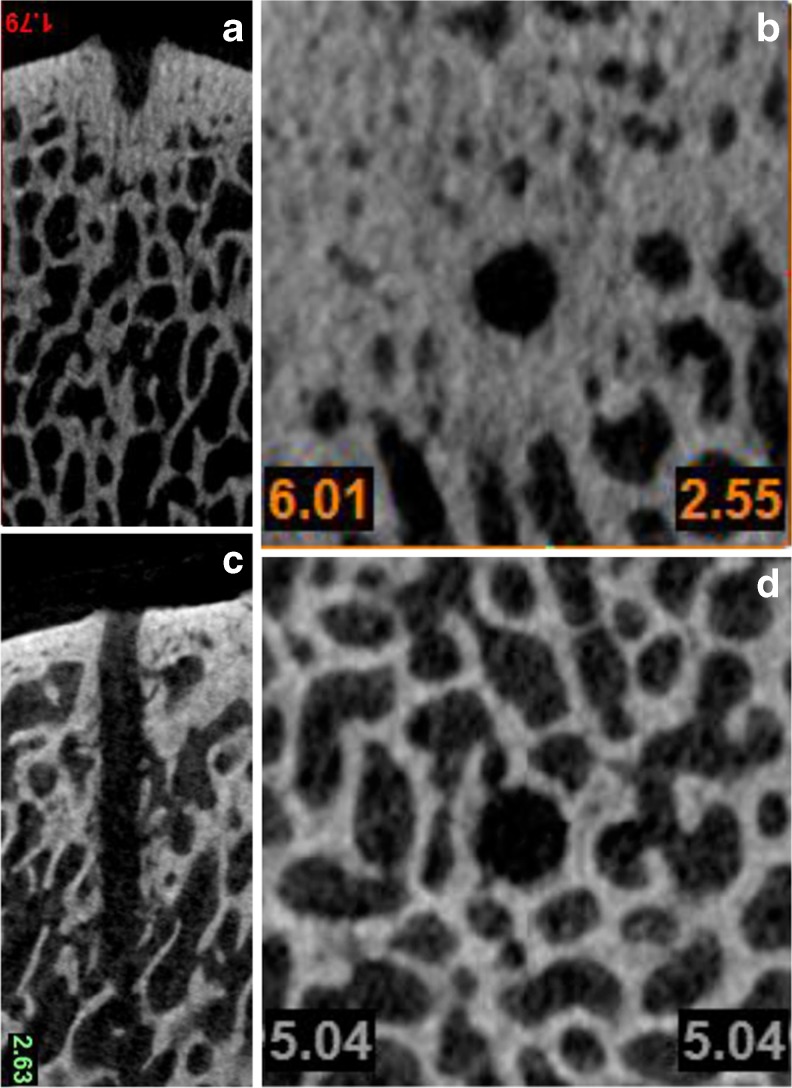
Results in cartilage repair with BMS and tissue engineered combination therapies depend on a systematic, quality controlled approach. Standardised procedures are necessary to improve future outcomes and help in a better understanding of the interaction between patient profile, operative procedure, and postoperative remodelling and rehabilitation. Bone marrow stimulation (BMS) is a complex entity and relies on a large number of factors influencing fill rate and grade, subchondral and lateral tissue integration, and biomechanical integrity and functional response to load sharing. Combined, they affect the longevity of the defect fill, the functional improvement and pain relief in patients and the protection from lesion expansion and degenerative pathways over time. The age-dependent response to MSS is well understood today—cell numbers and their synthetic activity decline over time leading to a lower defect fill rate with inferior tissue quality in older patients [5, 24]. As a result, the clinical success rate of microfracture has been most consistent in patients under the age of 40 years [5–7, 25, 26]. In addition to age restrictions, renewed interest in seeing cartilage damage in the context of the entire osteochondral architecture shows that the interaction between bone and cartilage is probably a complex system that influences repair response and durability of treatment regimens in all age groups [20, 27]. Chen et al. [11] compared subchondral cell recruitment at various depths. Results from histomorphometry and histological scoring found that deeper access channels to the marrow stroma produced statistically superior cartilage repair when compared to shallower channels. This is in contrast to the commonly accepted two to four millimetre depth used in conventional microfracture [3, 11, 21]. In addition to channel depth affecting cell recruitment, histology and micro-CT examinations of two millimetre deep microfracture awl perforations showed fracturing and bone compaction around each channel, sealing them largely off from adjacent bone marrow [10] (Fig. 5).
Fig. 5.
a–d Axial and sagittal microCT imaging. Adult bovine model courtesy of W.R. Walsh, Ph.D., N. Bertollo, Ph.D., D. Schaffner, M.D., R. Oliver, Ph.D., C. Christou BScVet. Surgical & Orthopaedic Research Laboratories (SORL), Prince of Wales Clinical School–The University of New South Wales, Sydney, Australia 2013. a Sagittal microCT following microfracture: dense bone compaction extending into cancellous bone with limited trabecular bone marrow channels. b Axial microCT depicting dense, compacted channel walls with well defined, highly regular channel walls. c Sagittal microCT following nanofracture: multiple open trabecular channels throughout the 9-mm deep subchondral bone perforation. d Axial microCT after nanofracture showing irregular wall outline and open trabecular channels. Trabecular bone structure appears to have normal thickness and density
The larger footprint of V-shaped microfracture perforations (1.5–2 mm wide) may expose a larger surface to the metabolic bone response following iatrogenic injury of the subchondral bone plate (Figs. 4 and 5). This may also play a role in subchondral bone stability, particularly when pattern density becomes too high and bone bridges between each perforation too small. Combined with postoperative weight bearing, microfracture perforations may stimulate an excessive bone response which may explain observations such as intralesional osteophytes and defect overgrowth [23, 27–30].
Consistent needle diameter and a smaller perforation footprint introduces less trauma to the subchondral bone plate and subarticular bone marrow. The influence of joint fluid pressure acting on each perforation is not well understood, but perforation density and diameter may play a role in subchondral cyst formation seen after microfracture, in particular when combined with weight bearing loads during the weakened remodelling state [23, 28, 29, 31]. The importance of individual surgical steps to maximise the tissue response in MSS is debated in the literature—concomitant procedures are performed first to avoid losing arthroscopic visualisation once subchondral blood and fatty droplets enter the joint [32]. Debridement of degenerated and unstable cartilage [3, 15, 21, 33, 34] and creation of healthy, vertical walls at the defect edge [3, 12, 13] prepare the lesion bed initially. Controversy still exists regarding removal of the thin calcified cartilage layer. Advocates [3, 15, 22, 26] refer to the work of Frisbie et al. [32, 35] who demonstrated better attachment of repair tissue following microfracture once the calcified layer was removed. However, challenges in postoperative defect protection in the equine model combined with the lack of technical reports such as perforation depth, bleeding response, and perforation density may have played a role in tissue bonding rather than the difference in defect preparation. Frisbie et al. [35] also reported advanced thickening or elevation of subchondral bone after removal of the calcified layer. The associated increase in stiffness may explain why secondary cell-based cartilage interventions achieve inferior results after microfracture when compared to their primary indications [5, 6, 10, 21, 31]. Authors who support the removal of the calcified layer are in agreement that attention must be paid to maintain the underlying bone plate and avoid excessive debridement and thinning as this is thought to stimulate the osseous response with further subchondral bone thickening and overgrowth [3, 21, 22, 30, 36]. Close arthroscopic visualisation and careful attention to technical details is therefore recommended [2, 15, 26, 37]. Future standardised investigations will need to provide further evidence on the depth of defect bed preparation and the pros and cons of maintaining distinct layers of the osteochondral architecture. Renewed focus on subchondral bone effects in cartilage injury and repair [21, 23, 27] has expanded the understanding of the strengths and limitations of MSS [4, 8, 38] and opened new pathways for potential improvement, in particular as they relate to channel depth, shape, diameter and the corresponding cell recruitment. The effects on the osteochondral architecture during subchondral bone remodelling, surface chondrogenesis and tissue repair are better understood today, but the surgical procedure is in need of standardisation to optimise individual outcomes of MSS in focal cartilage repair and improve comparability among various patient cohorts.
Conclusion
Microfracture’s shortcomings such as shallow marrow access, inconsistent depth, large diameter perforation, and intra-channel bone compaction have implications for quantity and quality of cartilage repair, subchondral bone stability, and rehabilitation requirements. Deeper marrow access with its improvement of cartilage character and volume provides a new direction. Thin, stop-controlled, deep needle perforation without associated thermal injury allows for a systematic and less traumatic treatment approach and benchmark testing in future clinical investigations. Further studies comparing the different methods of BMS are encouraged.
Contributor Information
Jan P. Benthien, Phone: +41-814148118, FAX: +41-814148120, Email: jbenthien@spitaldavos.ch
Peter Behrens, Email: orthobehr@web.de.
References
- 1.Pridie KH. A method of resurfacing osteoarthritic knee joints. J Bone Joint Surg. 1959;41B:618–619. [Google Scholar]
- 2.Steadman JR, Rodkey WG, Singleton SB, Briggs KK. Microfracture technique for full thickness chondral defects: technique and clinical results. Oper Tech Orthop. 1997;7:300–304. doi: 10.1016/S1048-6666(97)80033-X. [DOI] [Google Scholar]
- 3.Asik M, Ciftci F, Sen C, Erdil M, Atalar A. The microfracture technique for the treatment of full-thickness articular lesions of the knee: midterm results. Arthroscopy. 2008;24(11):1214–1220. doi: 10.1016/j.arthro.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 4.Kramer J, Böhrnsen F, Lindner U, Behrens P, Schlenke P, Rohwedel J. In vivo matrix-guided human mesenchymal stem cells. Cell Mol Life Sci. 2006;63(5):616–626. doi: 10.1007/s00018-005-5527-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kreuz PC, Steinwachs MR, Erggelet C, Krause SJ, Konrad G, Uhl M, Sudkamp N. Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthr Cartil. 2006;14:1119–1125. doi: 10.1016/j.joca.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Mithoefer K, Williams RJ, Warren RF, Potter HG, Spock CR, Jones EC, Wickiewicz TL, Marx RG. The microfracture technique for the treatment of articular cartilage lesions in the knee. A prospective cohort study. J Bone Joint Surg. 2005;87A:1911–1920. doi: 10.2106/JBJS.D.02846. [DOI] [PubMed] [Google Scholar]
- 7.Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG. Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy. 2003;19(5):477–484. doi: 10.1053/jars.2003.50112. [DOI] [PubMed] [Google Scholar]
- 8.Khan WS, Johnson DS, Hardingham TE. The potential of stem cells in the treatment of knee cartilage defects. Knee. 2010;17:369–374. doi: 10.1016/j.knee.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 9.Shapiro F, Koide S, Glimcher MJ. Cell origin and differentiation in the repair of full-thickness defects of articular cartilage. J Bone Joint Surg Am. 1993;75:532–553. doi: 10.2106/00004623-199304000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Chen H, Sun J, Hoeman CD, Lascau-Coman V, Ouyang W, McKee MD, Shive MS, Buschamnn MD. Drilling and microfracture lead to different bone structure and necrosis during bone-marrow stimulation for cartilage repair. J Orthop Res. 2009;27:1432–1438. doi: 10.1002/jor.20905. [DOI] [PubMed] [Google Scholar]
- 11.Chen H, Hoemann CD, Sun J, Chevrier A, McKee MD, Shive MS, Hurtig M, Buschmann MD. Depth of subchondral perforation influences the outcome of bone marrow stimulation cartilage repair. J Orthop Res. 2011;29(8):1178–1184. doi: 10.1002/jor.21386. [DOI] [PubMed] [Google Scholar]
- 12.Cole BJ, Cohen B. Chondral injuries of the knee: a contemporary view of cartilage restoration. Orthop Spec Ed. 2000;6:71–76. [Google Scholar]
- 13.Gomoll AH, Madry H, Knutsen G, van Dijk N, Seil R, Brittberg M, Kon E. The subchondral bone in articular cartilage repair: current problems in the surgical management. Knee Surg Sports Traumatol. 2010;18:434–447. doi: 10.1007/s00167-010-1072-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Minas T, Gomoll A, Solhpour S, Rosenberger R, Probst C, Brynat T. Autologous chondrocyte implantation for joint preservation in patients with early osteoarthritis. Clin Orthop Relat Res. 2009;468:147–157. doi: 10.1007/s11999-009-0998-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mithoefer K, McAdam T, Williams RJ, Kreuz PC, Mandelbaum BR. Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: an evidence-based systematic analysis. Am J Sports Med. 2009;37:2053–2063. doi: 10.1177/0363546508328414. [DOI] [PubMed] [Google Scholar]
- 16.Buckwalter JA, Mankin HJ. Articular cartilage: degeneration and osteoarthritis, repair, regeneration and transplantation. Instr Course Lect. 1998;47:487–504. [PubMed] [Google Scholar]
- 17.Lee SJ, Aadalen KJ, Malaviya P, Lorenz EP, Hayden JK, Farr J, Kang RW, Cole BJ. Tibiofemoral contact mechanics after serial medial meniscectomies in the human cadaveric knee. Am J Sports Med. 2006;34(8):1334–1344. doi: 10.1177/0363546506286786. [DOI] [PubMed] [Google Scholar]
- 18.Gomoll AH, Farr J, Gillogly SD, Kercher J, Minas T. Surgical management of articular defects of the knee. J Bone Joint Surg. 2010;92A(14):2470–2490. [PubMed] [Google Scholar]
- 19.Heijink A, Gomoll AH, Madry H, Drobnic M, Filardo G, Espregueira-Mendes J, Van Dijk CN. Biomechanical considerations in the pathogenesis of osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2012;20:423–435. doi: 10.1007/s00167-011-1818-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Benthien JP, Behrens P. The treatment of chondral and osteochondral defects of the knee with autologous matrix-induced chondrogenesis (AMIC): method description and recent developments. Knee Surg Sports Traumatol. 2011;19:1316–1319. doi: 10.1007/s00167-010-1356-1. [DOI] [PubMed] [Google Scholar]
- 21.Gomoll AH, Filardo G, de Girolamo L, Esprequeira-Mendes J, Marcacci M, Rodkey WG, Steadman RJ, Zaffagnini S, Kon E. Surgical treatment for early osteoarthritis. Part 1: cartilage repair procedures. Knee Surg Sports Traumatol Arthrosc. 2012;20:450–466. doi: 10.1007/s00167-011-1780-x. [DOI] [PubMed] [Google Scholar]
- 22.Mithoefer K, Williams RJ, Warren RF, Potter HG, Spock CR, Jones EC, Wickiewicz TL, Marx RG. Chondral resurfacing of articular cartilage defects in the knee with the microfracture technique. Surgical technique. J Bone Joint Surg. 2006;88A(Suppl 1):294–304. doi: 10.2106/JBJS.F.00292. [DOI] [PubMed] [Google Scholar]
- 23.Orth P, Goebel L, Wolfram U, Ong MF, Gräber S, Kohn D, Cucchiarini M, Ignatius A, Pape D, Madry H. Effect of subchondral drilling on the microarchitecture of subchondral bone: analysis in a large animal model at 6 months. Am J Sports Med. 2012;40(4):828–836. doi: 10.1177/0363546511430376. [DOI] [PubMed] [Google Scholar]
- 24.Hunziker EB. Articular cartilage repair: basic science and clinical progress. A review of the current status and prospects. Osteoarthr Cartil. 2001;10:432–463. doi: 10.1053/joca.2002.0801. [DOI] [PubMed] [Google Scholar]
- 25.Knutsen G, Engebretsen L, Ludvigsen TC, Drogset JO, Grontvedt T, Solheim E, Strand T, Roberts S, Isaksen V, Johansen O. Autologous chondrocyte implantation compared with microfracture in the knee. A randomized trial. J Bone Joint Surg Am. 2004;86:455–464. doi: 10.2106/00004623-200403000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Steadman R, Rodkey WG, Briggs KK. Microfracture: its history and experience of the developing surgeon. Cartilage. 2010;1(2):78–86. doi: 10.1177/1947603510365533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Madry H, Luyten FP, Facchini A. Biological aspects of early osteoarthritis. Knee Surg Sports Traumatol. 2012;20:407–422. doi: 10.1007/s00167-011-1705-8. [DOI] [PubMed] [Google Scholar]
- 28.Richmond J, Mandelbum B, DeDeyne PG. Outcomes after a single-stage procedure for cell-based cartilage repair: a prospective clinical safety trial with 2–year follow-up. Am J Sports Med. 2011;39:1170–1179. doi: 10.1177/0363546511399382. [DOI] [PubMed] [Google Scholar]
- 29.Niemeyer P, Koestler W, Sudkamp NP. Problems and complications of surgical techniques for treatment of full-thickness cartilage defects. Z Orthop Unfall. 2011;149:45–51. doi: 10.1055/s-0030-1250104. [DOI] [PubMed] [Google Scholar]
- 30.Saris DBF, Vanlauwe J, Victor J, Almqvist KF, Verdonk R, Bellemans J, Luyten FP. Treatment of symptomatic cartilage defects of the knee: characterized chondrocyte implantation results in better outcome at 36 months in a randomized trial compared to microfracture. Am J Sports Med. 2009;37(Suppl 1):10S–19S. doi: 10.1177/0363546509350694. [DOI] [PubMed] [Google Scholar]
- 31.Van Dijk C, Reilingh ML, Zengerink M, van Bergan CJA. Osteochondral defects in the ankle: why painful? Knee Surg Sports Traumatol. 2010;18:570–580. doi: 10.1007/s00167-010-1064-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Frisbie DD, Oxford JT, Southwood L, Trotter GW, Rodkey WG, Steadman JR, Goodnight JL, McIlwraith CW. Early events in cartilage repair after subchondral bone microfracture. Clin Orthop Relat Res. 2003;407:215–227. doi: 10.1097/00003086-200302000-00031. [DOI] [PubMed] [Google Scholar]
- 33.Cole BJ, Pascua-Garrido C, Grumet R. Surgical management of articular defects in the knee. J Bone Joint Surg. 2009;91A:1778–1790. [PubMed] [Google Scholar]
- 34.Gille J, Kunow J, Boisch L, Behrens P, Bos I, Hoffman C, Koller W, Risslies M, Kurz B. Cell-laden and cell-free matrix-induced chondrogenesis versus microfracture for the treatment of articular defects: a histological and biomechanical study in sheep. Cartil. 2010;1:29–42. doi: 10.1177/1947603509358721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Frisbie DD, Morisset S, Ho CP, Rodkey WG, Steadman JR, McIlwraith CW. Effects of calcified cartilage on healing of chondral defects treated with microfracture in horses. Am J Sports Med. 2006;34:1824–1831. doi: 10.1177/0363546506289882. [DOI] [PubMed] [Google Scholar]
- 36.Steinwachs MR, Giggi T, Kreuz PC. Marrow stimulation techniques. Inj Int J Care Inj. 2008;3951:S26–S31. doi: 10.1016/j.injury.2008.01.042. [DOI] [PubMed] [Google Scholar]
- 37.Steadman JR, Rodkey WG, Rodrigo JJ. “Microfracture”: surgical technique and rehabilitation to treat chondral defects. Clin Orthop Relat Res. 2001;391:S362–S369. doi: 10.1097/00003086-200110001-00033. [DOI] [PubMed] [Google Scholar]
- 38.McIlwraith CW, Frisbie DD, Rodkey WG, Kisiday JD, Werpy NM, Kawcak CE, Steadman JR. Evaluation of intra-articular mesenchymal stem class to augment healing of microfractured chondral defects. Arthroscopy. 2011;27:1552–1561. doi: 10.1016/j.arthro.2011.06.002. [DOI] [PubMed] [Google Scholar]